Mukbil Hourani M.D.
AUBMC
Diagnostic Radiology
Introduction to CXR
and
Chest CT
Objectives
• Technique
• Learn the difference
between PA vs. AP CXR
• Learn the utility of a
lateral decubitus CXR
• Anatomy
• Learn the basic anatomy of
the fissures of the lungs,
heart borders, bronchi, and
vasculature that can be
seen on a chest x-ray and
CT
• Interpretation
• Develop a consistent
technique
• Learn the silhouette sign
Pathology
• Learn the concept of
atelectasis and the ability
to recognize it on a chest
x-ray
• Appreciate the appearance
of pulmonary edema
• Appreciate the difference
findings of atelectasis and
pneumonia
• Recognize pleural effusions
and pneumothorax
• Recognize the signs of
COPD
• Pulmonary nodules & masses
• Others….
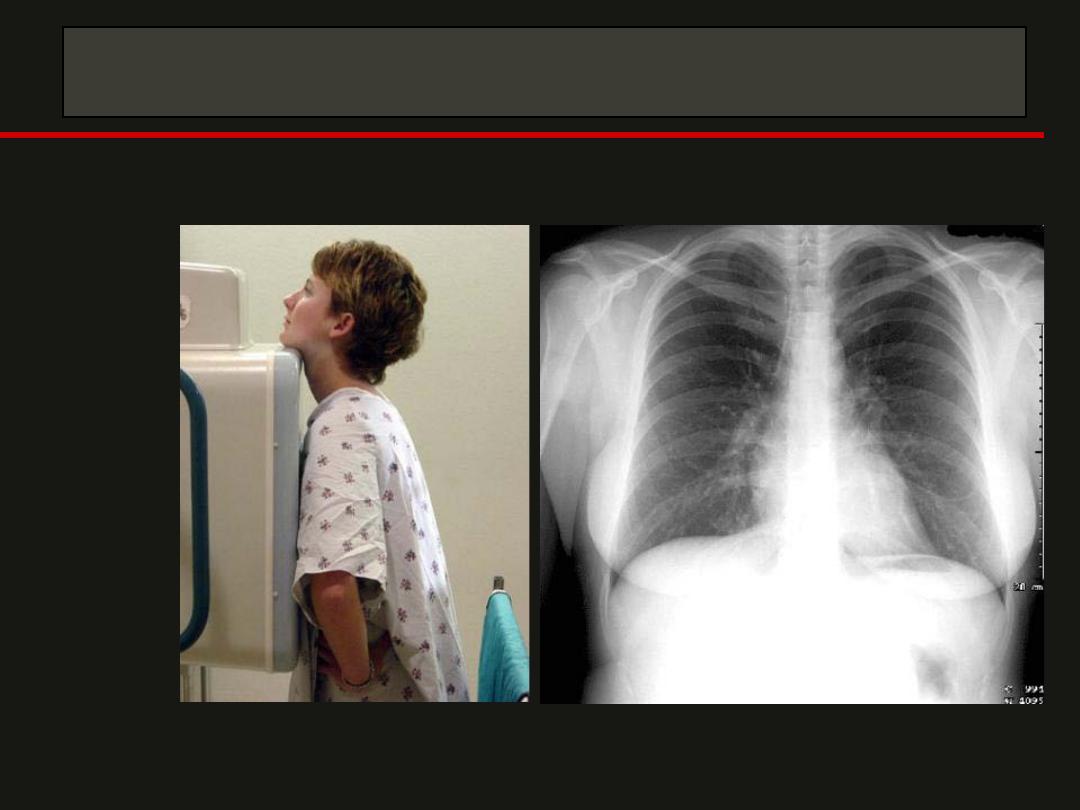
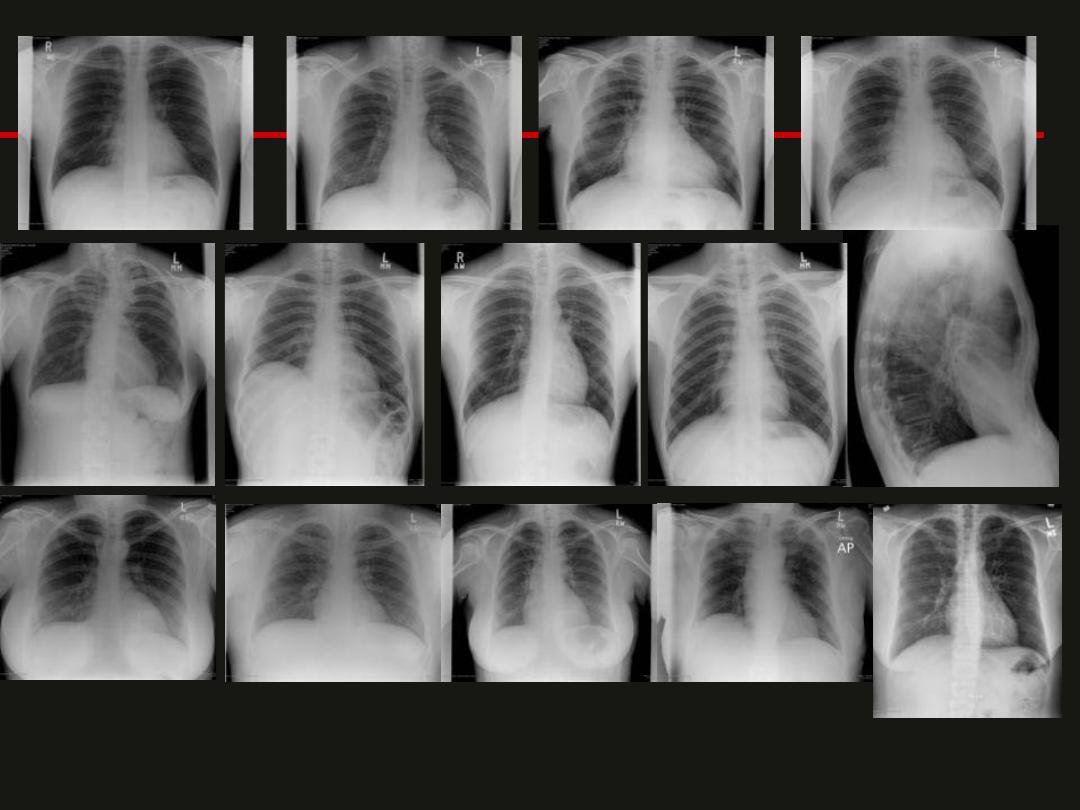
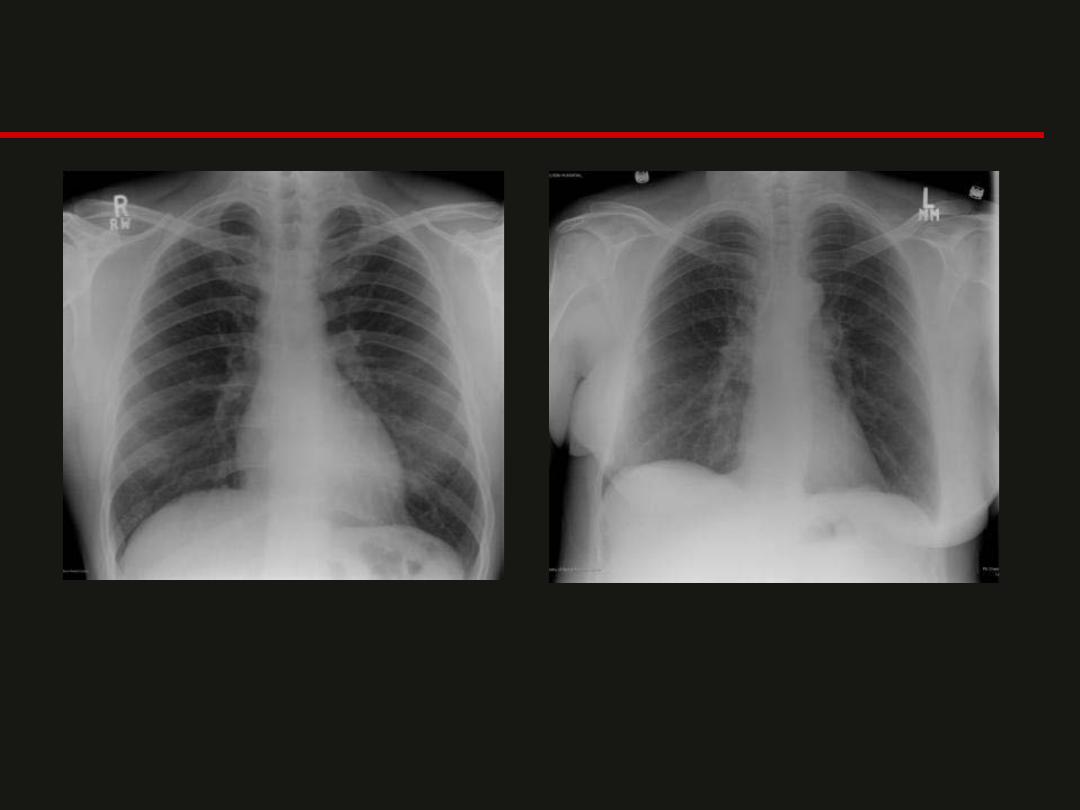
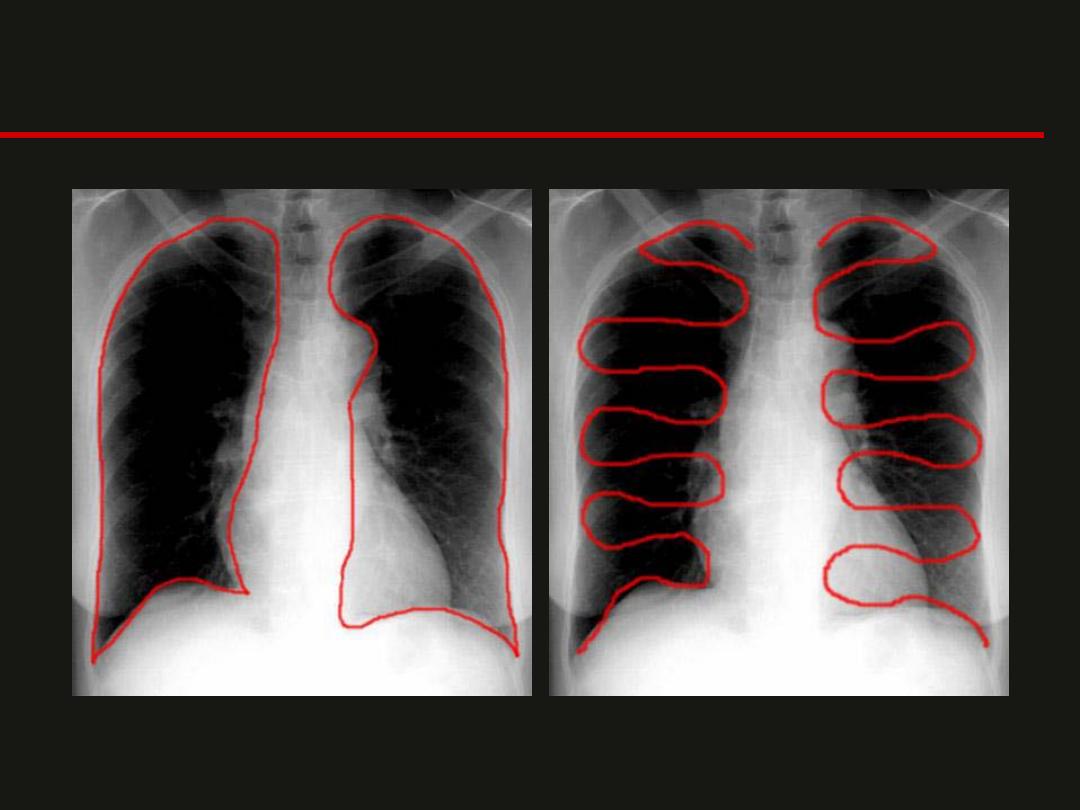
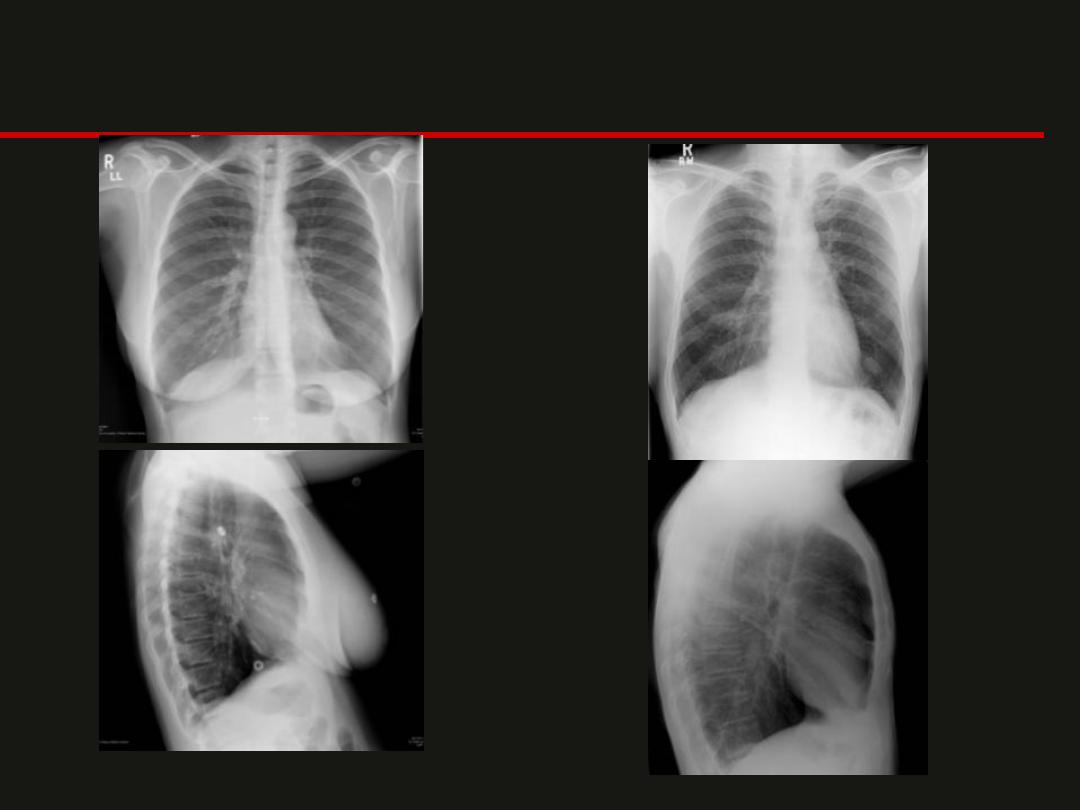
PA View
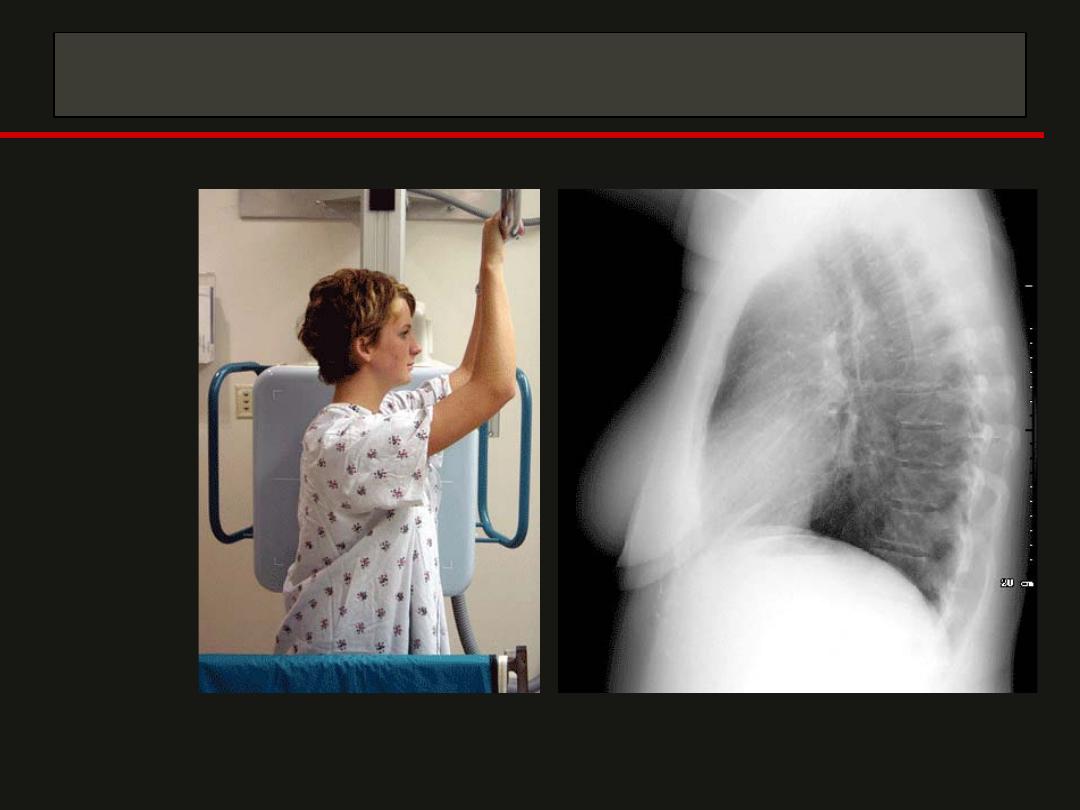
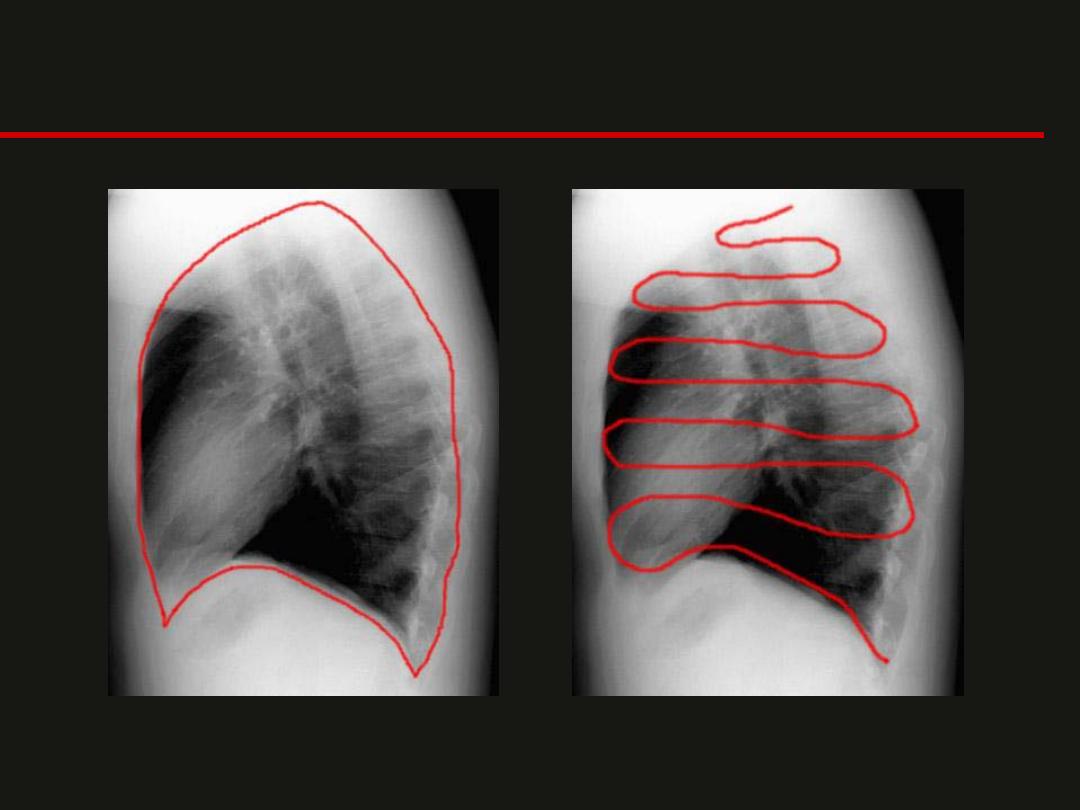
Lateral View
Ribs and Diaphragm
Postero-anterior or Antero-posterior
PA
AP
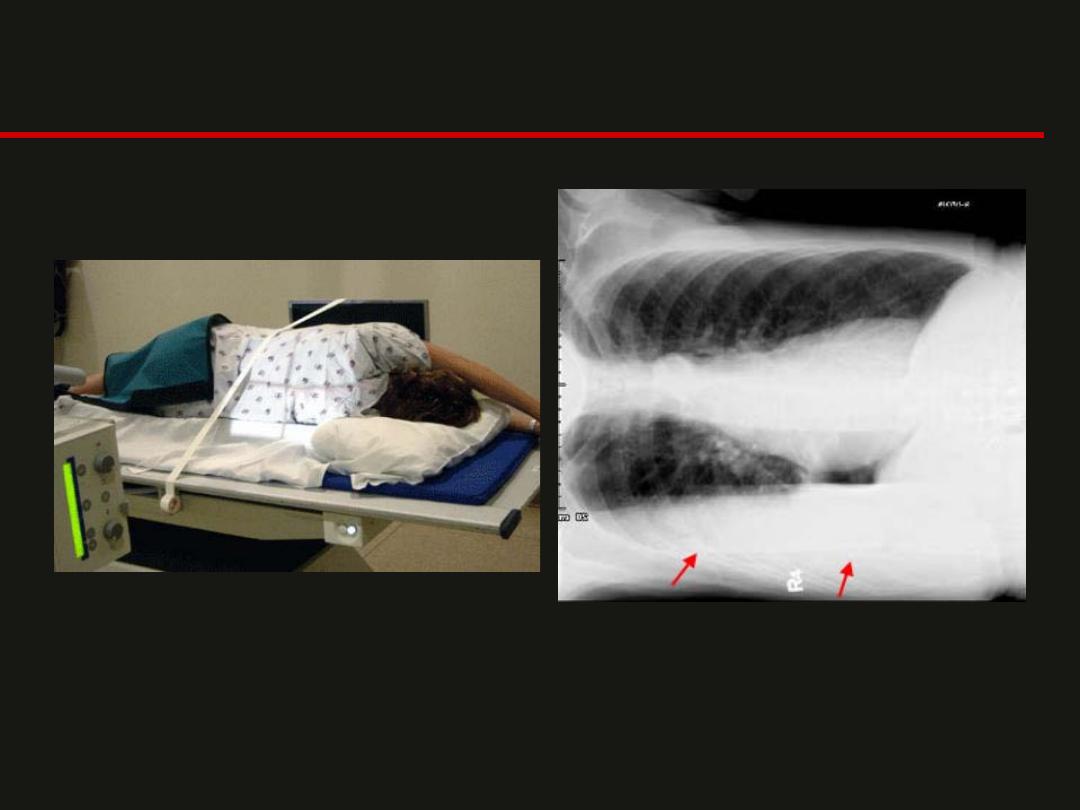
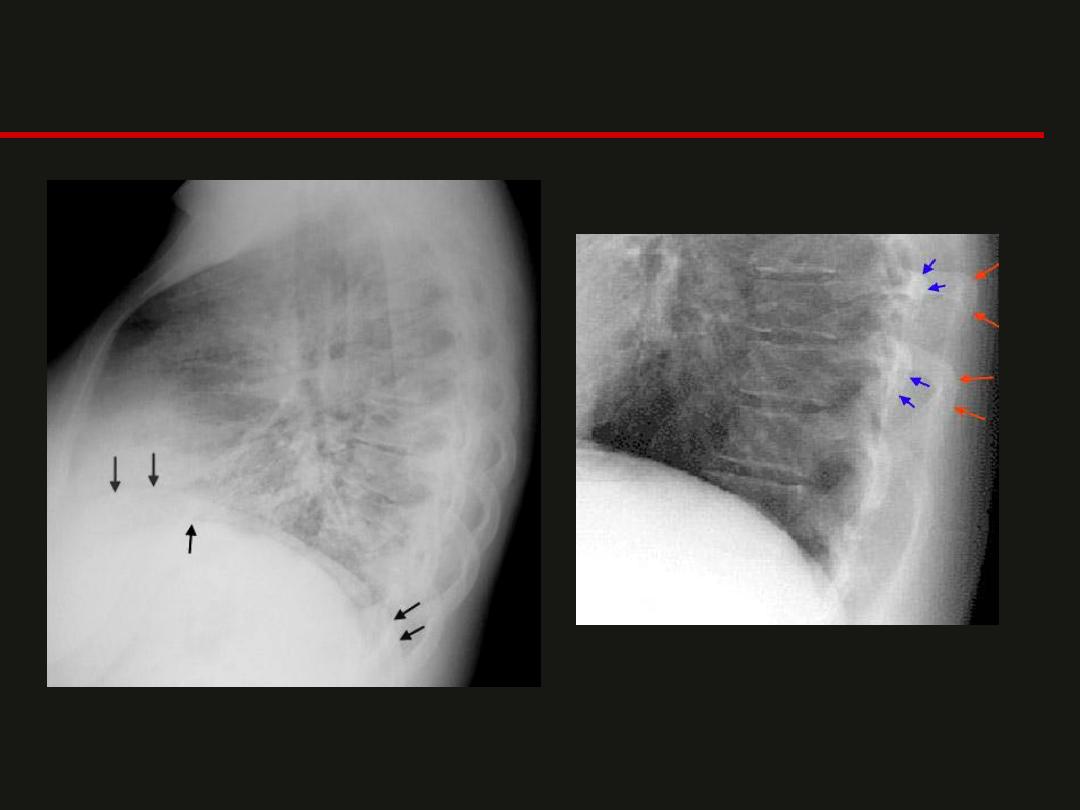
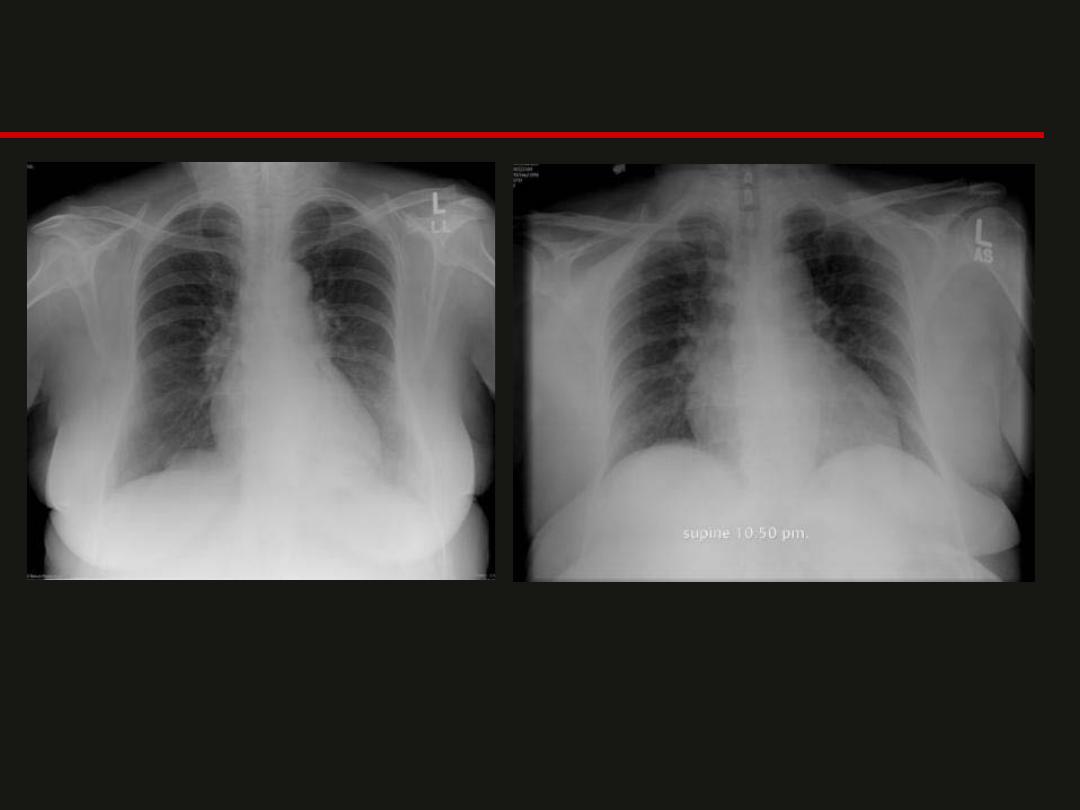
Lateral Decubitus
-Assess the volume of pleural effusion and demonstrate whether a
pleural effusion is mobile or loculated.
-You could also look at the nondependent hemithorax to confirm a
pneumothorax in a patient who could not be examined erect.
Inspiration
-
The patient should be examined in full inspiration.
-The diaphragm should be found at about the level
of the 8th - 10th posterior rib or 5th - 6th anterior rib
on good inspiration.
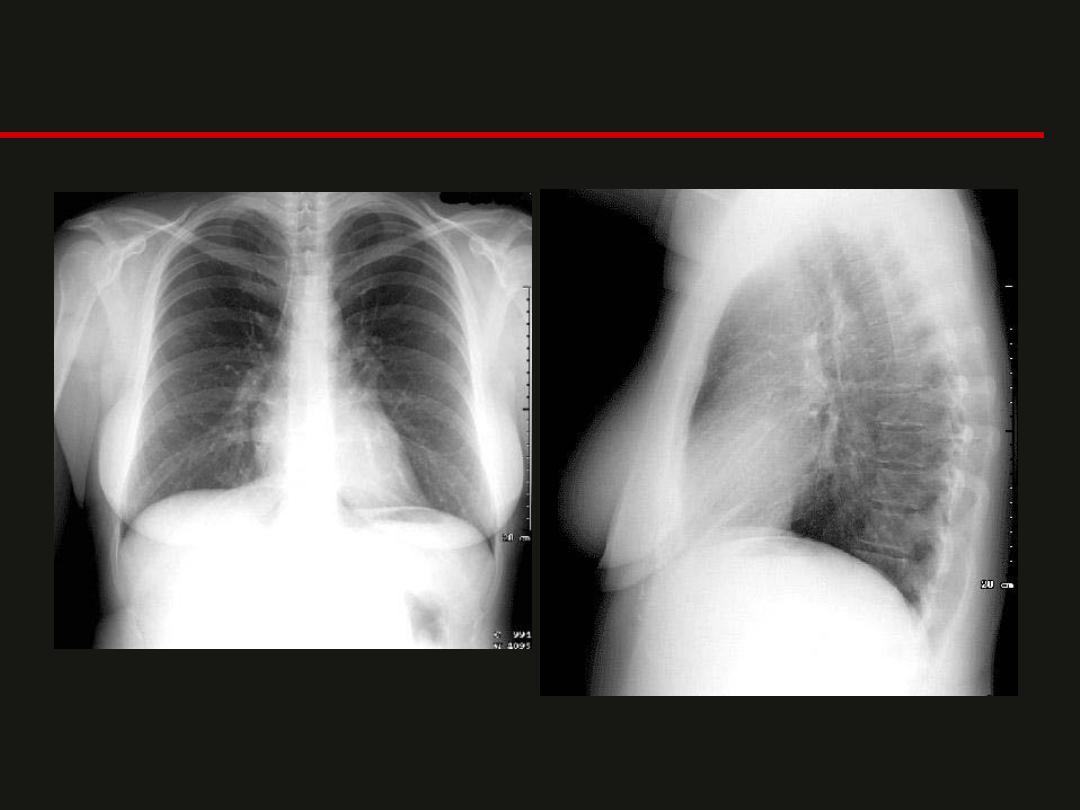
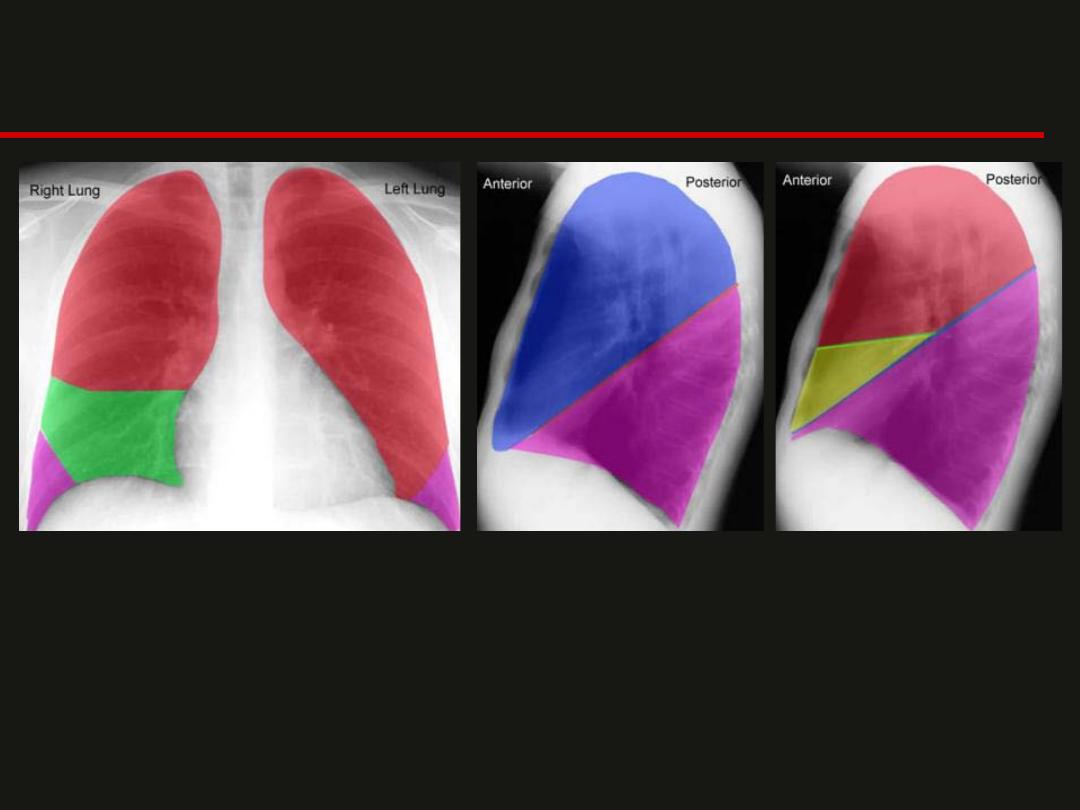
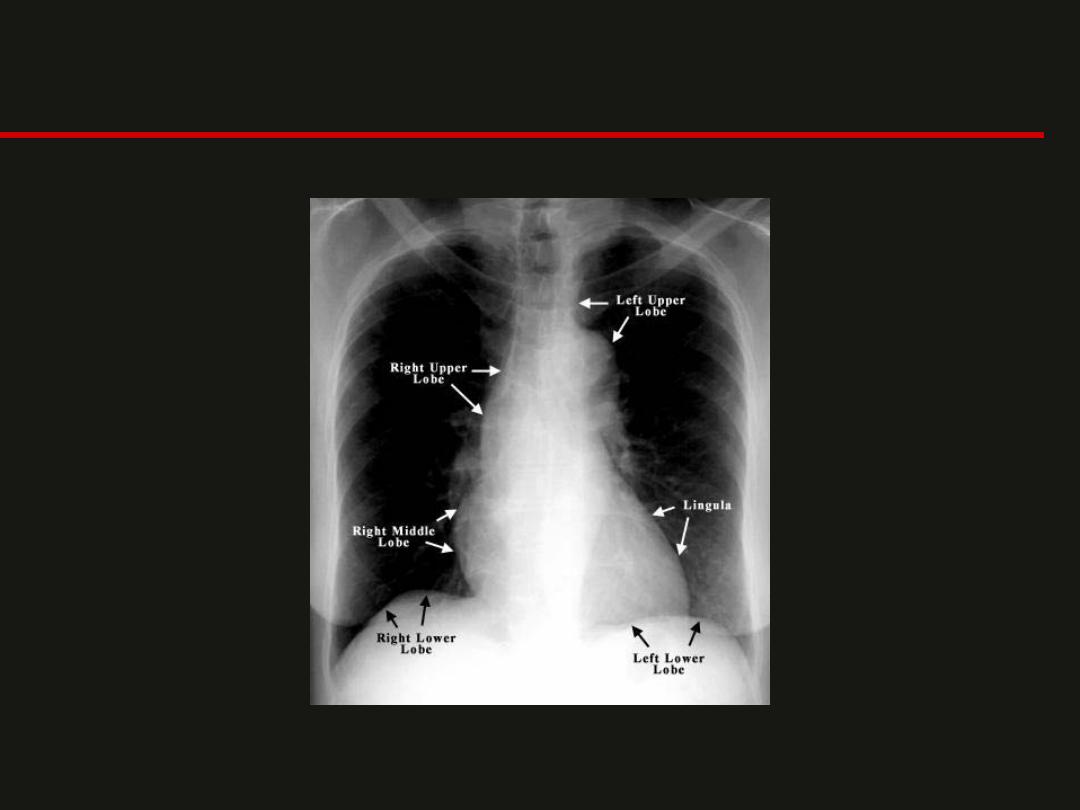
Right and Left Upper Lobes
Right Middle Lobe
Right and Left Lower Lobes
Left Upper Lobe
Major Fissure
Left Lower Lobe
Right Upper Lobe
Minor or Horizontal
Fissure
Right Middle Lobe
Major Fissure
Right Lower Lobe
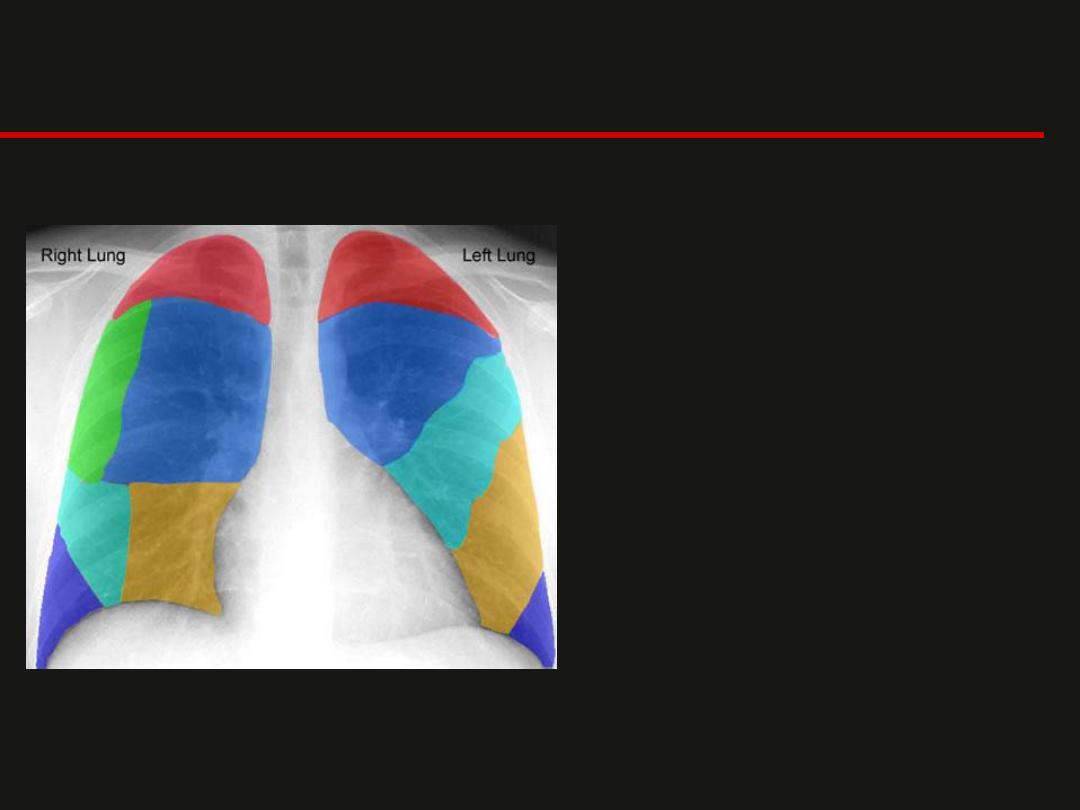
• Right Lung containing:
– RUL:
Apical Segment
– RUL:
Posterior Segment
– RUL:
Anterior Segment
– RML:
Lateral Segment
– RML:
Medial Segment
– RLL:
Anterior Basal Segment
• Left Lung containing:
– LUL:
Apical Posterior Segment
– LUL:
Anterior Segment
– LUL:
Lingula Superior Segment
– LUL:
Lingula Inferior Segment
– LLL:
Anteromedial Segment
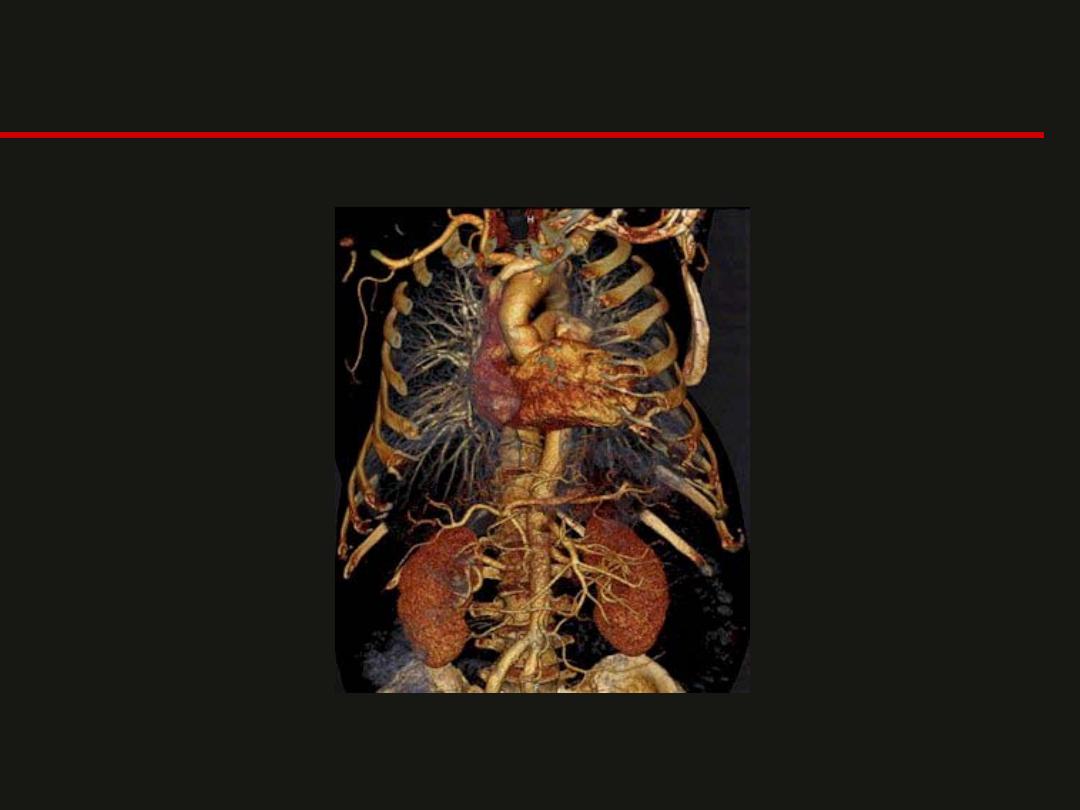
CT Anatomy
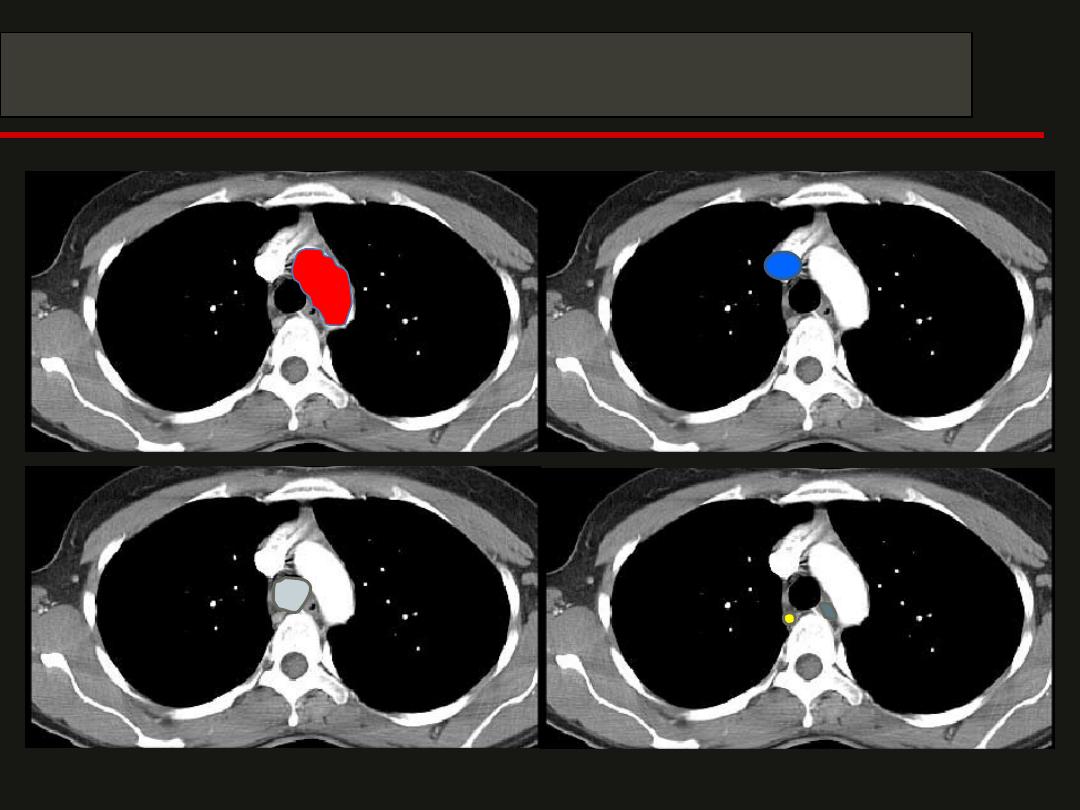
CT Anatomy

CT Anatomy
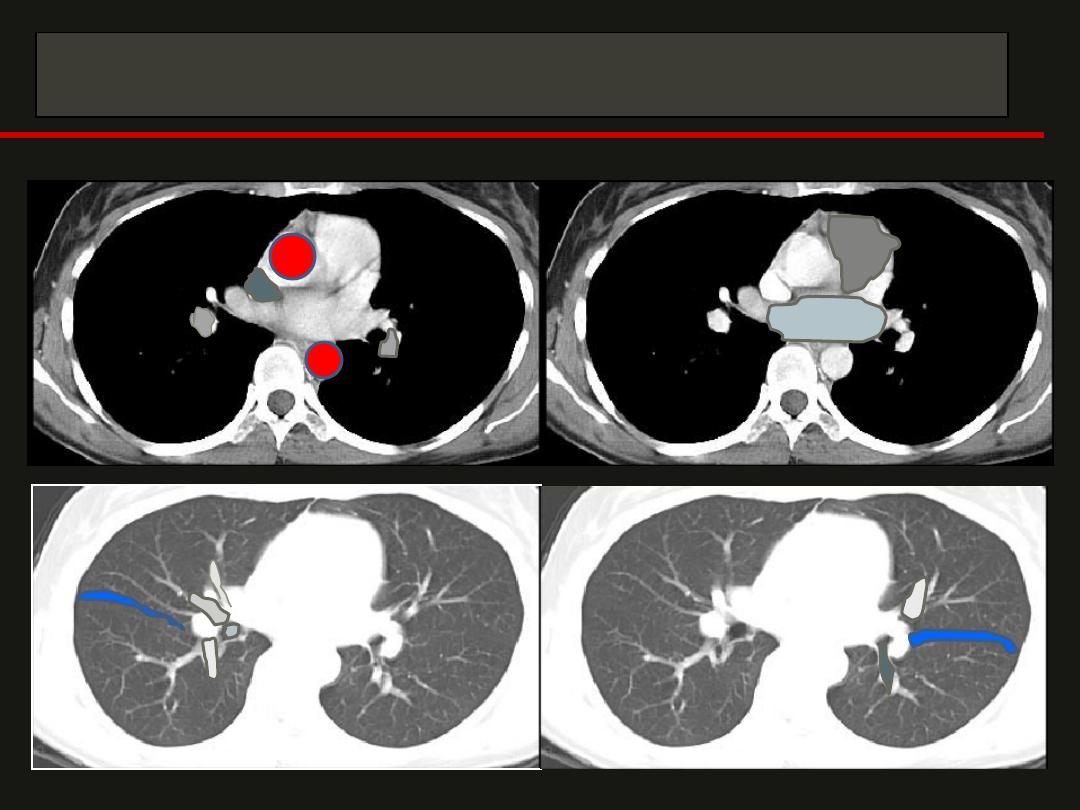
CT Anatomy
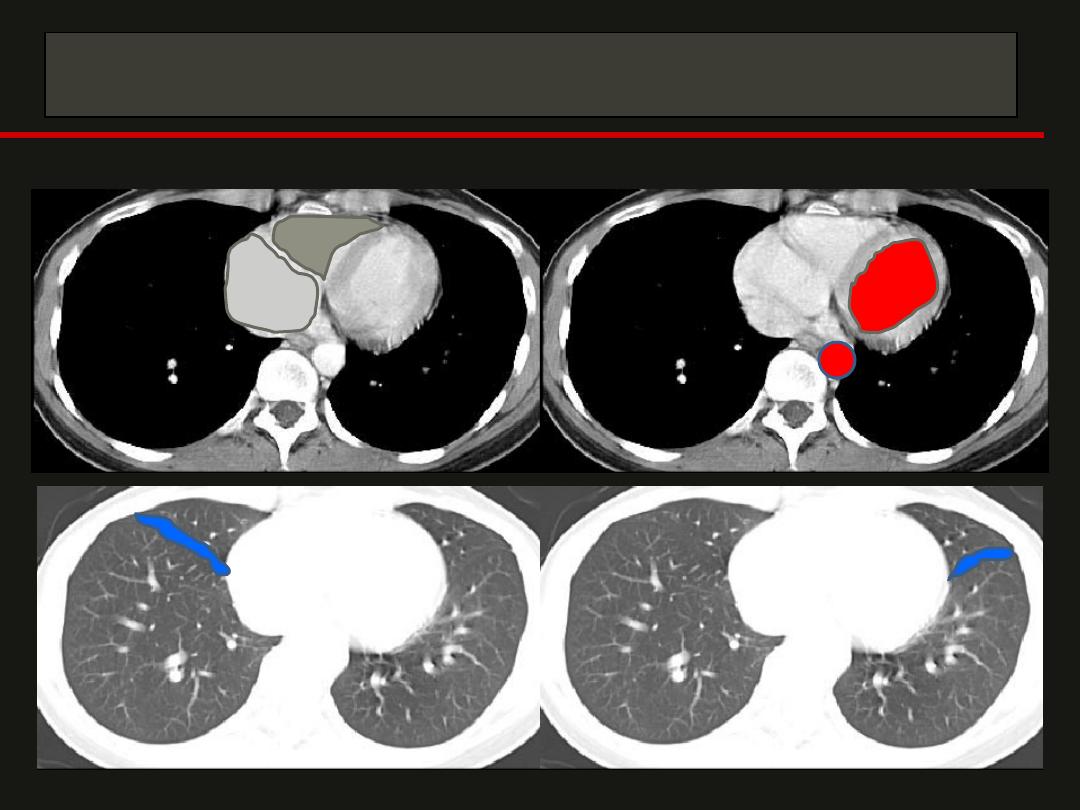
CT Anatomy
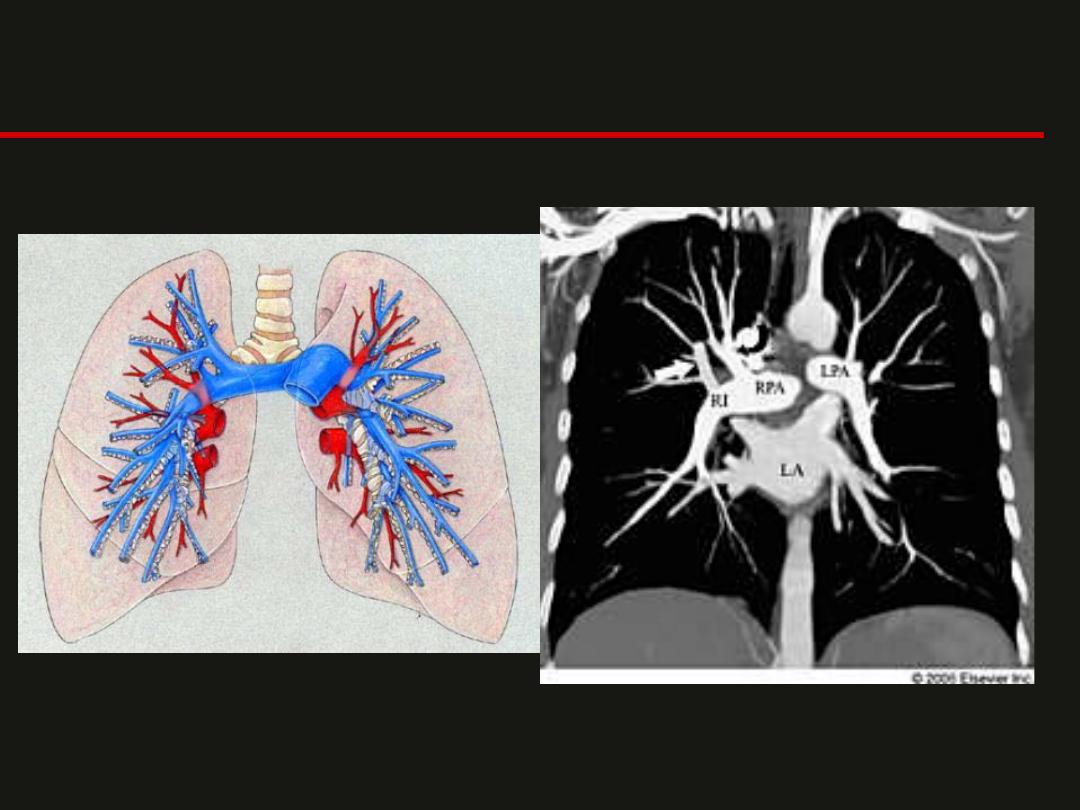
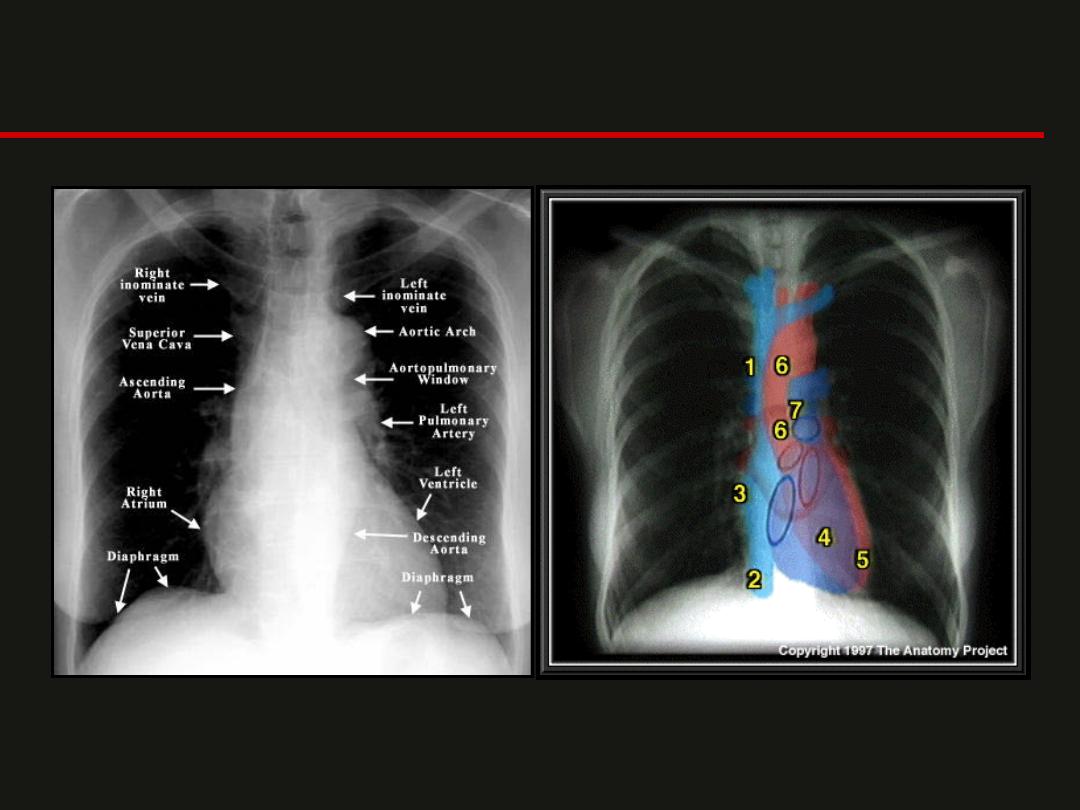
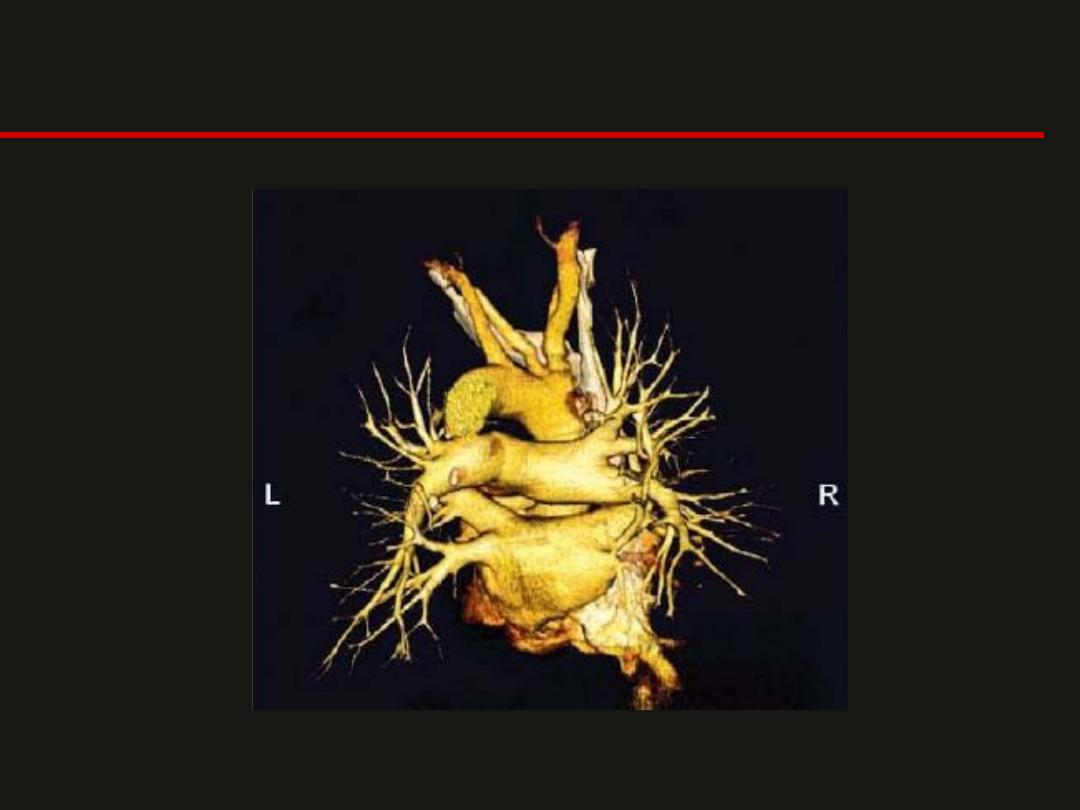
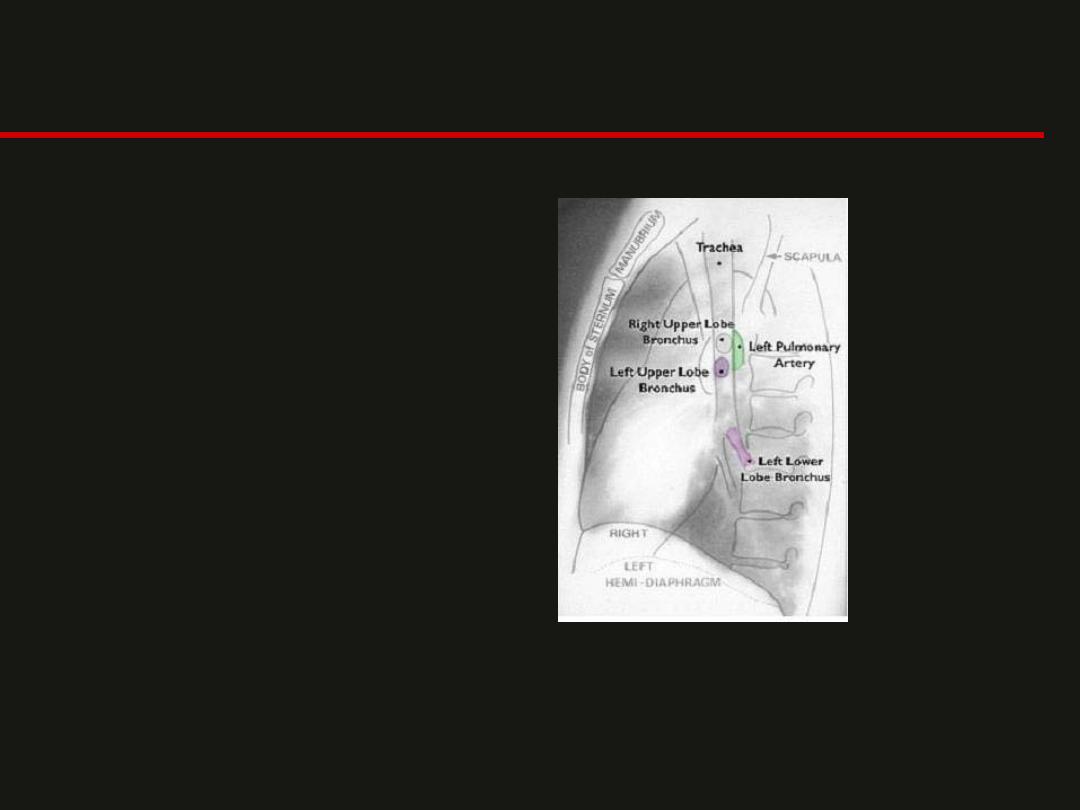
Pulmonary Vasculature

Fissures
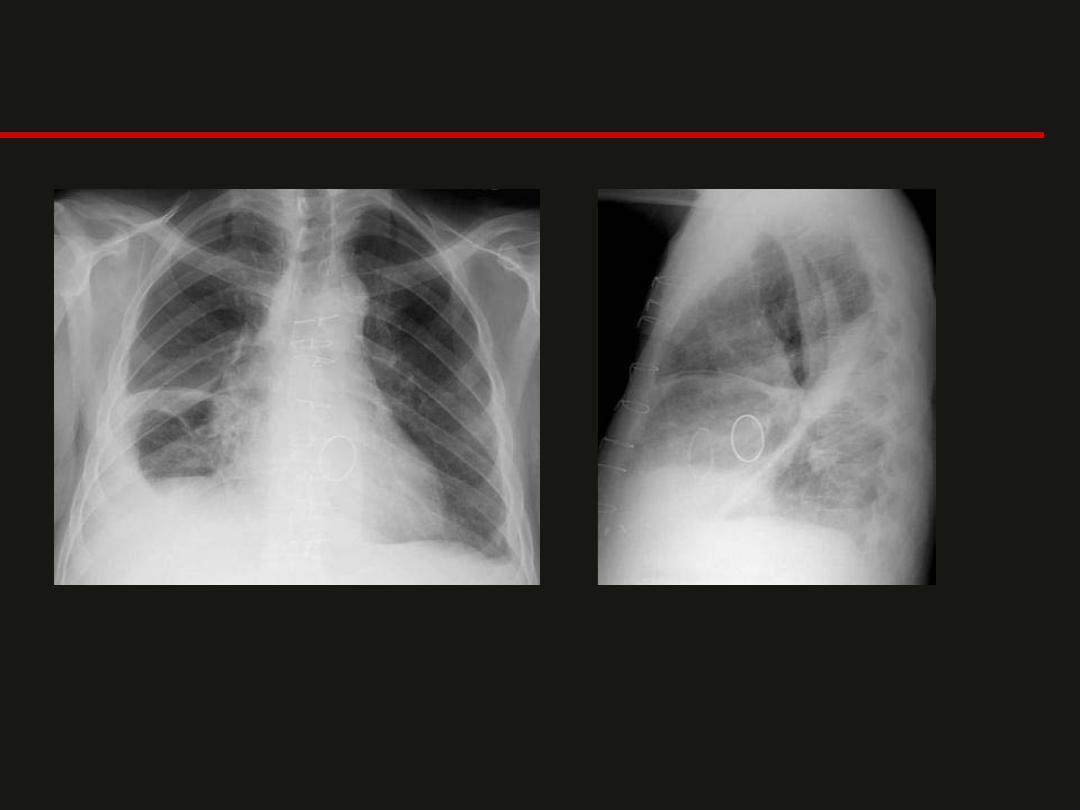
Lobes and Fissures
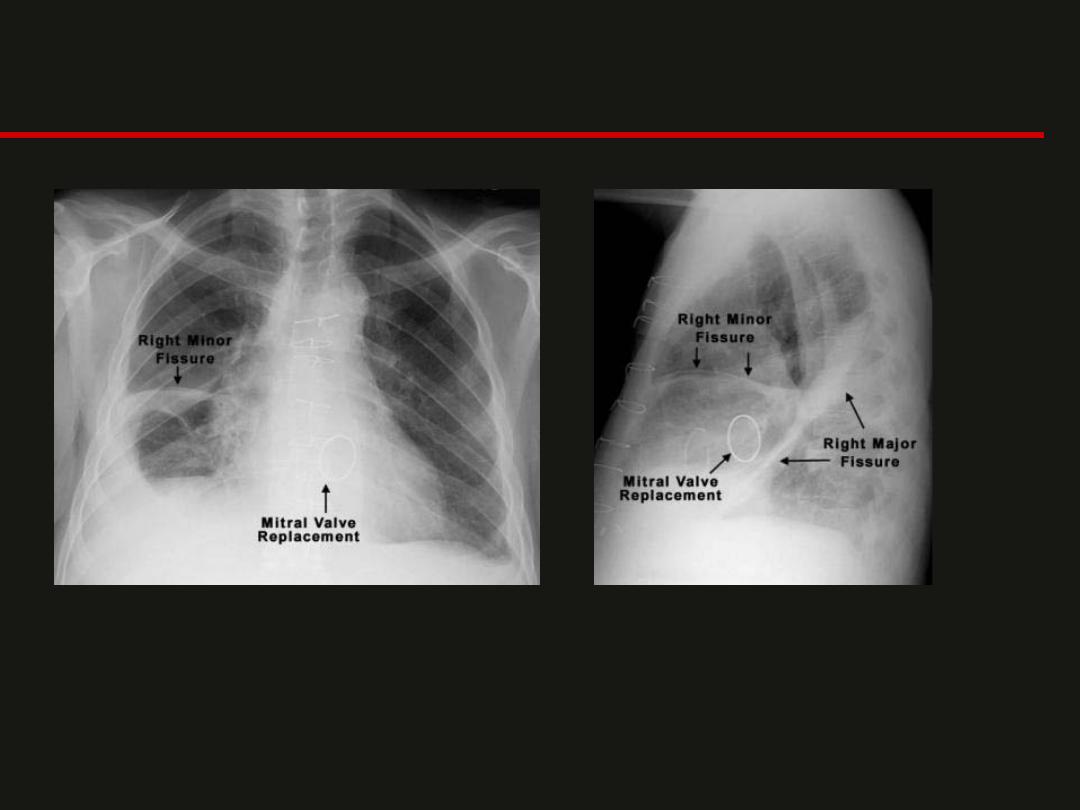
Lobes and Fissures
How to Read a Chest X-Ray
• Patient Data (name history #, age, sex, old films)
• Routine Technique: AP/PA, supine or erect
• Trachea: midline or deviated, caliber, mass
• Lungs: abnormal shadowing or lucency
• Pulmonary vessels: vascular enlargement
• Hila: masses, lymphadenopathy
• Heart: thorax: heart width > 2:1 ? Cardiac configuration?
• Mediastinal contour: width? mass? Course of aorta
• Pleura: effusion, thickening, calcification
• Bones: lesions or fractures
• Soft tissues: don’t miss a mastectomy
• ICU Films: identify tubes first and look for pneumothorax
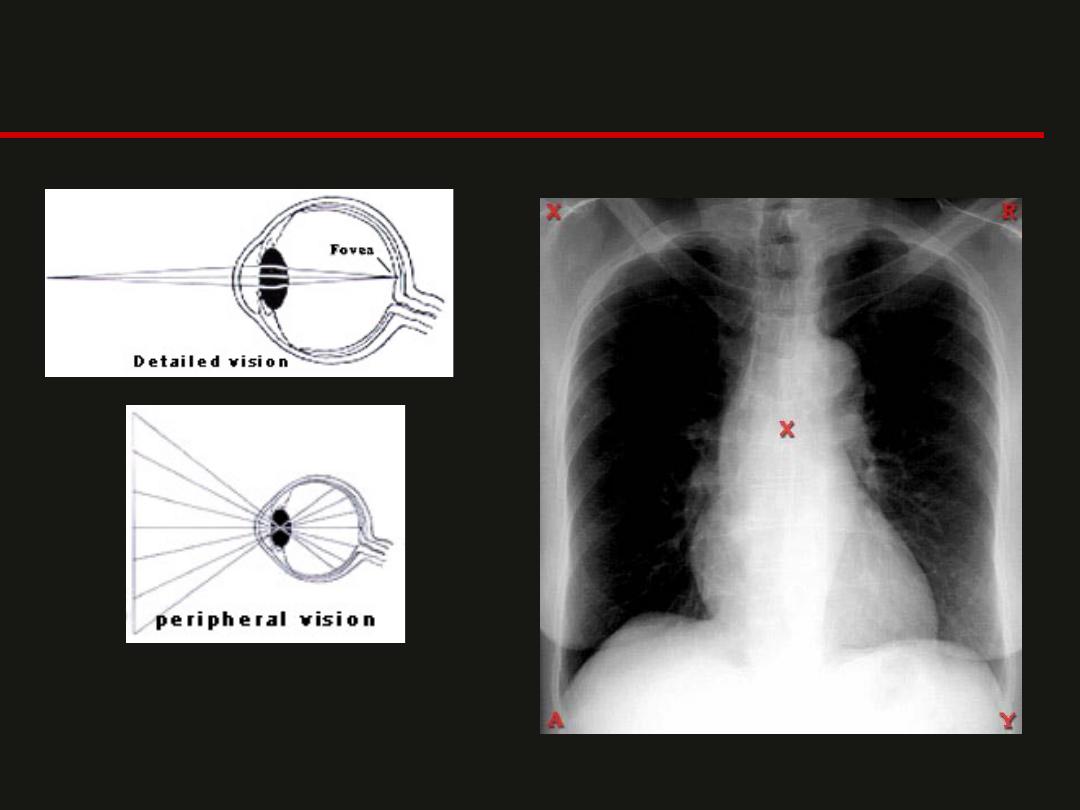
Looking for Abnormalities
Do a directed search of the chest film
rather than simply gazing at the film
Silhouette Sign
• One of the most useful
signs in chest radiology
• Described by Dr. Ben
Felson
• The silhouette sign is in
essence elimination of
the silhouette or loss of
lung (air)/soft tissue
interface caused by a
mass or fluid in the
normally air filled lung.
• If an intrathoracic opacity
is in anatomic contact with
the heart border, then the
opacity will obscure that
border.
• The sign is commonly
applied to the heart, aorta,
chest wall, and diaphragm.
• The location of this
abnormality can help to
determine the location
anatomically.
Which lobe is it?
Silhouette Sign
For the heart, the silhouette
sign can be caused by an opacity
in the
RML, lingula, anterior
segment of the upper lobe, and
anterior portion of the pleural
cavity
.
This contrasts with an opacity in
the
posterior pleural cavity,
posterior mediastinum, or lower
lobes
which cause an overlap and
not an obliteration of the heart
border.
Silhouette Sign
Silhouette Sign
Air Bronchogram
• Is a tubular outline of an
airway made visible by
filling of the surrounding
alveoli by fluid or
inflammatory exudates
• Six causes of air
bronchograms are;
– lung consolidation,
– pulmonary edema,
– nonobstructive pulmonary
atelectasis,
– severe interstitial disease,
– neoplasm, and
– normal expiration
.
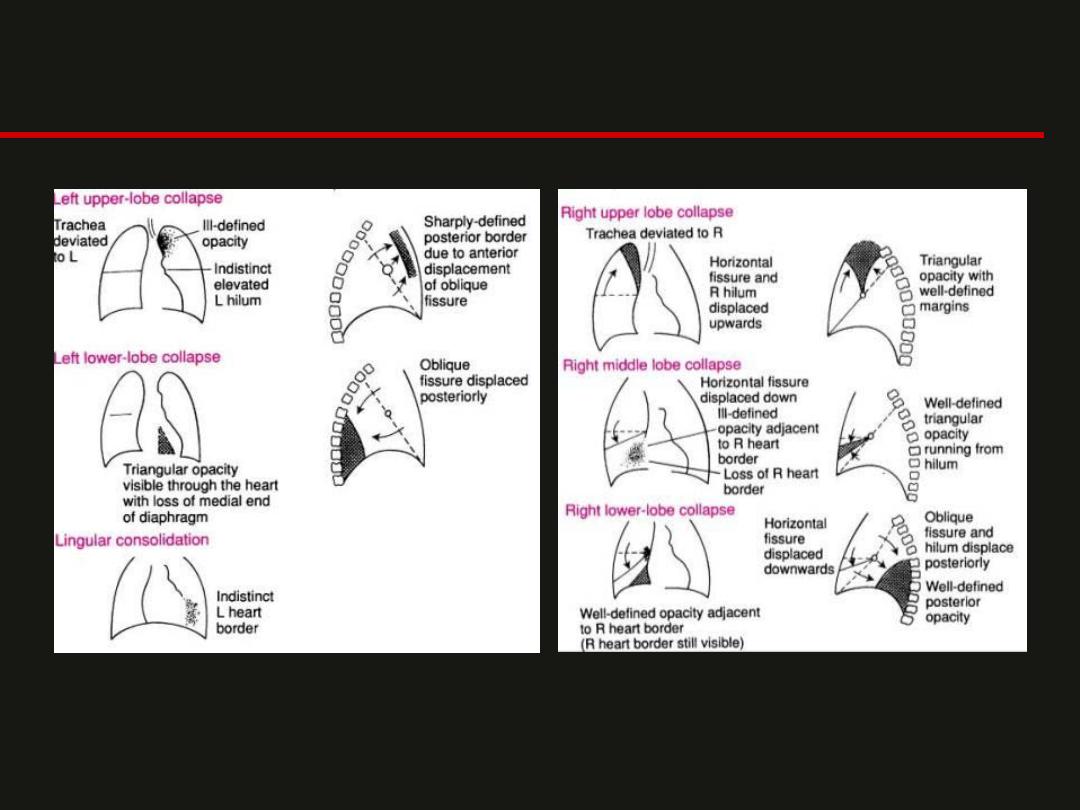
Atelectasis
• Collapse or incomplete
expansion of the lung or
part of the lung
• Often caused by an
endobronchial lesion,
such as mucus plug or
tumor
• Extrinsic compression
centrally by a mass such
as lymph nodes or
peripheral compression
by pleural effusion
• Atelectasis is almost
always associated with a
linear increased density
on chest x-ray
• Indirect signs of volume
loss include vascular
crowding or fissural,
tracheal, or mediastinal
shift, towards the
collapse.
• Segmental and
subsegmental collapse
may show linear,
curvilinear, wedge
shaped opacities. This is
most often associated
with post-op patients
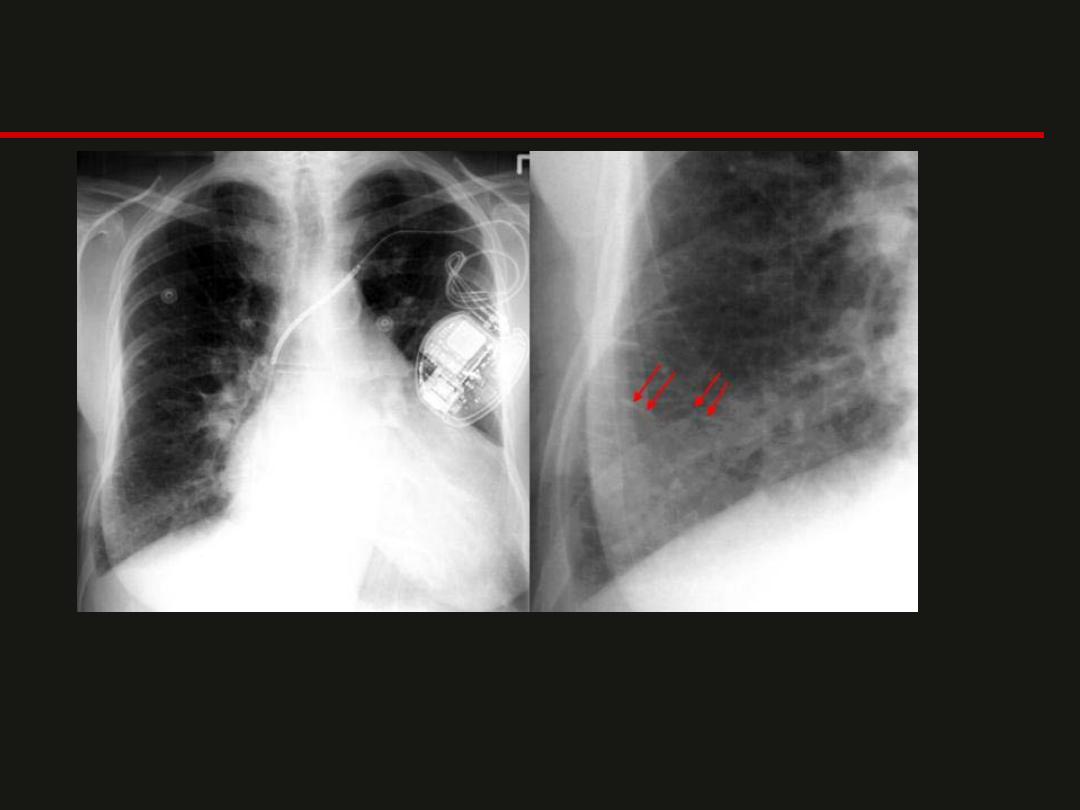
Atelectasis
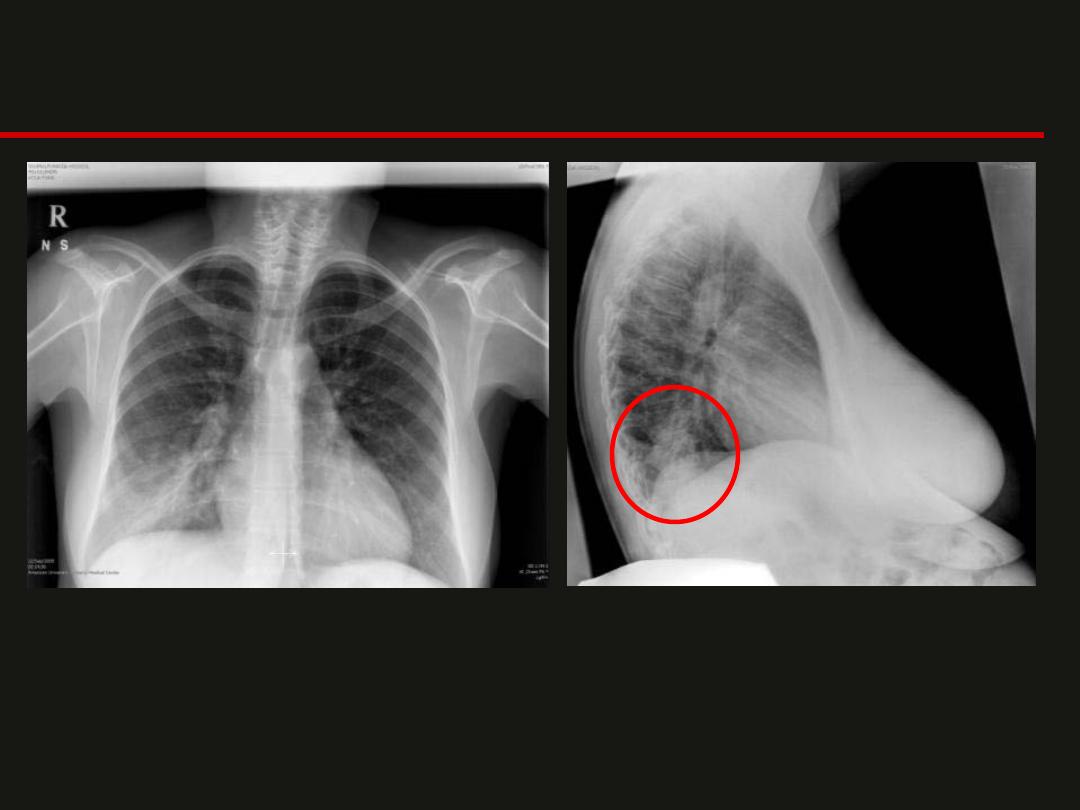
LLL Collapse
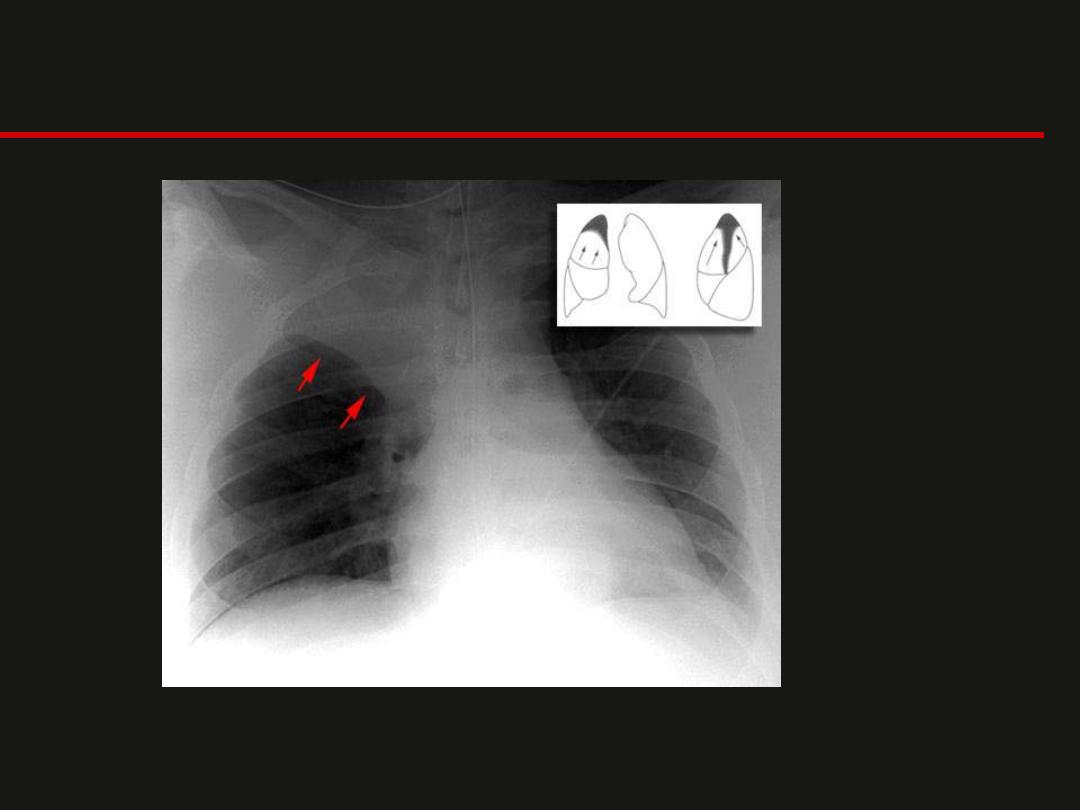
RUL Collapse
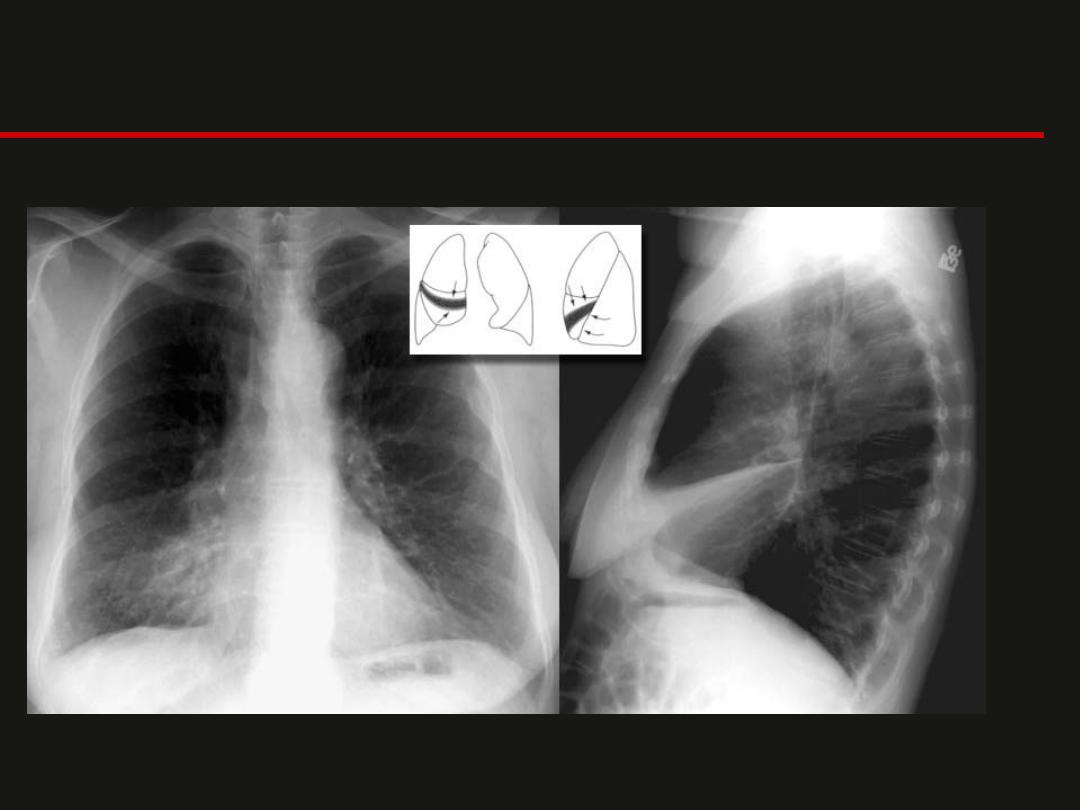
RML Collapse
Pulmonary Edema
• Two basic types of
pulmonary edema.
– cardogenic edema
caused
by increased hydrostatic
pulmonary capillary
pressure.
– noncardogenic
pulmonary
edema, and is caused by
either altered capillary
membrane permeability
or decreased plasma
oncotic pressure.
• NOT CARDIAC
– N
ear-drowning,
– O
xygen therapy,
– T
ransfusion or trauma,
– C
NS disorder,
– A
RDS, aspiration, or
altitude sickness,
– R
enal disorder or
resuscitation,
– D
rugs,
– I
nhaled toxins,
– A
llergic alveolitis,
– C
ontrast or contusion.
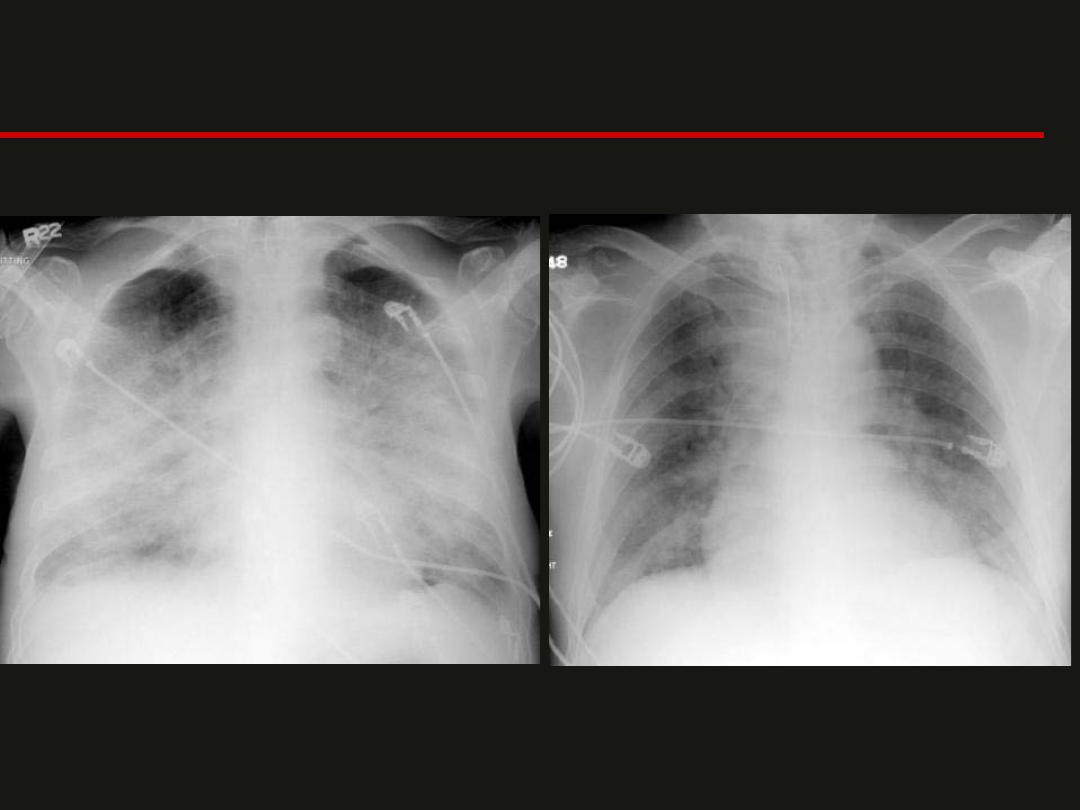
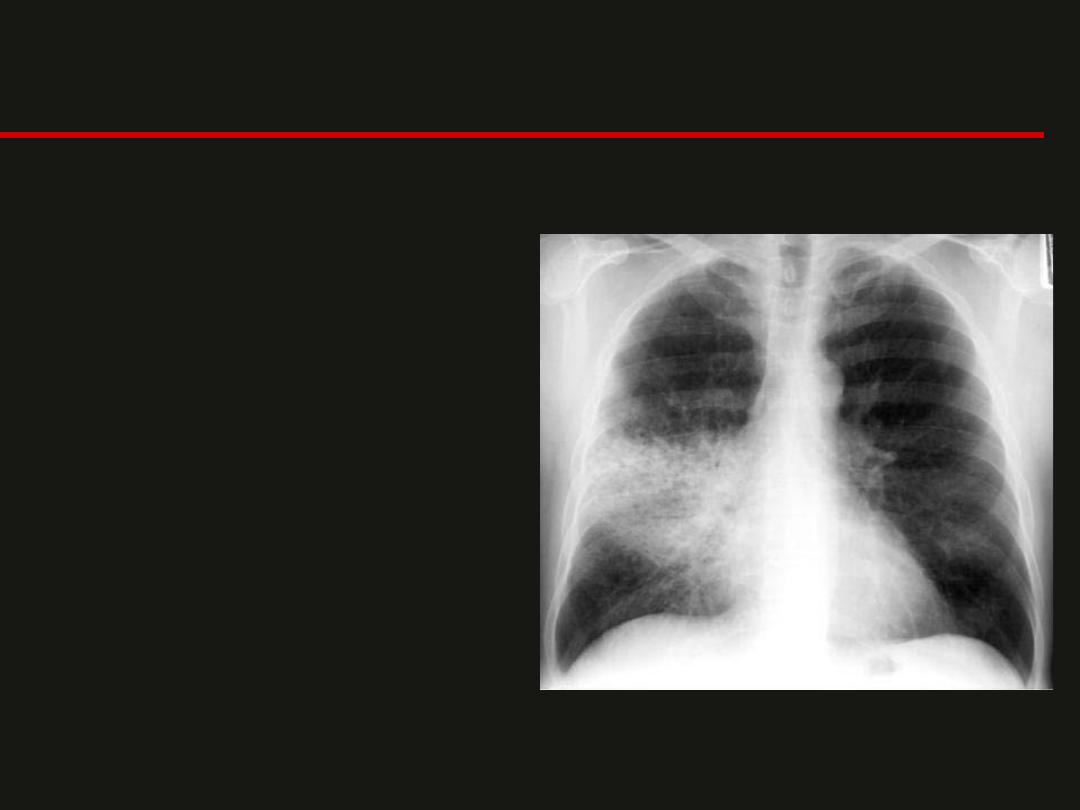
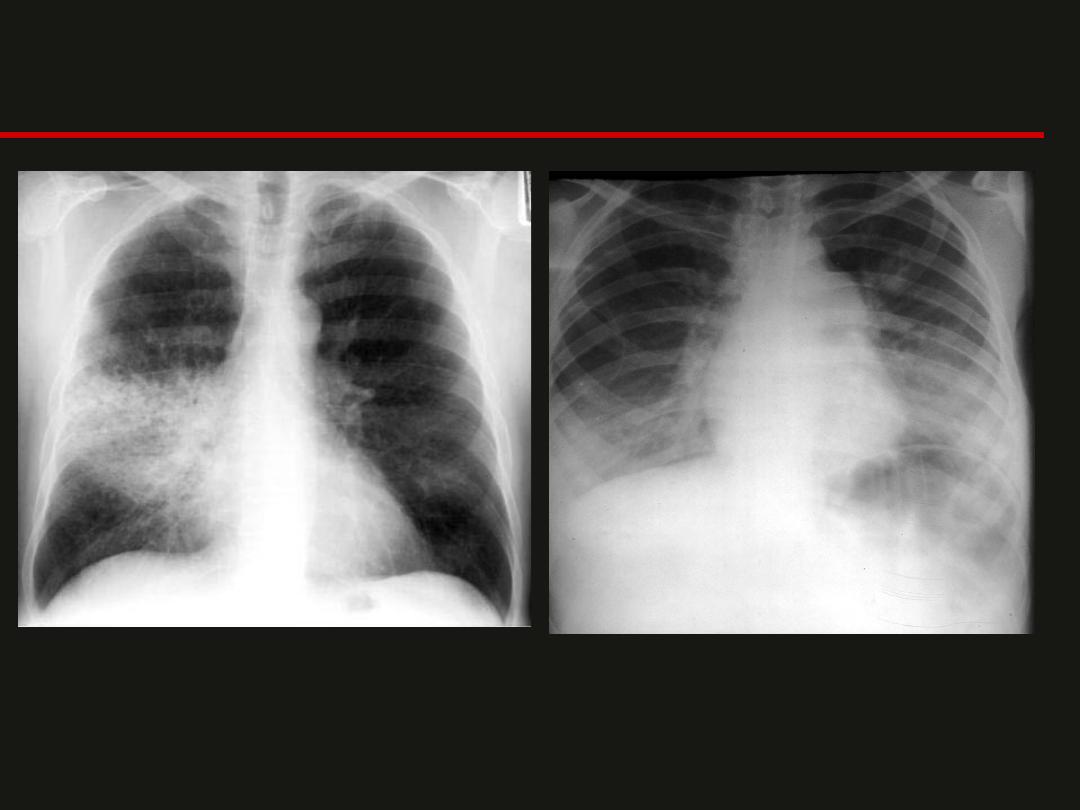
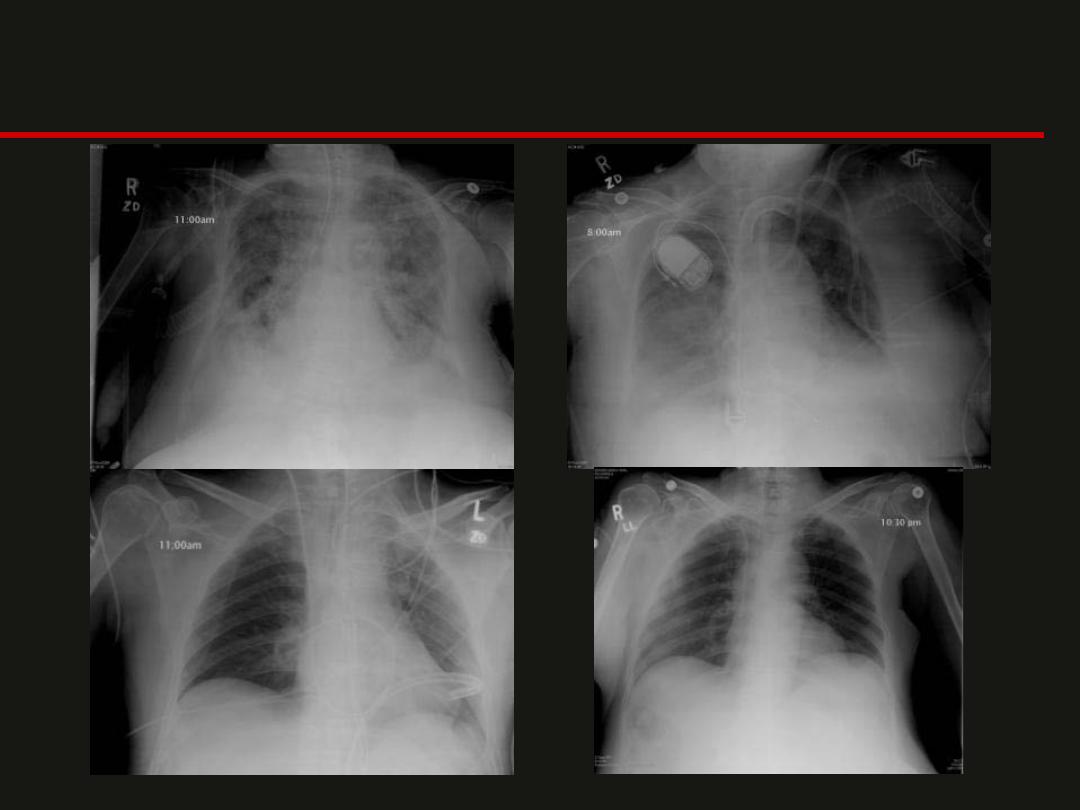
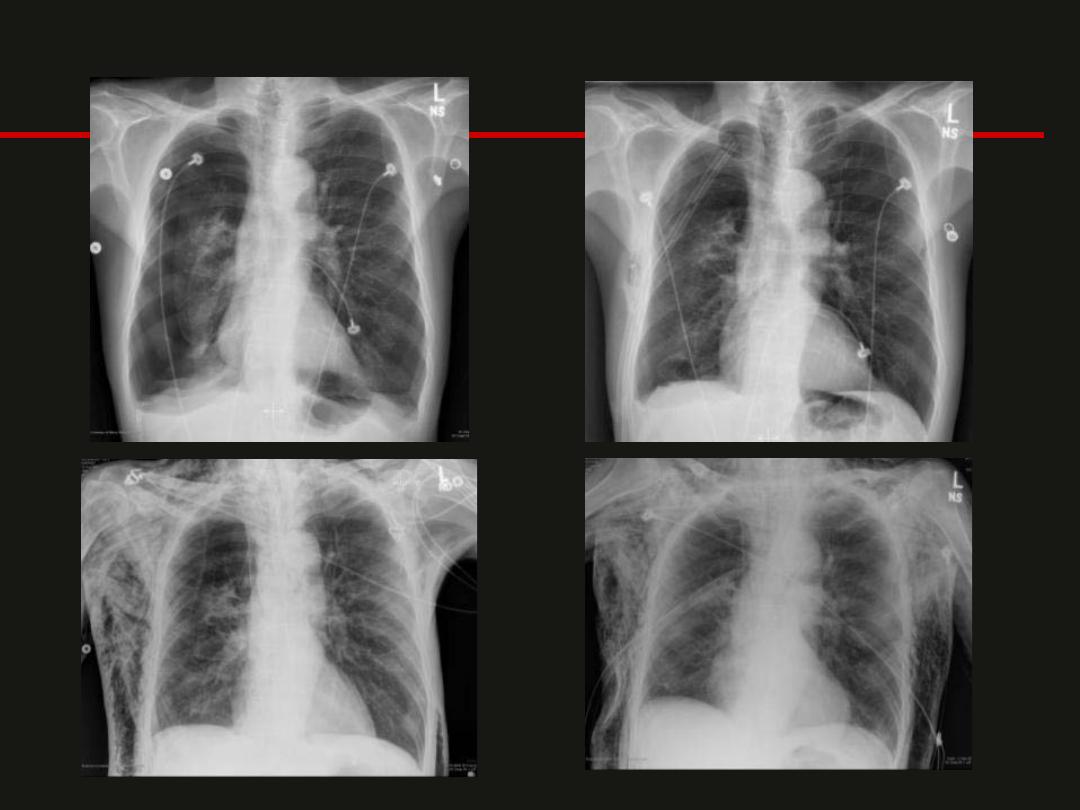
Pulmonary Edema

Pulmonary Edema
June 2, 2009
June 4, 2009
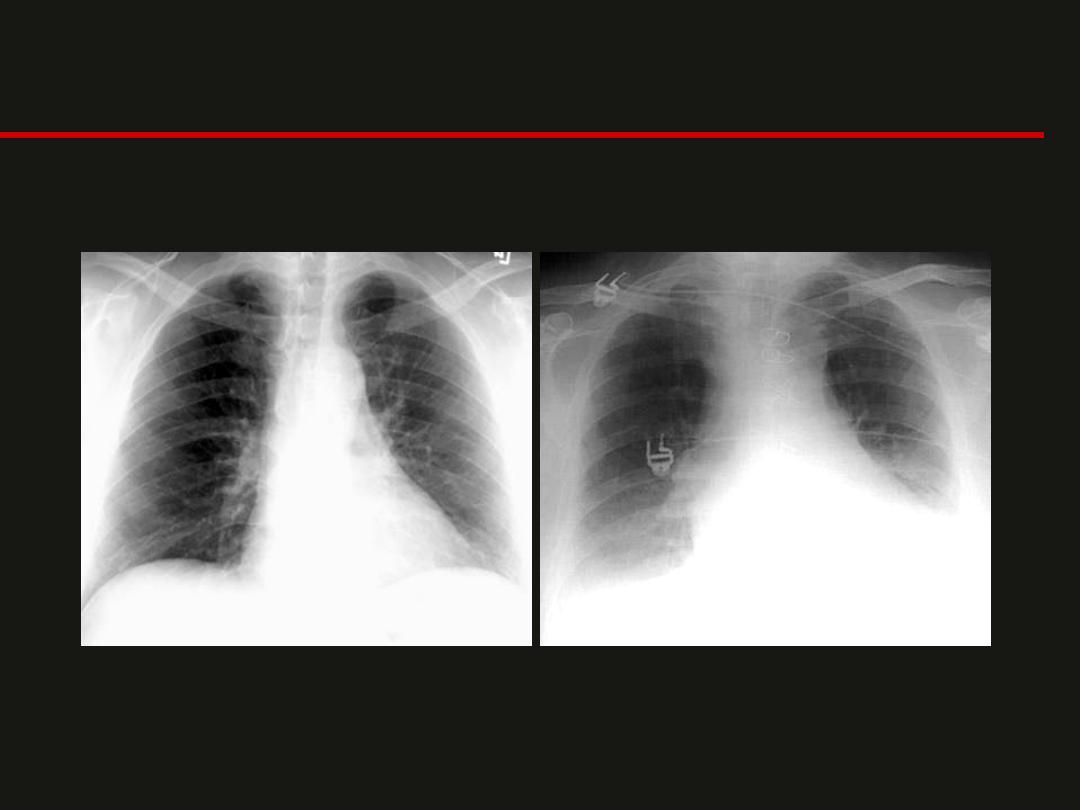
Congestive Heart Failure
• Congestive heart failure (CHF) is one of the
most common abnormalities evaluated by
CXR.
• The earliest CXR finding of CHF is
cardiomegaly, detected as an increased
cardiothoracic ratio (>50%).
• In the pulmonary vasculature of the normal
chest, the lower zone pulmonary veins are
larger than the upper zone veins due to
gravity.
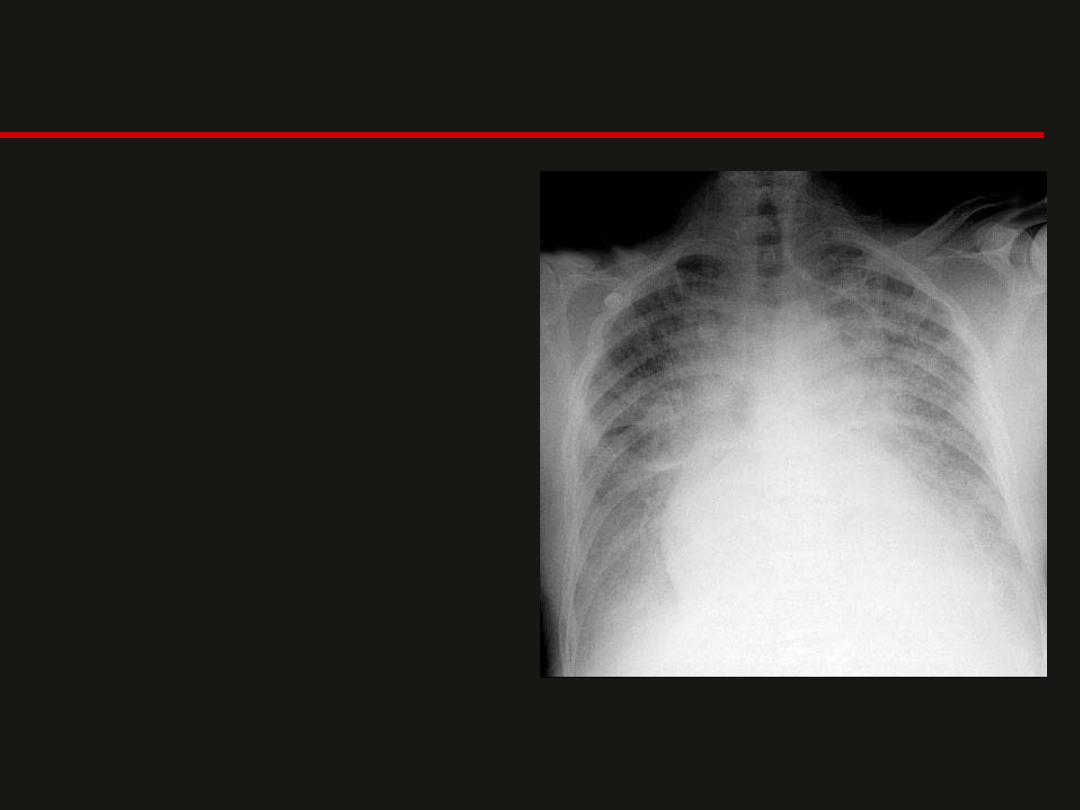
CHF
– In a patient with CHF, the
pulmonary capillary wedge
pressure rises to the 12-18
mmHg range and the upper
zone veins dilate and are
equal in size or larger,
termed
cephalization
.
– With increasing PCWP, (18-
24 mm. Hg.), interstitial
edema occurs with the
appearance of Kerley lines.
– Increased PCWP above this
level is alveolar edema,
often in a classic perihilar
bat wing pattern of density.
Pleural effusions also often
occur
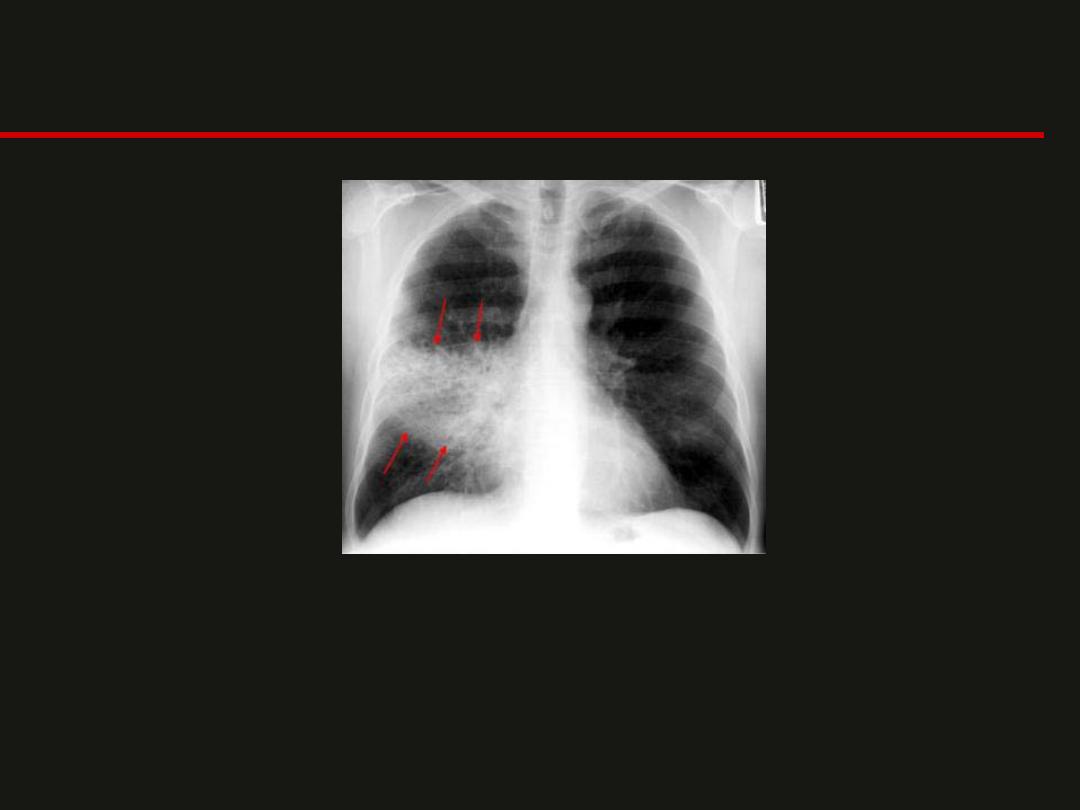
cardiomegaly, alveolar edema, cephalization and
haziness of vascular margins.
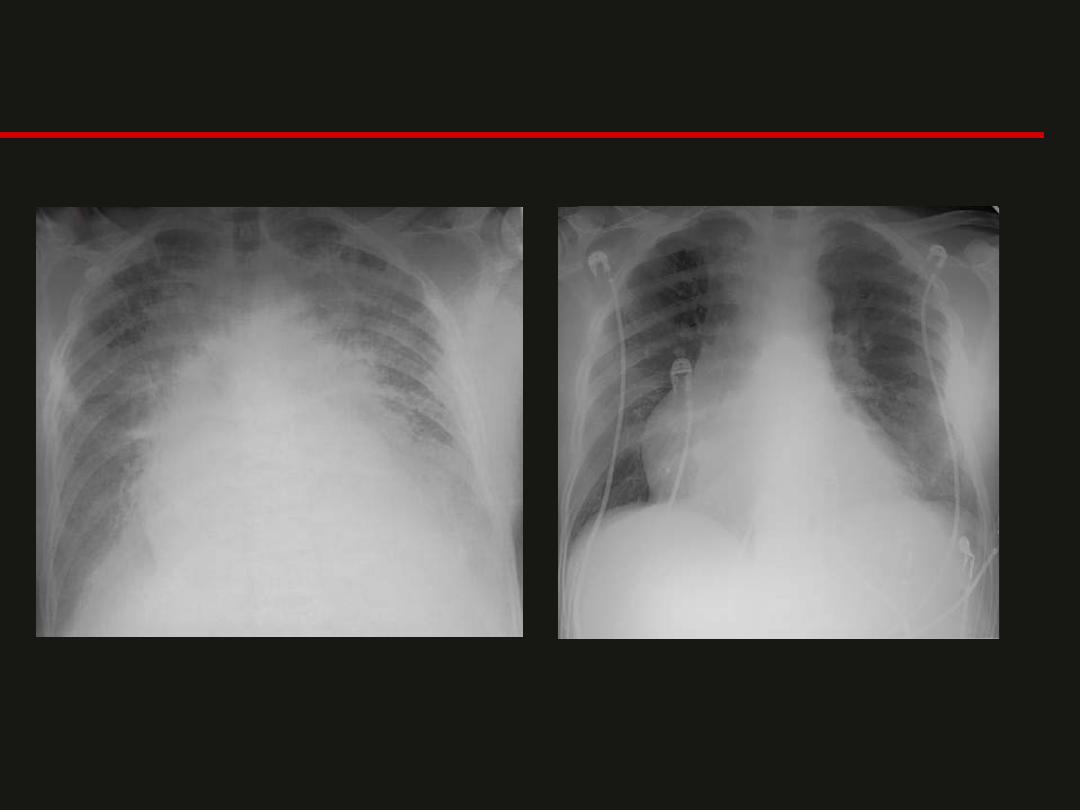
CHF
Kerley B lines
Horizontal lines less than 2cm long, commonly found in the lower zone periphery. These
lines are the thickened, edematous interlobular septa.
Causes include; pulmonary edema, lymphangitis carcinomatosa and malignant lymphoma,
viral and mycoplasmal pneumonia, interstital pulmonary fibrosis, pneumoconiosis,
sarcoidosis, chronic CHF
Atelactasis vs. Pneumonia
Atelectasis
Pneumonia
Volume Loss
Associated Ipsilateral Shift
Linear, Wedge-Shaped
Apex at Hilum
Normal or Increased Volume
No Shift, or if Present Then
Contralateral
Consolidation, Air Space
Process
Not Centered at Hilum
Air bronchograms can occur in both.
indistinct borders, air bronchograms, and silhouetting of the
right heart border.
LLL Pneumonia

--- Pneumonia
? Pneumonia
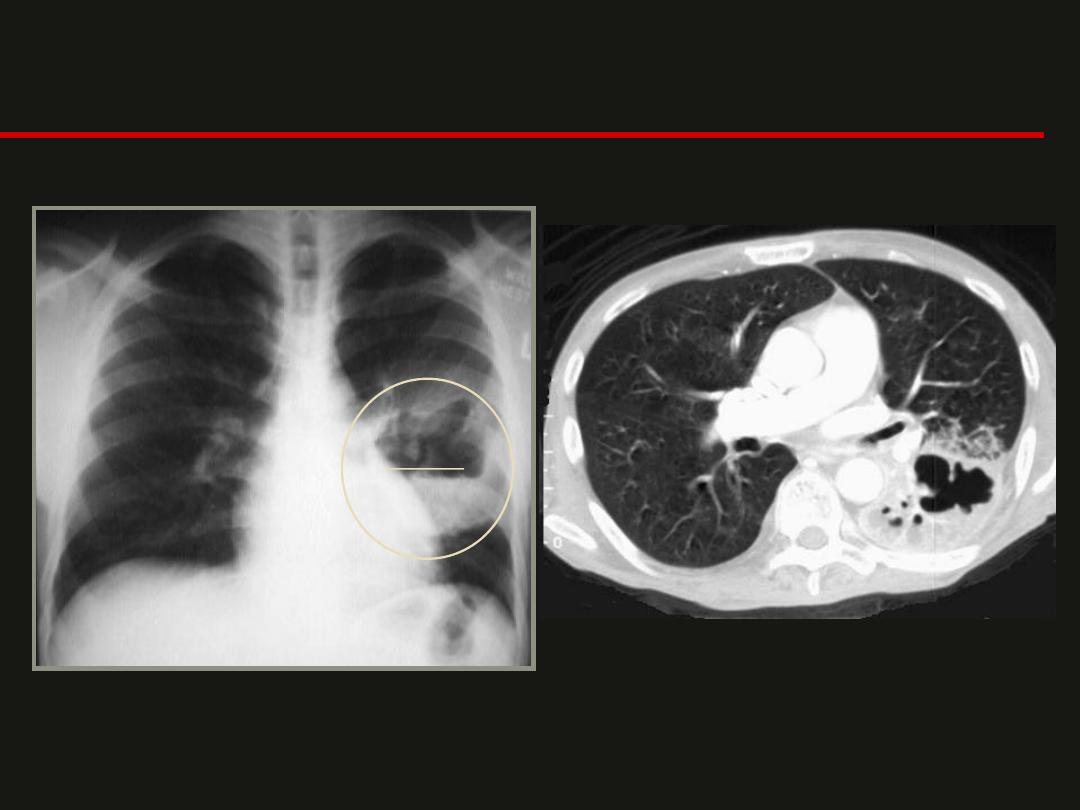
Lung abscess
A
F
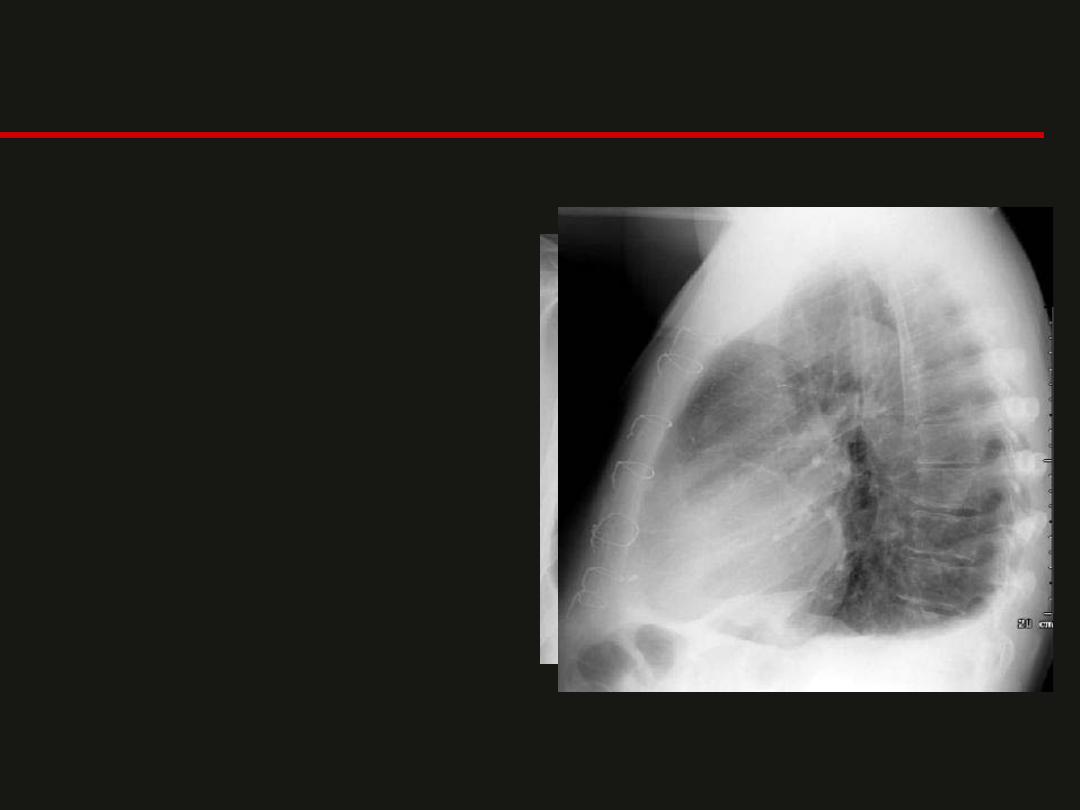
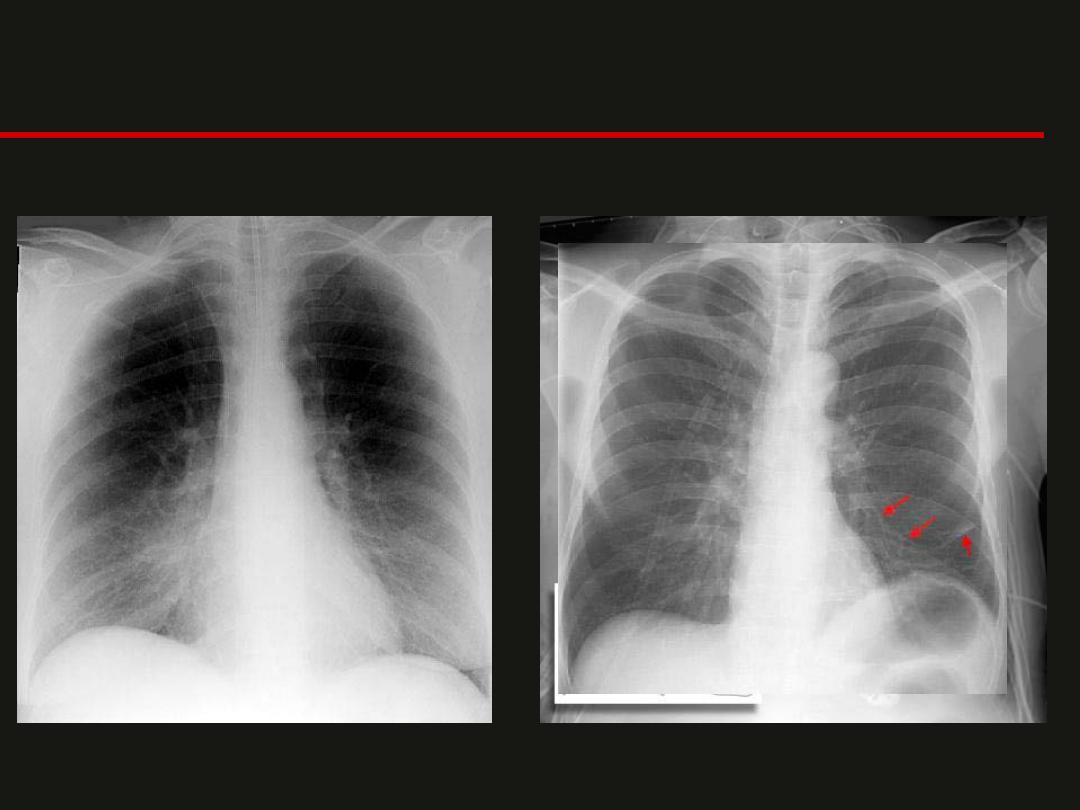
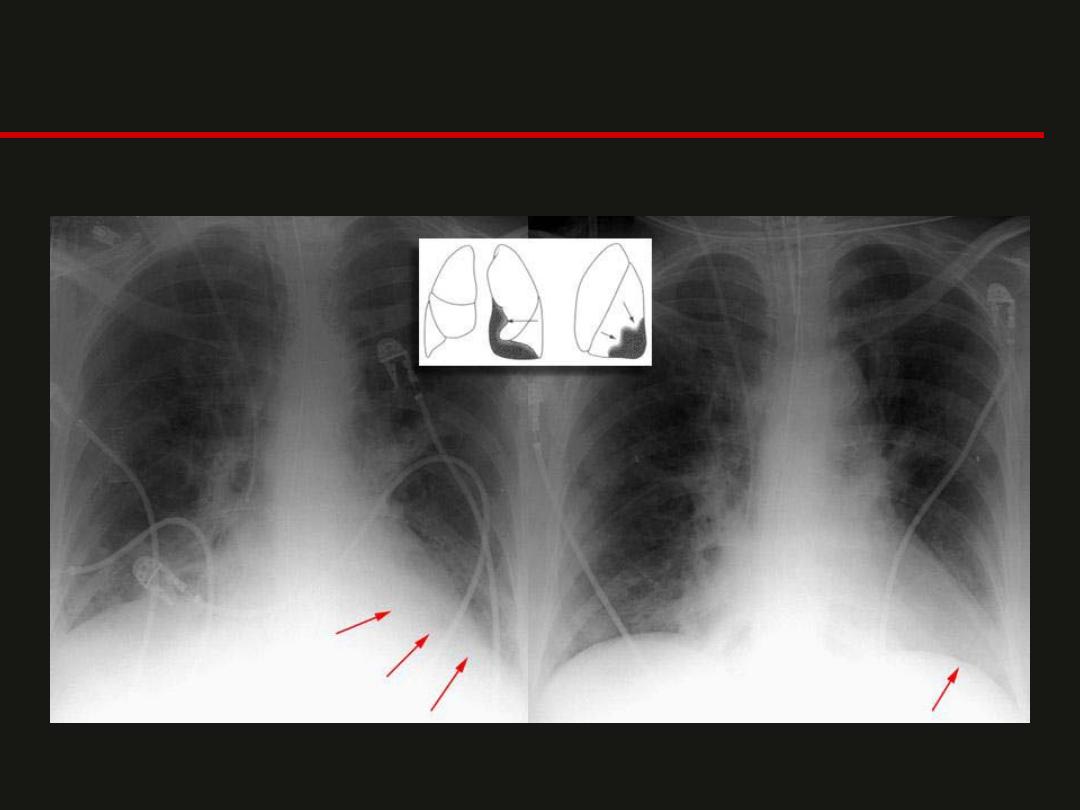
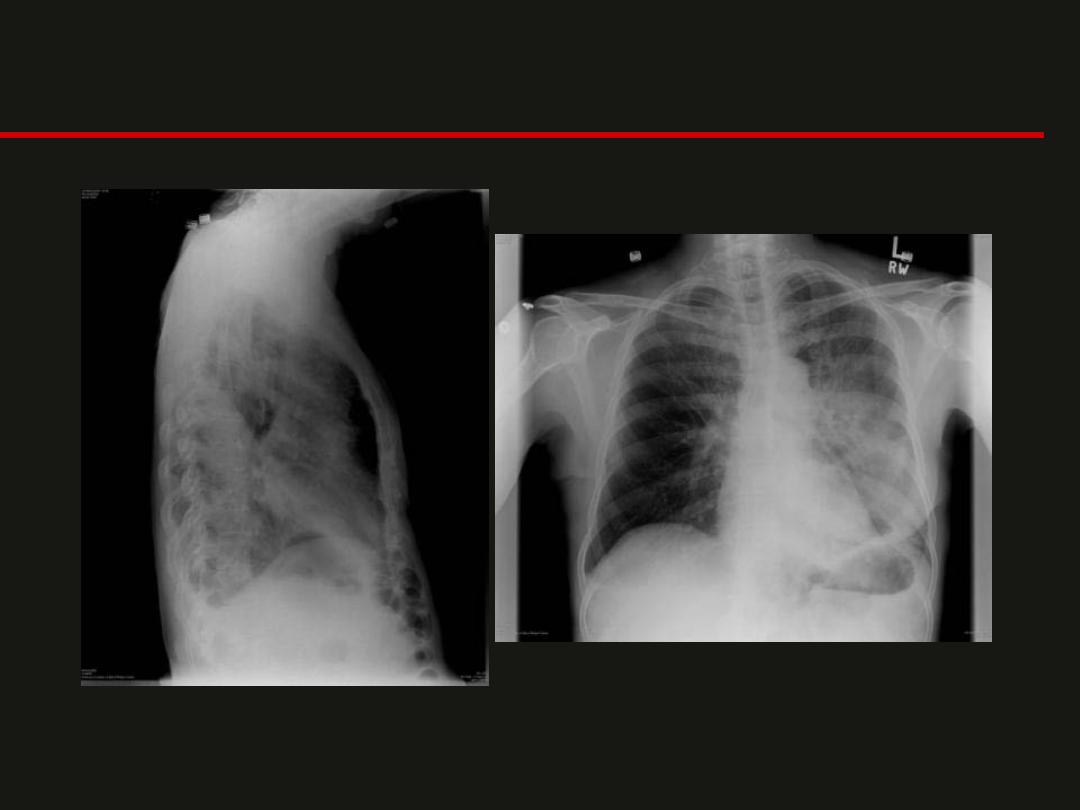
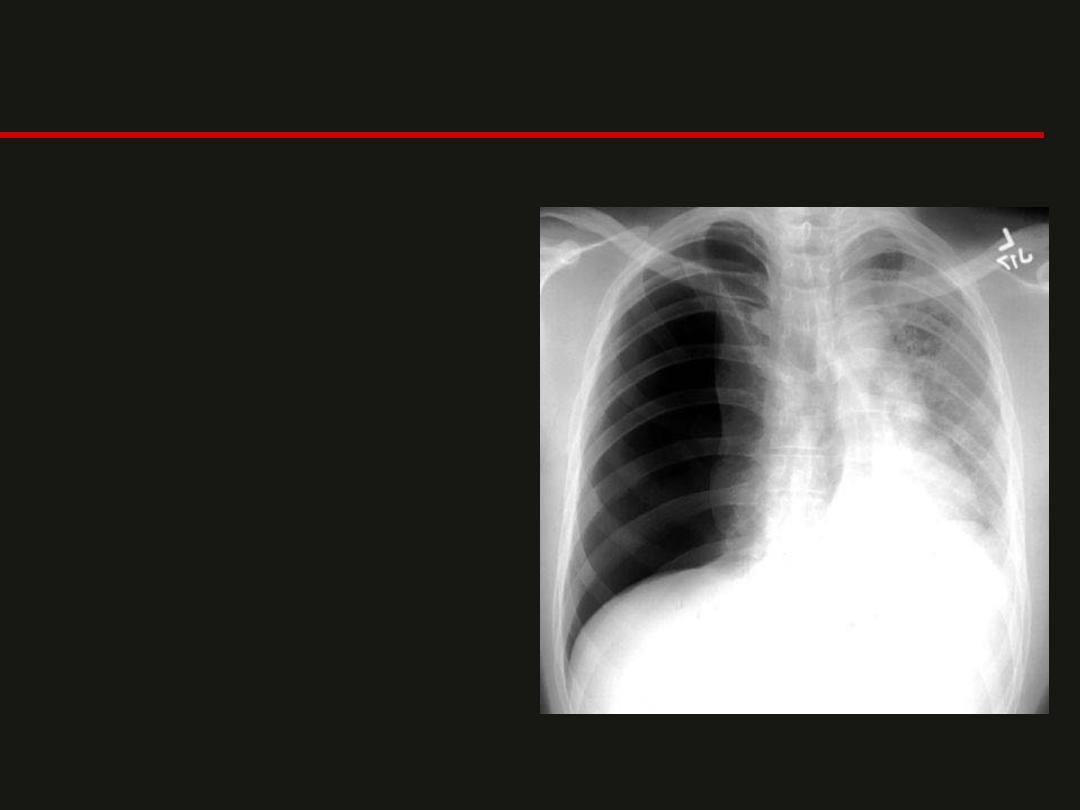
Pleural Effusion
• Upright film,
– will cause blunting on
the lateral and if
large enough, the
posterior costophrenic
sulci.
– A large effusion can
lead to a mediastinal
shift away from the
effusion and opacify
the hemithorax.
– Approximately 200 ml
of fluid are needed to
detect an effusion.



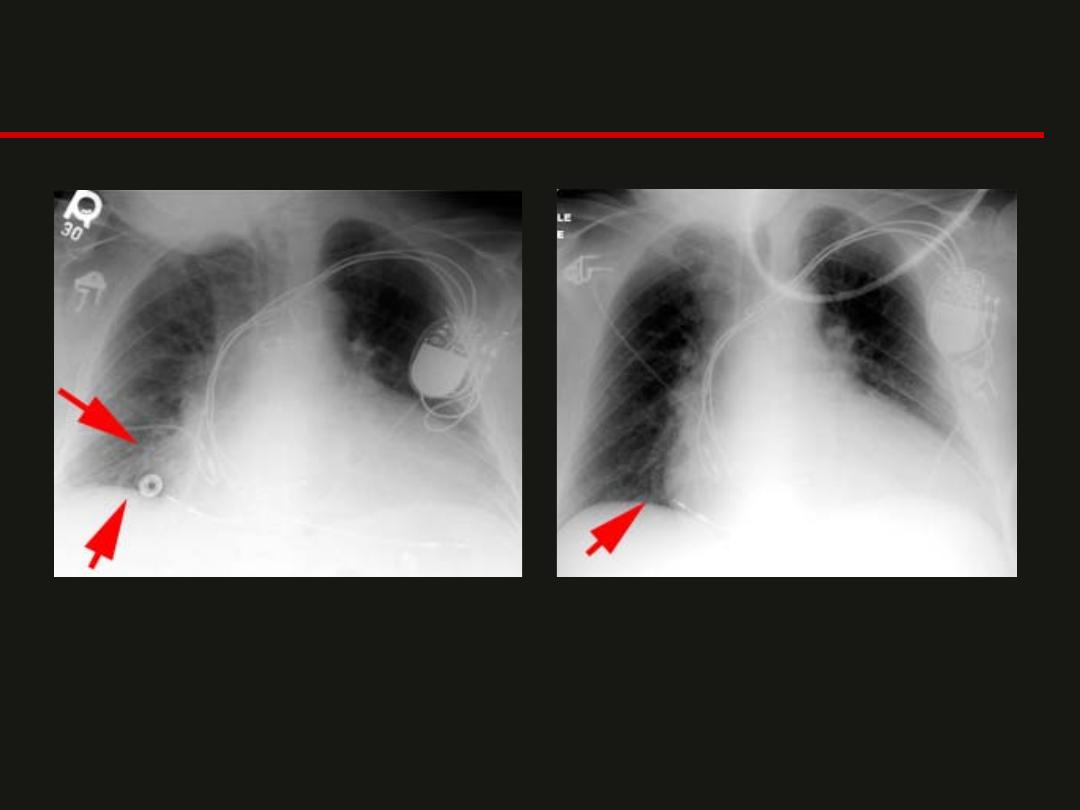
Pleural Effusion

Pericardial Effusion
• An enlarged heart shadow that
is often globular shaped
(transverse diameter is
disproportionately increased).
• Serial films can be helpful in
the diagnosis especially if rapid
changes in the size of the heart
shadow are observed.
• Approximately 400-500 ml of
fluid must be in the pericardium
to lead to a detectable change
in the size of the heart shadow
on PA CXR.
• Pericardial effusion can be
definitively diagnosed with
either echocardiography or CT
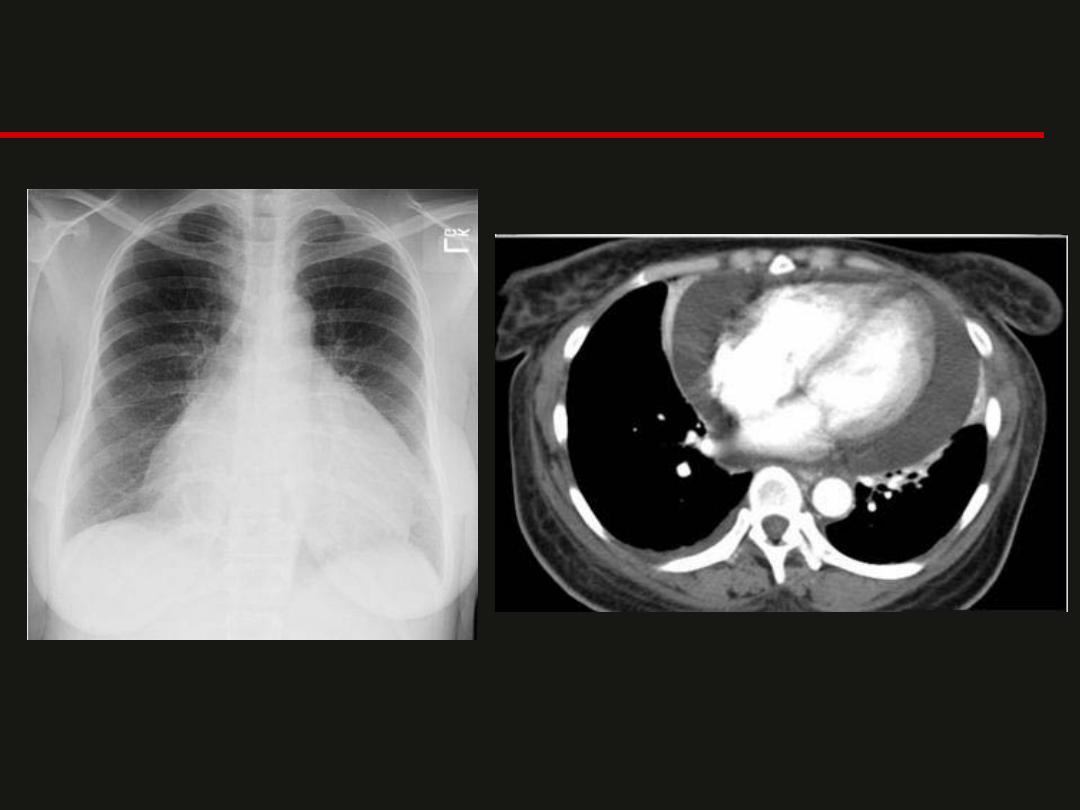
Pericardial Effusion
COPD

COPD / Emphysema

Calcified Granuloma
Tubes, Lines & Catheters
Tubes, Lines & Catheters
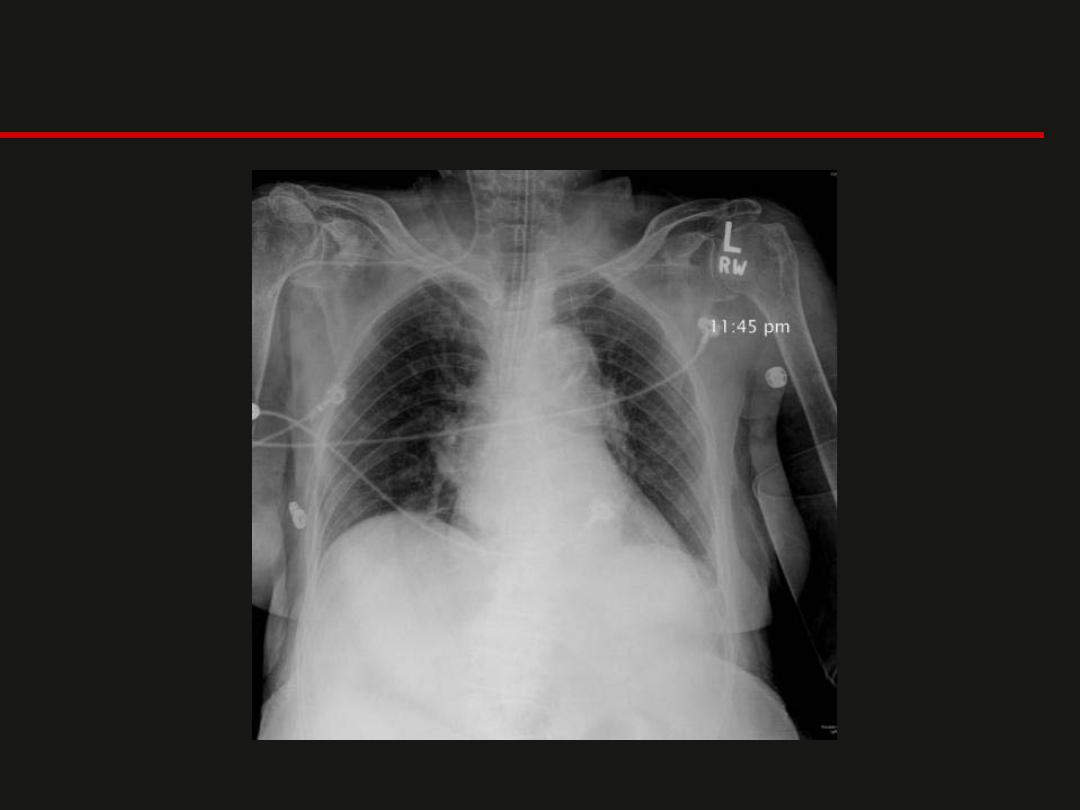
Pneumothorax
• A tension PTX; air enters
the pleural cavity and is
trapped during expiration
usually by some type of
ball valve mechanism. This
leads to increasing intra-
thoracic pressure.
Eventually the pressure
buildup is large enough to
collapse the lung and shift
the mediastinum.
Defined as air inside the
thoracic cavity but
outside the lung.

Mass vs. Infiltrate
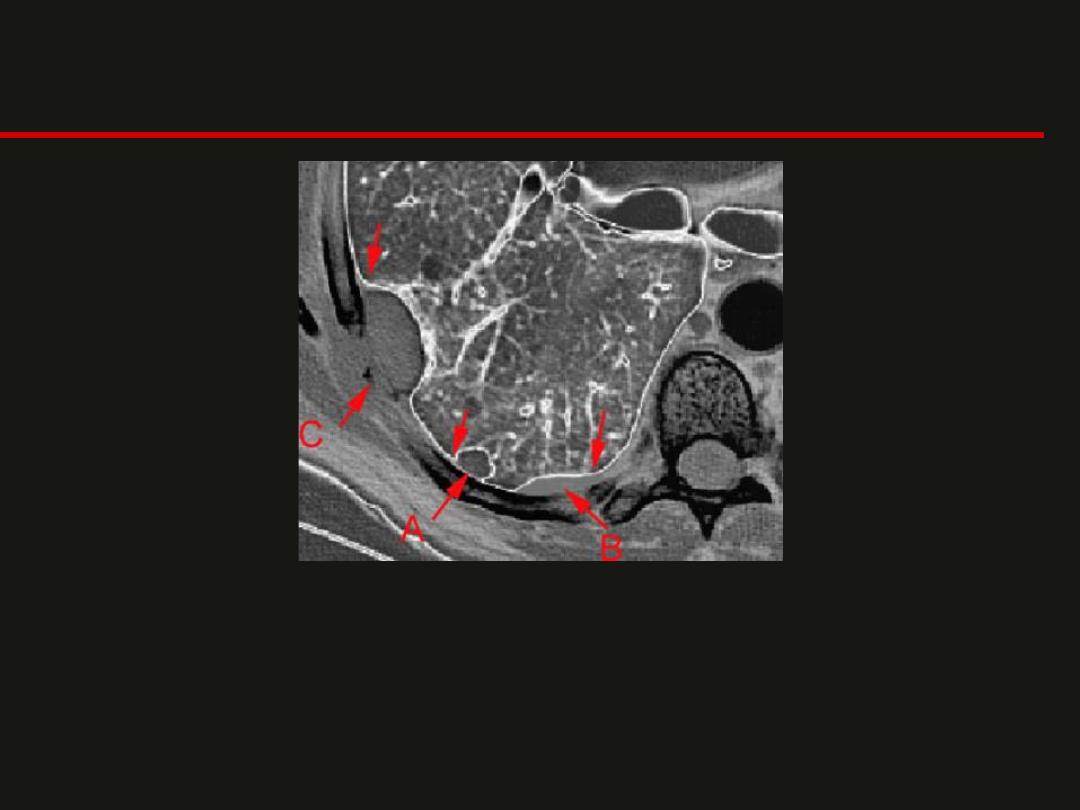
Mass Location
;
Intraparenchymal vs. pleural vs. extrapleural
Three locations that a mass can exist in the thoracic cavity.
A = intraparenchymal
B = pleural
C = extrapleural
Mass Location
;
Intraparenchymal vs. pleural vs. extrapleural

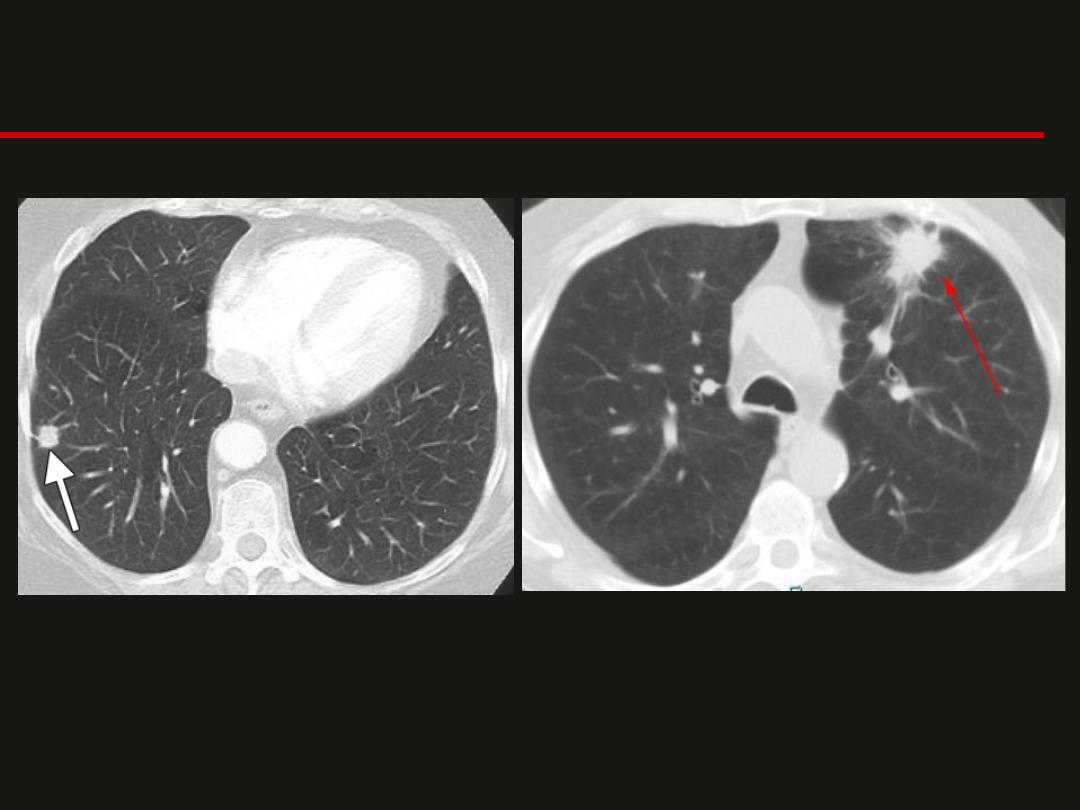
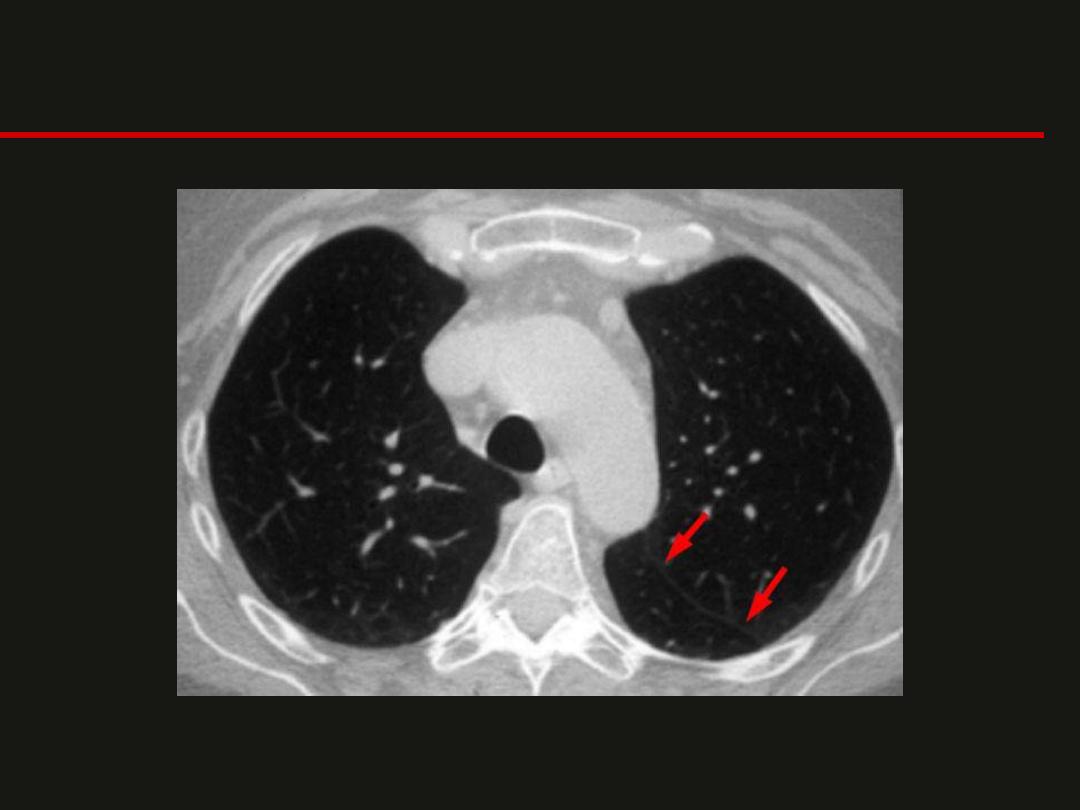
Sub-centemetric Nodules
• Low Risk Patient
– ≤4mm
No follow-up
needed
– 4-6mm
12 mo; if no
change – stop
– 6-8mm
6-12 mo; no
change - follow-up
at 18-24 mo
– > 8mm
CT follow-up
at 3, 9, 24mo or
PET/CT, or biopsy
• High Risk Patient
– ≤ 4mm
12 mo; if no
change – stop
– 4-6mm
6-12mo; no
change - follow-up at
18-24 mo
– 6-8mm
3-6mo; no
change - follow-up at
18-24 mo
– > 8mm
CT follow-up
at 3, 9, 24mo or
PET/CT, or biopsy
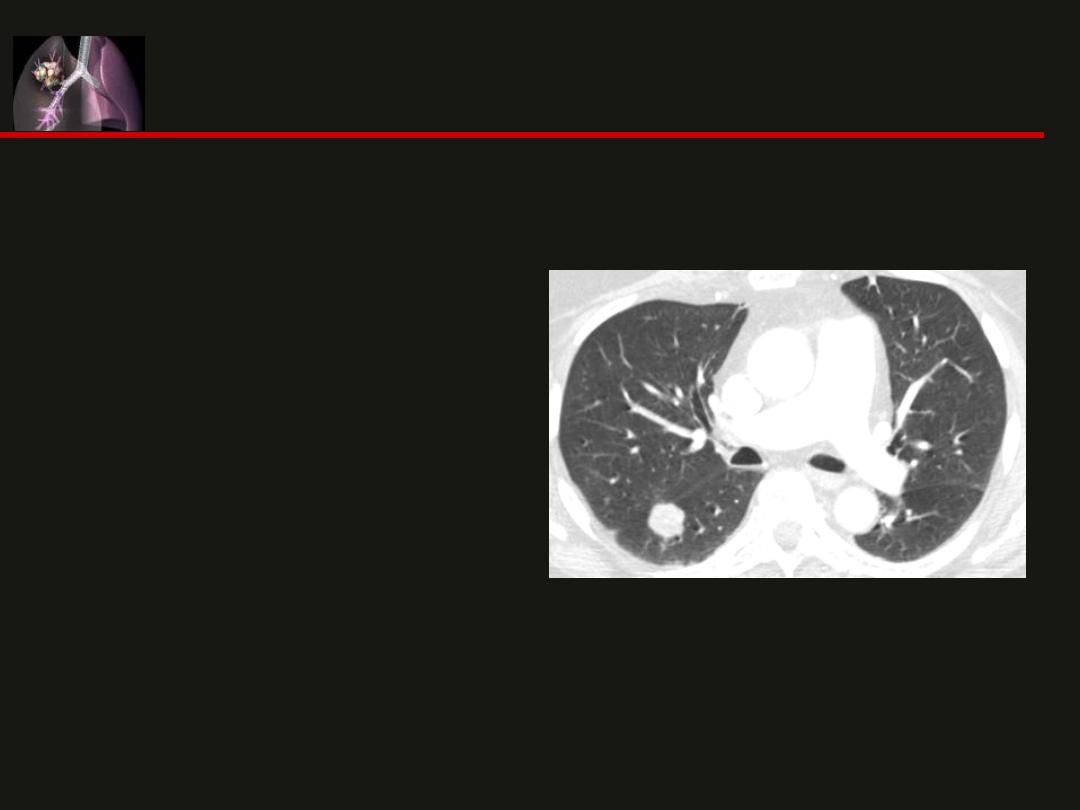
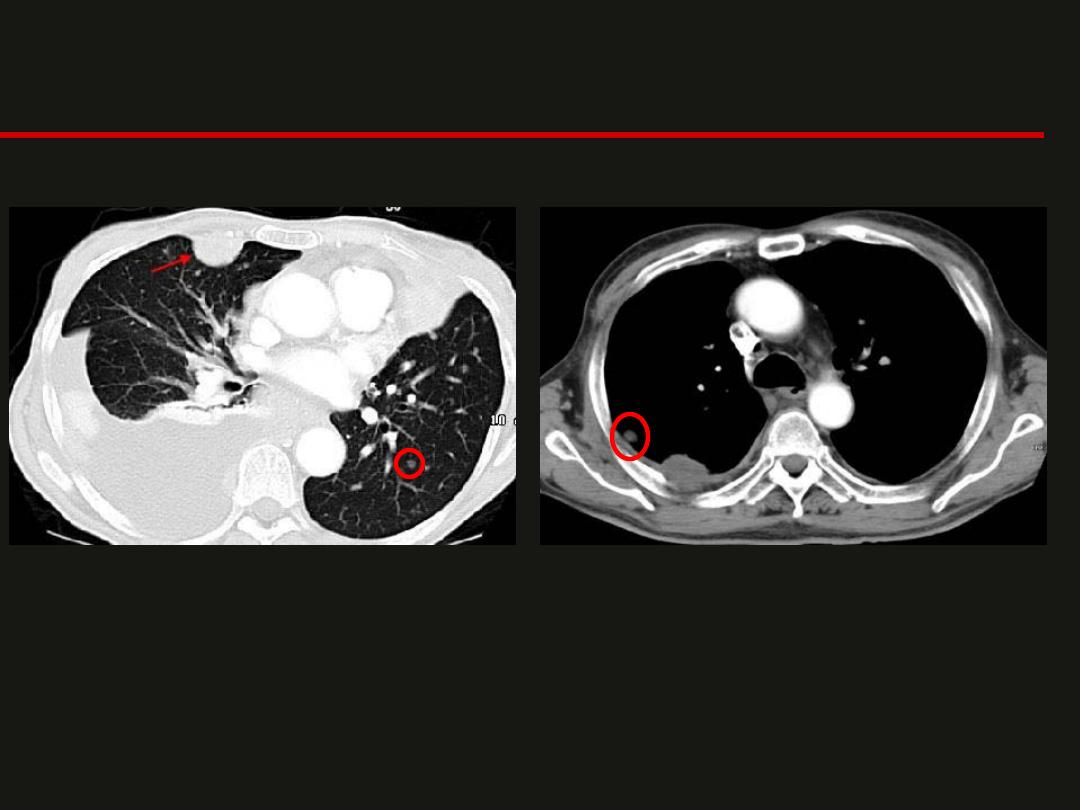
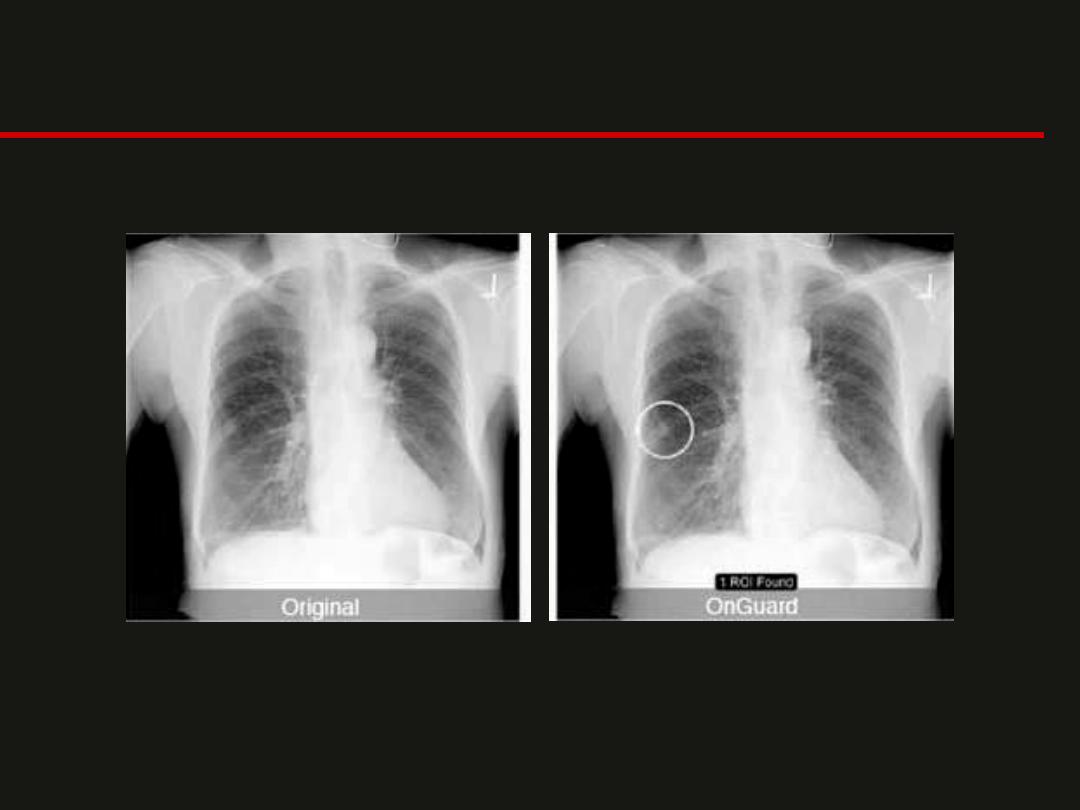
Solitary Pulmonary Nodule
• A common finding on a
chest x-ray.
• Most nodules are benign
• Nodules are diagnosed
as benign if they
– Show little or no growth
for 2 years
– Calcification
• Central, laminated or
diffuse pattern indicates
a granuloma
• Eccentric calcification can
be seen in a carcinoma or
in a cancer that has
engulfed a granuloma.

Hiatal Hernia
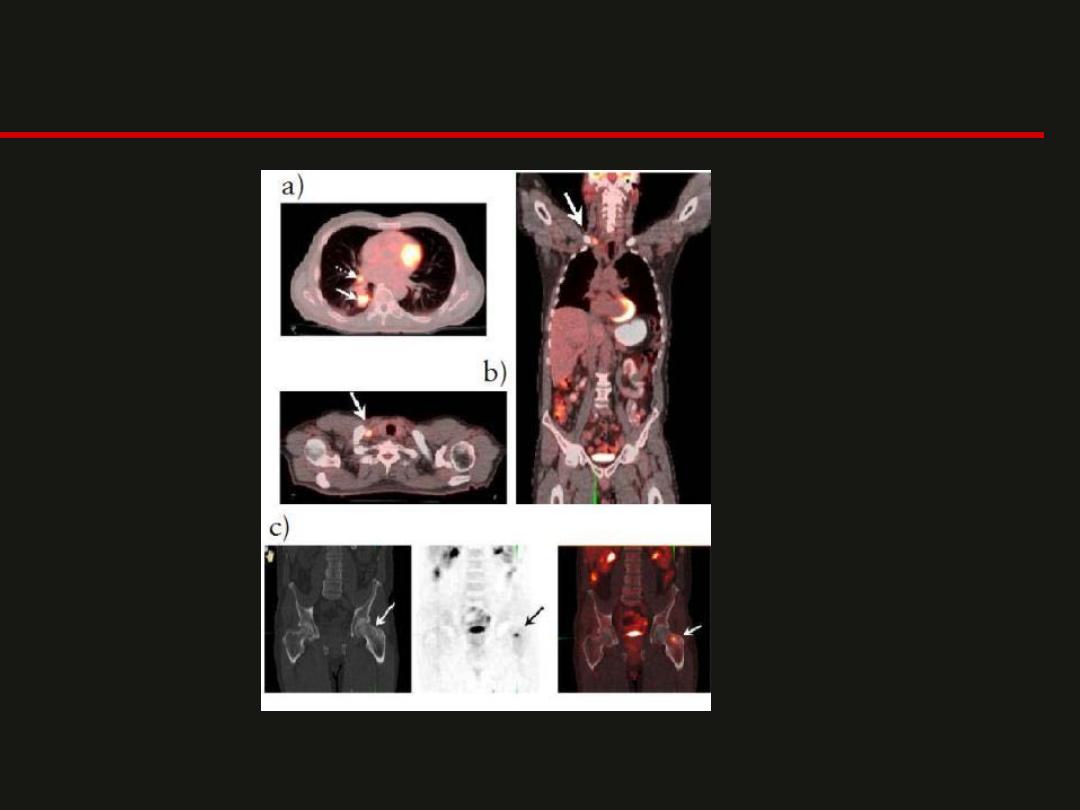
PET/CT
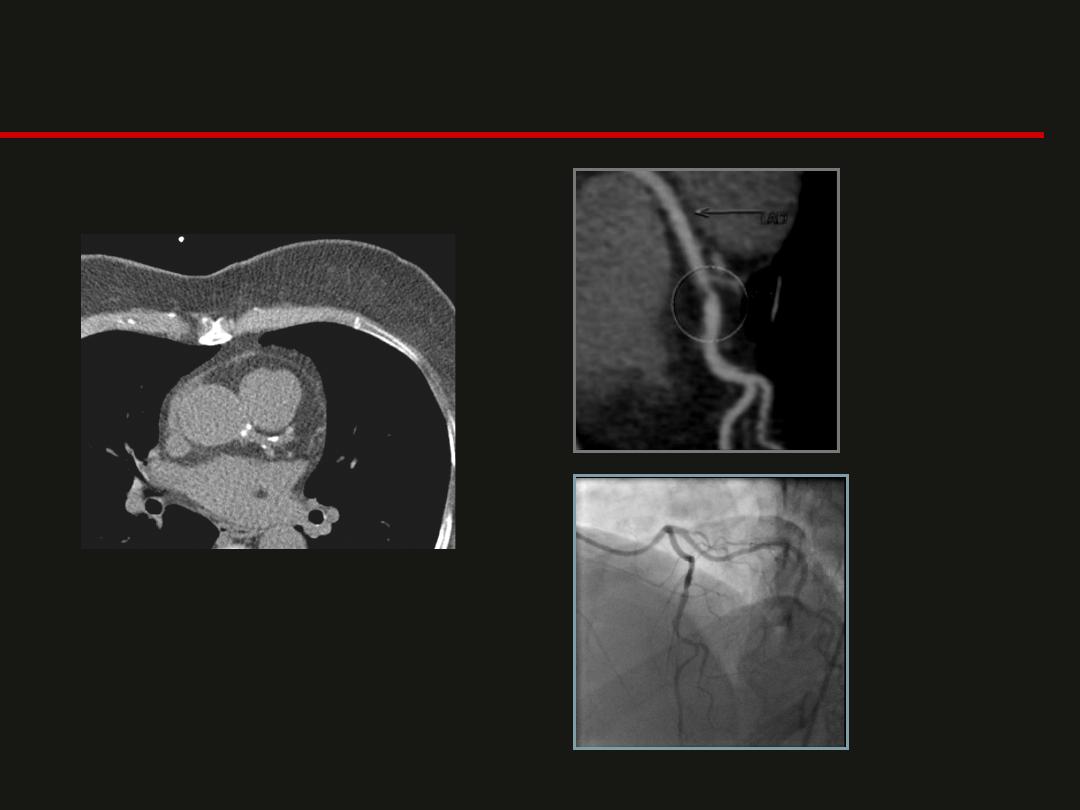
CT Calcium Score & CT Coronary Angiography
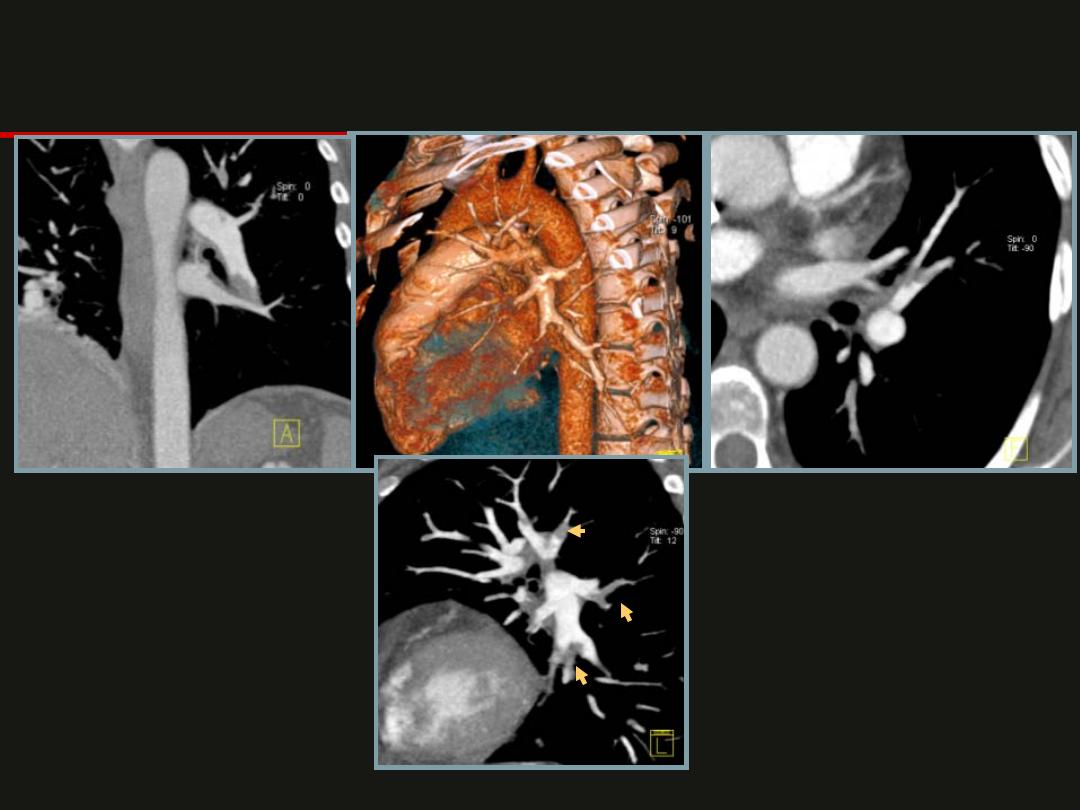
Pulmonary Emboli

Aortic Aneurysm
CAD
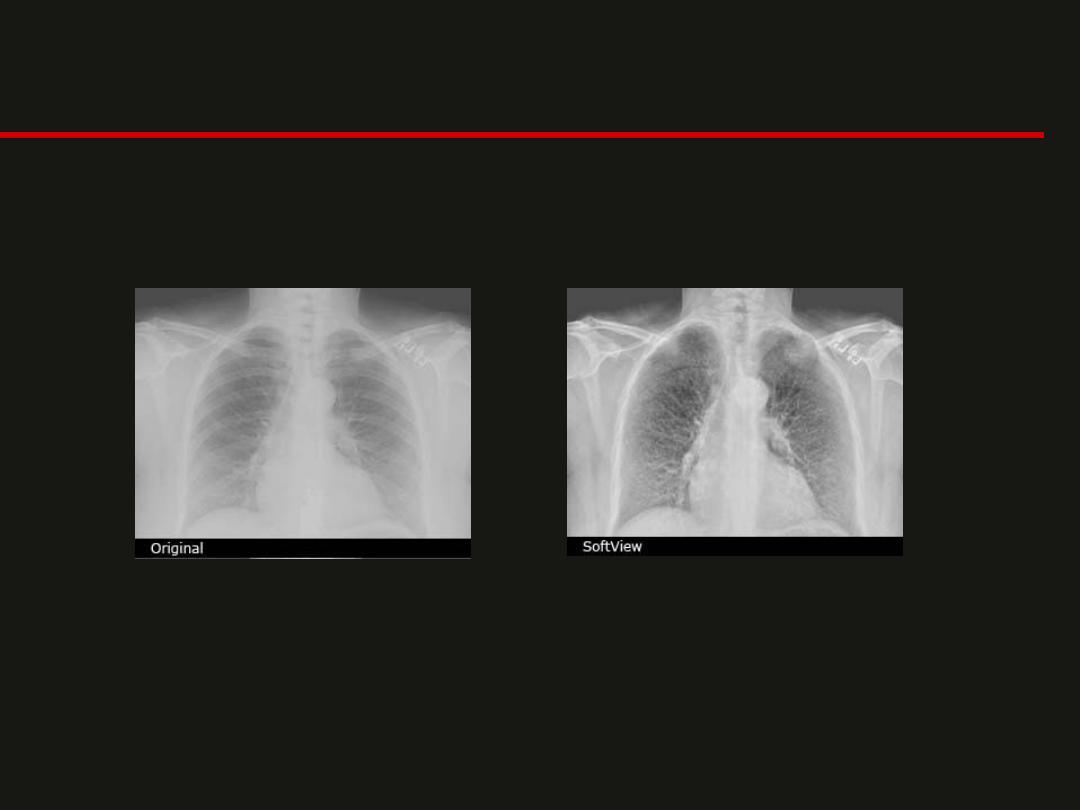
New Developments

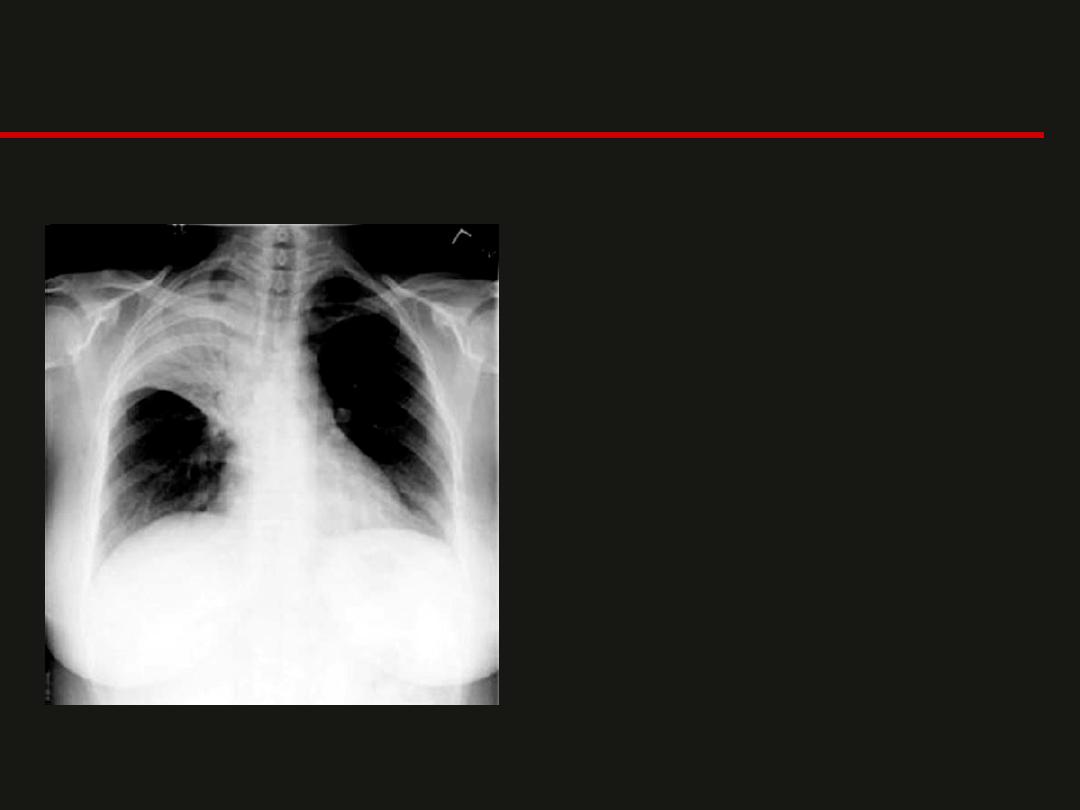
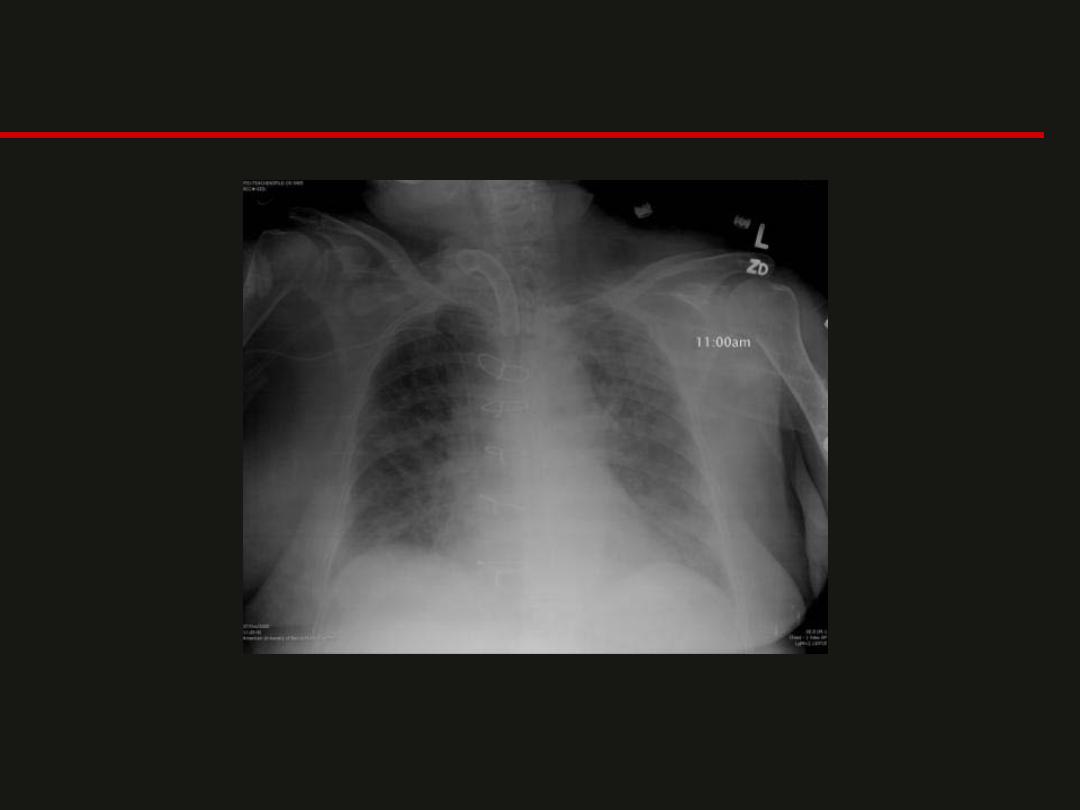
- This is a chest x-ray of an
adult female patient.
- The silhouette of the right
upper Mediastinum is lost
and the consolidation is
confined inferiorly by the
horizontal fissure.
- Within the consolidation air
bronchograms are evident.
- There is consolidation of the
right upper lobe
- In a patient of age 56, the presence of an
upper lobe collapse should alert one to the
possibility of an endobronchial neoplasm.
- An endobronchial malignancy may be the
underlying cause for an upper lobe collapse or
an upper lobe pneumonia which fails to resolve
with treatment.
- referral for bronchoscopy is advised
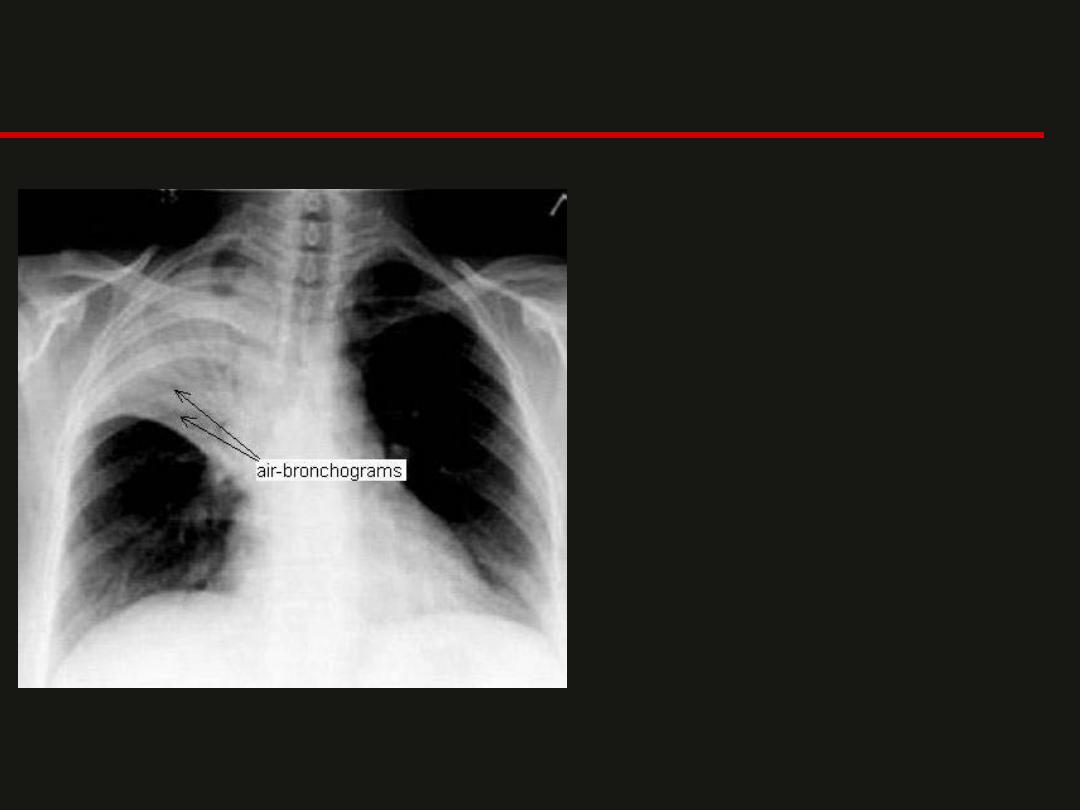
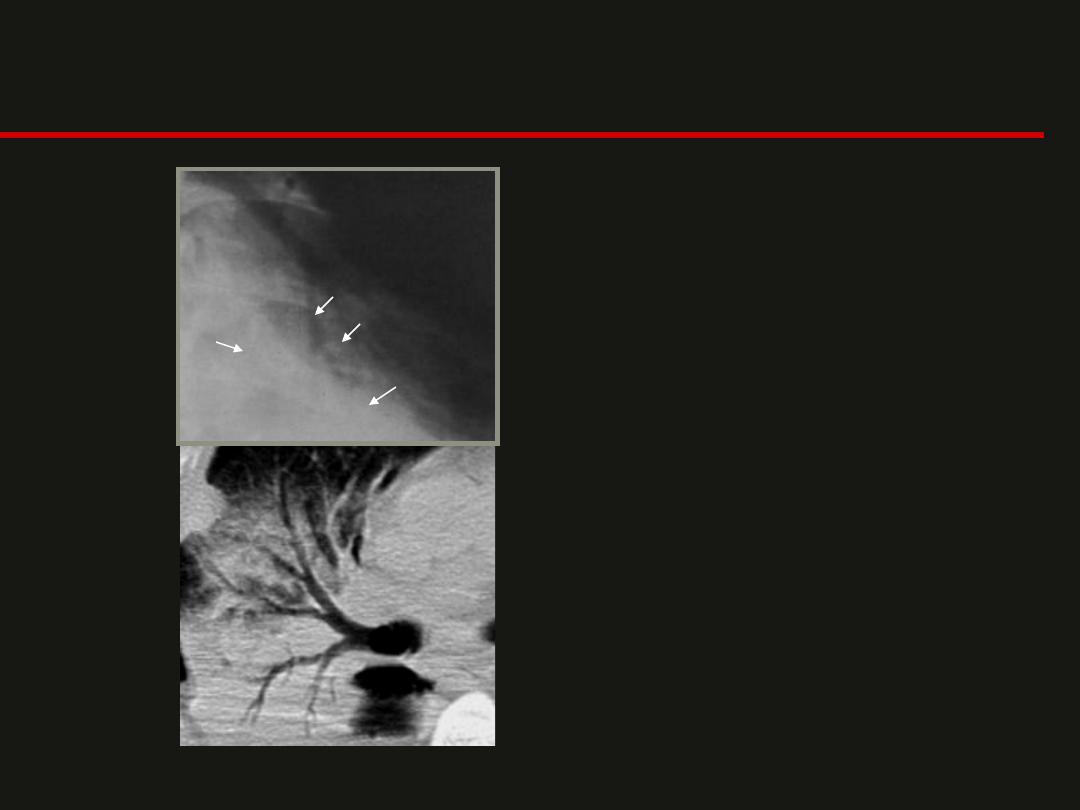
Air Bronchogram
Air bronchograms are due
to the air within bronchi
surrounded by
consolidated lung. These
smaller bronchi are not
normally delineated from
the lung, but due to
consolidation a contrast
difference occurs. They
are not always present,
but when they are they
suggest consolidation
(usually infection) in the
lung.
•
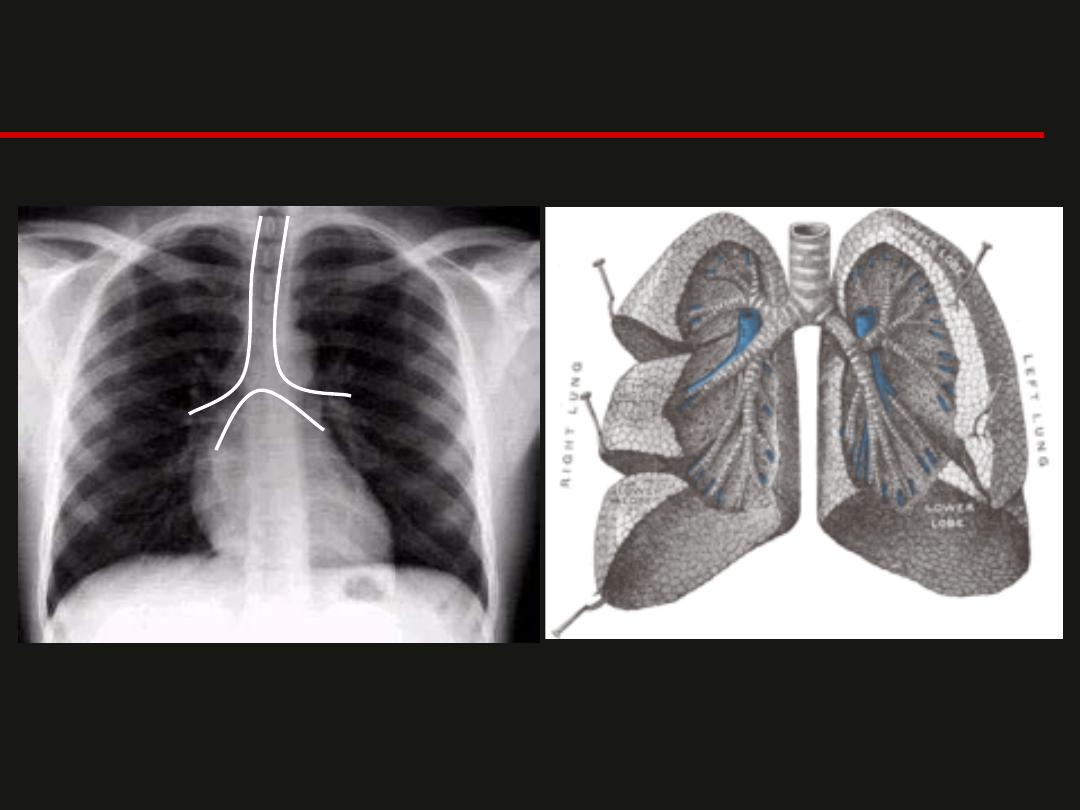
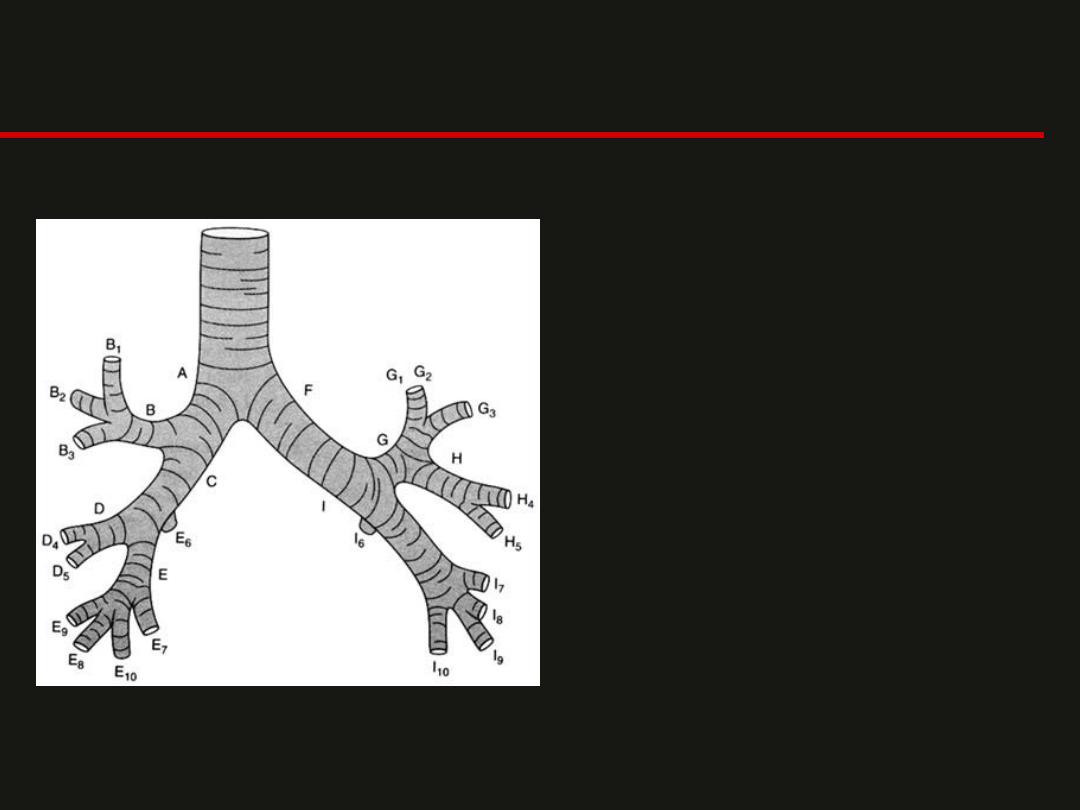
A = Right Main Stem Bronchus
B = Right Upper Lobe Bronchus
B1 = Apical Segmental Bronchus
B2 = Anterior Segmental Bronchus
B3 = Posterior Segmental Bronchus
C = Bronchus Intermedius
D = Right Middle Lobe Bronchus
D4 = Lateral Segmental Bronchus
D5 = Medial Segmental Bronchus
E = Right Lower Lobe Bronchus
E6 = Superior Segmental Bronchus
E7 = Medial Basal Segmental Bronchus
E8 = Anterior Basal Segmental Bronchus
E9 = Lateral Basal Segmental Bronchus
E10 = Posterior Basal Segmental Bronchus
F = Left Main Stem Bronchus
G = Left Upper Lobe Bronchus
G1, G2 = Apicoposterior Segmental Bronchus
G3 = Anterior Segmental Bronchus
H = Lingular Bronchus
H4 = Superior Lingular Segmental Bronchus
H5 = Inferior Lingular Segmental Bronchus
I = Left Lower Lobe Bronchus
I6 = Superior Segmental Bronchus
I7 = Medial Basal Segmental Bronchus
I8 = Anterior Basal Segmental Bronchus
I9 = Lateral Basal Segmental Bronchus
I10 = Posterior Basal Segmental Bronchus
Lobes and Fissures
