OSCE stations in Obstetrics and Gynecology
Q. Take a focused history form infertile couples?
Answer:
1. Age of both partners
2. Occupation of both partners
3. If they previously had children
4. Duration of infertility since marriage or last child born.
5. Sexual history: Frequency of intercourse, pain during intercourse, any
method of contraception previously used
6. Mesntrual cycle history: Menarche, regularity, duration of cycle and
menses, menorrhagia, dysmenorrhea
7. PCOS history: Oligo/amenorrhoea, hirsutism, obesity, diabetes
8. Past medical history: Hypothyroidism, hyperprolactinemia, SLE
9. Past surgical history: Abdominal surgery
10.
Past obstetrical: Previous abortion, Previous post partum
hemorrhage
11.
Drug history: Steroids, chemotherapy, radiotherapy
12.
Family history of infertility
13. Smoking
Q. A 27 year old lady with monochorionic monochorionic twin
pregnancy, what are the complications that may occur in pregnancy?
What is the mode of delivery?
Answer:
1. Miscarriage and severe preterm delivery
2. Increased perinatal mortality in twins
3. Death of one fetus in a twin pregnancy
4. Fetal growth restriction
5. Fetal abnormalities
6. Chromosomal defects and twinning
7. Twin to twin transfusion syndrome (unique to monochorionic twins)
8. Cord acciedents (unique to monoamniotic twins)
Mode of delivery is Cesarean section
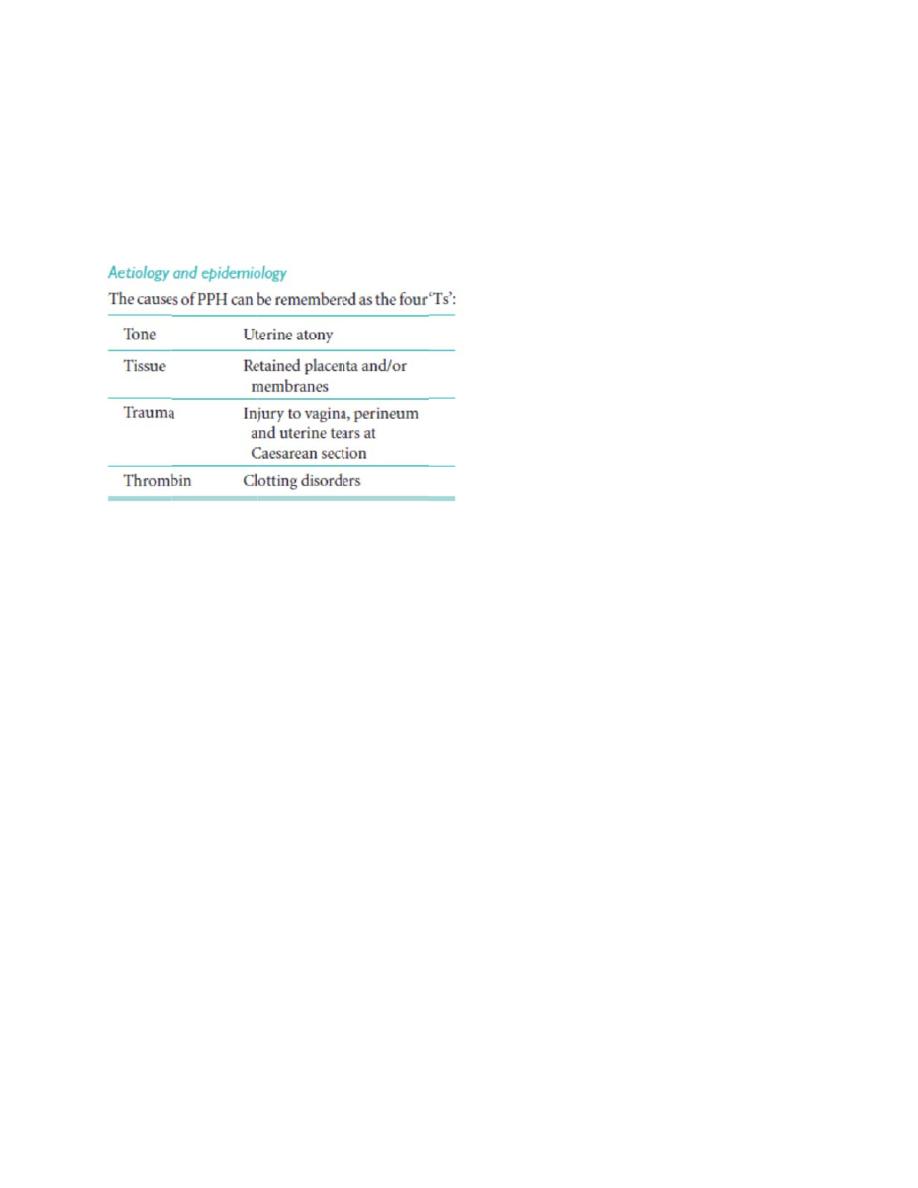
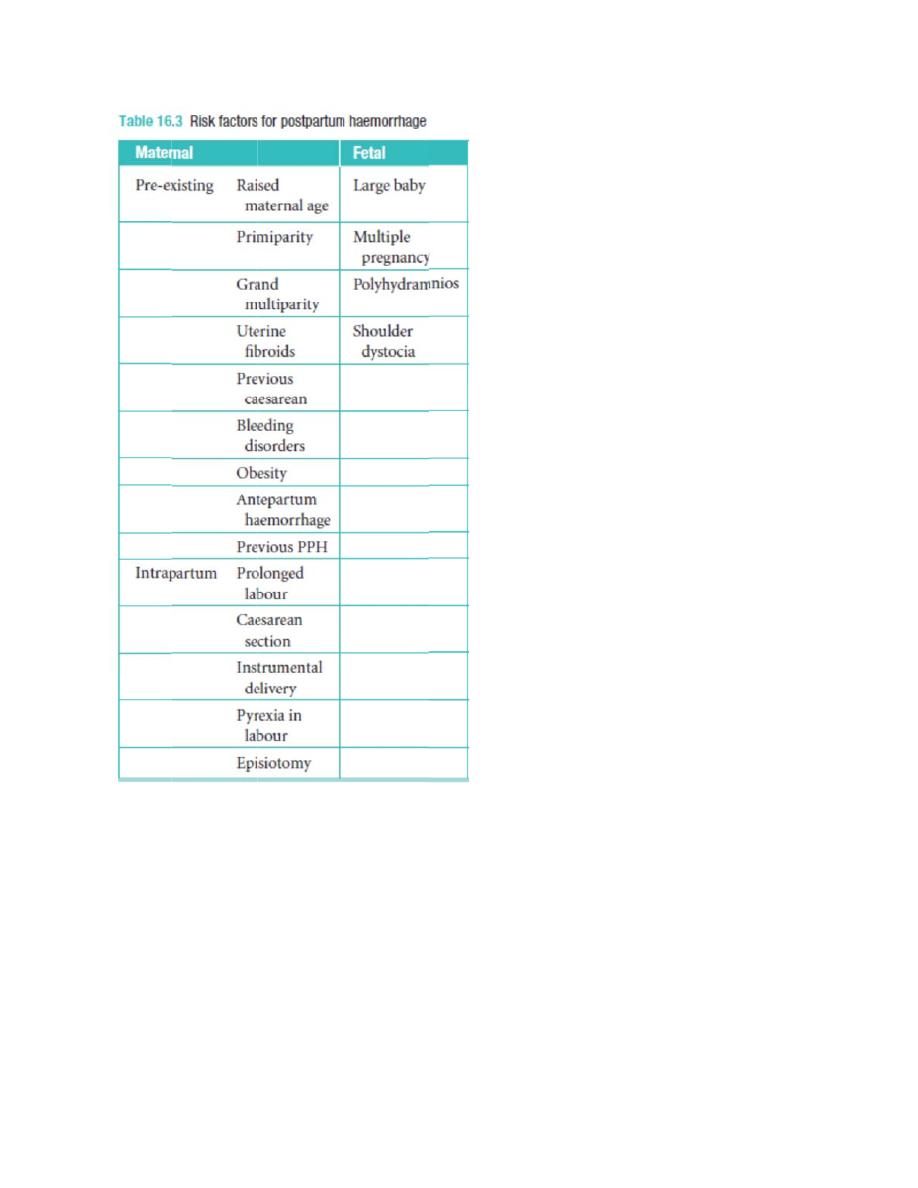
Q. A pregnant lady had hemorrhage after the delivery of her baby?
What is the diagnosis?
- Give
- Give
- Give
Answe
Diagno
3 causes
3 immed
3 further
er:
osis is prim
s
iate steps
r steps in
mary post
s in mana
managem
partum he
agement
ment
emorrhag
e

Assess
Feel th
1. M
2. O
3. In
4. In
5. B
6. R
7. U
8. L
In case
In case
s the level
e pulse fo
Massage
Oxytocin, M
ntrauterin
ntrautrine
B-lynch su
Radiograp
Uterine or
Last resort
e of perine
e of retain
l of the ute
or shock
Methergin
e balloon
packing
uture techn
phic embo
internal il
t is hyster
eal lacerat
ed tissue
erus and
ne
nique
lization
iac artery
rectomy
tion then
then man
feel it
y ligation
suture an
nual remo
nd repair
oval and ccurettage

Q. Fibroid specimen
- What is this? Define it?
- Give 3 presentations
- Give 2 intraoperative complications
- Give 4 complications in pregnancy
- What is the percentage of malignant transformation?
Answer:
A fibroid is a benign tumour of uterine smooth muscle, termed a
‘leiomyoma
Presentations:
1. Asymptomatic
2. Mass
3. Pain
4. Pressure symptoms especially urinary frequency
5. Menorrhagia
6. Infertility
Intraoperative complications:
1. Excessive bleeding
2. Loss of demarcation if previously treated with GnRH agonist
3. Injury to bowel, bladder, ureters, or Fallopian tubes
Complications in pregnancy:
1. Red degeneration
2. Malposition and malprestation
3. IUGR
4. Preterm labour
5. Prolonged labour
6. PPH
7. Placental abruption
Percentage of malignant transformation is 0.5 %
Q. Mention important points in history, investigations, and treatment
of urinary incontinence?
Answer:
History:
1. Age; looking for menopause
2. Parity; NVD or C/S
3. Duration of incontinence

4. Time; at day or night
5. Irritative symptoms: Dysuria, urgency, frequency, polyuria
6. Risk factors: Obesity, Chronic cough, ascites, intrabdominal
malignancy
7. Related to posture, Does it disturb her lifestyle
8. Prolapsed mass, Back pain
9. Past medical hx
10.
Past surgical history; pelvic surgery
11.
Drug hx including radiation
12. Family
history
13. Smoking
Investigations:
1. Midstream urine specimen
2. Urinary diary
3. Pad test
4. Uroflowmetry
5. Cystometry
6. Videocystourethrography
7. Intravenous urography
8. Ultrasound
9. Magnetic resonance imaging
10. Cystourethroscopy
11.
Urethral pressure profilometry
Treatment:
1. Prevention: Shortening the second stage of delivery and reducing
traumatic delivery may result in fewer women developing stress
incontinence
2. Conservative management:
Physiotherapy is the mainstay of the conservative treatment of
stress incontinence. Biofeedback techniques, e.g. perineometry and
weighted cones
3. Surgery:
to provide suburethral support;
•
restoration of the proximal urethra and bladder neck to the zone of intra-
abdominal pressure transmission;
•
to increase urethral resistance;or
a combination of both.
The choice of operation depends on the clinical and urodynamic features of
each patient, and the route of approach.
Options:
1. Colposuspension
2. TVT
3. TOT
Q. A patient collapsed 30 minutes after giving birth. Give 4 DDx and
mention the management of uterine inversion?
Answer:
DDx:
1. PPH
2. Acute uterine inversion
3. Chorioamnionitis
4. Pulmonary embolism
5. Amniotic fluid embolism
6. Shock including hemorrhage, sepsis, anaphylaxis
7. Cardiac causes, e.g.myocardial infarct
8. Intracranial events – bleeds, thrombosis
9. Biochemical causes e.g. hypoglycemia
10. Anesthetic
events
Management of acute uterine inversion:
1.ABC for resuscitation
2. Replacement of uterus quickly.
3. Administer tocolytics (MgSO4, terbutaline) to relax the uterus.
4. Replacement is undertaken (with placenta still attached) by slowly and
steady pushing upwards, hydrostatic pressure (500 cc normal saline + IV
line), or surgically
5. Epidural or spinal anesthesia can be used in the management of acute
inversion when the patient has a stable cardiovascular condition.
6. After replacement, uterine contraction is maintained with an oxytocic.

Q. 60 year old woman with 6 weeks hx of vaginal bleeding. Take
history, examination, and investigations.
Answer:
History:
1. Risk factor for endometrial CA e.g. nulliparity, early menarche, late
menopause, impaired glucose tolerance, obesity, unopposed
estrogen therapy, pelvic irradiation
2. Hx of trauma
3. Past medical history: Bleeding disorder, hypertension
4. Previous gynecologic surgery
5. Drug hx: Tamoxifen, warfarin, HRT
6. Family hx of uterine, ovarian, and cervical CA
Examination:
1. General examination:
General look, BMI looking for obesity, wasting (cachexic), pallor, vital
signs,
2. Abdominal examination:
Looking for masses
3. Pelvic speculum examination and pap smear
Investigations:
1. U/S to assess endometrial thickness
2. Endometrial biopsy
3. Hysteroscopy
4. D & C
5. CBC, blood film, and ESR
Q. COCP?Types, mechanism of action, and side effects:
Answer:
Types:
Most COC contains progestogens that are classed as second or third
generation. Second generation pills contain derivatives of norethindrone
and levonorgestrel. The third generation pills include desogestrel,
gestodene and norgestimate. Pills containing the newer progestogens,
drospirenone and dienogest, are also available in the UK

Mechanism of action:
1. Inhibtion of ovulation
2. Alteration of tubal motility
3. Endometrial atrophy and impaired uterine receptivity
4. Changes in cervical mucus interfering with sperm transport.
Advantages:
1. Menstrual cycle becomes more regular and menstrual blood is lighter
and shorter
2. Less dysmenorrhea and less PMS
3. Decreased incidence of Iron deficiency anemia
4. Decreased incidence of functional ovarian cysts, endometriosis,
acne, and PID
5. Decreased incidence of benign breast lumps
6. Protect against endometrial and ovarian CA
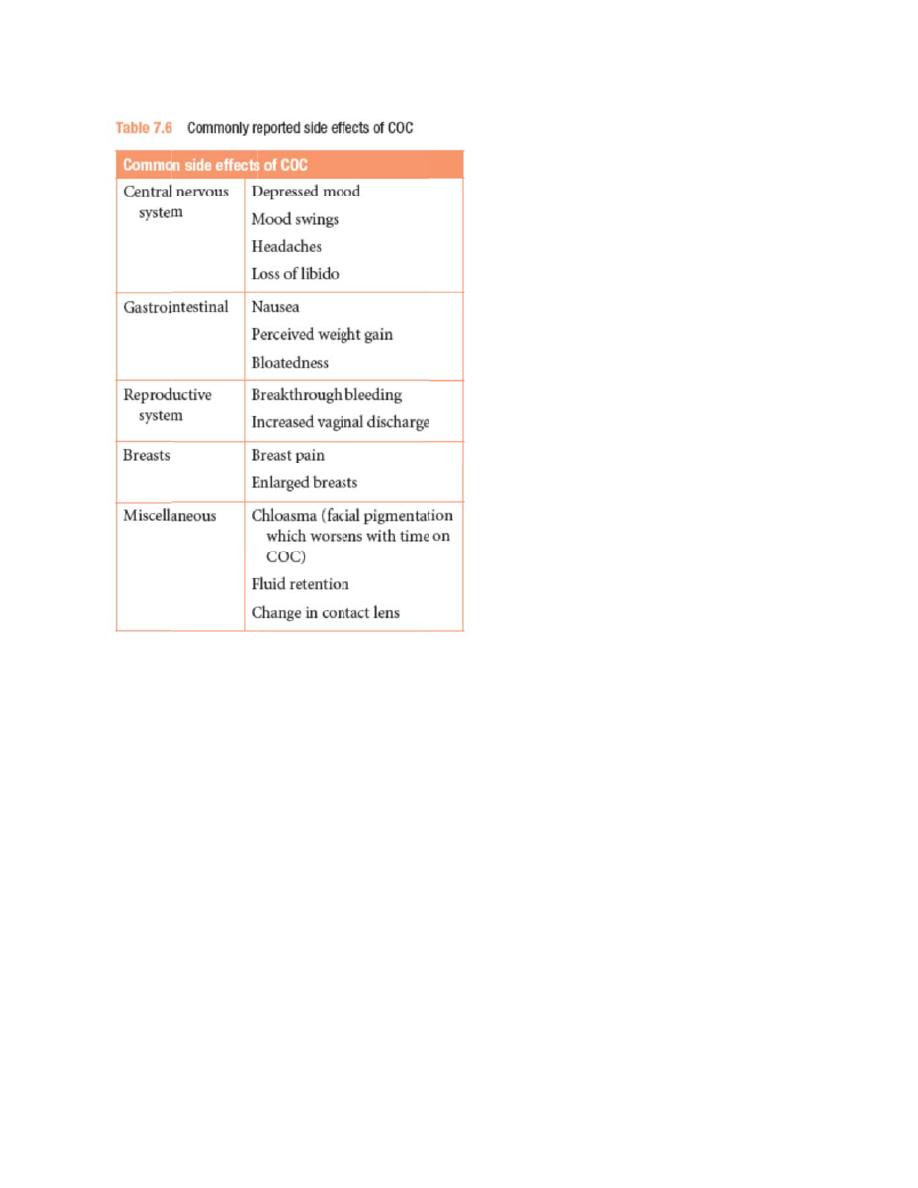
Side effects:
Contra
Absolu
1. IH
2. A
3. A
4. P
5. F
6. E
7. U
Relativ
1. G
2. L
3. D
indication
te:
HD, CVA,
Arterial or
Acute or s
Pregnancy
Focal migr
Estrogen d
Undiagnos
ve:
Generalize
Long term
DM, obesit
ns:
significan
venous th
evere live
y
raine
dependen
sed genita
ed migrain
immobiliz
ty, and he
nt hyperte
hrombosis
er disease
nt neoplas
al tract ble
ne
zation
eavy smok
ension, pu
s
e, hyperlip
sm e.g. Br
eeding
king
ulmonary
pidemia
reast CA
hypertenssion
Q. Sim
examin
Answe
Sim’s s
1. D
2. D
3. R
4. G
5. T
ms specul
nation
r:
speculum:
D & C
D & E
Routine ex
Genital tra
Taking bio
um and C
: Left later
xamination
act prolaps
opsy from
Cusco’s s
ral positio
n
se and inc
the genita
speculum
on (Sim’s p
continenc
al tract
m. Uses a
position)
e (need fu
and the p
ull bladde
osition o
er)
of
Cusco’s bivalve speculum: Dorsal and lithotomy position
1. Taking biopsy from the cervix
2. IUCD insertion
3. Routine examination
Q. Regarding oxytocin, what is the mechanism of action, which
endogenous organ secrete it, on which muscles it work, what are the
indications, S/Es and contraindication? What is the trade name?
Answer:
Oxytocin is a neurohypophyseal hormone that is synthesized by the
hypothalamus and secreted through the posterior pituitary.
It acts on the myometrium causing uterine contractions and inducing labor
It acts on the breast myoepithelial cells causing milk ejection
Indications:
1. Active Mx of 3
rd
stage of labor
2. Induction of labor
3. PPH
4. Incomplete or missed miscarriage
5. After molar pregnancy
Side effects:
1. Uterine rupture
2. PPH
3. Water intoxication and fluid overload
4. Fetal distress
Contraindications:
1. CPD
2. Previous classical uterine scar
3. Fetal distress
4. Abnormal presentation (brow or shoulder)
Trade names: Pitocin, syntocinon
Q. P
use
man
diag
Answ
Invs
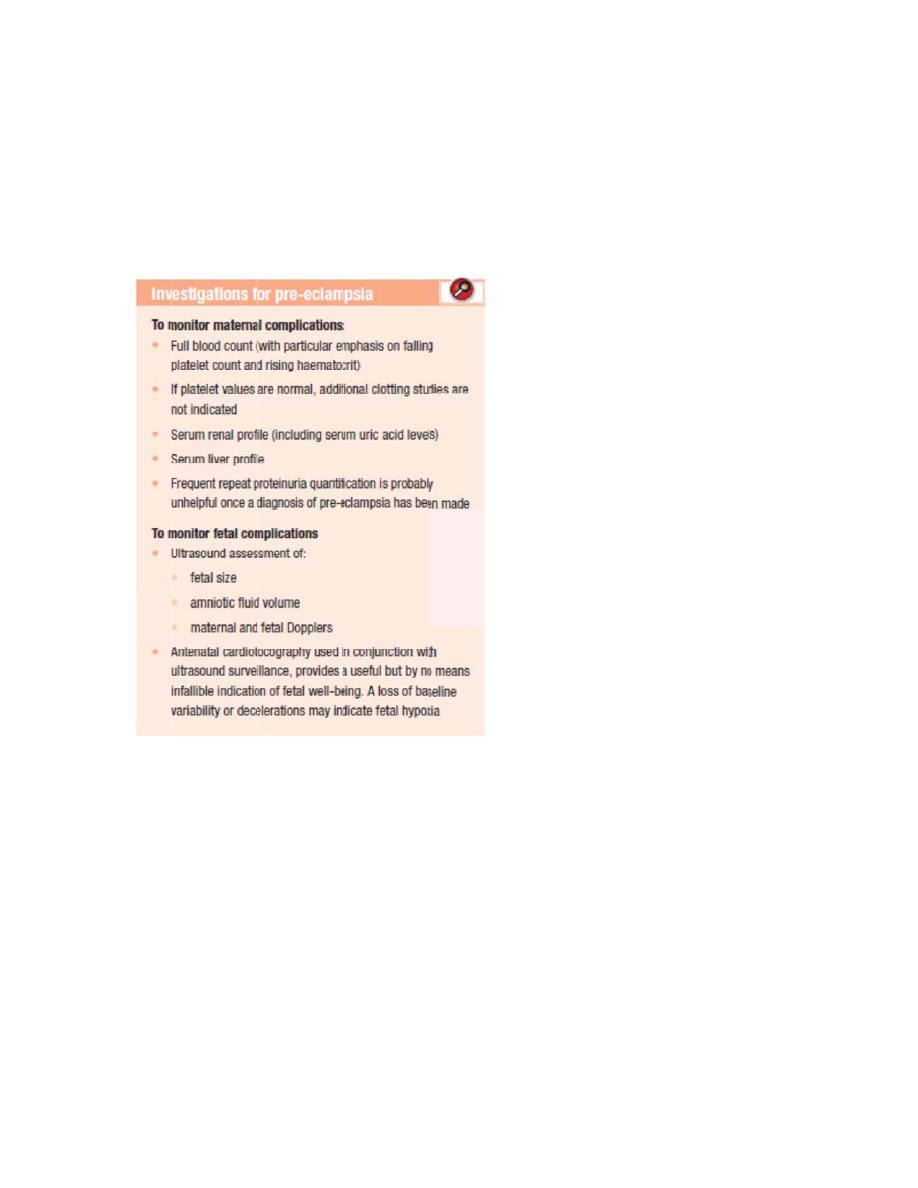
Pre-eclam
fulness?
ny metho
gnose pre
wer:
setigations
mpsia? Gi
Every ho
ods for me
e-eclamp
s:
ive 3 inve
ow long y
easuring
psia?
estigation
you meas
the bloo
ns and m
ure the b
od pressu
mention th
blood pre
ure? How
heir
essure? H
w you
How
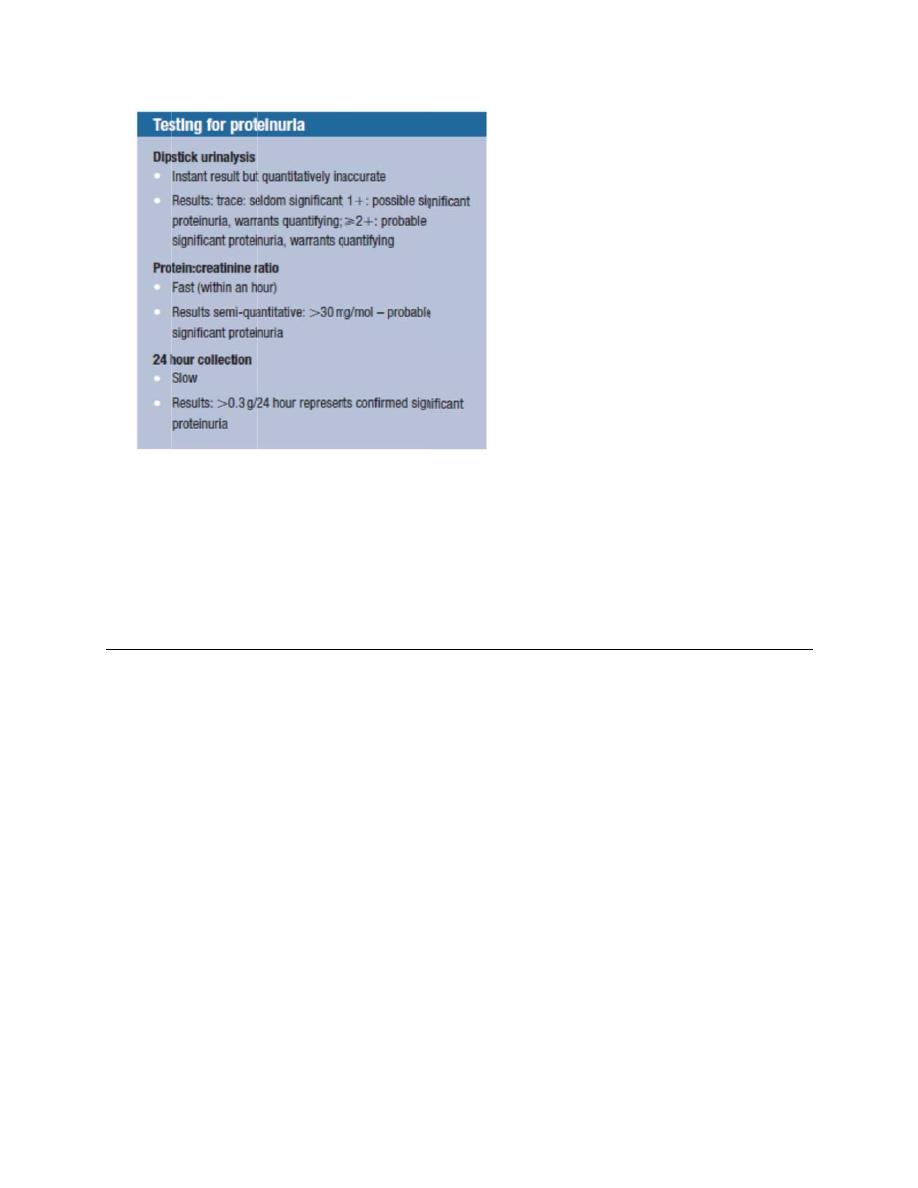
Bloo
pre-e
recorde
in the p
arising
normot
week.
Q. Nam
the ute
manag
Answe
Suppor
1. L
2. L
p
3. P
a
Risk fa
1. C
2. C
3. A
od pressu
eclampsia
ed on at le
presence
de
novo a
tensive wo
me the pr
erus to th
gement?
r:
rt structur
Ligaments
Levator an
position;
Posterior a
abdominal
ctors:
Congenita
Childbirth
Ageing
re should
a is define
east two s
of at least
after the 2
oman and
rolapse?
he pelvis?
res:
s and fasc
ni muscles
angulation
pressure
l
and raise
be meas
ed a
s hyp
separate o
t 300 mg
20th week
d resolving
Give the
? Give 3 r
cia, by sus
s, by cons
n of the va
e causing
d intrabdo
sured ever
pertension
occasions
protein in
k of pregn
g complet
names o
risk facto
spension f
stricting an
agina, whi
closure o
ominal pre
ry 15 minu
n of at leas
s and at le
n a 24 hou
nancy in a
tely by the
of the liga
ors? Wha
from the p
nd thereb
ich is enh
of the ‘flap
essure
utes
st 140/90
east 4 hou
ur collectio
a previous
e sixth po
aments th
at is the
pelvic side
by maintai
hanced by
p valve’.
mmHg
urs apart a
on of urine
sly
stpartum
hat suppo
e walls;
ning orga
y rises in
and
e,
ort
an

4. Pregnancy and menopause
5. Postoperative
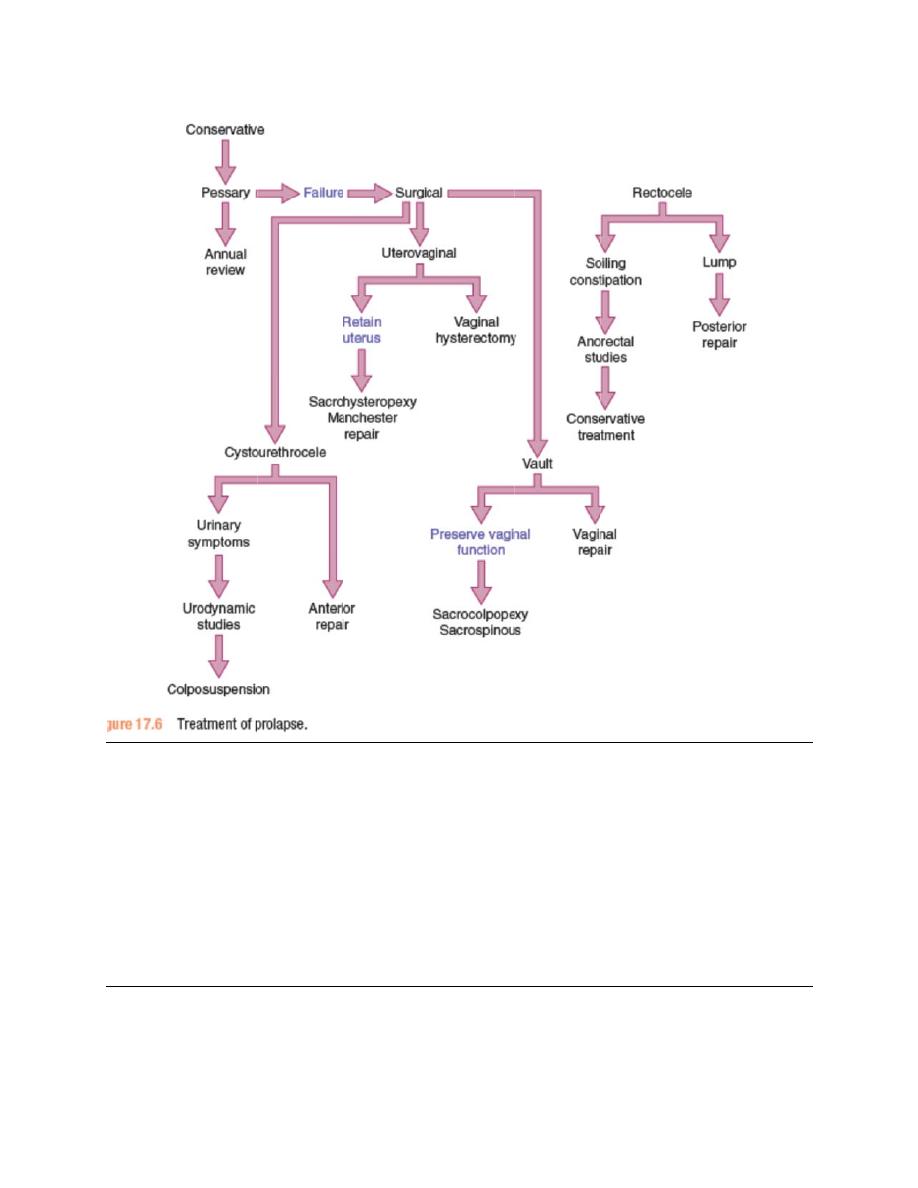
Management:
Medical Rx:
Prior to specific treatment, attempts should be made to correct obesity,
chronic cough or constipation. If the prolapse is ulcerated, a 7-day
course of topical oestrogen should be administered.
For prevention: Shortening the second stage of delivery and reducing
traumatic delivery may result in fewer women developing a prolapse.
Specific Rx:
1. Pelvic floor physiotherapy
2. Silicon rubber-based ring pessaries
Surgical Rx:
Q. Defi
Answe
Presen
canal o
Positio
part to
position
ine posit
r:
ntation: Po
or in close
n: Relatio
the right o
n.
ion and p
ortion of th
est proxim
onship of a
or left side
presentat
he fetal bo
mity to it. N
an arbitra
e of the b
tion
ody that is
Normal pre
rily chose
irth canal
s either fo
esentation
en portion
. Normal:
oremost w
n: cephalic
of the fet
Occiput a
within the b
c
tal presen
anterior
birth
ting
Q. IUCD.. What is this? Other types? Mechanism of action?
Complication? Contraindications
?
Answer:
This is Copper bearing IUCD
Other types:
1. Plastic inert devices such as Lippes loop
2. Hormone-releasing IUS such as levonorgestrel-releasing IUS
(mirena)
Mechanism of action:
All IUCDs induce an inflammatory response in the endometrium that
prevent implantation, Cu-bearing IUCD has a toxic effect on sperm that
prevent fertilization, Hormone releasing IUS prevent pregnancy by a local
hormone effect on CX mucous & endometrium.
Complications:
1. Increased menstrual blood loss
2. Increased dysmenorrhea
3. Increased risk of pelvic infection following insertion
4. Perforation
5. Expulsion
6. Ectopic pregnancy
Contraindications:
1. Previous PID.
2. Previous ectopic pregnancy.
3. Known malformations of uterus.
4. Copper allergy.
5. Endometrial and cervical CA
6. Malignant trophoblastic disease
Q. Mention 4 DDx for large for date baby? How to differentiate
between them?
Answer:
1. Wrong date:
2. Macrosomic baby: Suggested by diabetic mother. Confrim by U/S
3. Multiple pregnancy: Family hx of twins. Confirm by U/S
4. Polyhydramnios: Difficult to feel the fetal parts. Confirmed by U/S
5. Fibroids: Risk factors for fibroids. Abnormal lie and presentation.
Confirmed by U/S
6. Molar pregnancy: Risk factors for molar pregnancy. Rapidly enlarging
uterus. Snowstorm appearance on U/S
7. Placental abruption: Antepartum hemorrhage and severe abdominal
pain.
Q. Arey’s spatula and brush uses? Staging and management of CIN?
Answer:
Uses:
1. Collect cells from the ecto and endocervix for pap smear
2. Collect cells from the vaginal wall for vaginal swab
3. HPV typing can be done in liquid based cytology
Staging:
English classification:
1. CIN I: Only the deepest third of the epithelium from the basal layer
2. CIN II: Two thirds of the epithelium
3. CIN III: Affect the full thickness of the epithelium.
American classification:
1. Low grade SIL: CIN I and HPV cellular changes
2. High grade SIL: CIN II and CIN III
Management:
1. CIN I: Repeating the test (Pap smear + Colposcope) every 3-6
months until 1 year because the rate of regression of CIN I is high.
Also give folic acid to increase the integrity of the epithelium.
2. Persisten CIN I for more than 1 year, CIN II, and CIN III:
A. Excisional methods:
LEEP
LASER TZ excision
Cone biopsy
B. Ablative methods:
Electrodiathermy
Cold coagilation
Q. Reccurent miscarriage: Investigations? DDx? Uterine causes?
Management?
Answer:
Investigations:
1. Parental karyotype, karyotype of products of conception
2. Antiphospholipid Abs: Anticardiolipin Ab and lupus anticoagulant
3. Screening for thrombophilia and thyroid disease
4. Pelvic U/S to assess the ovarian and uterine appearance
5. Transvaginal U/S to assess the cervical length
6. Hysterosalpingography and hysteroscopy for suspected anomalies
DDx:
1. Ectopic pregnancy
2. Molar pregnancy
Uterine causes:
1. Congenital: Septate, bicornuate, and arcuate uterus
2. Acquired: Fibroids or Asherman’s syndrome, cervical incompetence
especially in the second trimester
Management:
1. Psychological support
2. Treatment of the underlying cause
For uterine abnormalities:
Congenital abnormalities: Metroplasty
Fibroids: Myomectomy
Asherman’s syndrome: Hysteroscopic resection of adhesions
Cervical incompetence: Cervical cerclage
Q. Small for date DDx and complications?
Answer:
DDx:
1. Wrong date
2. Transverse lie
3. Oligohydramnios
4. IUGR
5. Dead fetus
Complications:
1. IUD

2. Early neonatal morbidity and mortality
3. High incidence of mental and physical handicap
4. Congenital abnormalities if the cause is chromosomal abnormality or
congenital infection
5. Adult incidence of both hypertension and diabetes
Q. Case of Turner syndrome? Dx? Karyotype? Investigations? How
gonads look like? What 1 hormone should be given? How to Dx it
during pregnancy?
Answer:
Karyotype: 45XO
Mosaic forms (e.g. 45XO/46XX or 45XO/46XY) and
Partial deletions of an X chromosome.
Dx: Most have typical clinical features including short stature, webbing of
the neck and a wide carrying angle. Associated medical conditions include
coarctation of the aorta, inflammatory bowel disease, sensorineural and
conduction deafness, renal anomalies and endocrine dysfunction, such as
autoimmune thyroid disease. Diagnosis is usually made at birth or in early
childhood from the clinical appearance of the baby or due to short stature
during childhood. However, in about 10 per cent of women, the diagnosis is
not made until adolescence with delayed puberty.
Investigations:
Abdominal U/S
FSH, LH, and estrogen levels
Karyotype analysis
Gonads:
External genitalia are normal, uterus is present, breasts are absent with
widely spaced nipples. Ovaries are streak gonads.
Hormone:
In childhood, treatment is focused on growth, but in adolescence it focuses
on induction of puberty. So we give estrogen to induce puberty.
Dx during pregnancy:
It causes 1
st
trimester miscarriage so it will be diagnosed by maternal
karyotype. For proper pregnancy, the woman needs egg donation

Q. Cas
drugs?
Answe
Confirm
1. S
p
2. N
While a
So nitra
False p
B
3. F
d
p
Investig
1. U
2. V
a
3. C
4. C
5. a
c
G
DDx:
Drugs:
1. T
2. S
3. A
4. D
se of PPR
? Percent
r:
mation:
Speculum
posterior fo
Nitrazine te
amniotic f
azin pape
positive te
Blood, sem
Ferning tes
dry and vie
producing
gations:
U/S to ass
Vaginal sw
amniotic fl
CTG
CBC and C
amniocent
chorioamn
Gram stain
Tocolytics
Steroids
Antibiotics
Drugs for i
ROM? How
tage of de
examinat
ornix eithe
est:
luid has a
er changes
est result f
minal fluid
st: a samp
ewed und
ferning pa
sess the a
wab: testin
uid such a
CRP. Urin
tesis some
nionitis, so
n , C&S te
: e.g. Rito
nduction
w to conf
eveloping
tion: We s
er sponta
alkaline PH
s to blue i
from:
, infection
ple of fluid
er micros
attern.
mniotic flu
ng substa
as fetal fib
ne culture
e time nee
o sample o
est.
odrine. Ma
of labor a
firm it? 3
g preterm
see poolin
neously o
H (7-7.5)
if amniotic
n
d is place
scope –cry
uid volum
nces whic
bronectin
eded to c
of amnioti
agnesium
after 34 we
investig
m labor af
ng of amn
or after fun
c fluid pre
d on glas
ystallizatio
me and exc
ch are pre
, B-HCG
onfirm the
ic fluid tak
sulfate, n
eeks
ations? 2
fter 10 da
iotic fluid
ndal press
esent in th
s slide an
on of NaC
clude plac
esent in hi
e diagnos
ken and s
nifedipine,
2 DDx? 3
ays?
in the
sure
he vagina
nd allowed
Cl occur
centa prev
igh conc.
sis of
send for
Atosiban
d to
via
In
n
Percentage: 90 %
Q. Methergine? Biological effect? Indications? Contrindications?
Route? Dose?
Answer:
Biological effect:
Methylergometrine is an ergot alkaloid and a partial agonist/antagonist
on
serotonergic
,
dopaminergic
and
alpha-adrenergic
receptors. Its specific
binding and activation pattern on these receptors leads to a highly, if not
completely, specific contraction of smooth uterus muscle via
5-
HT
2A
serotonin receptors,
[6]
while blood vessels are affected to a lesser
extent compared to other ergot alkaloids
Indications:
1.
Bleeding in PPH or following spontaneous or elective abortion
2.
Active management of 3
rd
stage
3.
Expulsion of retained products of conception after missed abortion
4.
Prevention and acute treatment of migraine
Contraindications:
1. Hypertension and pre-eclampsia
2. Heart disease
3. Pregnancy and birth
4. During abnormal lie
5. Cord prolapse
Side effects:
1.
Fetal distress
2.
Uterine rupture
3.
Retained placenta
4.
Cholinergic
effects such as nausea, vomiting, and diarrhea
5.
Dizziness
6.
Coronary artery vasoconstriction
7.
Severe systemic hypertension (especially in patients
with
preeclampsia
)
8.
Convulsions

Route:
Injections: (IM or IV). IV form is used in obstetrics
Oral: Tablets or in liquid form
Dose: 0.5 mg/ml
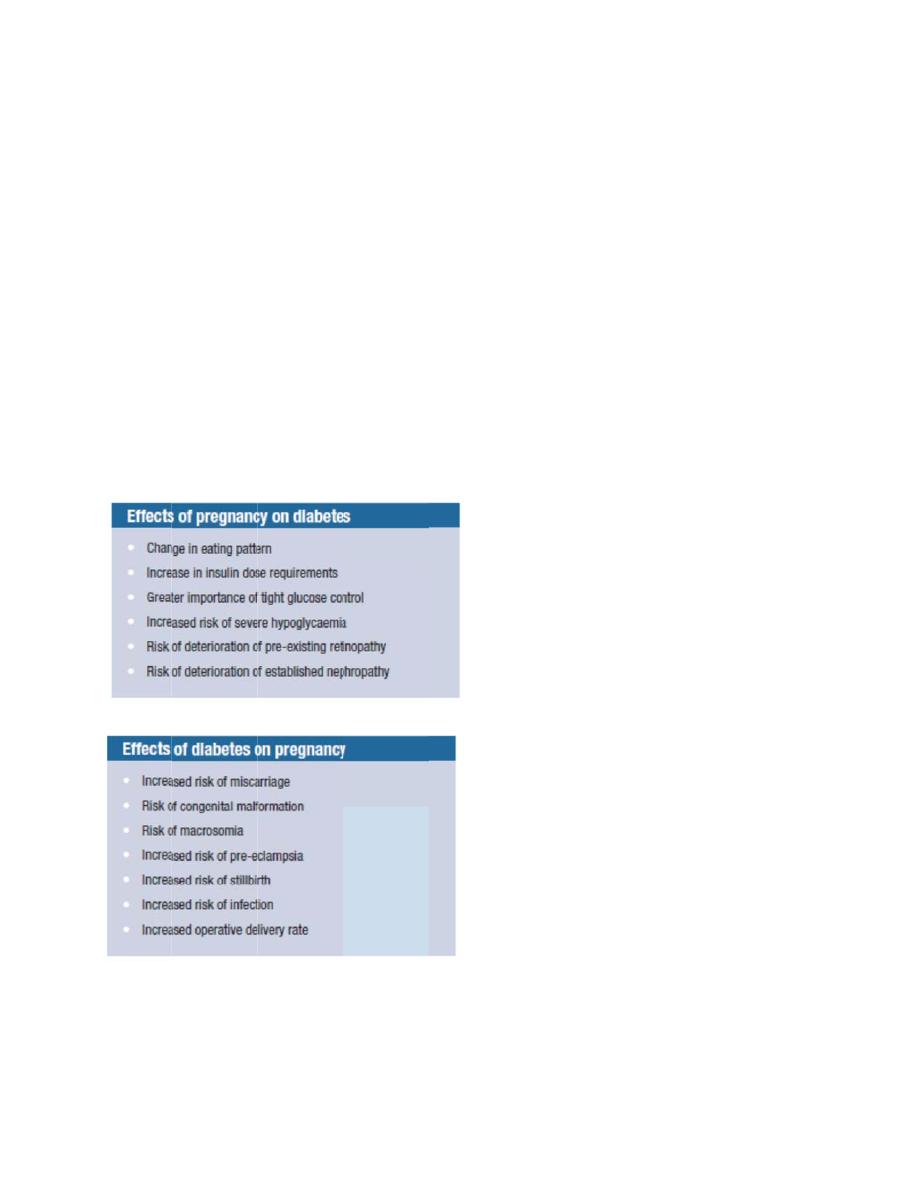
Q. DM Counselling? Whether to get pregnant or not? Complications?
Prepregnancy counselling
Answer:
The risk of problems for you and your baby can be greatly reduced by the
following advice:
Avoid unplanned pregnancies. It is very important to plan any
pregnancy and so contraception is very important.
Good control of blood sugar (glucose) levels before and during
pregnancy reduces the risks of stillbirth, miscarriage, congenital
malformation and neonatal death.
It is essential to follow the dietary advice, weight control and exercise
advice given to all people with diabetes.
Make sure you are regularly checked for any complications of diabetes,
including regular eye assessments and other assessments and
appointments with your practice nurse, GP or specialist.
If you are planning to become pregnant then you should take 5 mg
of
folic acid
daily until 12 weeks of pregnancy to reduce the risk of birth
defects in your baby.
Ketone testing strips should be used to test for ketones if you become
unwell. Ketones are substances the body makes if there is a lack of
insulin in the blood.
If you smoke then it is even more important to
stop smoking
before
pregnancy.
Reduce or cut down on the amount of
alcohol you drink
.
Think very positively about
breast-feeding
because it improves blood
glucose control and makes it easier to lose weight after giving birth.
Hyperg
organo
pregna
pregna
abnorm
pregna
is simil
congen
and ad
therapy
pre-me
creatin
function
Effect o
1. P
2. In
glycaemia
ogenesis –
ancy is me
ancycorrel
mality. Onc
ancy is aro
ar. Pre-pr
nital malfo
equate
co
y pre-preg
eal
glucos
ine conce
n.
of diabete
Pre-eclam
nfection
a exerts its
– the first
edically
co
ates well
ce HbA1c
ound
30 p
regnancy
ormation. T
ontracepti
gnancy sh
e levels o
entrations
es on the m
psia and
s teratoge
42 days o
onfirmed.
with the r
c is _10 pe
per cent, w
care coul
Therefore
ion used u
hould be to
of 4–7 mm
, the
highe
mother: In
eclampsia
enic effect
of
pregnan
The level
risk of ear
er cent,
th
while the r
d significa
e,
d
iabetes
until gluco
o
maintain
mol/L. The
er the risk
ncreased
a especia
ts during
t
ncy – ofte
of HbA1c
rly fetal los
he risk of f
risk of con
antly
redu
s therapy
ose contro
n HbA1c
e higher
th
k of perma
incidence
ally in pre-
the period
en before
c in early
ss andcon
fetal loss
ngenital m
uce the ra
y should b
ol is good
at 6.5 per
he pre-pre
anent loss
e of
-existing D
d of
the
ngenital
during
malformati
tes of
e intensif
.Targets f
r cent and
egnancy
s of renal
DM
on
ied
for
d
3. Traumatic delivery and C/S
4. Polyhydramnios
5. PPH
Effect of diabetes on the fetus:
1. Intrauterine death due to hypoxia and acidosis
2. Neonatal morbidity and mortality
3. Neonantal hypoglycemia, hypocalcemia, polycythemia, and
hyperbilirubinemia
4. RDS
5. Congenital anomalies (NTD and sacral agenesis)
Q. Lower abdominal pain: Examination? 3 uterine and 3 extrauterine
causes?
Answer:
1. General examination
2. Abdominal examination
3. Pelvic examination
Uterine causes:
1. Fibroids
2. Endometriosis and adenomyosis
3. PID
4. Ectopic pregnancy
5. Ovarian cysts
Extrauterine causes:
1. Acute Appendicitis
2. Acute Cholecystitis
3. UTI
4. Renal stones
5. Diverticulitis
Q. Iron deficiency anemia? History? Examination? DDx?
Investigations?
Answer:
History:

1. Symptoms of anemia:
General: Pallor, fatigue, malaise, weakness
CVS: palpitation, dyspnea, syncope
Neurological: Headache, vertigo, tinnitus, loss of concenteration
Specific for IDA: Pica
2. Dietary history
3. Anorexia and weight loss
4. Recent pregnancy
5. Chronic diarrhea
6. Bleeding source especially GIT and genitalia
7. Past medical history: Liver disease, renal disease, thyroid disease,
malabsorption
8. Past surgical history: Gastrectomy, blood transfusion
9. Drug hx: Aspirin, NSAIDs, sulfa drugs, chloramphenicol
10.
Exposure to radiation
11.
Family history of anemia, ethnicity
Examination:
1. General examination:
Vital signs
Pallor of skin and mucus membranes
Jaundice
Glossitis and angular stomatitis
Nails for koilonychia
Lymphadenopathy
Bleeding spots
2. CVS:
Tachycardia
Wide pulse pressure
Systolic flow murmur
Sometimes evidence of CHF
3. Abdominal examination
Splenomegaly
4. Neurological examination for B12 deficiency
DDx:
1. Microcytic hypochromic: IDA is the most common cause
2. Normochromic normocytic
3. Macrocytic
Investigations:
1. CBC, reticulocyte count, and blood film
2. Iron studies
3. Hb electrophoresis
4. B12 and folate levels
5. Coombs test
6. Osmotic fragility test
7. RBC enzyme studies
8. Bone marrow aspirate and biopsy.
Q. PCOS? Criteria? Complications in future? Treatment of hirsutism
and infertility?
Answer:
Criteria:
1. Oligomenorrhoea/amenorrhoea
2. Clinical and/or biochemical hyperandrogenism
3. Polycystic ovaries by U/S:
Ovary with 12 or more follicles measuring 2-9 mm in diameter and
increased ovarian volume (≥ 10 cm
3
)
Comlications in future:
Medical: DM and cardiovascular disease
Gynecological: Endometrial hyperplasia and CA
Treatment of hirsutism:
•
Eflornithine cream (Vaniqua™) applied topically;
•
Cyproterone acetate (Dianette™, anti-androgen
contraceptive pill);
•
Metformin: improves parameters of insulin
resistance, hyperandrogenemia, anovulation and
acne in PCOS;
•
GnRH analogues with low-dose HRT: this regime
should be reserved for women intolerant of other
therapies;
•
Surgical treatments, e.g. laser or electrolysis.
Treatment of infertility:

Life style modification with diet and exercise to achieve weight
reduction
Clomiphene citrate
Parenteral gonadotrophins or laparoscopic ovarian diathermy
