
Acute heart failure (AHF) occurs with the
rapid onset of symptoms and signs of heart
failure secondary to abnormal cardiac
function, causing elevated cardiac filling
pressures.
This causes severe dyspnoea and fluid
accumulates in the interstition and alveolar
spaces of the lung (pulmonary oedema).
AHF has a poor prognosis with a rate of death
or rehospitalization of 35% within 60 days.

Poor prognostic indicators include
◦
a high (> 16 mmHg) pulmonary capillary wedge
pressure (PCWP),
◦
low serum sodium concentration,
◦
increased left ventricular end-diastolic dimension
on echo
Patients with
ischaemic heart disease
present with an
acute coronary syndrome or develop a complication of a
myocardial infarct, e.g. papillary muscle rupture or
ventricular septal defect requiring surgical intervention.
Patients with
valvular heart disease
also present with AHF
due to valvular regurgitation in endocarditis or prosthetic
valve thrombosis.
Patients with
hypertension
present with episodes of ‘flash’
pulmonary oedema despite preserved left ventricular
systolic function.
In both
acute and chronic kidney disease
fluid overload
and a reduced renal excretion will produce pulmonary
oedema.
Atrial fibrillation
is frequently associated with AHF and
may require emergency cardioversion.

Initial investigations performed in the emergency
room should include:
◦
a 12-lead ECG
for acute coronary syndromes, left
ventricular hypertrophy, atrial fibrillation, chamber
enlargement, left bundle branch block
◦
a chest X-ray
(cardiomegaly, pulmonary oedema, pleural
effusion, non-cardiac disease)
◦
blood investigations
(serum creatinine and electrolytes,
full blood count, blood glucose, cardiac enzymes and
troponin)
plasma BNP or NTproBNP
(BNP > 100 pg/ml or NTproBNP >
300 pg/ml) indicates heart failure
◦
transthoracic echocardiography
should be performed
without delay to confirm the diagnosis of heart failure
and possibly identify the cause.

Patients with AHF should be managed in a
high-care area with regular measurements of
temperature, heart rate, blood pressure and
cardiac monitoring.
All patients require prophylactic
anticoagulation with low molecular weigh
heparin, e.g. enoxaparin 1 mg/kg s.c. daily.
This is urgent:
Sit the patient up
in order to reduce pulmonary
congestion.
Give oxygen
(high-flow, high-concentration).
◦
Noninvasive positive pressure ventilation (continuous
positive airways pressure (CPAP) of 5–10 mmHg) by a tight-
fitting facemask results in a more rapid improvement in the
patient’s clinical state.
Administer nitrates
, such as i.v. glyceryl trinitrate 10–
200 μg/min or buccal glyceryl trinitrate 2–5 mg,
titrated upwards every 10 minutes, until clinical
improvement occurs or systolic BP falls to < 110
mmHg.
Administer a
loop diuretic
such as furosemide 50–
100 mg i.v.
an intravenous bolus of Morphine
2.5 to 5 mg as
soon as an intravenous line is inserted; the same
doses can be repeated as required.
◦
Morphine should be used cautiously or avoided in the
presence of hypotension, bradycardia, advanced
atrioventricular block, or carbon dioxide retention
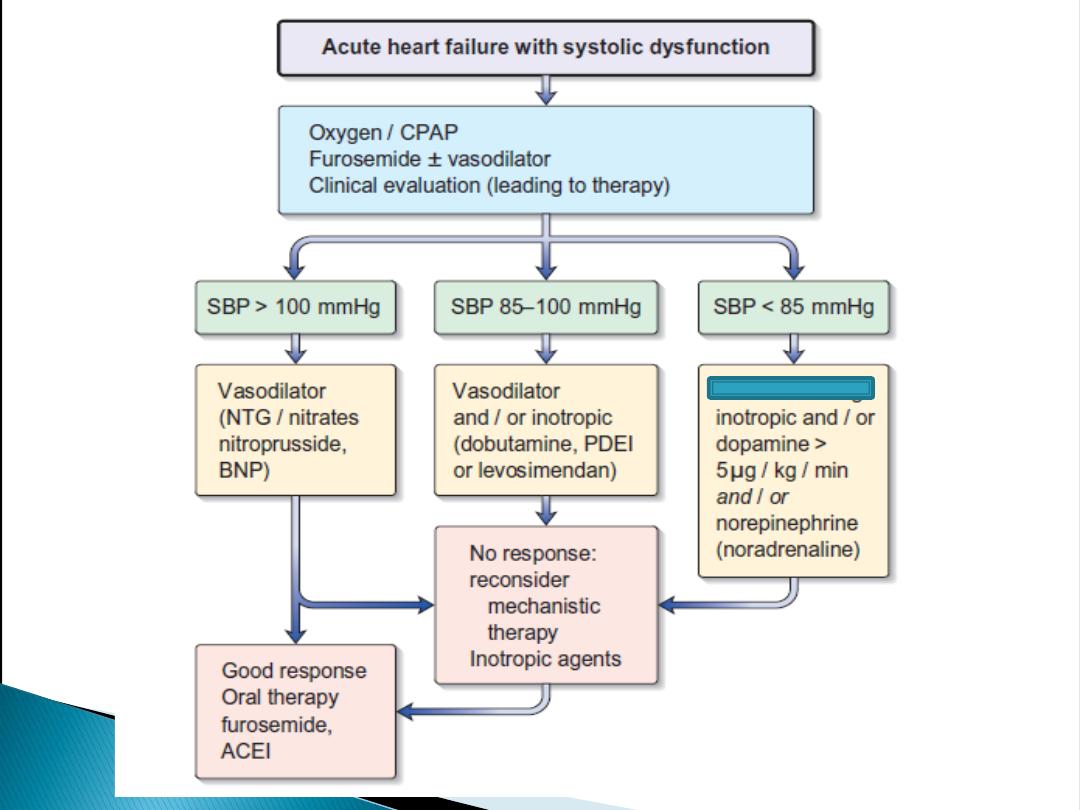
Vasodilators
◦
Nitrates
◦
Sodium Nitroprusside
◦
BNP, nestiride
Inotropes with Vasodilatory Properties
◦
Dopamine
◦
Dobutamine
◦
phosphodiesterase 3 inhibitor , milrinone
◦
Levosimendan is a calcium sensitizer and ATP-
dependent potassium channel opener that has positive
inotropic and vasodilatory effect
Vasopressor Agents
◦
vasopressin antagonists , tolvaptan ?
◦
NA

Inotropic support with dobutamine,
phosphodiesterase inhibitors or
levosimendan can be added in patients who
do not respond to the initial therapy .
If blood pressure is low use noradrenaline
(norepinephrine).
Patients with profound hypotension may
require inotropes and vasopressors to
improve the haemodynamic status and
alleviate symptoms, but these have not been
shown to improve mortality.
Definition
Cor pulmonale, often referred to as
pulmonary heart disease
, is defined as
dilation and hypertrophy of the right ventricle
in response to diseases of the pulmonary
vasculature and/or lung parenchyma.

Although chronic obstructive pulmonary
disease (COPD) and chronic bronchitis are
responsible for approximately 50% of the
cases of cor pulmonale , any disease that
affects the pulmonary vasculature or
parenchyma can lead to cor pulmonale.
Once patients with chronic pulmonary or
pulmonary vascular disease develop cor
pulmonale, the prognosis worsens.
Although many conditions can lead to cor
pulmonale, the common pathophysiologic
mechanism in each case is pulmonary
hypertension that is sufficient to lead to RV
dilation, with or without the development of
concomitant RV hypertrophy.
The symptoms of chronic cor pulmonale generally
are related to the underlying pulmonary disorder.
Dyspnea
, the most common symptom
Tussive or effort-related syncope
may occur
because of the inability of the RV to deliver blood
adequately to the left side of the heart.
Central chest pain
Abdominal pain and ascites
that occur with cor
pulmonale are similar to the right-heart failure
that ensues in chronic HF.
Lower-extremity edema
may occur secondary to
neurohormonal activation, elevated RV filling
pressures, or increased levels of carbon dioxide
and hypoxemia, which can lead to peripheral
vasodilation and edema formation.

Many of the signs encountered in cor pulmonale are also
present in HF patients with a depressed EF, including
tachypnea, elevated jugular venous pressures,
hepatomegaly, and lower-extremity edema
.
Patients may have
prominent
v
waves
in the jugular
venous pulse as a result of tricuspid regurgitation.
Other cardiovascular signs include an
RV heave
palpable
along the left sternal border or in the epigastrium.
The increase in intensity of the holosystolic murmur of
tricuspid regurgitation
with inspiration ("Carvallo's sign")
may be lost eventually as RV failure worsens.
Loud P2
which is sometimes palpable
Cyanosis
is a late finding in cor pulmonale and is
secondary to a low cardiac output with systemic
vasoconstriction and ventilation-perfusion mismatches in
the lung.
The ECG
in severe pulmonary hypertension shows
P pulmonale,
right axis deviation, and RV hypertrophy.
Radiographic examination of the chest
may show enlargement of
the main pulmonary artery, the hilar vessels, and the descending
right pulmonary artery.
Spirometry and lung volumes
can identify obstructive and/or
restrictive defects indicative of parenchymal lung diseases;
arterial blood gases
can demonstrate hypoxemia and/or
hypercapnia.
Spiral computed tomography (CT) scans of the chest
are useful in
diagnosing acute thromboembolic disease;
◦
however, ventilation-perfusion lung scanning remains best suited for
diagnosing
chronic thromboembolic disease
.
A high-resolution CT scan of the chest
can identify interstitial
lung disease.
Two-dimensional echocardiography
is useful for measuring RV
thickness and chamber dimensions as well as the anatomy of the
pulmonary and tricuspid valves.

The primary treatment goal of cor pulmonale is to
target the underlying
pulmonary disease
, since this will decrease pulmonary vascular
resistance and lessen RV afterload.
General principles
of treatment include decreasing work of breathing by
using
noninvasive mechanical ventilation
and
bronchodilation
, as well as
treating any underlying
infection
.
Adequate oxygenation
(oxygen saturation 90–92%)
and correcting
respiratory acidosis
are vital for decreasing pulmonary vascular
resistance.
Patients should be
transfused
if they are anemic, and
phlebotomy
may
be considered in extreme cases of polycythemia.
Diuretics
are effective in RV failure, and indications are similar to those
for chronic HF.
Digoxin
is of uncertain benefit in the treatment of cor pulmonale and
may lead to arrhythmias in the setting of tissue hypoxemia and acidosis.
Therefore, if digoxin is administered, it should be given at low doses
and monitored carefully.
Pulmonary vasodilators
can effectively improve symptoms through
modest reduction of pulmonary pressures and RV afterload when
isolated pulmonary arterial hypertension is present.
