
11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
1/12
Mitral valve disease
Mitral stenosis
Aetiology and pathophysiology
Mitral stenosis is almost always rheumatic in origin, although in older people it can be caused by heavy calcification of the
mitral valve apparatus. There is also a rare form of congenital mitral stenosis.
In rheumatic mitral stenosis, the mitral valve orifice is slowly diminished by progressive fibrosis, calcification of the valve leaflets,
and fusion of the cusps and subvalvular apparatus. The flow of blood from LA to LV is restricted and left atrial pressure rises,
leading to pulmonary venous congestion and breathlessness. There is dilatation and hypertrophy of the LA, and left ventricular
filling becomes more dependent on left atrial contraction.
Any increase in heart rate shortens diastole when the mitral valve is open and produces a further rise in left atrial pressure.
Situations that demand an increase in cardiac output also increase left atrial pressure, so exercise and pregnancy are poorly
tolerated.
The mitral valve orifice is normally about 5 cm
2
in diastole and may be reduced to 1 cm
2
in severe mitral stenosis. Patients usually
remain asymptomatic until the stenosis is less than 2 cm
2
. Reduced lung compliance, due to chronic pulmonary venous
congestion, contributes to breathlessness, and a low cardiac output may cause fatigue.
Atrial fibrillation due to progressive dilatation of the LA is very common. Its onset often precipitates pulmonary oedema because
the accompanying tachycardia and loss of atrial contraction lead to marked haemodynamic deterioration with a rapid rise in
left atrial pressure. In contrast, a more gradual rise in left atrial pressure tends to cause an increase in pulmonary vascular
resistance, which leads to pulmonary hypertension that may protect the patient from pulmonary oedema. Pulmonary
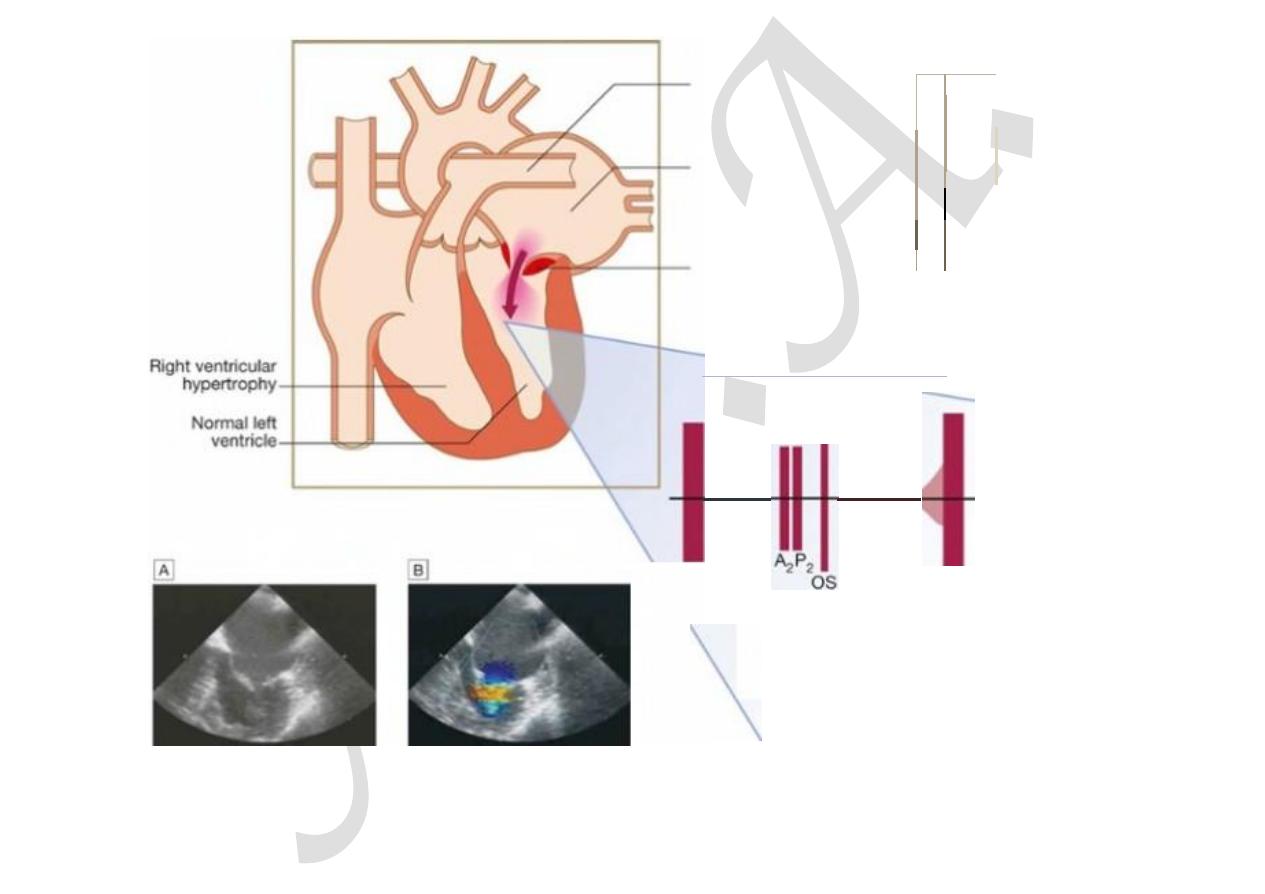
hypertension leads to right ventricular hypertrophy and dilatation, tricuspid regurgitation and right heart failure.
Fewer than 20% of patients remain in sinus rhythm; many of these have a small fibrotic LA and severe pulmonary hypertension.

11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
2/12
Clinical features
Effort-related dyspnoea is usually the dominant symptom (
Box 18.98
). Exercise tolerance typically diminishes very slowly over
many years and patients often do not appreciate the extent of their disability. Eventually, symptoms occur at rest. Acute pulmonary
oedema or pulmonary hypertension can lead to haemoptysis. All patients with mitral stenosis, and particularly those with atrial
fibrillation, are at risk from left atrial thrombosis and systemic thromboembolism. Prior to the advent of anticoagulant therapy,
emboli caused one-quarter of all deaths.
18.98 Clinical features (and their causes) in mitral stenosis
Symptoms
•
Breathlessness (pulmonary congestion)
•
Fatigue (low cardiac output)
•
Oedema, ascites (right heart failure)
•
Palpitation (atrial fibrillation)
•
Haemoptysis (pulmonary congestion, pulmonary embolism)
•
Cough (pulmonary congestion)
•
Chest pain (pulmonary hypertension)
•
Thromboembolic complications (e.g. stroke, ischaemic limb)
Signs
•
Atrial fibrillation
•
Mitral facies
•
Auscultation
Loud first heart sound, opening snap
Mid-diastolic murmur
•
Crepitations, pulmonary oedema, effusions (raised pulmonary capillary pressure)

11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
3/12
•
RV heave, loud P
2
(pulmonary hypertension)
The physical signs of mitral stenosis are often found before symptoms develop and their recognition is of particular importance
in pregnancy. The forces that open and close the mitral valve increase as left atrial pressure rises. The first heart sound (S1) is
therefore loud and can be palpable (tapping apex beat). An opening snap may be audible and moves closer to the second sound
(S2) as the stenosis becomes more severe and left atrial pressure rises. However, the first heart sound and opening snap may be
inaudible if the valve is heavily calcified.
Turbulent flow produces the characteristic low-pitched mid-diastolic murmur and sometimes a thrill (
Fig. 18.87
). The murmur
is accentuated by exercise and during atrial systole (pre-systolic accentuation). Early in the disease, a pre-systolic murmur may
be the only auscultatory abnormality but, in patients with symptoms, the murmur extends from the opening snap to the first heart
sound. Coexisting mitral regurgitation causes a pansystolic murmur that radiates towards the axilla.
11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
4/12
n
p
ar
Di
at
St
m
Lou
( o s
l
cteas
ed
mm
H
g
ulmonary
LV
tery
p
r
ess
u
r
e
1
00
l
ated
l
e
ft
75
num
50
25
O.astotic
enosed gradient
,tral va
l
ve
0
across valve
MDM
d Loud
R
o
ll p
a
t
ien
t
towards left to
hea
r
murm
u
r best
l
w
-
pi
t
c
h
ed
,
use bell of
tet
h
oscope a! ape
x
)
F I G.
1 8 . 8 7
Mitral stenosis: murmur and the diastolic pressure gradient between LA and LV. (Mea…
Pulmonary hypertension may ultimately lead to right ventricular hypertrophy and dilatation with secondary tricuspid
11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
5/12
regurgitation, which causes a systolic murmur and giant ‘v waves’ in the venous pulse.
Investigations
The ECG may show either atrial fibrillation or bifid P waves (P mitrale) associated with left atrial hypertrophy (
Box 18.99
). A
typical chest X-ray is shown in
Figure 18.9
(
p. 535
). Doppler echocardiography provides the definitive evaluation of mitral
stenosis (see
Fig. 18.87
). Cardiac catheterisation is used to assess coexisting conditions.
18.99 Investigations in mitral stenosis
ECG
•
Right ventricular hypertrophy: tall R
waves in V
1
–V
3
•
P mitrale or atrial fibrillation
Chest X-ray
•
Enlarged LA and appendage
•
Signs of pulmonary venous
congestion
Echo
•
Thickened immobile cusps
•
Reduced valve area
•
Enlarged LA
•
Reduced rate of diastolic filling
of LV
Doppler
•
Pressure gradient across mitral valve
•
Pulmonary artery pressure
•
Left ventricular function
Cardiac catheterisation
•
Coronary artery disease
•
Pulmonary artery pressure
•
Mitral stenosis and
regurgitation

11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
6/12
Management
Patients with minor symptoms should be treated medically. Intervention by balloon valvuloplasty, mitral valvotomy or mitral
valve replacement should be considered if the patient remains symptomatic despite medical treatment or if pulmonary
hypertension develops.
Medical management
This consists of anticoagulation to reduce the risk of systemic embolism, ventricular rate control (digoxin, β-blockers or rate-
limiting calcium antagonists) in atrial fibrillation, and diuretic therapy to control pulmonary congestion. Antibiotic prophylaxis
against infective endocarditis is no longer routinely recommended.
Mitral ba loon valvuloplasty and valve replacement
Valvuloplasty is the treatment of choice if specific criteria are fulfilled (
Box 18.100
and
Fig. 18.67
,
p. 587
), although
surgical closed or open mitral valvotomy is an acceptable alternative. Patients who have undergone mitral valvuloplasty or
valvotomy should be followed up at 1–2-yearly intervals because re-stenosis may occur. Clinical symptoms and signs are a guide
to the severity of mitral re-stenosis but Doppler echocardiography provides a more accurate assessment.
18.100 Criteria for mitral valvuloplasty*
•
Significant symptoms
•
Isolated mitral stenosis
•
No (or trivial) mitral regurgitation
•
Mobile, non-calcified valve/subvalve apparatus on echo
•
LA free of thrombus
Valve replacement is indicated if there is substantial mitral reflux or if the valve is rigid and calcified (
p. 629
).

11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
7/12
Mitral regurgitation
Aetiology and pathophysiology
Rheumatic disease is the principal cause in countries where rheumatic fever is common, but elsewhere, including in the UK,
other causes are more important (
Box 18.101
). Mitral regurgitation may also follow mitral valvotomy or valvuloplasty.
18.101 Causes of mitral regurgitation
•
Mitral valve prolapse
•
Dilatation of the LV and mitral valve ring (e.g. coronary artery disease, cardiomyopathy)
•
Damage to valve cusps and chordae (e.g. rheumatic heart disease, endocarditis)
•
Ischaemia or infarction of the papillary muscle
•
Myocardial infarction
Chronic mitral regurgitation causes gradual dilatation of the LA with little increase in pressure and therefore relatively few
symptoms. Nevertheless, the LV dilates slowly and the left ventricular diastolic and left atrial pressures gradually increase as a
result of chronic volume overload of the LV. In contrast, acute mitral regurgitation causes a rapid rise in left atrial pressure
(because left atrial compliance is normal) and marked symptomatic deterioration.
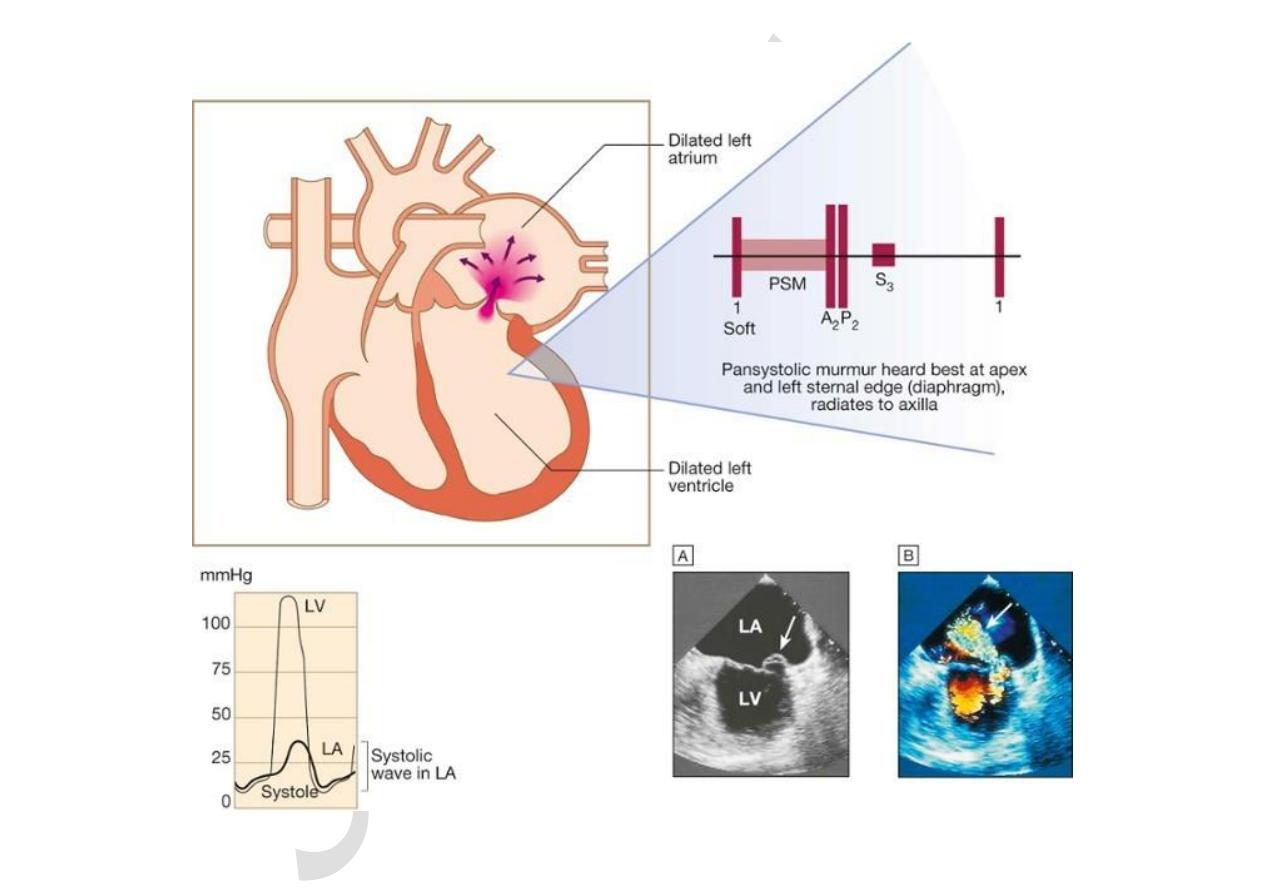
Mitral valve prolapse
This is also known as ‘floppy’ mitral valve and is one of the more common causes of mild mitral regurgitation (
Fig. 18.88
). It
is caused by congenital anomalies or degenerative myxomatous changes, and is sometimes a feature of connective tissue disorders
such as Marfan’s syndrome (
p. 603
).
11/18/2015
Diseases of the heart valves | Davidson
’s Principles and Practice of…
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
… 8/12

data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
… 99/12
F I G.
1 8 . 8 8
Mitral regurgitation: murmur and systolic wave in left atrial pressure. The first sound i…
In its mildest forms, the valve remains competent but bulges back into the atrium during systole, causing a mid-systolic click but
no murmur. In the presence of a regurgitant valve, the click is followed by a late systolic murmur, which lengthens as the
regurgitation becomes more severe. A click is not always audible and the physical signs may vary with both posture and respiration.
Progressive elongation of the chordae tendineae leads to increasing mitral regurgitation, and if chordal rupture occurs,
regurgitation suddenly becomes severe. This is rare before the fifth or sixth decade of life.
Mitral valve prolapse is associated with a variety of typically benign arrhythmias, atypical chest pain and a very small risk of
embolic stroke or TIA. Nevertheless, the overall long-term prognosis is good.
Other causes of mitral regurgitation
Mitral valve function depends on the chordae tendineae and their papillary muscles; dilatation of the LV distorts the geometry of
these and may cause mitral regurgitation (see
Box 18.101
). Dilated cardiomyopathy and heart failure from coronary artery disease
are common causes of so-called ‘functional’ mitral regurgitation. Endocarditis is an important cause of acute mitral regurgitation.
Clinical features
Symptoms depend on how suddenly the regurgitation develops (
Box 18.102
). Chronic mitral regurgitation produces a
symptom complex that is similar to that of mitral stenosis, but sudden-onset mitral regurgitation usually presents with acute
pulmonary oedema.
18.102 Clinical features (and their causes) in mitral regurgitation
Symptoms
•
Dyspnoea (pulmonary venous congestion)
•
Fatigue (low cardiac output)

data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
1010/12
•
Palpitation (atrial fibrillation, increased stroke volume)
•
Oedema, ascites (right heart failure)
Signs
•
Atrial fibrillation/flutter
•
Cardiomegaly: displaced hyperdynamic apex beat
•
Apical pansystolic murmur ± thrill
•
Soft S1, apical S3
•
Signs of pulmonary venous congestion (crepitations, pulmonary oedema, effusions)
•
Signs of pulmonary hypertension and right heart failure
The regurgitant jet causes an apical systolic murmur (see
Fig. 18.88
), which radiates into the axilla and may be accompanied
by a thrill. Increased forward flow through the mitral valve causes a loud third heart sound and even a short mid-diastolic
murmur. The apex beat feels active and rocking due to left ventricular volume overload and is usually displaced to the left as a
result of left ventricular dilatation.
Investigations
Atrial fibrillation is common, as a consequence of atrial dilatation. At cardiac catheterisation (
Box 18.103
), the severity of
mitral regurgitation can be assessed by left ventriculography and by the size of the v (systolic) waves in the left atrial or
pulmonary artery wedge pressure trace.
18.103 Investigations in mitral regurgitation
ECG
•
Left atrial hypertrophy (if not in atrial fibrillation)
•
Left ventricular hypertrophy
data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
1111/12
Chest X-ray
•
Enlarged LA
•
Enlarged LV
•
Pulmonary venous congestion
•
Pulmonary oedema (if acute)
Echo
•
Dilated LA, LV
•
Dynamic LV (unless myocardial dysfunction predominates)
•
Structural abnormalities of mitral valve (e.g. prolapse)
Doppler
•
Detects and quantifies regurgitation
Cardiac catheterisation
•
Dilated LA, dilated LV, mitral regurgitation
•
Pulmonary hypertension
•
Coexisting coronary artery disease
Management
Mitral regurgitation of moderate severity can be treated medically (
Box 18.104
). In all patients with mitral regurgitation,
high afterload may worsen the degree of regurgitation, and hypertension should be treated with vasodilators, such as ACE
inhibitors. Patients should be reviewed at regular intervals because worsening symptoms, progressive cardiomegaly or
echocardiographic evidence of deteriorating left ventricular function are indications for mitral valve replacement or repair.
Mitral valve repair is used to treat mitral valve prolapse and offers many advantages when compared to mitral valve

data:text/html;charset=utf-8,%3Ch2%20id%3D%22117c39178bfb408990c0e19ba018a4bc%22%20style%3D%22margin%3A%201.3em%200px%200.5em%3B%20padding%3A%200px%3B%20border%3A%200px%3B%20font-fa
…
1212/12
replacement, such that it is now advocated for severe regurgitation, even in asymptomatic patients, because results are excellent
and early repair prevents irreversible left ventricular damage. Mitral regurgitation often accompanies the ventricular dilatation
and dysfunction that are concomitants of coronary artery disease. If such patients are to undergo coronary bypass graft surgery, it
is common practice to repair the valve and restore mitral valve function by inserting an annuloplasty ring to overcome annular
dilatation and to bring the valve leaflets closer together. It can be difficult, however, to determine whether it is the ventricular
dilatation or the mitral regurgitation that is the predominant problem. If ventricular dilatation is the underlying cause of mitral
regurgitation, then mitral valve repair or replacement may actually worsen ventricular function, as the ventricle can no longer
empty into the low-pressure LA.
18.104 Medical management of mitral regurgitation
•
Diuretics
•
Vasodilators, e.g. ACE inhibitors
•
Digoxin if atrial fibrillation is present
•
Anticoagulants if atrial fibrillation is present
