د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
The Obstetric history and examination
د
.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
HISTORY TAKING
•
Greeting patients in appropriate way.
•
Introduces yourself to the patient.
•
Puts the patient at ease.
•
Enables the patient to elaborate presenting problem fully.
•
Listens attentively.
•
Use clear language and avoid medical jargon.
Seeks clarification of
words used by the patient as appropriate
•
Phrases questions simply and clearly
•
Identifies the patient's ideas, concerns and expectations
•
Considers physical, social and psychological factors as appropriate
•
Summarize and closing the interview
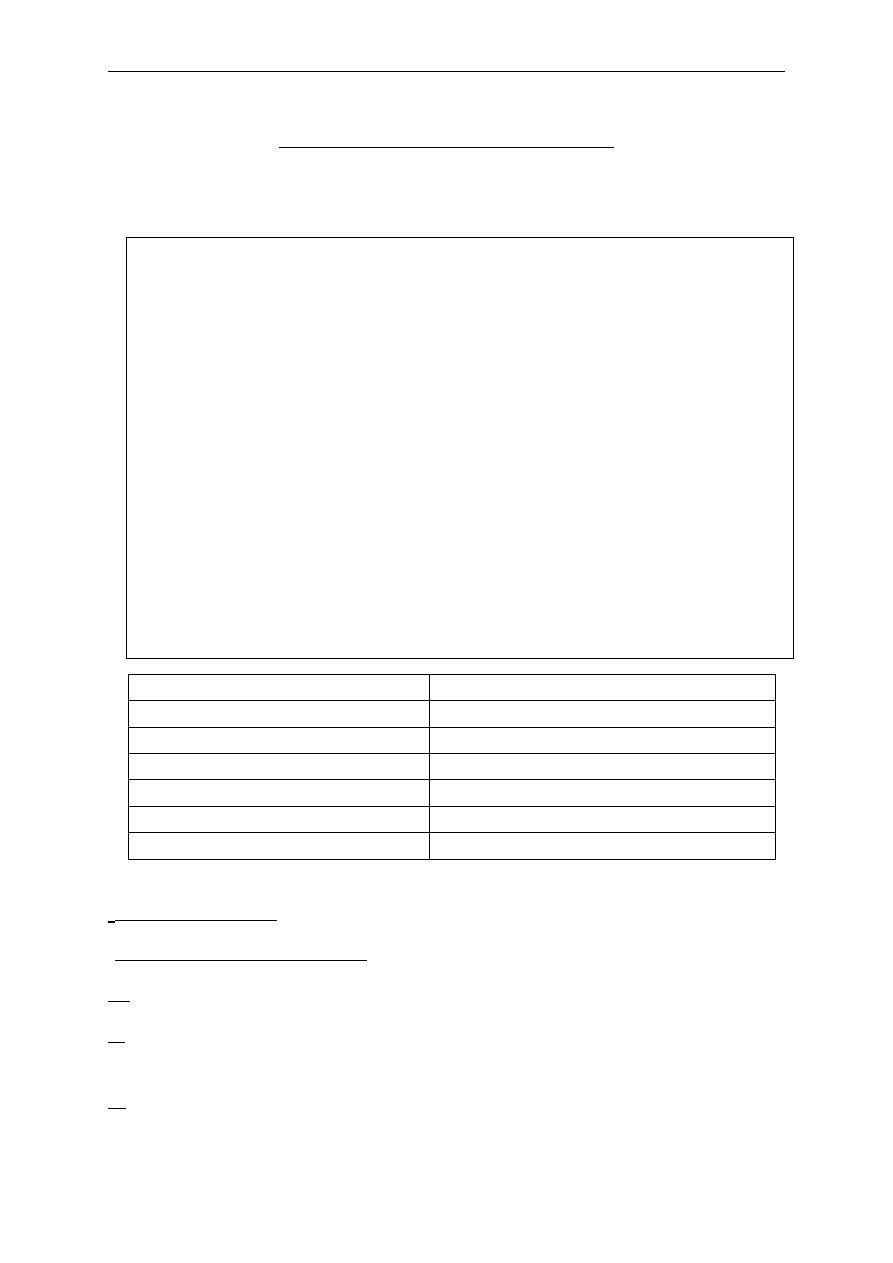
* patient's name
*husband's name
* Age
*age
* Occupation
* Occupation
* Residence
* Residence
* Religion
* Blood group&Rh
* Marital status
* Blood group&Rh
Date of admission:
-
:
Date of delivery or operation
-
ncies regardless of how they ended
. of pregna
No
G:
parity is the number of live births at any gestation or stillbirths after 24
P:
weeks
A: (expulsion of conceptus before 24 weeks gestation)
1
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
If the patient had ectopic or H.mole considered G1 & 1 ectopic or H.mole
Twin preg. Considered as G1 P2
-LMP = First day of the last menstrual period.
1. the patients certainty of dates
2. the regularity of the cycle
3. the use of contraception
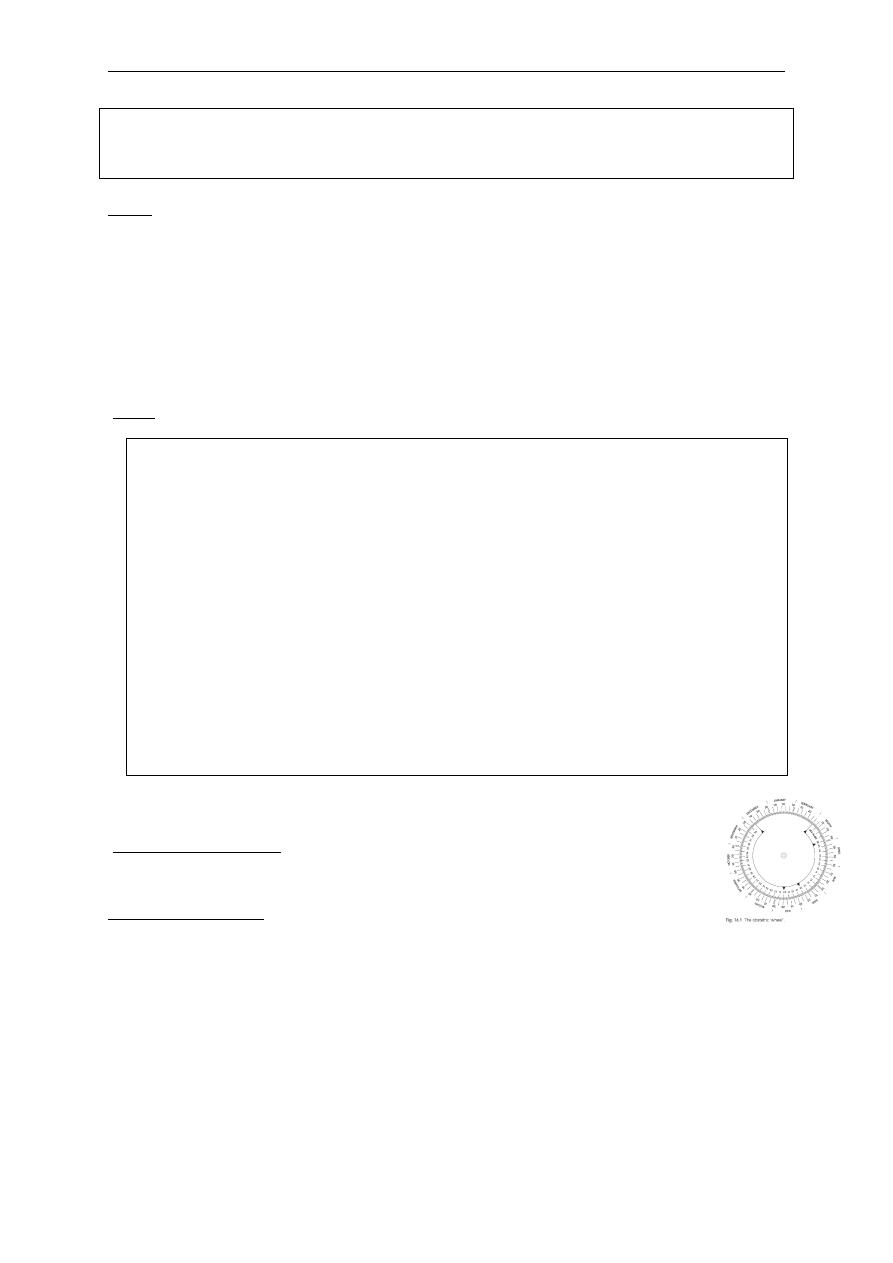
Naegles rule
:
calendar
day of Gregorian
st
Expected date of delivery (1
EDD:
-
What was the first day of her last menstrual period (LMP)? What was
the length of her menstrual cycle and was it regular?
EDD=LMP-3mths+7days (for 28 day cycle)
EDD=LMP+9mths+7days (for 28 day cycle)
For a cycle longer than 28 days:
will be later and needs to be adjusted:
the number of days by which the cycle is longer than 28 is added to the
date calculated using Nägle’s rule
EDD=LMP+9mths/-3mths+7days+ (cycle length−28days)
The reverse applies if the cycle is shorter than 28 days
If a woman has recently stopped the combined oral contraceptive, her
cycles can be anovulatory and LMP is less useful
In the UK, ultrasound between 11 and 13 + 6 weeks is routine, and
considered more accurate even than ‘certain’ dates.
In practice, this can be quickly calculated using an obstetric (wheel)
(until time of delivery or operation
Weeks of gestation
-
or until presentation if the patient still pregnant)
complaint:
Chief
Main complaint (one or more)
In the patient’s own words.
Duration of the complaint
In chronological order
2
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
Common obstetric symptoms are:
Bleeding per vagina, abdominal pain, urinary symptoms, headaches,
reduced fetal movements, Emesis gravidarum, Urinary disturbances, Fetal kicks
& quickening, Late Bleeding, PROM, Contractions
History of presenting complaint:
This section should focus on the presenting complaint
Each of the problems of the patient describes must be
obtained in detail by
questioning regarding:
1. what exactly the problem is
2. When exactly the problem is occurring, the date and time of
onset(Onset, severity, duration)
3. whether the symptoms are getting worse(course)
4. the duration of the symptoms when they do occur
5. And how these symptoms are related to or influence other events in
her life.
6. What increases/decreases the symptom
7. Associated Other symptoms
8. Investigations done (date, place & results)
9. Treatment received (details & response)
10. Any complications
11. Admission history: course of illness, medication given and
investigations done, postoperative course until presentation
Certain important points should always be enquired about
1. Abdominal pain (site, continuous or intermittent, character, relieving and
aggravating factors, radiation and associated symptoms).
2. Vaginal bleeding: Amount of blood loss, passage of clots, associated with
pain or fainting attacks.
3. Vaginal discharge- amount, color, itching, odour, presence of blood.
4. if the patient in the third trimester, ask about fetal movement
5. if the patient is hypertensive or diabetic, ask about time of diagnosis and
the treatment she receive
6. If the patient has similar or related complaints previously mention this
and its timing
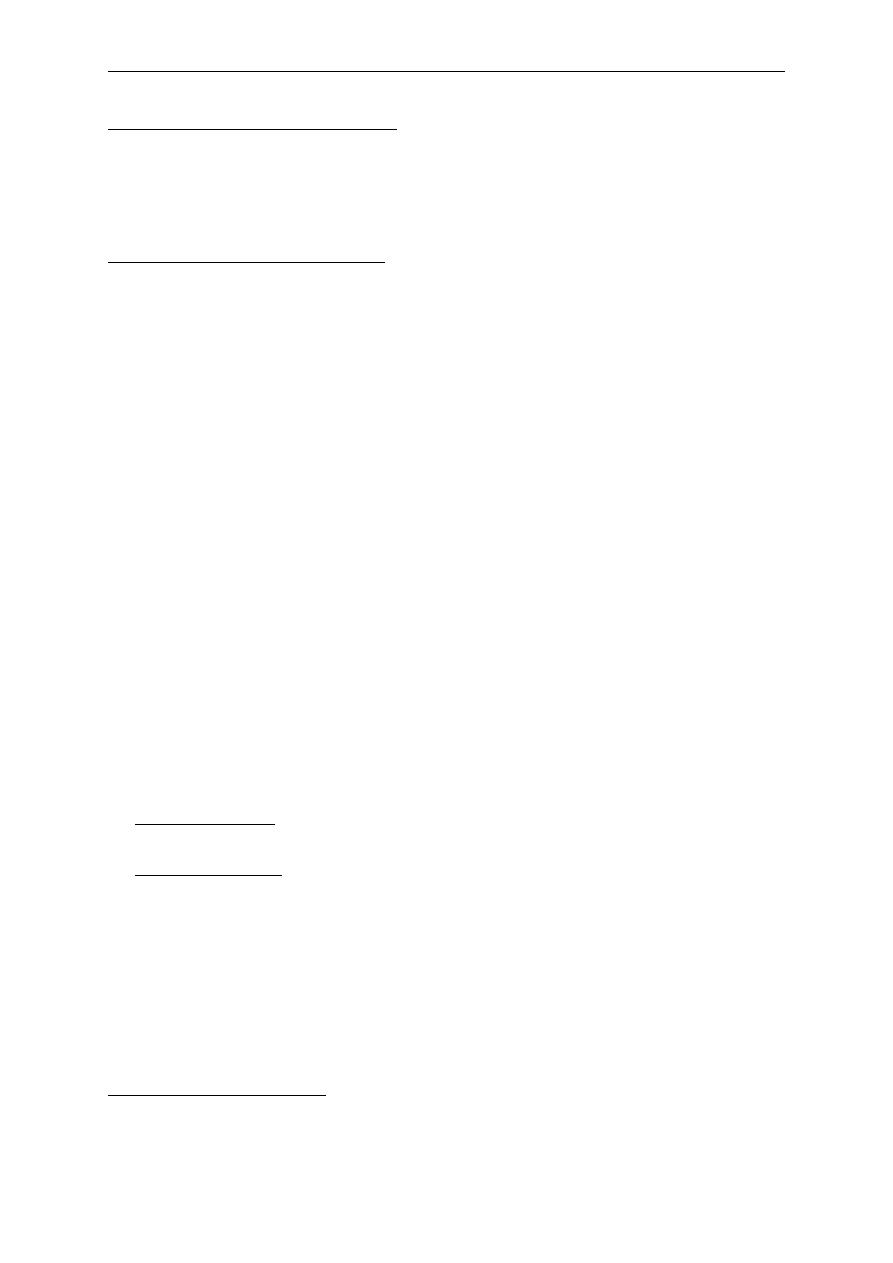
Review of other systems:
o
Appetite, weight loss or gain.
3
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
o
GIT, Urinary symptoms
o
Cardiovascular, respiratory and other systems.
Review of other systems:
History of present pregnancy:
:
weeks)
3
1
–
First trimester (0
*
4
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
1. How pregnancy is diagnosed (conceived spontaneously or on
treatment):
2. ANC (regular or irregular):
3. pain (abdominal or back pain):
4. bleeding (amount and duration):
5. Severe nausea and vomiting (hyper emesis gravidarum), weight
loss, hospital admission:
6. Urinary and bowel symptoms:
7. Any febrile illness or hospitalization:
8. Drugs and radiation exposure:
9. If the patient is hypertensive or diabetic, ask about early ANC
visits & treatment received.
:
28 weeks)
–
4
Second trimester (1
*
1. Quickening: the first fetal movement (as the patient told in
which month of pregnancy)
2. Abdominal pain:
3. Vaginal bleeding or discharge:
4. Urinary and bowel symptoms:
5. Weight gain and edema:
6. ANC (blood pressure and routine investigations):
delivery):
–
weeks
9
2
trimester (
Third
*
1. Fetal movements (normally at least 4 movements in 1 hour or 10 in 12
hours)
2. Abdominal pain:
3. Vaginal bleeding or discharge:
4. Urinary and bowel symptoms:
5. Weight gain and edema:
6. ANC (blood pressure and routine investigations):
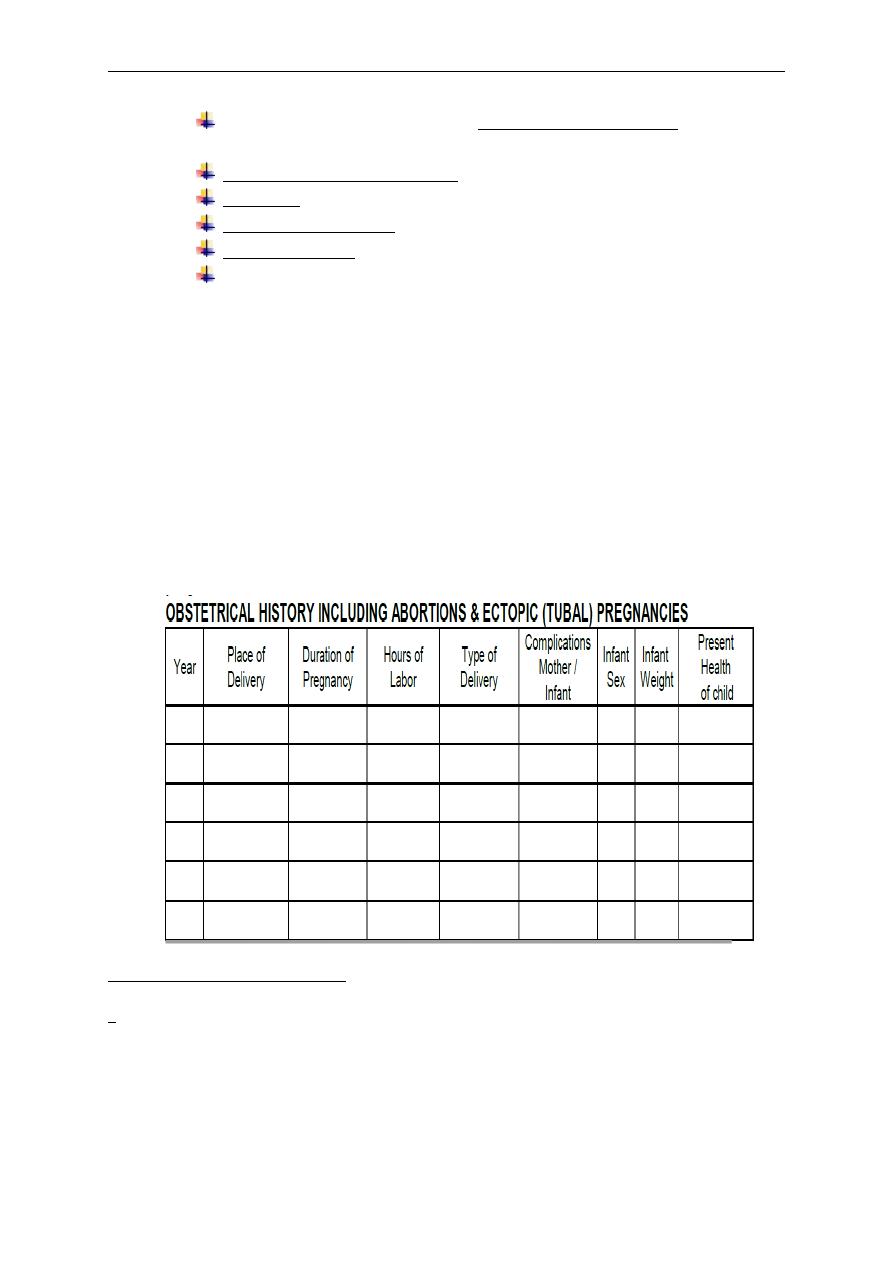
Past Obstetric history:
1. Date of marriage
2. when she conceived (any period of infertility)
3. For each pregnancy ask about:
duration(term, preterm or post term)
5
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
any antenatal complication ( eventful or un eventful such as
APH, medical diseases)
mode and place of delivery
outcome of delivery
puerperal problems
Breast feeding.
Time until the next pregnancy (any contraception or infertility).
4. The features that are likely to have impact on future pregnancies include:
1. recurrent miscarriage (increased risk of
2. miscarriage, fetal growth restriction (FGR));
3. preterm delivery (increased risk of preterm delivery);
4. early-onset pre-eclampsia (increased risk of pre eclampsia/FGR);
5. abruption (increased risk of recurrence)
6. congenital abnormality (recurrence risk depends on type of
abnormality);
7. macrosomic baby (may be related to gestational diabetes);
8. FGR (increased recurrence);
9. unexplained stillbirth (increased risk of gestational diabetes)
history:
gynecological
Past
history:
. Menstrual
1
Age of menarche.
Usual duration of each period?
Length of cycle.
Painful cycles (treatment received)
6
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
Does bleeding or spotting occur between periods or after
intercourse?
2. Previous gynecological surgery or treatment.
The date of last cervical smear.
History of discomfort, pain, or bleeding during intercourse.
3. The use of contraception and type of contraception used.
.
of infertility
4. History
medical history:
t
s
a
P
* Any serious illness or medical diseases, chronic disease e.g.
1. Diabetes mellitus:
.
2. Hypertension: pre-eclampsia
.
3. Renal disease
4. Epilepsy
5. Venous thromboembolic disease
6. Human immunodefi ciency virus (HIV) infection
7. Connective tissue diseases
8. Myasthenia gravis/myotonic dystrophy
history:
surgical
t
s
a
P
*Anesthetic complications (as scoline apnea)
* Previous operations (postoperative complications).
* Blood transfusion.
Drug history:
Allergy to any drug.
Chronic drug use such antihypertensive and antiepileptic drugs.
Family history:
1. Any chronic medical diseases such as hypertension, DM,
,thromboembolic disease(increased risk of
thrombophilia,thrombosis)
2. Consanguineous marriage
3. History of pre-eclampsia (increased risk of pre-eclampsia)
7
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
4. History of psychiatric disorder (increased risk of puerperal
psychosis.
5. History of twin pregnancy, congenital malformations or cerebral
palsy or any potential genetic problems such as
haemoglobinopathies or fetal inborn errors of metabolism
6. History of malignancies in the family.
7. History of tuberculosis ,allergies
Social history
1. Marital status, relative or not.
2. Family problems
3. living environment
4. Occupation
5. Income
6. Level of education
7. Housing conditions
8. Smoking and alcohol use.
9. Drug abuse
8
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
• patient consent √
• privacy √
• cover the patient √
• explain the procedure √
Examination:
General examination:
© General look: level of consciousness, ill, well, body built( obese or thin),
dyspnea.
© Hands and mucous membranes for pallor, yellowish discoloration,
cyanosis and clubbing.
© Lymph nodes
© Oedema (press over the lower medial third of the tibial shin for 30
seconds), other sites the medial side of the ankle and dorsum of the
foot.
© If the patient has cannula examine for site and signs of
thrombophlibitis
9
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
Vital signs:
1. B.P.
:
The
patient lies comfortably with her back semi-prone at
45°.
Diastolic blood pressure is recorded as
Korotkoff V(when the sound
disappears)
2. Pulse rate volume and rhythm (for 30 sec.
if abnormal then count for 1
min.)
3. respiratory rate
4. temperature
An examinayion of the thyroid gland and breast is an important part of a first
assessment
• height (calculate and record the BMI)
• chest, breasts,
• cardiovascular system
Abdominal examination:
Inspection:
-
The contour of the abdomen for any distension as pregnant uter.
-
Assess the shape of the uterus and note any asymmetry
-
Obvious fetal movements
-
Movement with respiration(if absent indicates peritonism)
-
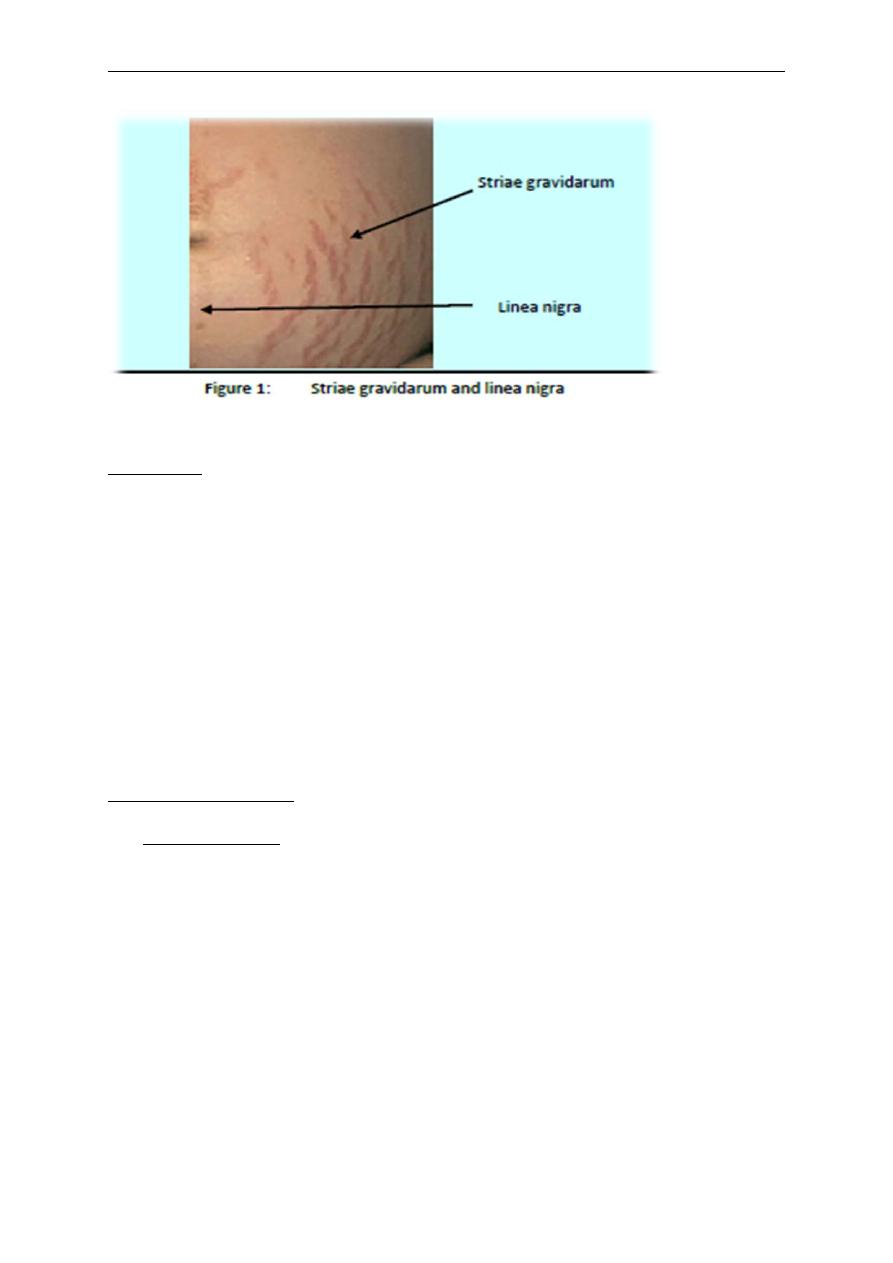
Hair distribution , umbilicus, dilated veins or striae gravidarum and
albicans or linea nigra(the faint brown line running from the umbilicus
to the symphysis pubis)
-
The patient is asked to cough or raise her head for any herniae ,
divarication of the rectus muscles
-
Surgical scars:
(suprapubic {pfannenstiel scar }=caesarean section,Laprotomy
for ectopic pregnancy or ovarian masses),
(sub-umbilical scars =Laparoscopy)
right upper quadrant(cholycystectomy)
-
Any surgical dressings (dry or soaked with blood or discharge)
10
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
Palpation :
1. First, if the patient has any pain, she should be asked to point to the
site, this area should not be examined until the end of palpation.
2. Using the right hand, examine the left lower quadrant and proceed
to the right lower quadrant while looking to the patient face.
3. palpate for masses, liver, spleen and kidneys
4. Signs of peritonism: guarding and rebound tenderness
5. examination for inguinal herniae and lymph nodes
6. if the patient had caesarean section, palpate for the fundal height
(it should be at or just below the umbilicus)
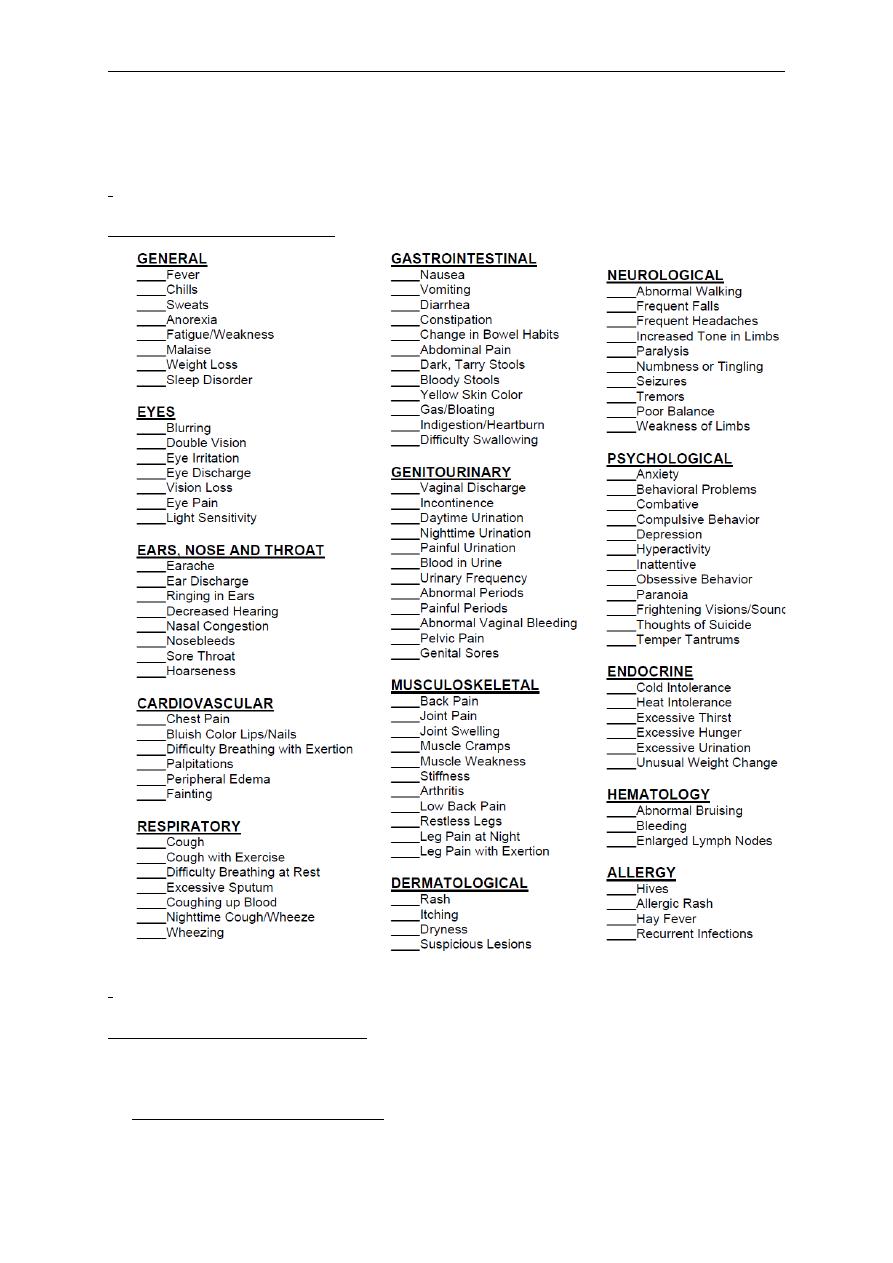
Obstetric maneuvers:
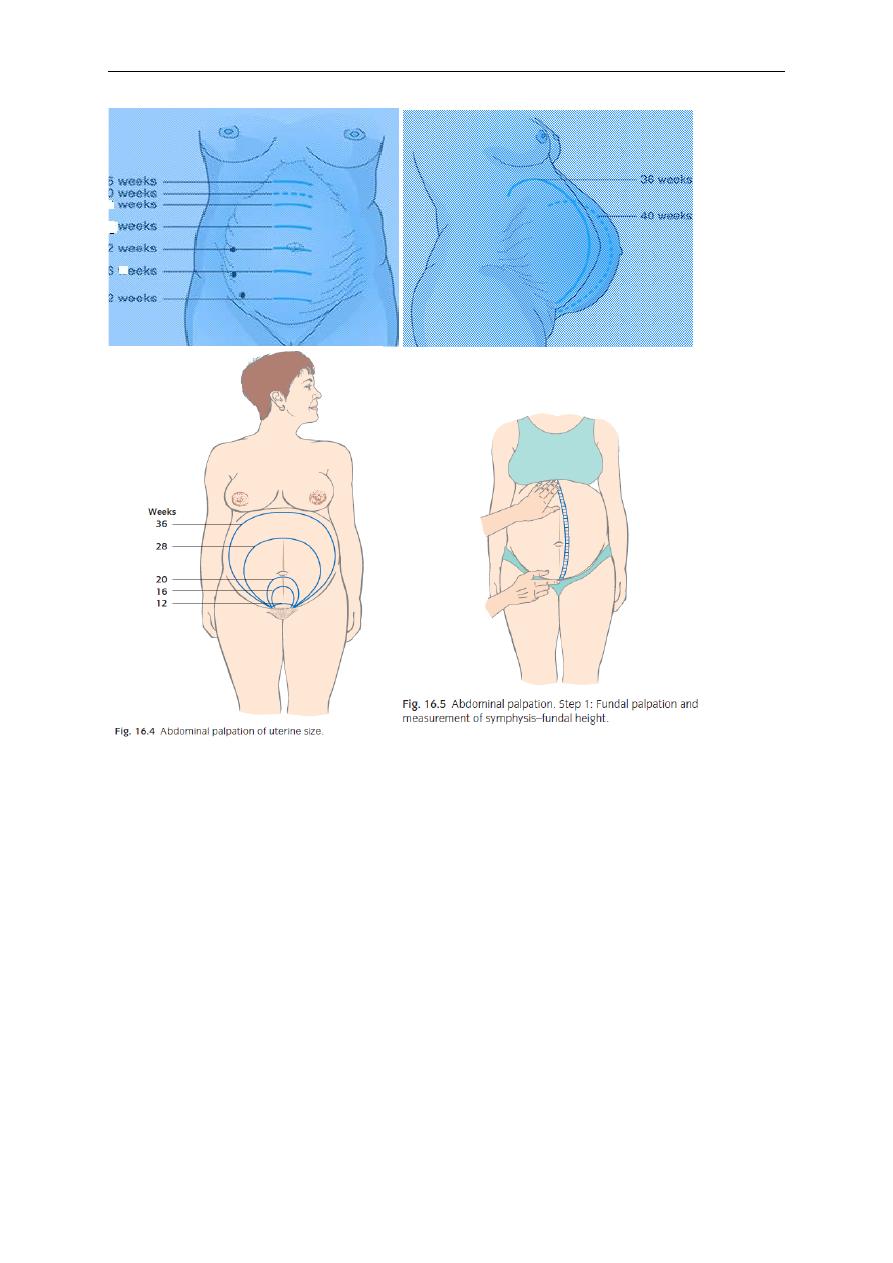
1.Fundal height
by the ulnar border of the left hand, mention fundal ht.
in weeks as in the following figure:
•
At 12 weeks of gestation, the fundus is just above the symphysis pubis
•
At 22 weeks of gestation, the fundus is at umbilicus
•
At 36 weeks, the fundus is at xiphisternum, depending on the level of
pre-senting part whether it descends into the pelvis.
•
At 16 weeks, the fundus is equidistance between the symphysis pubis
and umbilicus.
•
At 30 weeks, the fundus is equidistance between the xiphisternum and
umbilicus.
11
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
Or by symphysis fundal height measurement between (24 weeks-36weeks)
using tape measure (each 1cm equal 1 week±2 cm.
Uterine size
symphysis fundal Ht in cm = GA in wk
This will give you a clue regarding potential problems such as
1. polyhydramnios
2. multiple pregnancy
3. growth restriction
•
Feel carefully for the top of the fundus. This is rarely in the midline.
Make a mental note of where it is. Now feel very carefully and gently
for the upper border of the symphysis pubis. Place the tape measure on
the symphysis pubis and, with the centimeter marks face down,
measure to the previously
12
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
•
Noted top of the fundus. Turn the tape measure over and read the
measurement.
•
Late third trimester the fundal height is usually approximately 2 cm
less than the number of weeks.
A large SFH raises the possibility of:
1. macrosomia;
2. multiple pregnancy;
3. Polyhydramnios.
4. Rarely, a twin is missed on ultrasound!
A small SFH could represent:
1. FGR;
2. Oligohydramnios.
After you have measured the SFH, palpate to count the number of fetal poles
a pole: is a head or a bottom. If you can feel one or two, it is likely to be a
singleton pregnancy. If you can feel three or four, a twin pregnancy is likely.
Sometimes large fibroids can mimic a fetal pole.
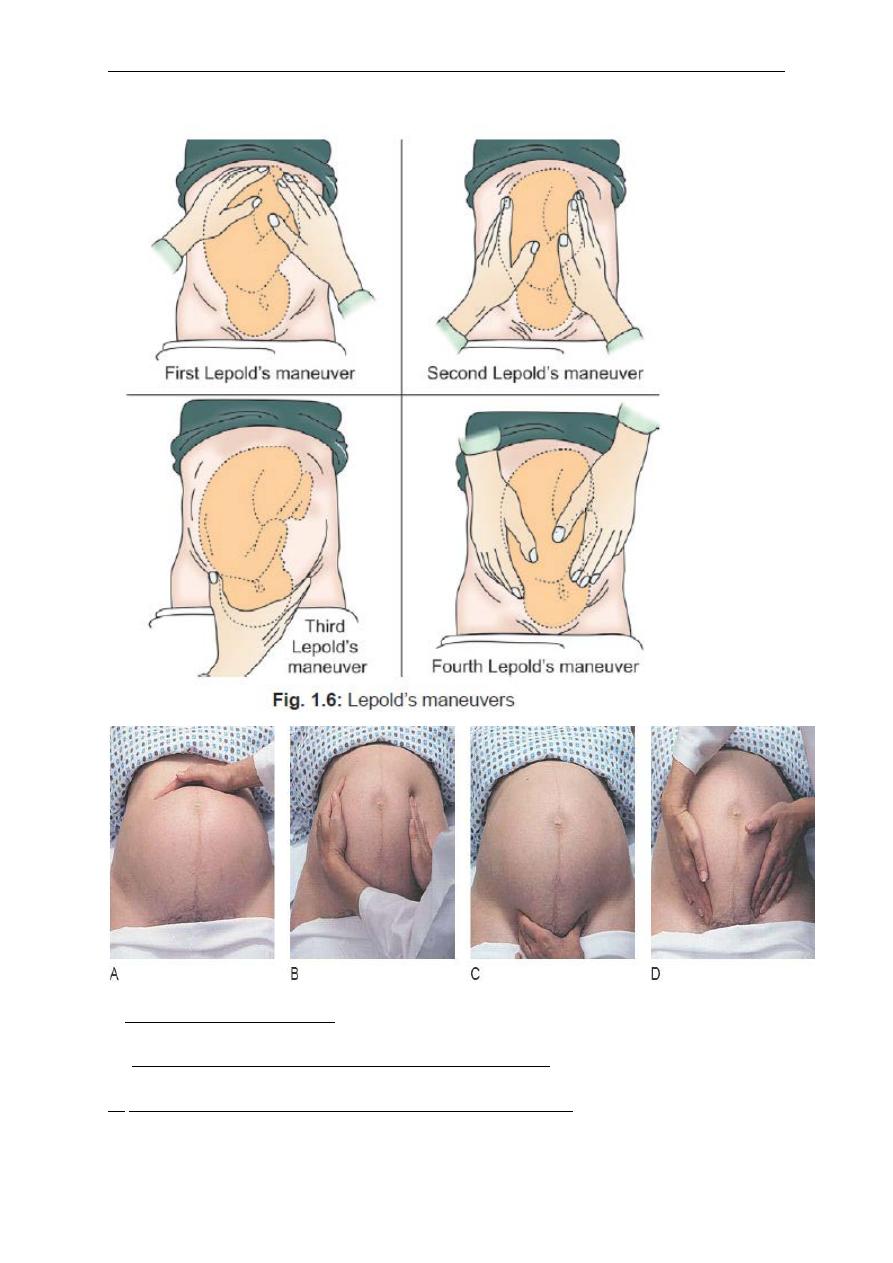
2.Obstetric Grips or Lepold’s Maneuvers of Abdominal Palpation
(Figure 1.6)
Obstetric grips which help in determining fetal lie and presentation are also
known as Lepold’s maneuvers. Lepold’s maneuvers basically include four
steps and must be performed while the woman is lying comfortably on her
back. The examiner faces the patient for the first three maneuvers and faces
towards her feet for the fourth. Obstetric grips must be conducted when the
uterus is relaxed and not when the woman is experiencing contractions.
A -
Fundal grip (Lepold’s first maneuver)
For which of the fetal poles (head or breech) is present at the fundus.
The fundal area is palpated by placing both the hands over the fundal
area.
Palpation of broad, soft, irregular mass is suggestive of fetal legs
and/or buttocks, thereby pointing towards head presentation
Palpation of a smooth, hard, globular, ballotable mass at the fundus is
suggestive of fetal head and points towards breech presentation
13
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
B -
Lateral grip (Lepold’s second maneuver)
For the lie of the fetus and the site of the back.
While facing the patient’s face. The hands are placed flat over the
abdomen on the either side of the umbilicus.
C -
2
nd
pelvic grip
or
Pawlic grip
or
Third Leopold’s maneuver
for
engagement.
This examination is done while facing the patient’s face.
The clinician places the outstretched thumb and index finger of the right
hand keeping the ulnar border of the palm on the upper border of the
patient’s pubic symphysis.
If a hard, globular mass is gripped, it implies vertex presentation.
If A soft, broad part is suggestive of fetal breech
If the presenting part is not engaged, it would be freely ballotable
between the two fingers
In case of transverse presentation the pelvic grip is empty
Normally the size of head in a baby at term would fit in the hand of the
examining clinician
D -1
st
pelvic grip (Fourth Leopold’s maneuver):
With two hands for the presenting part.
First pelvic grip is performed while facing the patient’s feet.
Tips of three fingers of each hand are placed on the either side of
the
midline in downwards and backwards direction in order to deeply
palpate the fetal parts present in the lower pole of the uterus.
The fingers of both the hands should be placed parallel to the inguinal
ligaments and the thumbs should be pointing towards the umbilicus on
both the sides
In case of vertex presentation a hard smooth globular mass suggestive
of fetal head can be palpated on pelvic grip
In case of breech presentation broad soft, irregular mass is palpated.
14
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
3. Uterine contractions (frequency, strength and duration)
4.-estimated fetal size and fetal movements.
5.
Assessment of the Amount of Liquor Present
15
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
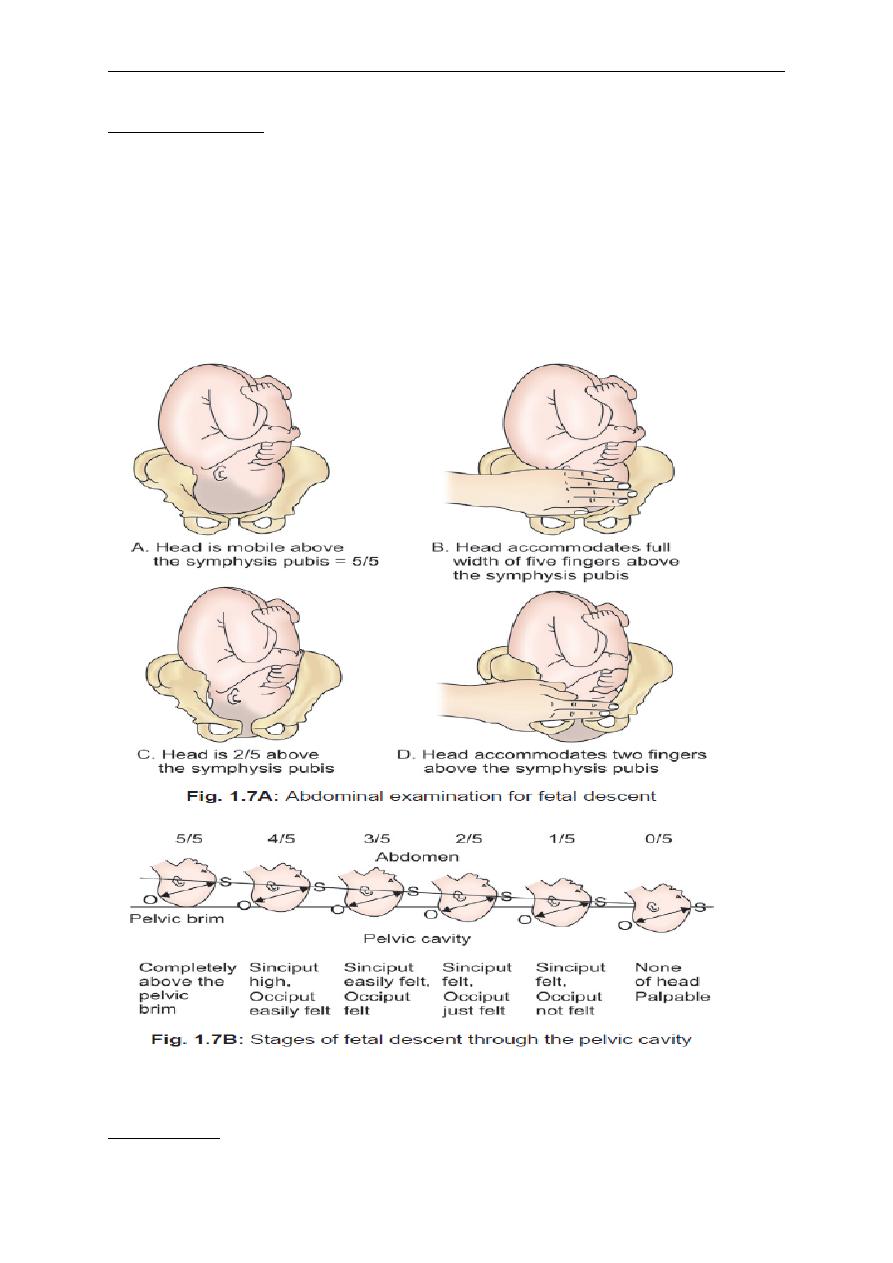
6. Engagement:
Engagement is only applied to cephalic presentation.
If you can feel the whole of the fetal head and it is easily movable, the
head is likely to be ‘free’. This equates to 5/5th palpable and is recorded
as 5/5
As the head descends into the pelvis, less can be felt. When the head is
no longer movable, it has ‘engaged’ and only 1/5th or 2/5th will be
palpable
Percussion:
Shifting dullness and fluid thrill can also be elicited.
16
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
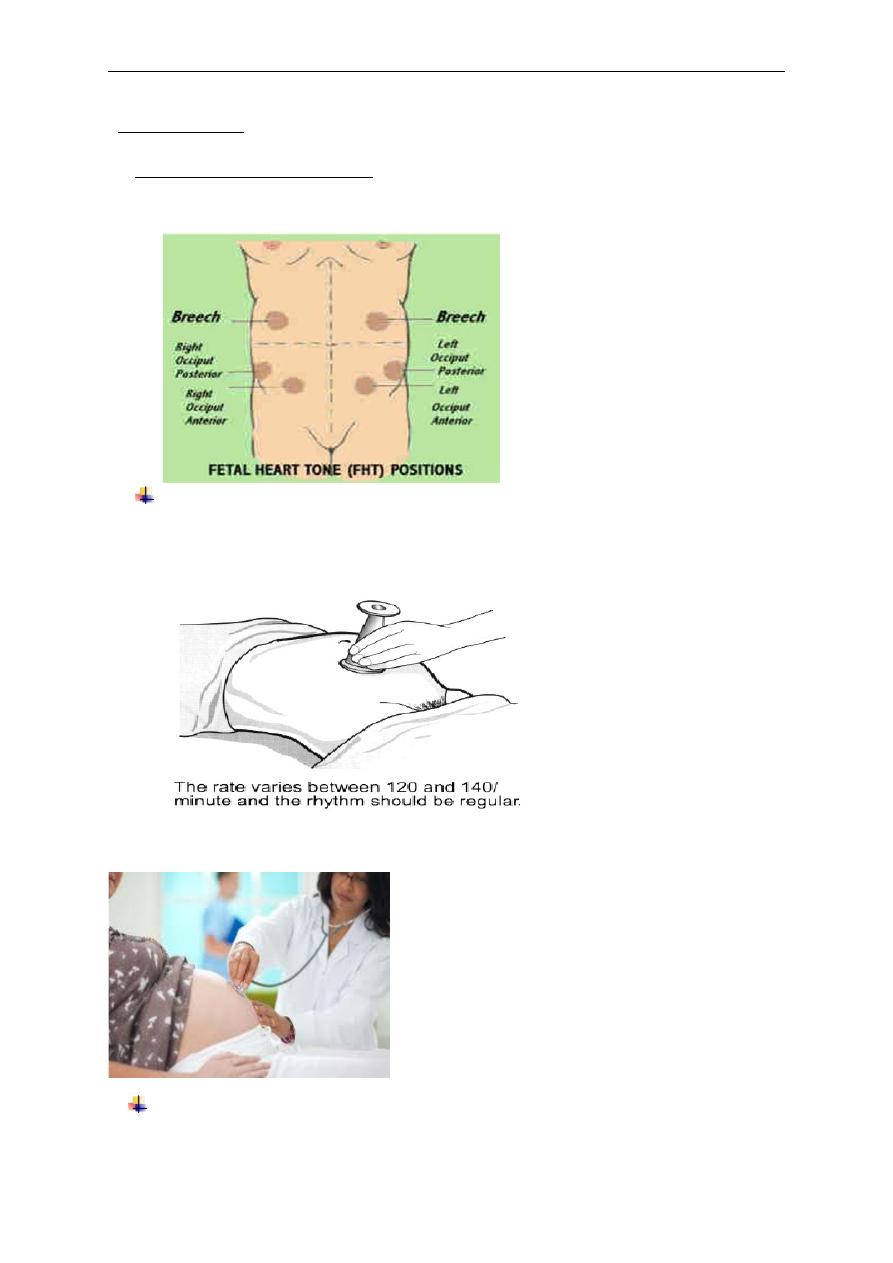
Auscultation:
1.
Fetal heart auscultation
depends on presentation and site of the back.
(
Listening over the anterior shoulder (usually
between the head and the
umbilicus).
The fetal heart
should be heard with a Pinard’s stethoscope. Place this
flat over the shoulder, press it on the abdomen with
your ear, keeping
both hands free and time the heart
rate with your watch. It should be
110–160 beats/
minute.
•
Heard with stethoscope after 24 weeks
With hand-held Doppler device (portable sonicaide) at 12 weeks.
17
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
With twins, you must be confident that both have been heard.
2.
Postoperative patient
listen for bowel sounds at the Mc Burney's
point (ileocecal valve at the junction of lateral third with medial two
thirds of the line joining the umbilicus and ant. Sup. Iliac spine). absent in
ileus
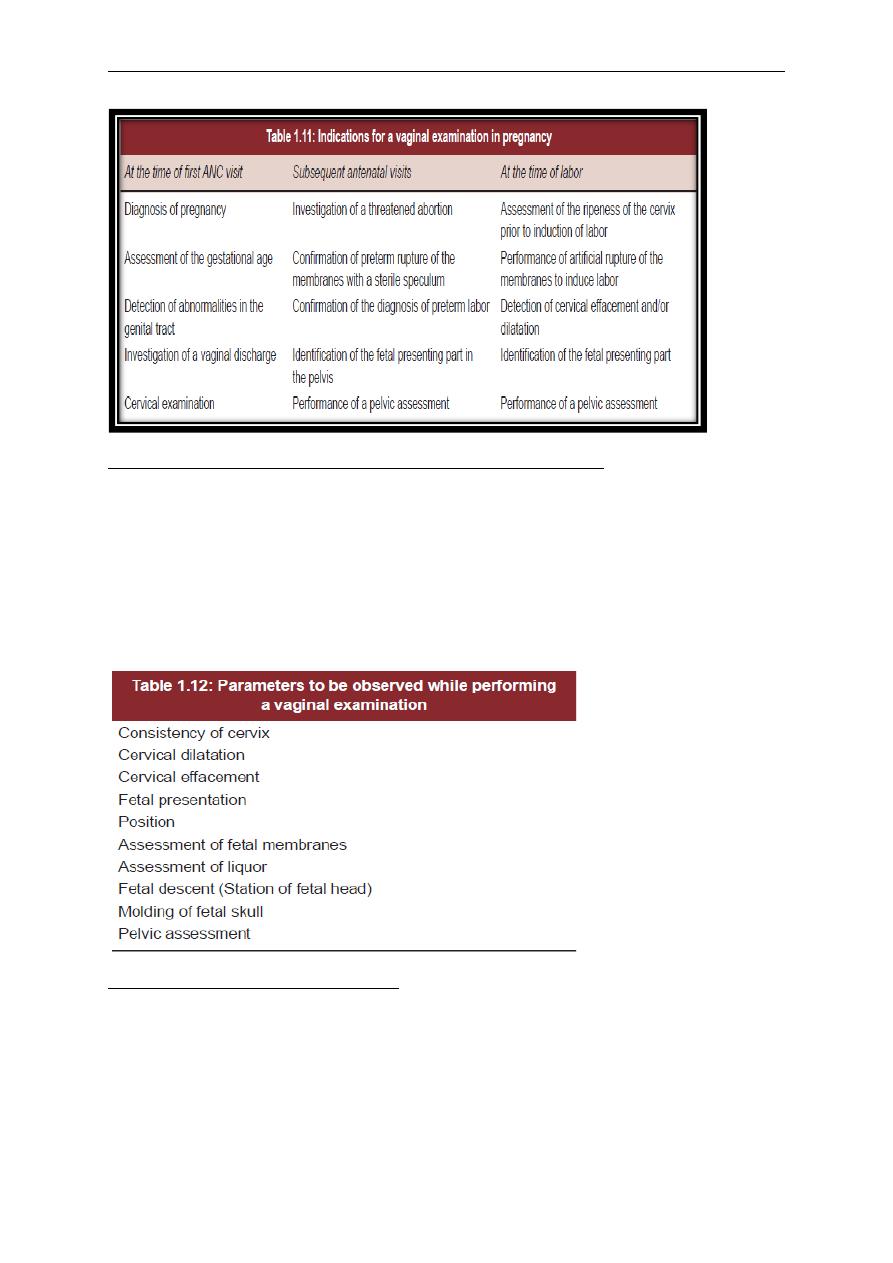
Pelvic examination
Prerequisites for a Vaginal Examination
1. The patient must be carefully explained about the examination,
prior to performing the examination.
2. Adequate permission must be taken from the patient.
3. There should be a valid reason for performing the examination. A
vaginal examination must always be preceded by an abdominal
examination.
18
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
Contraindications to a Vaginal Examination in Pregnancy
1. Antepartum hemorrhage
2. Preterm rupture of the membranes without contractions are
conditions in which the vaginal examination is contraindicated. In
these cases a sterile speculum examination can be done to confirm
or exclude rupture of the membranes.
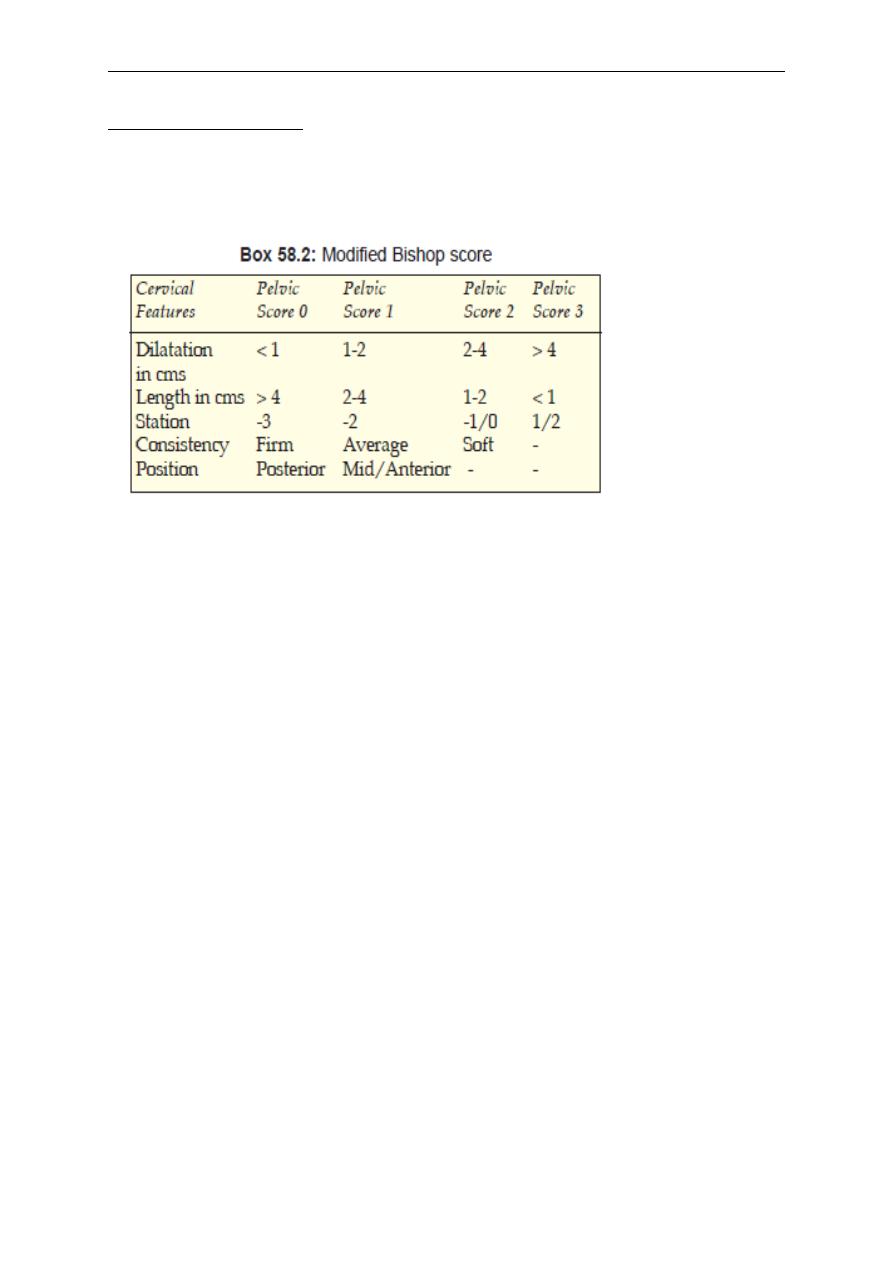
Features of a vertex presentation
The posterior fontanelle is normally felt. It is a small triangular Space. In
contrast, the anterior fontanelle is diamond shaped. If the head is well flexed,
the anterior fontanelle will not be felt. If the anterior fontanelle can be easily
felt, the head is deflexed.
19
د.
زﯾﻧب ﻋﺑد اﻻﻣﯾر
The Obstetric history and examination
2014
-
2015
CLINICAL PELVIMETRY
20
