A.F.A.
Myocardial disease , is a disaese of the
myocardium that is not due to an ischaemic,
valvular or hypertensive heart disease,
It may be caused by:
O
an acute or chronic inflammatory pathology
(myocarditis)
O
idiopathic myocardial disease
(cardiomyopathy).
O
This is an acute inflammatory condition that can have an
infectious, toxic or autoimmune aetiology.
O
Myocarditis can complicate many
infections
in which
inflammation may be due directly to infection of the
myocardium or the effects of circulating toxins.
O
Viral infections are the most common causes, such as
Coxsackie and influenza A and B viruses.
O
Myocarditis may occur several weeks after the initial viral
symptoms and susceptibility is increased by corticosteroid
treatment, immunosuppression, radiation, previous
myocardial damage and exercise.
A.F.A.
O
Some bacterial and protozoal infections may be
complicated by myocarditis; for example, approximately
5% of patients with Lyme disease (Borrelia burgdorferi)
develop myopericarditis, which is often associated with
AV block.
O
Toxic aetiologies
include drugs,
O
which may directly injure the myocardium (e.g. cocaine,
lithium and anticancer drugs such as doxorubicin)
O
or which may cause a hypersensitivity reaction and
associated myocarditis (e.g. penicillins and
sulphonamides), lead and carbon monoxide.
O
Occasionally,
autoimmune
conditions such as systemic
lupus erythematosus and rheumatoid arthritis are
associated with myocarditis.
Pathology
O
In the acute phase myocarditic hearts are flabby with
focal haemorrhages;
O
in chronic cases they are enlarged and hypertrophied.
O
Histologically an inflammatory infiltrate is present
O
– lymphocytes predominating in viral causes;
O
- Polymorphonuclear cells in bacterial causes;
O
- eosinophils in allergic and hypersensitivity causes
A.F.A.
Clinical features
O
Myocarditis may be an acute or chronic process;
O
its clinical presentations range from an
asymptomatic
state associated with limited and focal inflammation
O
to
fatigue, palpitations, chest pain, dyspnoea and
fulminant congestive cardiac failure
due to diffuse
myocardial involvement.
O
Physical examination includes soft heart sounds, a
prominent third sound and often a tachycardia.
O
A pericardial friction rub may be heard.
Investigations
O
Chest X-ray may show some cardiac enlargement, depending on
the stage and virulence of the disease.
O
ECG demonstrates ST- and T wave abnormalities and arrhythmias.
O
Heart block may be seen with diphtheritic myocarditis, Lyme
disease and Chagas’ disease .
O
Cardiac enzymes are elevated.
O
Viral antibody titres may be increased.
O
However, since enteroviral infection is common in the general
population, the diagnosis depends on the demonstration of acutely
rising titres.
O
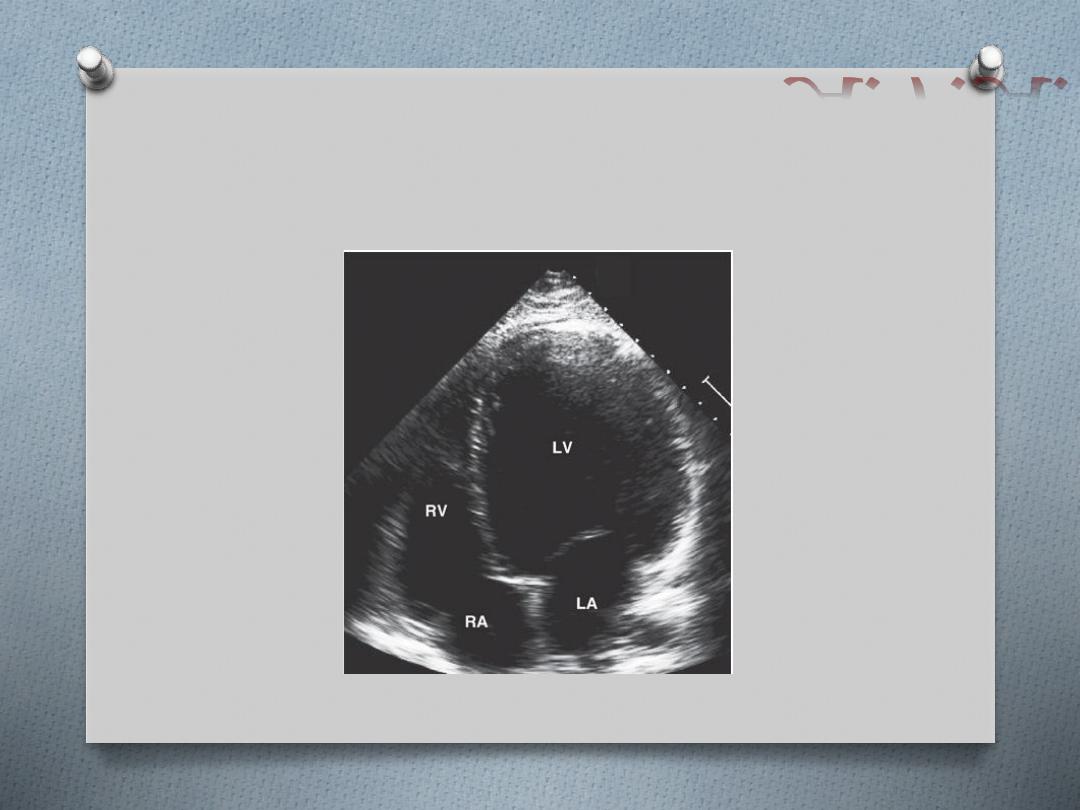
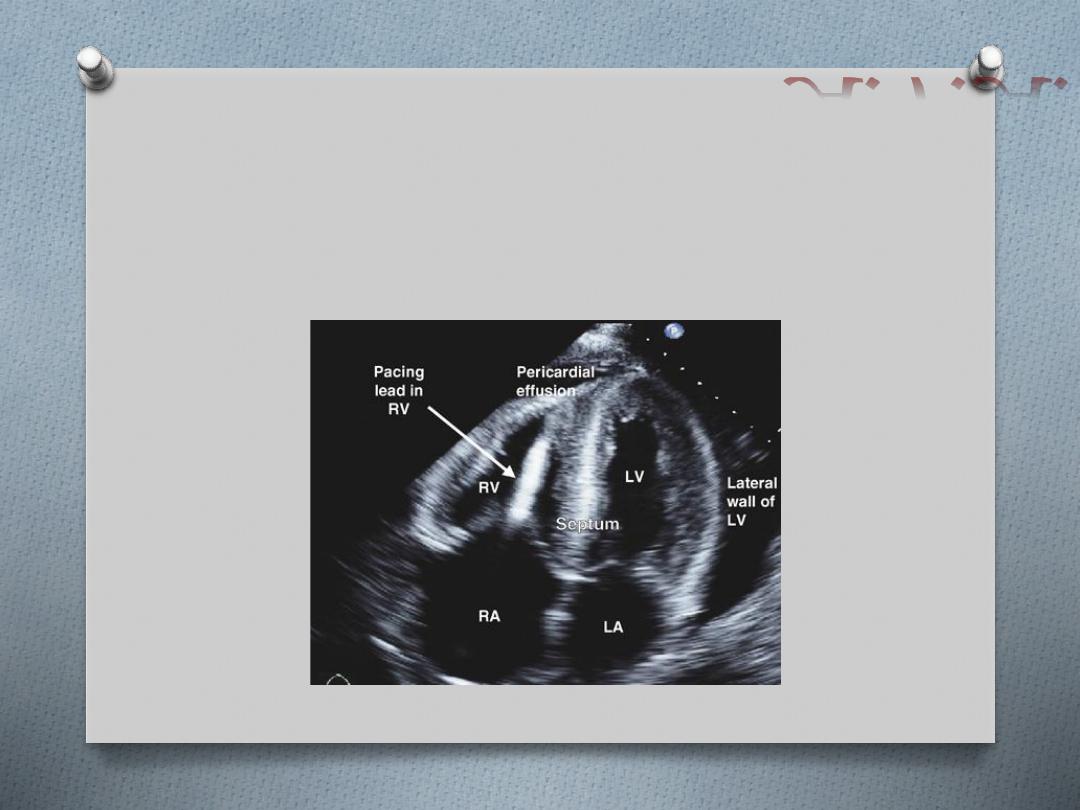
Echocardiography may reveal left ventricular dysfunction that is
sometimes regional (due to focal myocarditis)
O
Endomyocardial biopsy may show acute inflammation
O
Viral RNA can be measured from biopsy material using
polymerase chain reaction (PCR).
A.F.A.
Treatment
O
The underlying cause
must be identified, treated, eliminated or
avoided.
O
Bed rest
is recommended in the acute phase of the illness and
athletic activities should be avoided for 6 months.
O
Heart failure
should be treated conventionally with the use of
diuretics, ACE inhibitors/ARB, beta-blockers, spironolactone ± digoxin.
O
Antibiotics
should be administered immediately where appropriate.
O
NSAIDs
are contraindicated in the acute phase of the illness but may
be used in the late phase.
O
The use of
corticosteroids
is controversial and no studies have
demonstrated an improvement in left ventricular ejection fraction or
survival following their use.
O
The administration of
high-dose intravenous immunoglobulin
on the
other hand appears to be associated with a more rapid resolution of
the left ventricular dysfunction and improved survival
O
cardiomyopathies are defined as "a
heterogeneous group of diseases of the
myocardium associated with mechanical
and/or electrical dysfunction that usually
(but not invariably) exhibit inappropriate
ventricular hypertrophy or dilatation and are
due to a variety of causes that frequently are
genetic."
A.F.A.
O
DCM has a prevalence of 1 in 2500 and is
characterized by dilatation of the ventricular
chambers and systolic dysfunction with
preserved wall thickness.
is predominantly autosomal
dominant and can be associated with over
20 abnormal loci and genes .
O
Many of these are genes encoding
cytoskeletal or associated myocyte proteins
(
dystrophin in X-linked cardiomyopathy;
actin, desmin, troponin T, beta myosin heavy
chain, sarcoglycans, vinculin and lamin a/c
in autosomal dominant DCM
) .
A.F.A.
O
Sporadic DCM
can be caused by multiple
conditions:
O
myocarditis – Coxsackie, adenoviruses,
erythroviruses, HIV, bacteria, fungae,
mycobacteria, parasitic (Chagas’ disease)
O
toxins – alcohol, chemotherapy, metals
(cobalt, lead, mercury, arsenic)
O
autoimmune
O
endocrine
O
neuromuscular.
Clinical features
O
DCM can present with heart failure, cardiac
arrhythmias, conduction defects,
thromboembolism or sudden death.
O
Increasingly, evaluation of relatives of DCM
patients is allowing identification of early
asymptomatic disease, prior to the onset of
these complications.
A.F.A.
Investigations
O
Chest X-ray demonstrates generalized cardiac enlargement.
O
ECG may demonstrate diffuse non-specific ST segment and T
wave changes.
O
Sinus tachycardia, conduction abnormalities and arrhythmias (i.e.
atrial fibrillation, ventricular premature contractions or ventricular
tachycardia) are also seen.
O
Echocardiogram reveals dilatation of the left and/or right
ventricle with poor global contraction function .
O
Cardiac MR may demonstrate other aetiologies of left
ventricular dysfunction (e.g. previous myocardial infarction) or
demonstrate abnormal myocardial fibrosis .
O
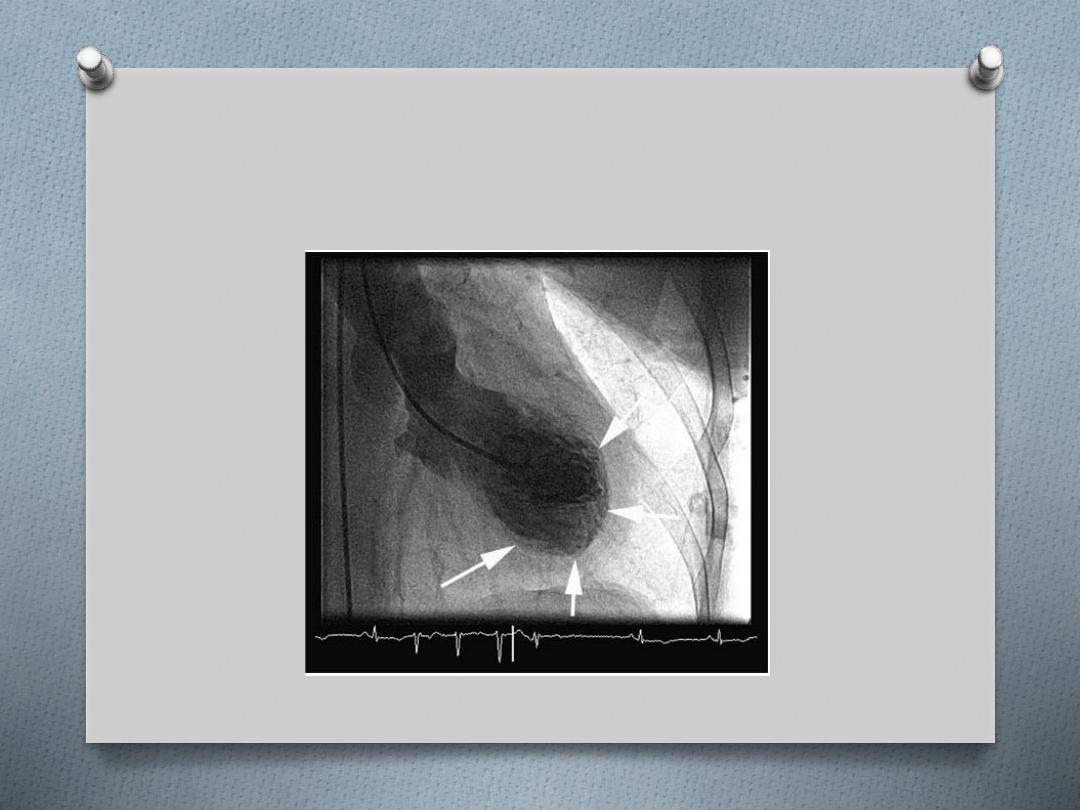
Coronary angiography should be performed to exclude
coronary artery disease in all individuals at risk (generally
patients > 40 years or younger if symptoms or risk factors are
present).
O
Biopsy is generally not indicated outside specialist care.
Treatment
O
Treatment consists of the conventional
management of heart failure with the
option of cardiac resynchronization therapy
and ICDs in patients with NYHA III/IV
grading.
O
Cardiac transplantation is appropriate for
certain patients.
A.F.A.
O
HCM includes a group of inherited conditions that
produce hypertrophy of the myocardium in the
absence of an alternate cause (e.g. aortic stenosis or
hypertension).
O
It is the most common cause of sudden cardiac
death in young people and affects 1 in 500 of the
population.
O
The majority of cases are familial autosomal
dominant, due to mutations in the genes encoding
sarcomeric proteins .
O
The most common causes of HCM are mutations of
the β-myosin heavy chain and myosin-binding protein
C.
Clinical features
O
HCM is characterized by:
O
variable myocardial hypertrophy frequently involving the
interventricular septum
O
and disorganization (‘disarray’) of cardiac myocytes and myofibrils.
O
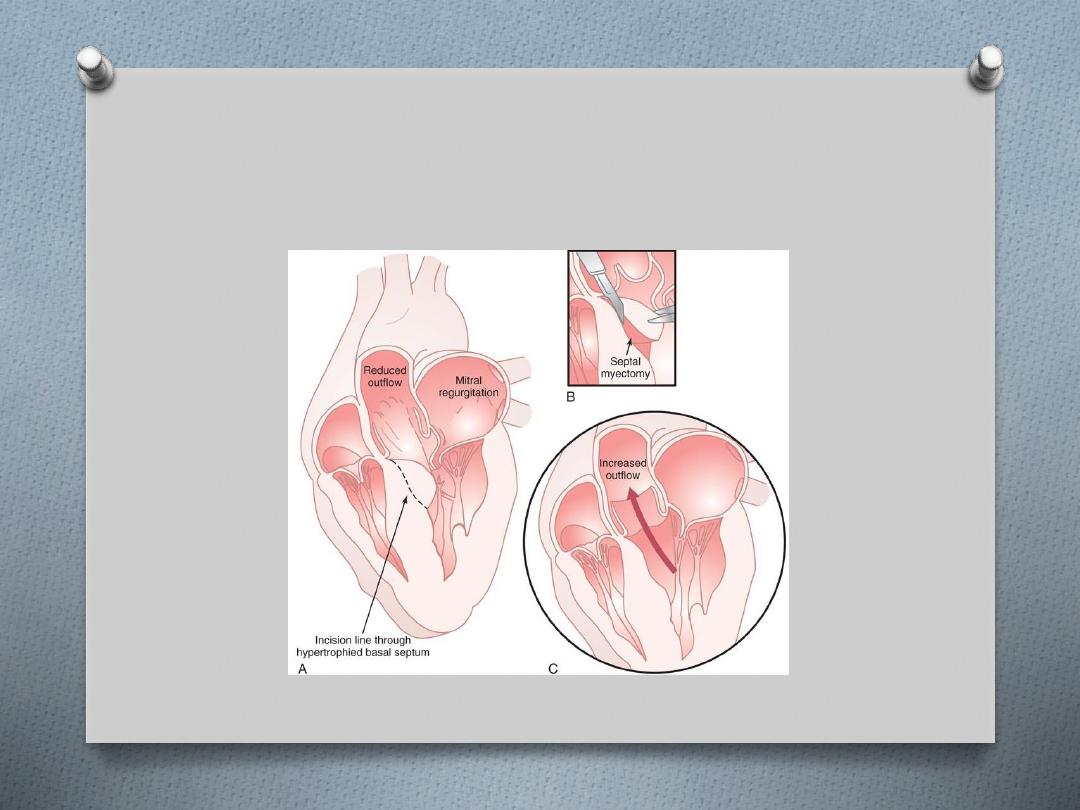
Twenty-five per cent
of patients have dynamic left ventricular
outflow tract obstruction due to the combined effects of
hypertrophy, systolic anterior motion (SAM) of the anterior mitral
valve leaflet and rapid ventricular ejection.
O
The salient clinical and morphological features of the disease vary
according to the underlying genetic mutation.
O
For example, marked hypertrophy is common with β myosin heavy
chain mutations whereas mutations in troponin T may be
associated with mild hypertrophy but a high risk of sudden death.
O
The hypertrophy may not manifest before completion of the
adolescent growth spurt, making the diagnosis in children difficult.
A.F.A.
Symptoms
O
many are
asymptomatic
and are detected through family screening of
an affected individual or following a routine ECG examination
O
chest pain, dyspnoea, syncope or pre-syncope
(typically with exertion),
cardiac arrhythmias
and
sudden death
are seen
O
sudden death occurs at any age but the highest rates (up to 6% per
annum) occur in adolescents or young adults.
O
dyspnoea occurs due to impaired relaxation of the heart muscle or
the left ventricular outflow tract obstruction that occurs in some
patients.
O
The systolic cavity remains small until the late stages of disease when
progressive dilatation may occur.
O
If a patient develops atrial fibrillation there is often a rapid deterioration
in clinical status due to the loss of atrial contraction and the tachycardia –
resulting in elevated left atrial pressure and acute pulmonary oedema.
A.F.A.
Signs
O
double apical pulsation
(forceful atrial contraction producing
a fourth heart sound)
O
jerky carotid pulse
because of rapid ejection and sudden
obstruction to left ventricular outflow during systole
O
ejection systolic murmur
due to left ventricular outflow
obstruction late in systole –
O
it can be increased by manoeuvres that decrease after-load,
e.g. standing or Valsalva,
O
and decreased by manoeuvres that increase after-load and
venous return, e.g. squatting
O
pan-systolic murmur
due to mitral regurgitation (secondary
to SAM)
O
fourth heart sound
(if not in AF).
Investigations
O
ECG abnormalities of HCM include left ventricular
hypertrophy, ST and T wave changes, and abnormal Q waves
especially in the infero-lateral leads.
O
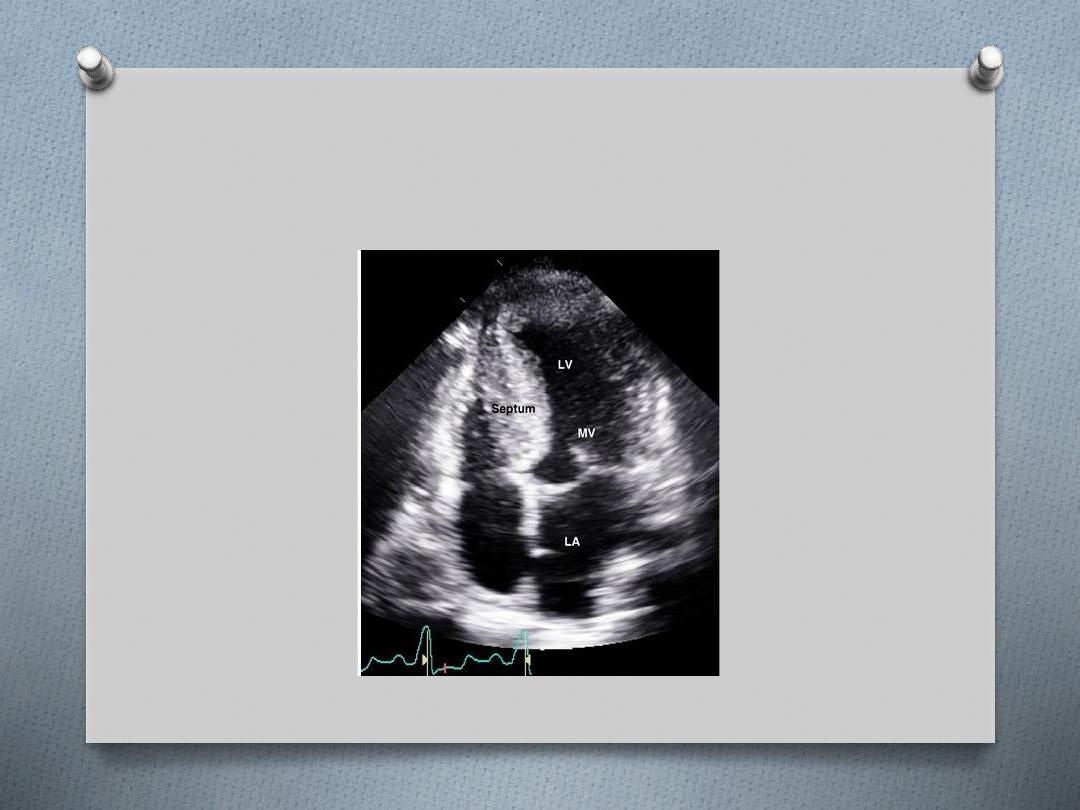
Echocardiography is usually diagnostic and in classical HCM
there is
asymmetric left ventricular hypertrophy
(involving the
septum more than the posterior wall),
systolic anterior
motion
of the mitral valve, and a vigorously contracting
ventricle .
O
Cardiac MR can detect both the hypertrophy but also
abnormal myocardial fibrosis .
O
Genetic analysis, where available, may confirm the diagnosis
and provide prognostic information for the patient and
relatives.
A.F.A.
Treatment
HCM
HCM with obstruction
HCM without obstruction
1.
BB
2.
BB +/- disopyramide if obstruction persist
3.
Diuretics for congestive symptom
4.
Verapamide in stead of disopyramide
5.
Surgical myectomy or alcohol septal ablation
6.
Dual chamber cardiac pacing
1.
BB &/or verapamil
2.
Diuretics for congestion
3.
Transplantation
A.F.A.
O
The management of HCM includes treatment of
symptoms and the prevention of sudden cardiac
death in the patient and relatives.
O
Risk factors for sudden death:
1.
massive left ventricular hypertrophy (> 30 mm on
echocardiography)
2.
family history of sudden cardiac death (< 50 years
old)
3.
non-sustained ventricular tachycardia on 24-hour
Holter monitoring
4.
prior unexplained syncope
5.
abnormal blood pressure response on exercise
(flat or hypotensive response).
O
The presence of these cardiac risk factors is
associated with an increased risk of sudden
death, and patients with one or more should
be assessed for implantable cardioverter–
defibrillator (ICD).
O
In patients in whom the risk is less,
amiodarone is an appropriate alternative.
A.F.A.
O
This is a rare condition in which there is normal or
decreased volume of both ventricles with bi-atrial
enlargement, normal wall thickness, normal cardiac
valves and impaired ventricular filling with restrictive
physiology but near normal systolic function.
O
The restrictive physiology produces symptoms and
signs of heart failure.
O
Conditions associated with this form of
cardiomyopathy include amyloidosis (commonest),
sarcoidosis,….
O
The idiopathic form of restrictive cardiomyopathy may
be familial.
Clinical features
O
Patients with restrictive cardiomyopathy may
present with dyspnoea, fatigue and embolic
symptoms.
O
On clinical examination there will be elevated
jugular venous pressure with diastolic collapse
(Friedreich’s sign) and elevation of venous
pressure with inspiration (Kussmaul’s sign),
hepatic enlargement, ascites and dependent
oedema.
O
Third and fourth heart sounds may be present.
O
Irrgular pulse (AF)
A.F.A.
Investigations
O
Chest X-ray may show pulmonary venous congestion.
O
The cardiac silhouette can be normal or show biatrial
enlargement.
O
ECG may demonstrate low-voltage QRS and ST segment and T
wave abnormalities.
O
Echocardiography shows a normal systolic ejection fraction but
there is diastolic dysfunction.
O
Cardiac MR may demonstrate abnormal myocardial fibrosis in
amyloidosis or sarcoidosis
.
O
Cardiac catheterization and haemodynamic studies may help
distinguish between restrictive cardiomyopathy and constrictive
pericarditis, although volume loading may be required.
O
Endomyocardial biopsy in contrast with other cardiomyopathies
is often useful in this condition and may permit a specific
diagnosis, such as amyloidosis, to be made.
Treatment
O
There is no specific treatment. Cardiac failure
and embolic manifestations should be treated.
O
Cardiac transplantation is necessary in some
severe cases, especially the idiopathic variety.
O
In primary amyloidosis combination therapy
with melphalan plus prednisolone with or
without colchicine may improve survival.
O
However, patients with cardiac amyloidosis have
a worse prognosis than those with other forms of
the disease, and the disease often recurs after
transplantation.
A.F.A.
O
In this condition, patches of the right ventricular myocardium
are replaced with fibrous and fatty tissue.
O
It is inherited as an autosomal dominant trait and has a
prevalence of approximately 10 per 100 000.
O
The dominant clinical problems are ventricular arrhythmias,
sudden death and right-sided cardiac failure.
O
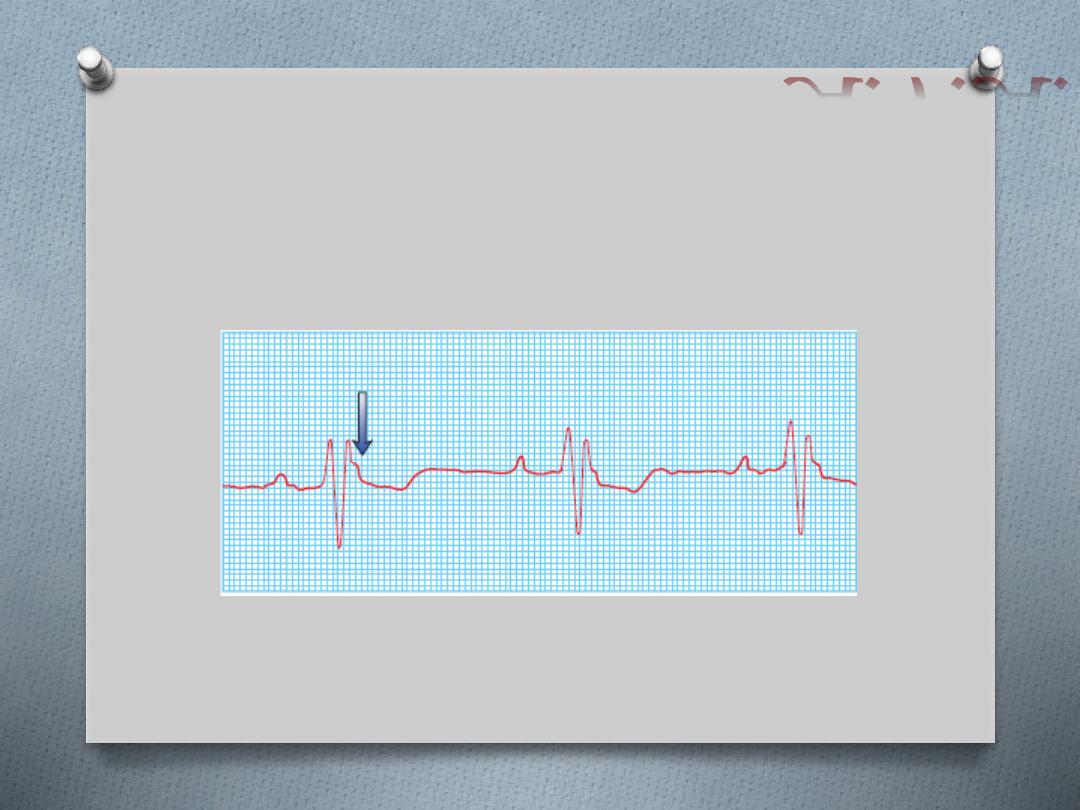
The ECG typically shows a slightly broadened QRS complex
and inverted T waves in the right precordial leads.
O
MRI is a useful diagnostic tool and is often used to screen the
first-degree relatives of affected individuals.
O
Patients at high risk of sudden death can be offered an ICD.
A.F.A.
Acquired cardiomyopathies
O
This is a recently described acute and
reversible cardiomyopathy that occurs in the
absence of coronary artery disease and is
usually triggered by profound psychological
stress.
O
It is more common in middle–old aged
women and classically affects the left
ventricular apex causing apical ballooning
A.F.A.
Peri-partum
cardiomyopathy
O
This rare condition affects women in the last
trimester of pregnancy or within 5 months of
delivery.
O
It presents as a dilated cardiomyopathy, is more
common in obese, multiparous women over 30
years old and is associated with preeclampsia.
O
Nearly half of patients will recover to normal
function within 6 months but in some patients it
can causes progressive heart failure and sudden
death.
Alcoholic CMP
O
Long-term exposure to alcohol is an
important preventable cause of DCM.
O
The risk is seen when more than 90 g of
alcohol (about seven standard alcoholic
drinks) is consumed daily for more than 5
years; lower exposure may lead to
cardiomyopathy in women.
O
Abstinence from alcohol may lead to
sustained improvements in ventricular
function.
A.F.A.
Tachycardia
cardiomyopathy
O
Prolonged periods of supraventricular or
ventricular tachycardia will lead to dilated
cardiomyopathy.
O
Cardioversion and ablation may be
necessary to restore sinus rhythm and allow
for recovery of cardiac function.
A.F.A.
A.F.A.