1
The anesthetic plan
Premedication
Type of anesthesia
General
o Airway management
o Induction
o Maintenance
o Muscle relaxation
o Recovery
Local or regional anesthesia
o Technique
o Agent
Monitored anesthetic care
o Supplemental oxygen
o Sedation
Intraoperative management
Monitoring
Positioning
Fluid management
Post-operative management
Pain control
Intensive care
Postoperative ventilation
Hemodynamic monitoring
The goals of anesthesia:
Anesthesia
Akinesia
Muscle relaxation
Autonomic control
There are 3 main types of anesthesia:
General anesthesia
Regional anesthesia
Local anesthesia
2
Preoperative preparation & assessment
Is a vital part of the anesthetic care given to patients scheduled for both routine &
emergency surgery.
Preoperative visits:
The purposes of preoperative visit are to:
Establish rapport with the patient.
Obtain a history & perform a physical examination.
Order special investigations.
Assess the risks of anesthesia & surgery & if necessary postpone or cancel the date of
surgery.
A physical status classification is assigned.
Institute preoperative management.
Prescribe premedication & plan the anesthetic management.
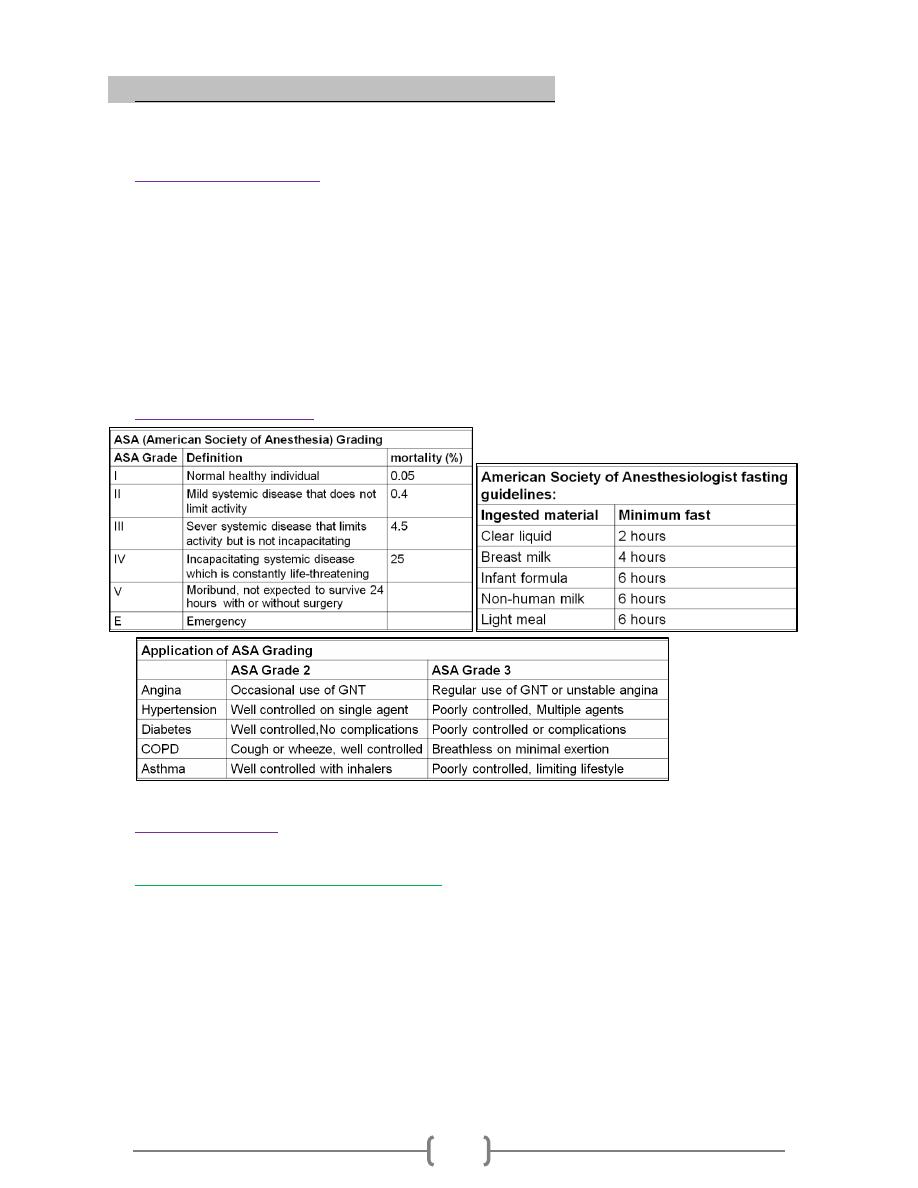
Risk assessment :
Premedication
Involves the prescription of drugs before the induction of anesthesia.
Goals for preoperative medication
Relief of anxiety & fear. Sedation, Amnesia, Analgesia.
Drying of airway secretion.
Prevention of autonomic reflex responses & bronchospasm.
Prevent or minimize the impact of aspiration (Reduction of gastric fluid volume &
increase PH). Antiemetic effects.
Reduction of anesthetic requirements. Prophylaxis against allergic reaction.
Secondary goals for pharmacologic premedication
- Facilitation of induction of anesthesia. - Postoperative analgesia.
- Prevention of pon & v (IV antiemetic).
3
Types of anesthesia
General anesthesia
• General anesthesia uses drugs given systemically to render the patient unaware of any
think that is being done to or around him or her.
Determinants of drugs choice & dose
- Patient age & weight - Physical status
- Previous adverse experience with drugs used for preoperative medication.
- Level of anxiety
- Tolerance for depressant drugs
- Allergy - Elective & emergency surgery
- Inpatient & outpatient surgery
Modern anesthetics
- Inhalational anesthetics - Intravenouse anesthetics
Mostly used in conjunction with each other, seldom alone. TIVA alone iv
Also administered in combination with other drug classes. (neurolapetic an, analgesia)
opiod, droperidol
Inhalation Anesthetic
Original agents were vapours from volatile liquids or gases.
Indication of inhalational induction:
o Young children
o Upper airway obstruction eg. Epiglottis
o Lower airway obstruction with foreign body
o Bronchopleural fistula or empyema
o No accessible vein.
Nitrous oxide (N2O) (laughing gas)
Commonly used but least potent. MAC for true anesthesia =105%
Halothane
MAC- 0.3%. Volatile liquid, widely used, good control, smooth induction & recovery
Enflurane
Less chance of dysrhythmia than with halothane. More hypotesion & respiratory
depression on induction but recovers with the start of surgery.
Isoflurane
Less CV or respiratory depression than enflurane but more so than halothane.
Intravenous anesthetic
Mainly selected members of sedative drugs classes, Act by:
Potentiating the action of an inhibitory ionophores (GABA receptors).
Blocking the action of excitatory ionophores (Nicotinic Ach & NMDA receptor).
Barbiturates
Ultra short acting. Methohexital , Thiopentone , pentobarbital
Very lipid soluble, induce anesthesia (hypnosis) in 1 time circulation
4
Alkylphenols
Propofol (milk of amnesia). Patient recover more rapidly & fell less hungover
Contraindicated for sedation in children due to acidosis & possible neurological sequelae
Imidazoles
Etomidate- used mainly for induction & short duration procedure. Minimal cardio-
vascular or respiratory effect. Rapid onset (seconds) but not analgesia-reflexes present
Benzodiazepines
Midazolam- water soluble but slower in onset than barbiturates. Mainly used
preoperatively. Prolonged recovery with amnesia
Flumanezil- receptor antagonist; used to speed recovery, or act as antidote in overdose
Cyclohexylamine
Ketamine-channel blocking agent related phencyclidine. Blocks both nicotinic Ach &
NMDA (glutamic acid) receptor channels
Indicated mainly in outpatient procedures ,children & burn dressings
Muscle relaxants
Depolarising MR: Succinylcholine, (suxamethonium) (scoline). Rapid onset, act
within seconds & last for approximately 5 minutes. Short- acting
Non-depolarizing MR: Competitive antagonism of acetylcholine receptor. Have
duration of action ranging from 15 min - > 2hrs
Local & regional anesthesia
Act by reducing membrane permeability to sodium. - Act on small unmyelinated C fiber
before large A fibers. - Reduce pain & temperature sensation before touch & power
What drugs are used?
Bupivacaine (Marcaine) is a common longer – actiner anesthetic, widely used for
epidurals,spinal&other blocks. Effective. Medium duration.
Lidocaine (Xylocaine, lignocaine) the most common of the short acting local
anesthetics (duration of action of about 1 hr) & is used in many procedures. With addition
of adrenaline duration of action can be increased to 2 hrs.
Mepivacaine is similar to lidocaine
Ropivacaine is a new longer acting agent which appears to be safer than Bupivacaine
Tetracaine is used mainly for spinal
Cocaine is still used as a local anesthetic in special cases
Other drugs may be added to the local anesthetic
Adjuncts: Opoid, Epinephrine, Clonidine, others
Regional anesthesia
With a regional anesthesia, a small amount of an anesthetic drug is injected near to the
nerves that supply a part of the body.
Why choose a local or regional anesthesia
Avoids some of the risks & unpleasantness, such as nausea & vomiting, which
sometimes occurs with GA.
5
Providing pain relief for several hours after the operation.
Reduce blood loss.
Some patients feel more (in control) when they are awake during surgery.
Blocks for various parts of the body
Local infiltration for cuts & small procedures.
Blocks for eye surgery.
Blocks for hand& arm surgery: local infiltration, blocks of individual fingers, IV
regional blocks, axillary blocks.
Spinal & epidural anesthesia.
Caudal anesthesia.
Pain relief in labour.
Spinal & epidural anesthesia
Spinal anesthesia – local anesthetic or opiad injected into CSF below termination of
cord at L1 (adult). Used for operations below the waist or in the pelvic region. The
patient completely numb from the waist down for a couple of hours.
Epidural anesthesia - local anesthetic or opiad injected into fatty epidural space.
An epidural uses a similar technique to spinal anesthesia, with a (catheter) narrow
plastic cannula left in position near to the nerves in the back. This means that the
anesthetist can give repeated doses of local anesthetics & (painkillers) without further
injection. This makes it useful for longer operations. An epidural can be used for
postoperative pain relief & for labour pain.
Both can produce good anesthesia for up to 2hours. The quality of block is often better
with a spinal. Epidural anesthesia is technically more demanding.
Contraindications to central blockade
Absolute: - Sepsis - Bacteremia - Skin infection at injection site - Sever hypovolaemia -
Coagulopathy - Therapeutic anticoagulation - Increase intracranial pressure - Lack of consent
IV Regional anesthesia
Also known as a Bier block
Used on surgery of the upper & lower extremities
Patient must an IV cannula inserted in the operative extremity. After a pneumatic
tourniquet is applied to extremity , Lidocaine is injected through IV. Anesthesia lasts
until the tourniquet is deflated at the end of the case.
Important- to prevent an overdose of lidocaine it is impotant not to deflate the
tourniquet quickly at the end of the procedure
The anesthetist will deflate/ inflate tourniquet several times before complete deflation
of tourniquet cuff

6
Complication during anesthesia
Bradycardia
Tachycardia
Atrial arrhythmia
Ventricular arrhythmia
Heart block
Hypotension
Hypertension
Myocardial ischemia
Cardiac arrest
Embolism
Hypoxemia
Hypercapnia
Hypocapnia
Respiratory obstruction
Intubation problems
Aspiration of gastric content
Adverse drug effects
Malignant hyperthermia
Porpheria
Hypothermia
Hyperthermia
injury
7
Delayed recovery
The duration of impaired consciousness depend on:
1) The drug used
- Volatile with high blood/ gas solubility coefficient
- Barbiturates: large doses
- Benzodiazepines
- Opioid with long duration
2) The timing of drug use: if given toward the end of the procedure
3) Pain: long duration drug
If not: - Hypoglycemia (diabetic patient) - Hyperglycemia
- Cerebral pathology - Hypoxemia – Hypercapnia – Hypotension – Hypothermia - Hypo-
osmolar or TURP syndrome – Hypothyrodism - Hepatic & renal failure
Cyanosis
Postoperative hypoxemia is common & may be caused by many factors. Detected using a
pulse oximeter
Oxygen therapy device
Nasal cannula:
2 L /min =28%, simple, easy to use & well tolerated. May dry nasal
membrane.
Simple facemask:
35-50%, simple and easy to use. If flow < 5L/min accumulate CO2
Venturi mask:
24, 28, 31, & 60%. Simple, reliable, effective.
Non-rebreathing mask:
60-90%, tight fitting & flow rate should adjusted to prevent
collapse of reservoir bag during inspiration.
Postoperative pain management
Relief of surgical pain with minimal side effect is a primary goal in PACU care
Methods of providing postoperative pain relief
Drug treatment:
Opioid
Non-steriodal ant-inflammatory drugs
Paracetamol & combinations
Regional anesthetic techniques:
Central neuraxial blocks (spinal & epidural)
Peripheral nerve blocks
Local infiltration .
Psycological methods
Relaxation
Hypnosis
Psychoprophylaxis.
8
Fluid Management
All patients except those undergoing the most minor surgical procedures require venous
access & IV fluid therapy. Some require transfusion of blood or blood component
Physiology
Approximately two–third of total body (TBW) is intra-cellular (ICF) & one third is
extracellular fluid (ECF). The ECF is further subdivided into interstial fluid & plasma.
To replace a given blood loss requires 3 times the volume as saline (0.9%) or 9 times the
volume as dextrose (5%).
Intravenous fluids
IV fluid therapy may consist of infusion crystalloid, colloid or a combination of both.
Intravascular half – life of a crystalloid solution is 20 – 30 minutes, while most colloid
solutions have intravascular half – lives between 3 – 6 hours.
Crystalloid solutions
Are aqueous solutions of low- molecular weight ions (salts) with or without glucose.
They rapidly equilibrate with & distributed throughout the entire ESF
Commonly used crystalloid solutions
o Sodium chloride 0.9%
o Glucose 5%
o Glucose 4% + saline 0.18%
o Glucose 5% + saline 0.45%
o Lactate ringers (Hartmann solution)
o Sodium bicarbonate 8.4%
Colloid solutions
Also contain high molecular weight substances such as proteins or large glucose
polymers. Colloid solutions maintain plasma colloid oncotic pressure & for the most
part remain intravascular.
Generally accepted indication for colloids include:
o Fluid resuscitation in patient with severe intravascular fluid deficit (eg.
Hemorrhagic shock) prior to the arrival of blood for transfusion.
o Fluid resuscitation in the presence of severe hypoalbominemia or conditions
associated with large protein losses such as burn.
Several colloids solutions are generally available:
o Blood derived colloid include: - Albumin 5% - Plasma protein fraction 5%
o Synthetic colloids include: - Detrose starches - Gelatins - Hetastarch
(Hydroxyethyl starch)
Normal requirement:
Water:
Maintenance requirement are approximately 1.5 ml / kg /hr
Sodium (Na+)
Average requirements are 1 mmol/kg. This could be provided by:
- 2500 ml of 4% dextrose with 0.18 saline over 24 hrs.
9
- 2000ml of 5%dextrose& 500ml of 0.9% saline over 24h
Potassium (K+):
Average requirements are 1 mmol / kg.
Abnormal losses
o These are common in surgical patient. They may be sensible or insensible & either overt
or covert
o Losses from the gut
o Replacement with saline 0.9% with 13-20mmol/L of K+ as KCL.
o The usual insensible losses from skin & lung increase by 12% for each 1 C rise in body
temperature.
o Sequestration of fluid at the site of operative trauma (third space) losswhich are not
measured easily.
Existing deficits
These occur preoperatively & arise primarily from the gut. Dehydration with
accompanying salt loss is a common disorder in the acute surgical patient .
Assessment of dehydration:
History & examination
The severity of dehydration may be described clinically as:
o Mild dehydration
loss of 4% of body weight (approximately 3L in 70kg patient)
Reduced skin turgor
Sunken eye
Dry mucous membrane
o Moderate dehydration
Loss of 5-8% body weight (approximately 4-6L in 70kg patient)
Oliguria
Orthostatic hypotension
Tachycardia
Addition to the above
o Severe dehydration
Loss of 8 – 10 % body weight (7 L in 70 kg patient)
Profound oliguria
Compromised cardiovascular function
Laboratory assessment
The degree of haemoconcentration & increase in albumin concentration
Perioperative fluid requirements:
Fluid therapy can be divided into: * Maintenance * Deficit * Replacement
requirement: which is further subdivided into: - Blood loss - Third space loss
Maintenance fluid requirements
In adult & pediatric patients can be determined by the following formula: (4 : 2 : 1)
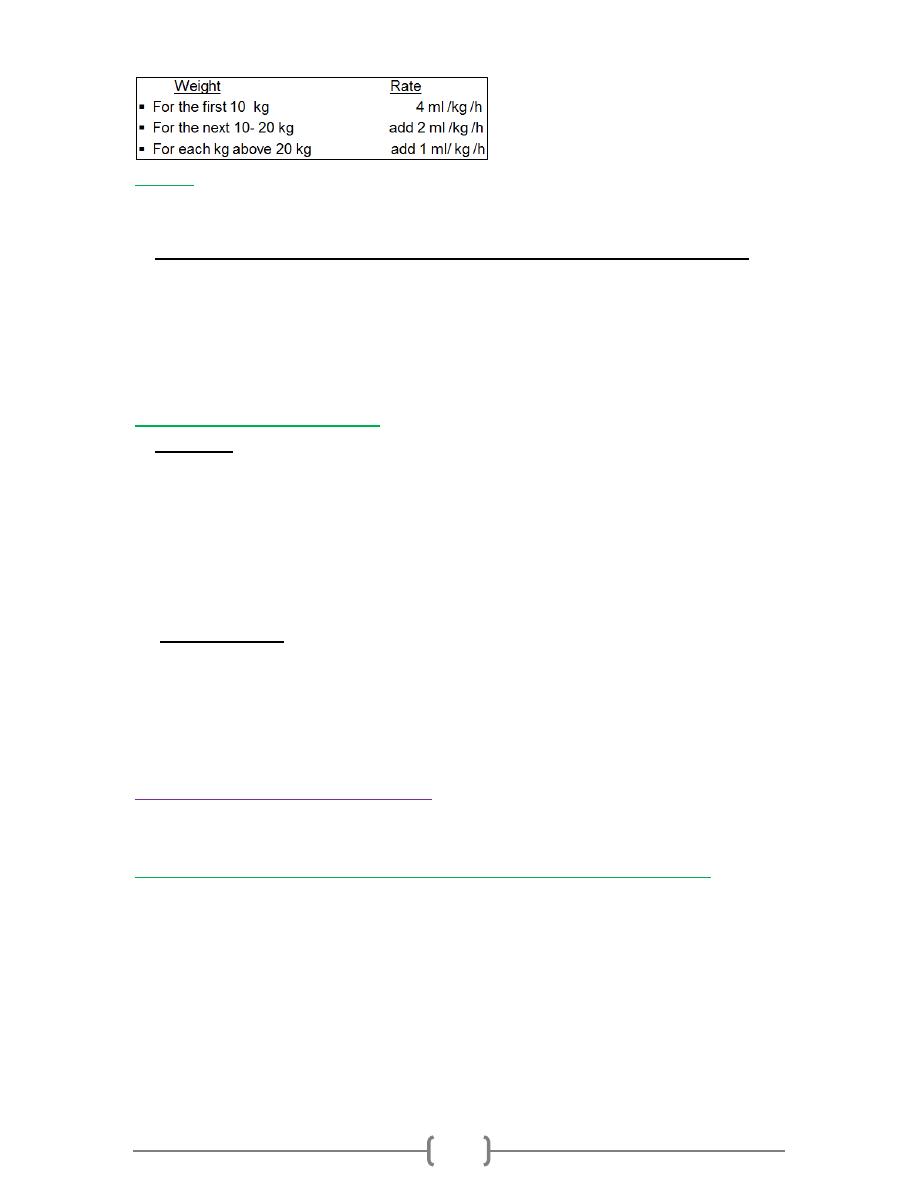
10
Deficit
In addition to a maintenance infusion, any preoperative fluid deficits must be replaced
Deficit = maintenance x hours of fasting
Preoperative fluid deficit are typically administered with hourly maintenance
o requirement in aliquots of: - 50 % in the 1
st
hr - 25 % in the 2
nd
hr - 25 % in
the 3
rd
hr.
o In the example above, a total of 60 ml would be given in the 1
st
hr (80/2 + 20), 40
ml would be given in the 2
nd
& 3
rd
hr (80/4 + 20 )
o Preoperative fluid deficit are usually replaced with a balanced salt solution eg.
Lactate ringer injection.
Replacement requirements:
are subdivided into:
Blood loss
o The blood volume of: - Premature 100 ml /kg - Full term neonate 85-90 ml /kg
- Infant 80 ml /kg - Adult 65- 70 ml/kg
o Blood loss is typically replaced with non – glucose containing crystalloid eg. 3 ml
of lactated ringer injection for each ml of blood loss Or colloid solutions eg. 1 ml
of 5% albumin per ml of blood lost.
o Blood loss in excess of 15% of blood volume in adult are usually replaced by
infusion of stored blood
Third space loss
o Is impossible to measure & must be estimated by the extent of surgical procedure.
o One popular guideline is:
o 2 ml/kg/ h for relatively a traumatic surgery eg. Strabismus correction
o 6-10 ml/ kg/h for traumatic procedure eg. abdominal abscess
o 3
rd
space loss is usually replaced with lactate ringer injection
Postoperative requirements
In the postoperative period, normal maintenance fluid should be given (= 1.5 ml/kg/h) as
4% dextrose with 0.18 saline.
Additional fluid may be required in the following circumstances:
If blood or serum is lost from drains
If GIT losses continue ex. From NG tube or fistula
After major surgery eg. Total gastrectomy, when additional water & electrolytes may
be required for 24 – 48 h to replace continuing third space losses
During rewarming if the patient has became hypothermic during surgery
Normally K+ is not administered in the first 24 – 48 h after surgery as endogenous
release of K+ from tissue trauma & catabolism warrants restriction

11
The Intensive Care Unit (ICU)
is the hospital facility within which the highest levels of continuous patient care &
treatment are provided.
Indication of ICU admission
Patient requiring or likely to requiring advanced respiratory support.
Patient requiring support of two or more organ systems
Patient with co-morbidity who require support for an acute reversible failure of another
organ system.
Indications for mechanical ventilation
The main indication for mechanical ventilation is Respiratory failure.
Other clinical indications include:
A prolonged postoperative recovery.
Altered conscious level ,
Inability to protect the air way.
Exhaustion when the patient is likely to proceed to respiratory failure.
Control of intracranial pressure in head injury.
Airway protection following drug overdose.
Following cardiac arrest.
For recovery after prolonged major surgery or trauma.
Types of mechanical ventilation
The most commonly used type of artificial ventilation is
intermittent positive
pressure ventilation (IPPV).
The lungs are intermittently inflated by +ve pressure
generated by a ventilator. & gas flow is delivered through an endotracheal or
tracheostomy or mask.
Tracheal intubation
2 main types of ventilators commonly in use in ICU
Volume- cycled ventilation:
Occurs when the ventilator delivers a preset tidal volume
regardless of the pressure generated
Pressure – preset ventilation
The ventilator delivers a preset target pressure to the airway during inspiration.
Modes of ventilation
Controlled Mechanical Ventilation (CMV)
This mode of ventilation isn’t often used in ICU as it doesn’t allow any synchronization
with patients own breathing. As a consequence CMV is not well tolerated
Assisted Mechanical ventilation (AMV)
The patients inspiratory effort is detected & triggers the ventilator to boost the
inspiratory breath
12
These modes have two important advantages:
1) They are better tolerated by the patient
2) They allow the patient to perform muscular work throughout the breath, thereby
reducing the likelihood of developing respiratory muscular atrophy
There are several variations of assisted ventilation
o Intermittent Mandatory ventilation (IMV): is a combination of spontaneous &
mandatory ventilation.
o Synchronised Intermittent Mandatory ventilation (SIMV) With SIMV , the
mandatory breaths are synochronised with the patients own inspiratoy effort
o Pressure- support ventilation (PSV) or assisted spontaneous breaths (ASB): A
preset pressure – assisted breath is triggered by the patient own inspiratory effort.
This is one of the most comfortable forms of ventilation
o Positive End Expiratory pressure (PEEP): Is used with all forms of IPPV.
o Continuous Positive Airway Pressure (CPAP): Is effectively the same as PEEP,
but in spontaneously breathing patients.
Criteria for starting mechanical ventilation
o Respiratory rate >35 or < 5 breaths/min.
o Exhaustion, with laboured pattern of breathing ,
o Hypoxia, central cyanosis, SaO2<90% on oxygen or PaO2<8 kpa.
o Hypercarbia – PaCO2> 8 kpa.
o Decreasing conscious level.
o Significant chest trauma.
o Tidal volume < 5ml/kg or vital capacity < 15 ml/kg
Initiation Mechanical ventilation
Optimizing oxygenation
Strategies to improve oxygenation (other than to increase FiO2) include:
Increasing the mean airway pressure by either raising the PEEP to 10 cmH2O
Or, by increasing the peak inspiratory pressure.
Avoiding very high inflating pressure (above 35cmH2O)
In sever hypoxia, it may be possible to improve oxygenation by increasing the PEEP
further to 15 cmH2O (or above)
Prolong the inspiratory time.
In sevsre ARDS the patient can be repositioned & ventilated in prone position.
Weaning from mechanical ventilation
Weaning is the process by which the patients’ dependence on mechanical ventilation is
gradually reduced to the point where spontaneous breathing sufficient to meet metabolic
needs may be sustained.
Criteria for weaning
Clear consciousness with adequate gag &cough reflex
13
Cardiovascular stability.
Stable metabolic state
Adequate pulmonary function.
Tidal volume > 5 ml/kg .
Vital capacity > 10 ml/kg.
SaO2 > 90% on oxygen 40% or PaO2 > 10 kpa
PaO2 < 6 kpa
