SYSTEMIC HYPERTENSION
• Hypertension is one of the leading causes of
the global burden of disease.
• Hypertension doubles the risk of
cardiovascular diseases, including coronary
heart disease (CHD), congestive heart
failure (CHF), ischemic and hemorrhagic
stroke, renal failure, and peripheral arterial
disease.
• Although antihypertensive therapy clearly
reduces the risks of cardiovascular and
renal disease, large segments of the
hypertensive population are either untreated
or inadequately treated.
Definition
• Hypertension currently is defined as a
usual BP of 140/90 mm Hg or higher,
for which the benefits of drug treatment
have been definitively established
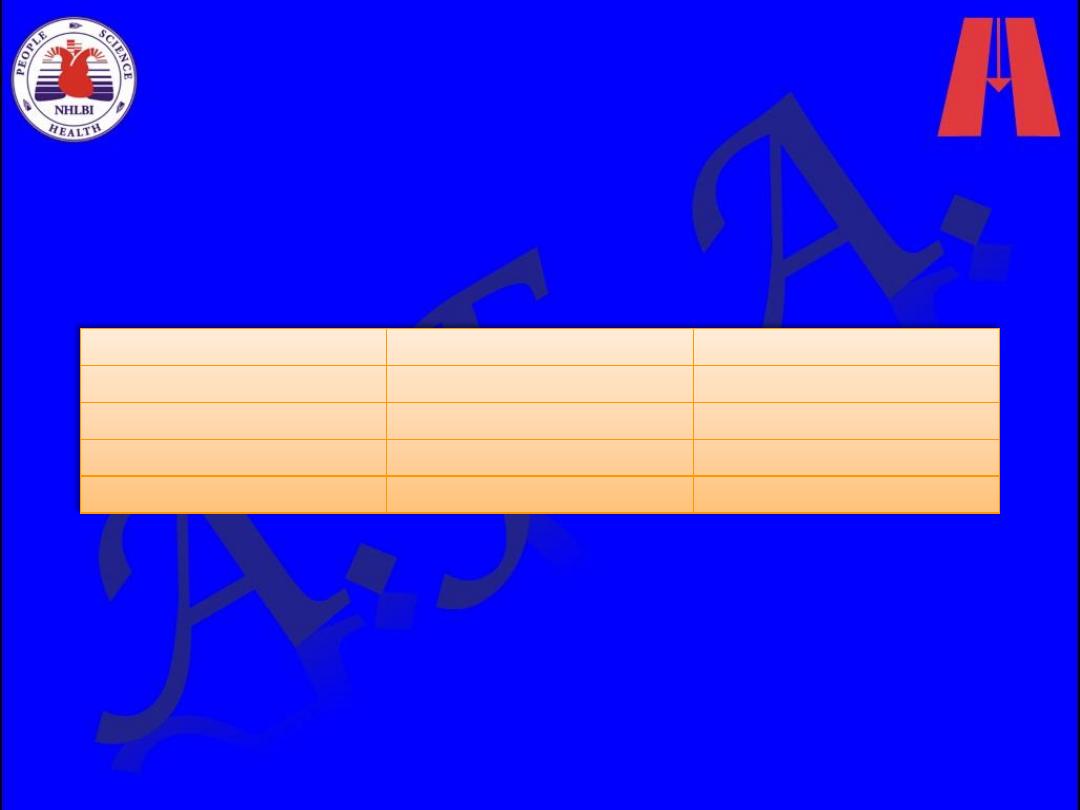
Staging of Office Blood Pressure
BP STAGE
SYSTOLIC BP (mm Hg) DIASTOLIC BP (mm Hg)
Normal
<120
<80
Prehypertension
120-139
80-89
Stage 1 hypertension
140-159
90-99
Stage 2 hypertension
≥160
≥100
Aetiology
1. Primary (Essential) hypertension
– The majority (90–95%) of patients with
hypertension have primary elevation of
blood pressure, i.e. essential hypertension
of unknown cause.
2. Secondary hypertension (5-10%).
Many factors may contribute to
development of essential HT
1. Neural Mechanisms
– Baroreflex control of sinus node function is
abnormal
– Obesity-Related Hypertension
– Obstructive Sleep Apnea
2. Renal Mechanisms
– acquired or inherited defect in the kidneys' ability
to excrete the excessive sodium load
– Low Birth Weight
– Genetic Contributions
3. Vascular Mechanisms
– Endothelial Cell Dysfunction
– Vascular Remodeling: An increase in the medial
thickness relative to lumen diameter (increased
media-to-lumen ratio) is the hallmark of
hypertensive remodeling in small and large arteries.
4. Hormonal Mechanisms
– Activation of the renin-angiotensin-aldosterone
system (RAAS) is one of the most important
mechanisms contributing to endothelial cell
dysfunction, vascular remodeling, and hypertension
Secondary hypertension
1. Renal diseases
These account for over 80% of the cases
of secondary hypertension.
The common causes are:
■ diabetic nephropathy
■ chronic glomerulonephritis
■ adult polycystic disease
■ chronic tubulointerstitial nephritis
■ renovascular disease.
2. Endocrine causes
These include:
– Conn’s syndrome
– Congenital adrenal hyperplasia
– phaeochromocytoma
– Cushing’s syndrome
– acromegaly.
– Hyperparathyroidism
– Primary hypothyroidism
– Thyrotoxicosis
3. Congenital cardiovascular causes
– The major cause is coarctation of the aorta
4. Drugs:
NSAIDs, oral
contraceptives, steroids,
carbenoxolone, liquorice,
sympathomimetics and
vasopressin.
5. Pregnancy (pre-eclampsia)
6. Alcohol
7. Obesity
• All adults should have blood pressure measured
routinely at least every 5 years until the age of 80
years.
•
Seated blood pressure
when measured after 5
minutes’ resting with appropriate cuff size and arm
supported is usually sufficient, but
standing blood
pressure
should be measured in diabetic and
elderly subjects to exclude orthostatic
hypotension.
•
The cuff should be deflated at 2 mm/s and the
blood pressure measured to the nearest 2 mmHg.
•
Two consistent blood pressure measurements
are needed to estimate blood pressure, and more
are recommended if there is variation in the
pressure.
• When assessing the cardiovascular risk, the
average blood pressure at separate visits is more
accurate than measurements taken at a single
visit.
Assessment
History
• Family history, lifestyle (exercise, salt intake, smoking
habit) and other risk factors should be recorded.
• The patient with mild hypertension is usually
asymptomatic.
• Higher levels of blood pressure may be associated
with headaches, epistaxis or nocturia.
• Attacks of sweating, headaches and palpitations point
towards the diagnosis of
phaeochromocytoma.
• Breathlessness may be present owing to left
ventricular hypertrophy or cardiac failure,
• symptoms of peripheral arterial vascular disease
suggest the diagnosis of
atheromatous renal artery
stenosis.
Examination
• Findings related to hypertension
Loud A2
S4
Forceful sustained apical impulse
(heaving)
Examination
1. Secondary causes
: Radio-femoral delay (coarctation of
the aorta), enlarged kidneys (polycystic kidney disease),
abdominal bruits (renal artery stenosis) and the
characteristic facies and habitus of Cushing's syndrome are
all examples of physical signs that may help to identify
causes of secondary hypertension.
2. Risk factors
: Examination may also reveal features of
important risk factors such as central obesity and
hyperlipidaemia (tendon xanthomas etc.).
3. Complications:
– The optic fundi are often abnormal
– and there may be evidence of generalised atheroma or
specific complications such as aortic aneurysm or
peripheral vascular disease.
Investigations
investigation of all patients
• Urinalysis for blood, protein and glucose
• Blood urea, electrolytes and creatinine
– N.B. Hypokalaemic alkalosis may indicate
primary hyperaldosteronism but is usually due
to diuretic therapy
• Blood glucose
• Serum total and HDL cholesterol
• 12-lead ECG (left ventricular hypertrophy,
coronary artery disease)
investigation of selected
patients
• Chest X-ray
: to detect cardiomegaly, heart failure,
coarctation of the aorta
• Ambulatory BP recording
: to assess borderline or 'white
coat' hypertension
• Echocardiogram
: to detect or quantify left ventricular
hypertrophy & for the diagnosis ofcoactation of aorta
• Renal ultrasound
: to detect possible renal disease
• Renal angiography
: to detect or confirm presence of renal
artery stenosis
• Urinary catecholamines
: to detect possible
phaeochromocytoma
• Urinary cortisol and dexamethasone suppression test
:
to detect possible Cushing's syndrome
• Plasma renin activity and aldosterone
: to detect
possible primary aldosteronism
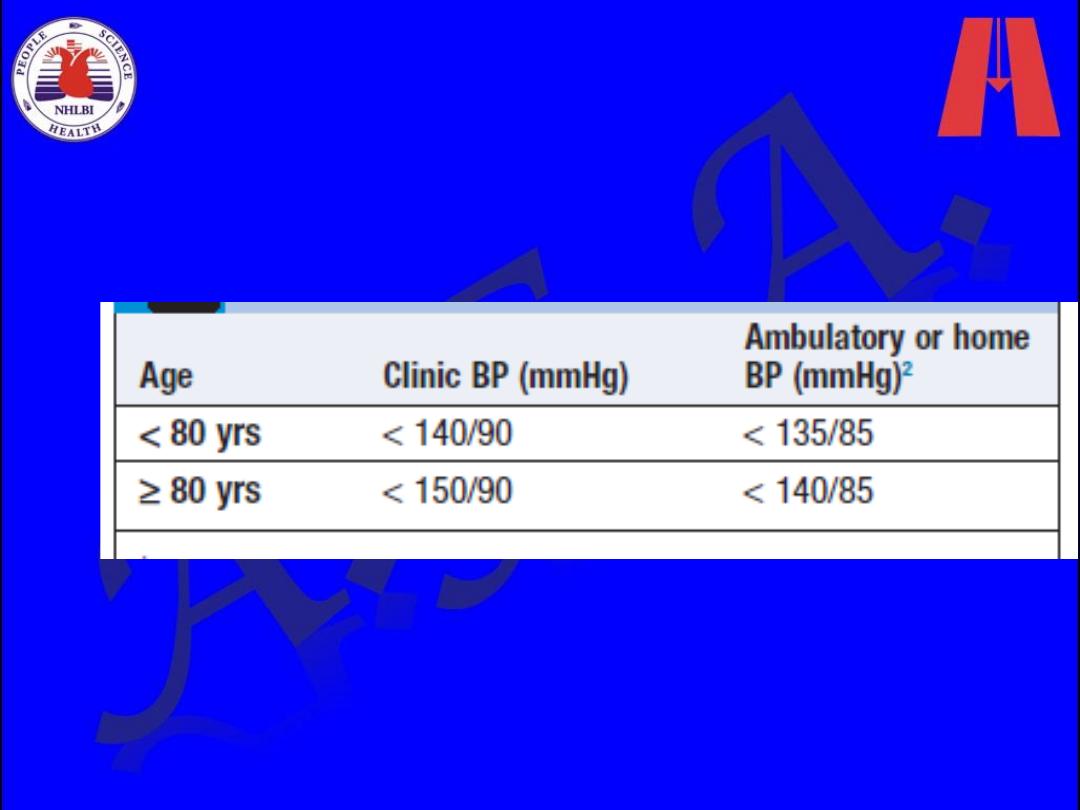
Ambulatory blood pressure monitoring
• Indirect automatic blood pressure measurements
can be made over a 24-hour period using a
measuring device worn by the patient.
• they are used to confirm the diagnosis in those
patients with
‘white-coat’ hypertension
, i.e.
blood pressure is completely normal at all stages
except during a clinical consultation
• These devices may also be used to monitor the
response of patients to drug treatment and, in
particular, can be used to determine the adequacy
of 24-hour control with once-daily medication
• Ambulatory blood pressure recordings
seem to be better predictors of
cardiovascular risk than clinic
measurements.
• Analysis of the diurnal variation in blood
pressure suggests that those
hypertensives with loss of the usual
nocturnal fall in
blood pressure (‘non-
dippers’) have a worse prognosis than
those who retain this pattern.
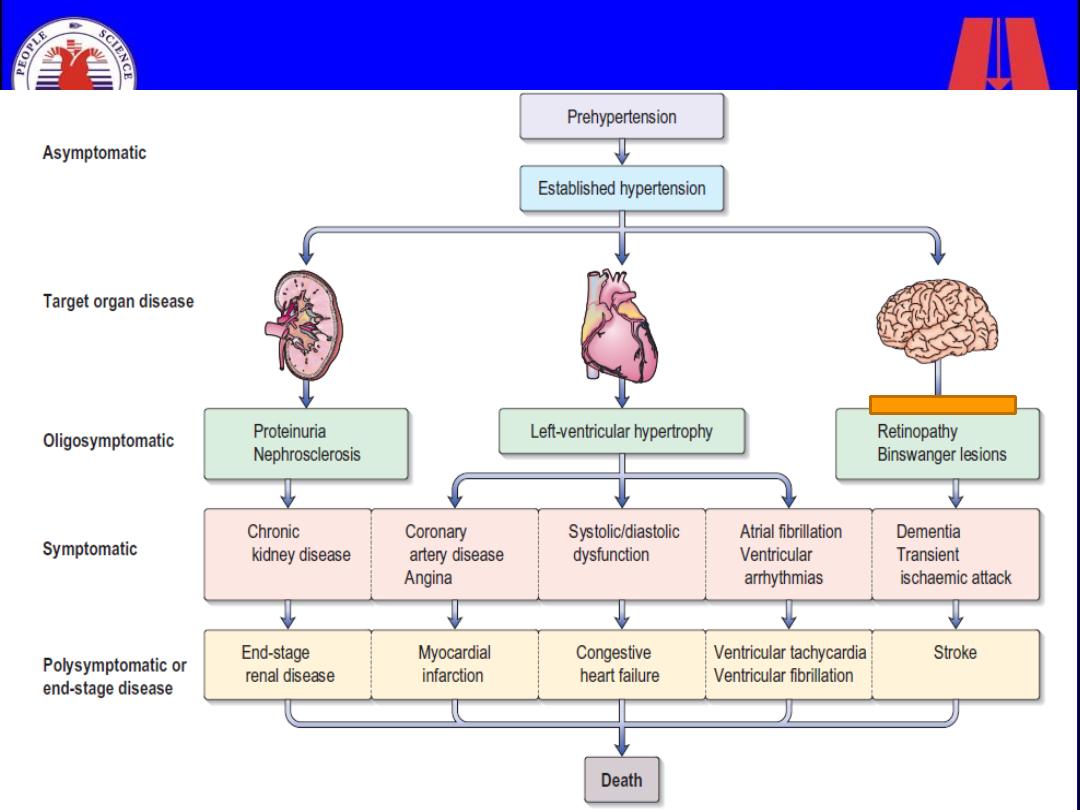
Complications

1. Blood vessels
– In larger arteries (> 1 mm in diameter), the internal
elastic lamina is thickened, smooth muscle is
hypertrophied and fibrous tissue is deposited.
– In smaller arteries (< 1 mm), hyaline arteriosclerosis
– aortic aneurysm and aortic dissection
2. Central nervous system
– Stroke (due to cerebral haemorrhage or infarction).
– Carotid atheroma and transient ischaemic attacks are
more common in hypertensive patients.
– Subarachnoid haemorrhage is also associated with
hypertension.

– Hypertensive encephalopathy is a rare
condition characterised by high BP and
neurological symptoms, including transient
disturbances of speech or vision,
paraesthesiae, disorientation, fits and loss
of consciousness. Papilloedema is
common.
3. Retina
– central retinal vein thrombosis
– Hypertensive retinopathy
Grade I
Arteriolar thickening, tortuosity and increased reflectiveness ('silver wiring')
Grade 2
Grade 1 plus constriction of veins at arterial crossings ('arteriovenous nipping')
Grade 3
Grade 2 plus evidence of retinal ischaemia (flame-shaped or blot haemorrhages and 'cotton
wool' exudates)
Grade 4
papilloedema
4. Heart
– coronary artery disease.
– left ventricular hypertrophy
– Atrial fibrillation
– Diastolic dysfunction
– LV failure.
5. Kidneys
– Long-standing hypertension may cause proteinuria and
progressive renal failure by damaging the renal vasculature.
6. 'Malignant' or 'accelerated' phase hypertension
(Diastole>130 mmgh)
– This rare condition may complicate hypertension of any
aetiology and is characterised by accelerated microvascular
damage and by intravascular thrombosis.
– The diagnosis is based on evidence of high BP and rapidly
progressive end organ damage, such as
retinopathy
(grade 3
or 4),
renal dysfunction
(especially proteinuria) and/or
hypertensive encephalopathy
.
– Left ventricular failure may occur and, if this is untreated, death
occurs within months.
Treatment
Overview
بورد عراقي
)
دكتوراه
(
في الطب الباطني
بورد عربي
)
دكتوراه
(
في الطب الباطني
بورد عراقي
)
دكتوراه
(
اختصاص دقيق في أمراض
وقسطرة القلب والشرايين

Treatment
Overview
Goals of therapy
Lifestyle modification
Pharmacologic treatment
• Algorithm for treatment of hypertension
"The Goal is to Get to Goal!”
Hypertension
-PLUS-
Diabetes or Renal Disease
< 140/90 mmHg
< 130/80 mmHg
Measurements and goals
should be provided to the
patient verbally and in writing
at each office visit
Lifestyle Interventions
• Implementation of lifestyles that
favorably affect blood pressure has
implications for both the prevention and
the treatment of hypertension.
• Health-promoting lifestyle modifications
are recommended for individuals with
prehypertension and as an adjunct to
drug therapy in hypertensive individuals.
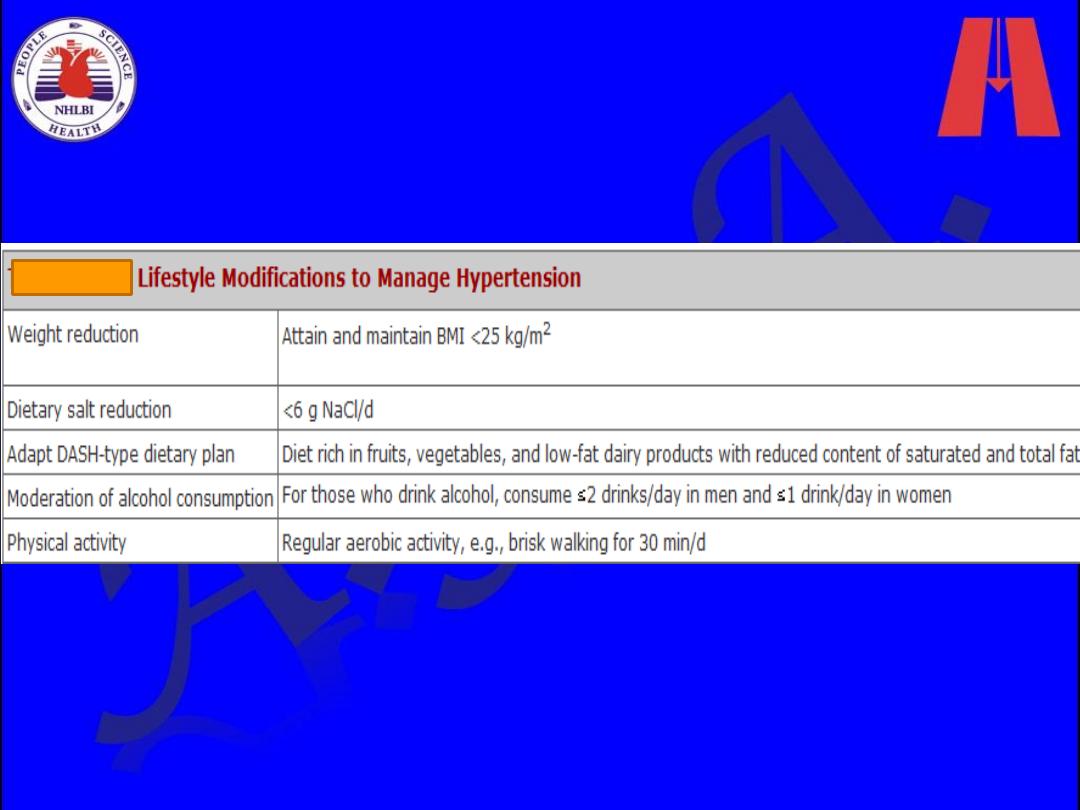
Lifestyle Modification
Modification
Approximate SBP reduction
(range)
Weight reduction
5–20 mmHg/10 kg weight loss
Adopt DASH eating plan
8–14 mmHg
Dietary sodium reduction
2–8 mmHg
Physical activity
4–9 mmHg
Moderation of alcohol
consumption
2–4 mmHg
Dietary
Approaches to
Stop
Hypertension
• Lowers systolic BP
– in normotensive
patients by an
average of 3.5 mm
Hg
– In hypertensive
patients by 11.4 mm
Hg
• Copies available
from NHLBI website
http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/
DASH Eating Plan
• Low in saturated fat, cholesterol, and total fat
• Emphasizes fruits, vegetables, and low fat
diary products
• Reduced red meat, sweets, and sugar
containing beverages
• Rich in magnesium, potassium, calcium,
protein, and fiber
• 3 -1.5 g sodium per day
• Can reduce BP in 2 weeks
Sacks FM. NEJM. 2001; 344:3-10.
Sample Menu
• Breakfast
– 1 whole-wheat bagel
– 2 tablespoons peanut butter
– 1 medium orange
– 1 cup fat-free milk
– Decaffeinated coffee
• Lunch
– Spinach salad made with 4 cups of fresh spinach leaves, 1 sliced pear,
1/2 cup mandarin orange sections, 1/3 cup unsalted peanuts and 2
tablespoons reduced-fat red wine vinaigrette
– 12 reduced-sodium wheat crackers
– 1 cup fat-free milk
• Dinner
– Herb crusted baked cod
– 1 cup bulgur
– 1/2 cup fresh green beans, steamed
– 1 sourdough roll with 1 teaspoon trans-free margarine
– 1 cup fresh berries with chopped mint
– Herbal iced tea
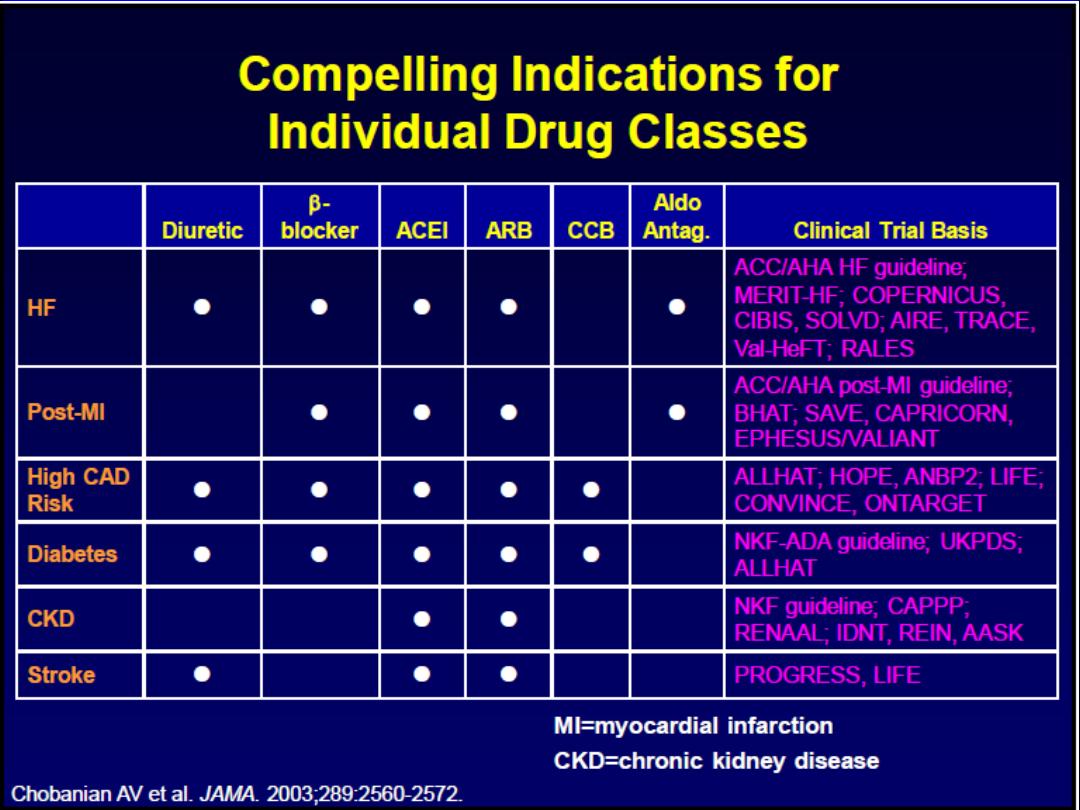
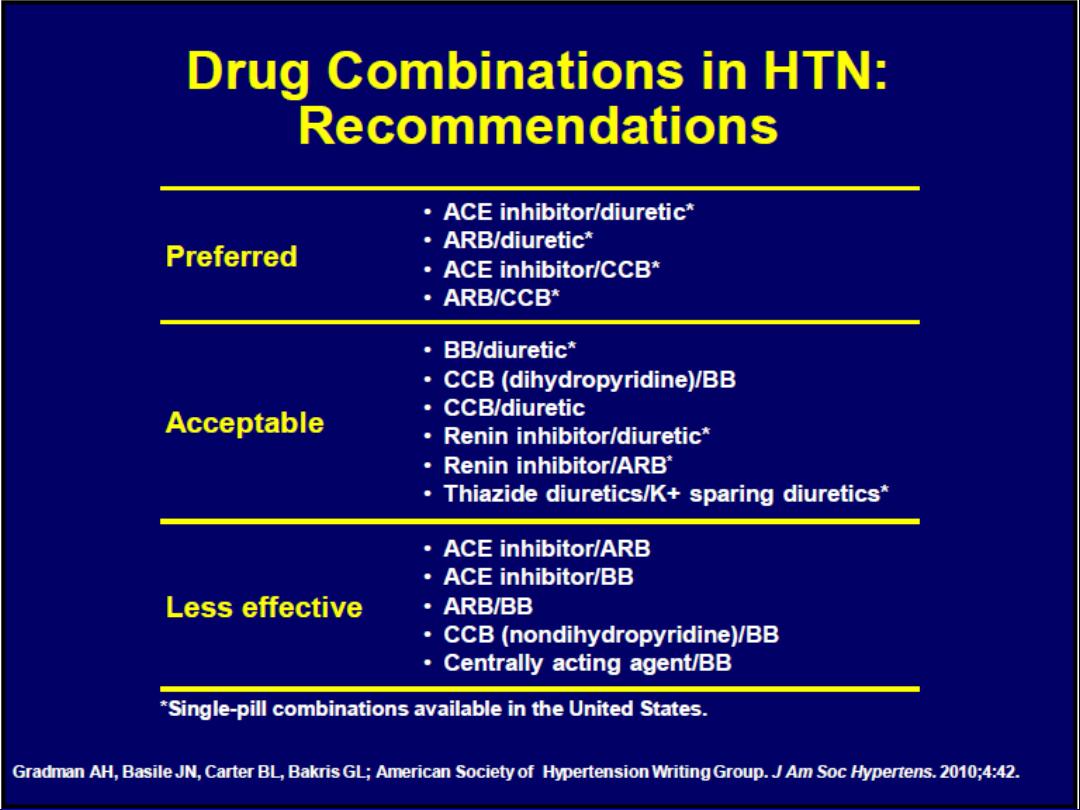
Algorithm for Treatment of Hypertension
Not at Goal Blood Pressure (<140/90 mmHg)
(<130/80 mmHg for those with diabetes or chronic kidney disease)
Initial Drug Choices
Drug(s) for the compelling
indications
Other antihypertensive drugs
(diuretics, ACEI, ARB, BB, CCB)
as needed.
With Compelling
Indications
Lifestyle Modifications
Stage 2 Hypertension
(SBP >160 or DBP >100 mmHg)
2-drug combination for most
Stage 1 Hypertension
(SBP 140
–159 or DBP 90–99 mmHg)
Thiazide-type diuretics , ACEI, ARB,
BB, CCB,
or combination.
Without Compelling
Indications
Not at Goal
Blood Pressure
Optimize dosages or add additional drugs
until goal blood pressure is achieved.
Consider consultation with hypertension specialist.
Pharmacologic Therapy
Drug therapy is recommended for individuals with blood
pressures 140/90 mmHg. The degree of benefit derived
from antihypertensive agents is related to the
magnitude of the blood pressure reduction.
Benefits of Lowering BP
Average Percent Reduction
Stroke incidence
35–40%
Myocardial infarction
20–25%
Heart failure
50%
Lowering systolic blood pressure by 10–12 mmHg and diastolic blood pressure by 5–6
mmHg
Diuretics
Low-dose thiazide diuretics often were previously used as first-line agents
alone or in combination with other antihypertensive drugs.
Thiazides inhibit the Na
+
/Cl
–
pump in the distal convoluted tubule and hence
increase sodium excretion.
In the long term, they also may act as vasodilators.
Thiazides are safe, efficacious, inexpensive, and reduce clinical events.
They provide additive blood pressure–lowering effects when combined with
beta blockers, angiotensin-converting enzyme inhibitors (ACEIs), or
angiotensin receptor blockers (ARBs).
In contrast, addition of a diuretic to a calcium channel blocker is less effective.
Drugs recommended
• Indapamide 1.5 mg
• Chlorthalidone 6.25-50 mg/dl
Owing to an increased incidence of metabolic side effects (hypokalemia,
insulin resistance, increased cholesterol), higher doses generally are not
recommended.
Indications:
• HF
• Stroke
Loop diuretics generally are reserved for hypertensive
patients with
• reduced glomerular filtration rates [reflected in
serum creatinine >220 mol/L (>2.5 mg/dL)],
• CHF,
• or sodium retention and edema
Low-dose eplerenone (6.25 to 25 mg/day) or spironolactone
(6.25 to 12.5 mg/day) can be effective in treatment of primary
hypertension, particularly low-renin hypertension in African
Americans.
Angiotensin-Converting Enzyme Inhibitors
These inhibit the conversion of angiotensin I to angiotensin II and are
usually well tolerated.
They are particularly useful in diabetics with nephropathy, where they
have been shown to slow disease progression, and in those patients
with symptomatic or asymptomatic left ventricular dysfunction, where
they have been shown to improve survival.
Electrolytes and creatinine should be checked before and 1-2 weeks
after commencing therapy.
Side-effects include first-dose hypotension, cough, rash,
hyperkalaemia and renal dysfunction.
• The most common side effect of ACE inhibitors is a dry
cough. Patients may complain not of a cough but rather of
having to clear the throat or loss of voice later in the day.
These symptoms occur in 3 to 39% of patients, resolve in a
few days after the drug is discontinued, and can be
eliminated by switching the patient to an ARB. The incidence
is higher in African Americans than in whites and is highest in
Asians.
Angiotensin II receptor antagonists
This group of agents selectively block the receptors for
angiotensin II. They share many of the actions of ACE
inhibitors but, since they do not have any effect on
bradykinin, do not cause a cough. They are currently
used for patients who cannot tolerate ACE inhibitors
because of persistent cough.
Angioneurotic oedema and renal dysfunction are
encountered less with these drugs than with ACE
inhibitors.
Indications of both:
• HF
• MI
• Diabetes
• CKD
• Stroke
Beta-adrenoceptor blockers
B-Adrenergic receptor blockers lower blood pressure by
decreasing cardiac output, due to a reduction of heart
rate and contractility.
They are no longer a preferred initial therapy for
hypertension.
Indications:
• Angina
• MI
• HF
• Tachycardia
The major side-effects of this class of agents are
bradycardia, bronchospasm, cold extremities, fatigue,
bad dreams and hallucinations.
Atenolol has been shown to reduce brachial arterial
pressure but not aortic pressure, which is more
significant in causing strokes and heart attacks. Atenolol
is now not a preferred drug for hypertension.
Calcium-channel blockers
These agents effectively reduce blood pressure by
causing arteriolar dilatation, and some also reduce the
force of cardiac contraction. Like the beta-blockers, they
are especially useful in patients with concomitant
ischaemic heart disease.
The major side-effects are particularly seen with the
short-acting agents and include headache, sweating,
swelling of the ankles, palpitations and flushing.
Indications:
• Angina

Alpha-blockers
By blocking the interaction of norepinephrine on
vascular α-adrenergic receptors, these drugs cause
peripheral vasodilation, thereby lowering blood
pressure.
they are effective third- or fourth-line therapy for difficult
hypertension and are particularly useful in older men
with prostatism.
Indications:
• Prostatism
• Phenoxybenzamine remains the drug of choice for preoperative
management of pheochromocytoma
Renin inhibitors
Aliskerin is the first orally active renin inhibitor which
directly inhibits plasma renin activity: it reduces the
negative feedback by which angiotensin II inhibits renin
release.
It has been used in combination with ACE inhibitors and
angiotensin receptor blockers with a significant
reduction in blood pressure. Side-effects are few but
hypokalaemia occurs.
Centrally acting drugs
Reserpine
is used in a low dose of 0.05 mg/day, which
provides almost all its antihypertensive action with fewer
sideeffects than higher doses. It has a slow onset of
action (measured in weeks).
Methyldopa
is still widely used despite central and
potentially serious hepatic and blood side-effects. It acts
on central á2-receptors, usually without slowing the
heart.
Clonidine
provide all the benefits of methyldopa with
none of the rare (but serious) autoimmune reactions.
vasodilators
These include hydralazine (up to 100 mg daily) and
minoxidil (up to 50 mg daily). Both are extremely potent
vasodilators that are reserved for patients resistant to
other forms of treatment.
Hydralazine can be associated with tachycardia, fluid
retention and a systemic lupus erythematosus-like
syndrome.
Minoxidil can cause severe oedema, excessive hair
growth and coarse facial features.
If these agents are used, it is usually in combination
with a beta-blocker.
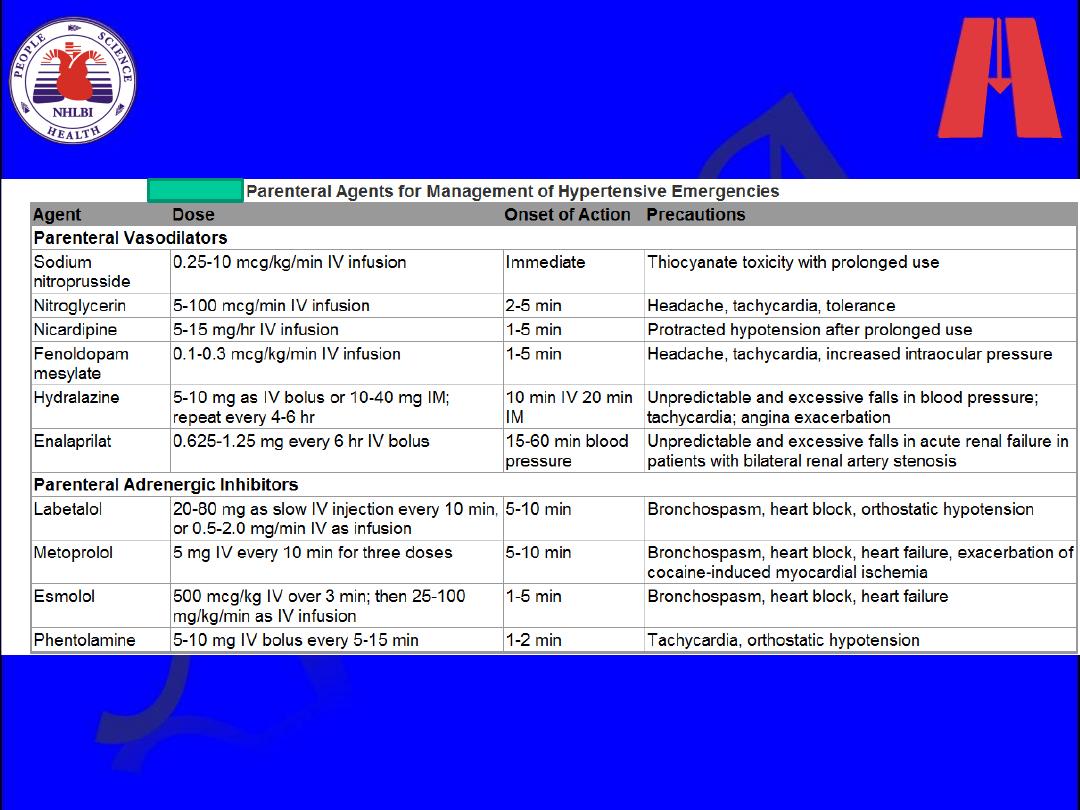
Acute Severe Hypertension
Twenty-five percent of all emergency department patients
present with an elevated blood pressure .
Hypertensive emergencies
are acute, often severe,
elevations in blood pressure, accompanied by acute (or
rapidly progressive) target organ dysfunction, such as
myocardial or cerebral ischemia or infarction, pulmonary
edema, or renal failure.
Hypertensive urgencies
are severe elevations in blood
pressure without severe symptoms and without evidence of
acute or progressive target organ dysfunction. The key
distinction depends on the state of the patient and the
assessment of target organ damage, not just the absolute
level of blood pressure.
The full-blown clinical picture of a hypertensive
emergency is a critically ill patient who presents with a
blood pressure above 220/140 mm Hg, headaches,
confusion, blurred vision, nausea and vomiting,
seizures, pulmonary edema, oliguria, and grade 3 or
grade 4 hypertensive retinopathy .
Hypertensive emergencies require immediate intensive
care unit (ICU) admission for intravenous therapy and
continuous blood pressure monitoring;
In most other hypertensive emergencies, the goal of
parenteral therapy is to achieve a controlled and
gradual lowering of blood pressure.
A good rule of thumb is to lower the initially
elevated arterial pressure by 10% in the first hour
and by an additional 15% during the next 3 to 12
hours to a blood pressure of no less than 160/110
mm Hg. Blood pressure can be reduced further
during the next 48 hours.
hypertensive urgencies often can be managed with oral
medications and appropriate outpatient follow-up in 24
to 72 hours.
Most patients who present to the emergency
department with hypertensive urgencies either are
nonadherent with their medical regimen or are
being treated with an inadequate regimen.
To expedite the necessary changes in medications,
outpatient follow-up should be arranged within 72
hours
Resistant Hypertension
Defined as persistence of usual blood pressure above
140/90 mm Hg despite treatment with full doses of three or
more different classes of medications including a diuretic in
rational combination, resistant hypertension is the most
common reason for referral to a hypertension specialist. In
practice, the problem usually falls into one of four
categories: (1) pseudoresistance, (2) an inadequate medical
regimen, (3) nonadherence or ingestion of pressor
substances, or (4) secondary hypertension.
• Pseudoresistant hypertension is caused by white coat
aggravation

Adjuvant drug therapy
Aspirin.
Antiplatelet therapy is a powerful means of reducing
cardiovascular risk but may cause bleeding, particularly intracerebral
haemorrhage, in a small number of patients. The benefits are thought to
outweigh the risks in hypertensive patients aged 50 or over who have well-
controlled BP and either target organ damage, diabetes or a 10-year
coronary heart disease risk of ≥ 15% (or 10-year cardiovascular disease
risk of ≥ 20%).
Statins.
Treating hyperlipidaemia can produce a substantial reduction in
cardiovascular risk. These drugs are strongly indicated in patients who
have established vascular disease, or hypertension with a high (≥ 20% in
10 years) risk of developing cardiovascular disease