
Appendix
It is located at the terminal end of the caecum where three taeniae join, about 2 cm below the
ileocaecal orifice. Usually, around 5-10 cm in size but can be varible. Size of its lumen is that of
matchstick.
Diameter of appendix is 3-8 mm; diameter of lumen is 1-3 mm.
Mesoappendix is extension of the mesentery contains appendicular artery, a branch of ileocolic
artery. Often an accessory appendicular artery may be present.
Thrombosis of these vessels leads to gangrenous appendicitis.
Most common position is retrocaecal (75%) , pelvic (21%). Preileal— (1%) Postileal
Paracaecal Subcaecal Subhepatic
Often it may be in subserosal plane leading to difficult dissection during appendicectomy.
In situs inversus appendix is on the left side.
Mucosa of appendix is lined by columnar cells with crypts.
Submucosa contains numerous lymphatic aggregations (follicles) (‘abdominal Tonsil’).
Opening of the appendix into caecum is guarded by ‘valve of Geralch’.
ACUTE APPENDICITIS
Aetiology;- It is common in young males. - It is common in white races.
Fibre rich diet prevents appendicitis. Less fibre diet increases chance of appendicitis.
It is common in May and August—often called as epidemic appendicitis.
Viral infection may cause mucosal oedema and inflammation which later gets infected by
bacteria causing appendicitis.
Family history may be relevant in 30% of appendicitis in children with appendicitis
occurring in first degree relatives.
Obstruction of the lumen of appendix causing obstructive appendicitis.
Blockage occurs due to—faecoliths, stricture, foreign body, round worm or threadworm.
Adhesions and kinking—carcinoma caecum near the base, ileocaecal Crohn’s disease.
Distal colonic obstruction.
Abuse of purgatives. Faecolith is the most common cause.

Organisms:
E. Coli , enterococci, streptococci, Anaerobic streptococci, Cl. welchii, bacteroides.
Pseudoappendicitis is appendicitis due to acute ileitis following Yersinia infection.
It is often due to Crohn’s disease.
Types
1. Acute nonobstructive appendicitis (catarrhal):
Inflammation of mucous membrane occurs with redness, oedema
and haemorrhages which may go for following courses:
Resolution. Ulceration. Fibrosis. Suppuration. Recurrent appendicitis.
Gangrene—rare initially in nonobstructive type but later can occur. Peritonitis.
2. Acute obstructive appendicitis:-pus collects in the blocked lumen
of appendix which is blackish, Gangrenous, oedematous and rapidly progresses leading to
perforation either at the tip or at the base of appendix. This leads to peritonitis, formation of
appendicular abscess or pelvic abscess. Most often, there will be thrombosis of the appendicular
artery.
3. Recurrent appendicitis: Repeated attacks of nonobstructive appendicitis leads to fibrosis,
adhesions causing recurrent appendicitis.
4. Subacute appendicitis is milder form of acute appendicitis.
5. Stump appendicitis is retained long stump of appendix after commonly laparoscopic
appendicitomy.
Clinical Features
It is rare before the age of two, common in children and other age groups.
1- Pain: It is the earliest symptom.
Visceral pain starts around the Umbilicus due to distension of appendix, later after few
hours, somatic pain occurs in right iliac fossa due to irritation of parietal peritoneum due
to inflamed appendix.
Pain eventually becomes severe and diffuse which signifies spread of Infection into the
general peritoneal cavity.

2- Vomiting: Due to reflex pylorospasm.
3-Constipation is the usual feature but diarrhoea can occur if appendix is in postileal or pelvic
positions.
4- Fever, tachycardia, foetor oris are other features.
5- Urinary frequency: Inflamed appendix may come in contact with Bladder And can cause
bladder irritation.
Signs ;-
1- Tenderness and rebound tenderness at McBurney’s point in right Iliac Fossa (release sign—
Blumberg’s sign) are typical.
2-Rovsing’s sign: On pressing left iliac fossa, pain occurs in right iliac
fossa which is due to shift of bowel loops which irritates the parietal peritoneum.
3- Hyperextension (in case of retrocaecal appendix—Cope’s psoas test)
Or internal rotation (in case of pelvic appendix—obturator test) of Right Hip Causes
pain in right iliac fossa due to irritation of psoas muscle and obturator internus muscle
respectively.
4-Baldwing’s test is positive in retrocaecal appendix—when legs are lifted off the bed
with knee extended, the patient complains of pain while pressing over the flanks.
5- P/R examination shows tenderness in right side of the rectum.
6-Hyperaesthesia in ‘Sherren’s triangle’. This triangle is formed by Anterosuperior iliac spine,
umbilicus, pubic symphysis.
Often infection gets localised by omentum, dilated ileum and parietalperitoneum leading to
appendicular mass.Often suppuration occurs in the localised area resulting in appendicular
abscess.
Acute appendicitis in infancy:
it is rare, when it occurs, it has got 80% chances of perforation with high mortality .

Acute appendicitis in children:
Here localisation is not present, and so peritonitis occurs Early.
It requires early surgery. Dehydration, septicaemia are common.
In elderly: Gangrene and perforation are common.
Because of lax abdominal wall, localisation is poor and so peritonitis sets in early.
In pregnancy: Incidence is 1 in 2,000 pregnancies.
It is more common in 1st and 2
nd
trimesters.
Appendix shifts to upper abdomen. So pain is higher and more lateral.
Rebound tenderness and guarding may not be evident.
TC will be very high with neutrophilia.
Risk of premature labour is 15%.
Foetal death in early appendicitis is 5% but becomes 29% once appendix perforates in
Pregnancy.
After 6 months, maternal mortality increases by 10 times than usual and also leads to
premature labour.
Appendicitis is the most common non-gynaecologic surgical emergency during pregnancy.
Incidence of perforation is highest in 3rd trimester.
Surgery is the treatment.
Differential diagnosis
GIT =( Perforated peptic ulcer -Acute cholecystitis- Enterocolitis - Crohn’s disease
Acute pancreatitis -Meckel’s diverticulitis - Typhlitis
URINARY=( Right ureteric colic - Right acute pyelonephritis
CHILDREN= Mesenteric lymphadenitis - Intussusception - Roundworm colic
RESPIRATORY= Lobar pneumonia
METABOLIC= Acute crisis of porphyria -Diabetic abdomen.

Differential diagnosis in females
Ruptured ectopic gestation
Mittelschmerz rupture of ovarian follicle during midmenstrual period
Ovarian cyst torsion
Salpingo-oophoritis
Differential diagnosis in elderly
Acute diverticulitis
Carcinoma caecum—acute features
Mesenteric ischaemia
Intestinal obstruction
Aortic aneurysm leak
Crohn‘s disease
Sequelae of acute appendicitis
1- Resorption
2-Relapse and recurrent appendicitis
3-Appendicular mass
4-Appendicular abscess
5-Perforation—has got 20% mortality
6-Peritonitis, septicaemia
7-Portal pyaemia
8- Intestinal obstruction due to obstructive ileus, inflammatory adhesion, formation of band
between appendix and omentum or between appendix and small bowel.
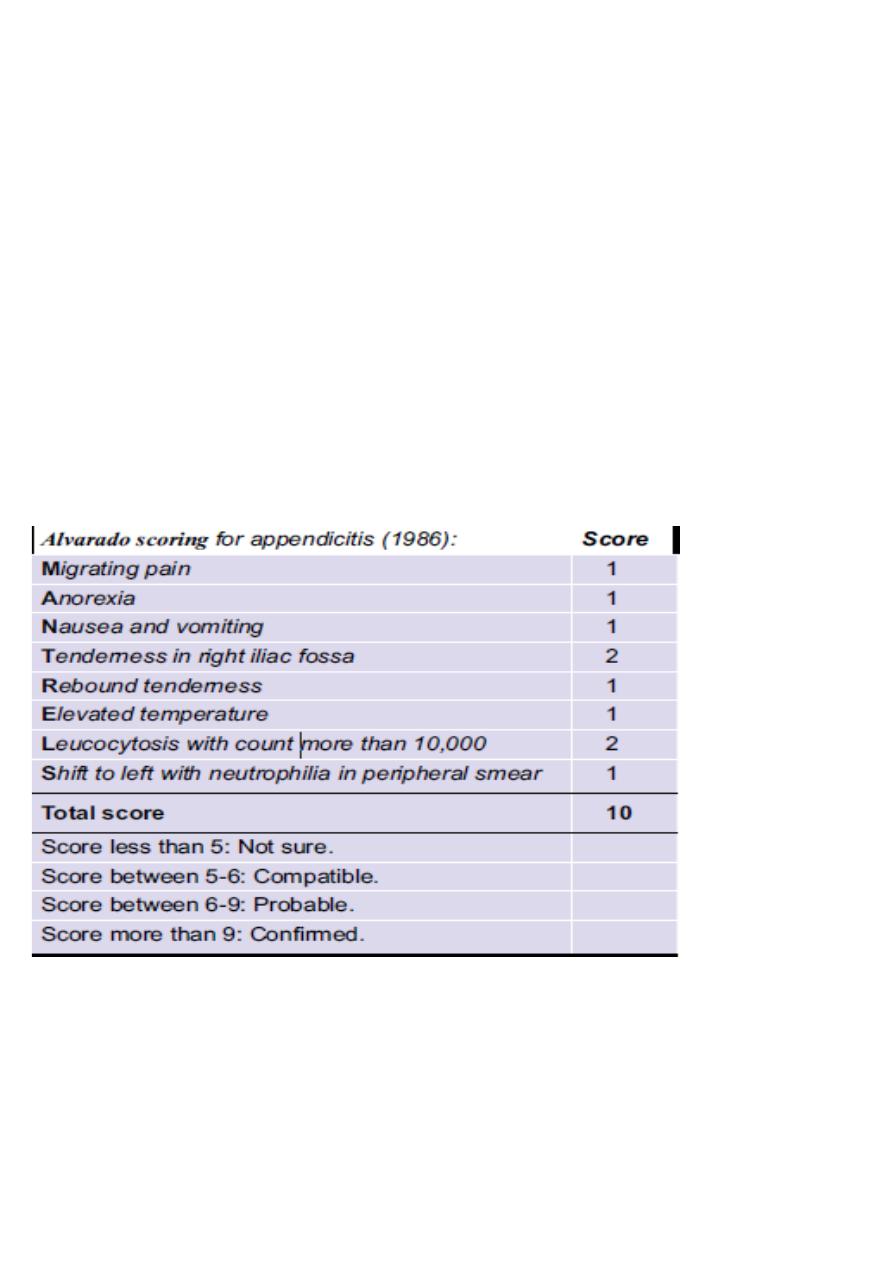
Investigations
1- BLOOD ;- *Total leucocyte count is increased.
*C-reactive protein, even though nonspecific increases in acute phase.
2-IMAGINGS;-
*Plain X-ray -X-ray is useful to rule out ;-
1=DU perforation, 2- intestinal obstruction, 3-ureteric stone.
* Ultrasound is done to rule out other conditions like;-
*ureteric stone, pancreatitis, ovarian cyst, ectopic pregnancy and also to confirm appendicular
mass or abscess.
*-Contrast CT scan is very much useful when diagnosis is difficult especially in old people.
3- Laparoscopy is the most useful method.
!
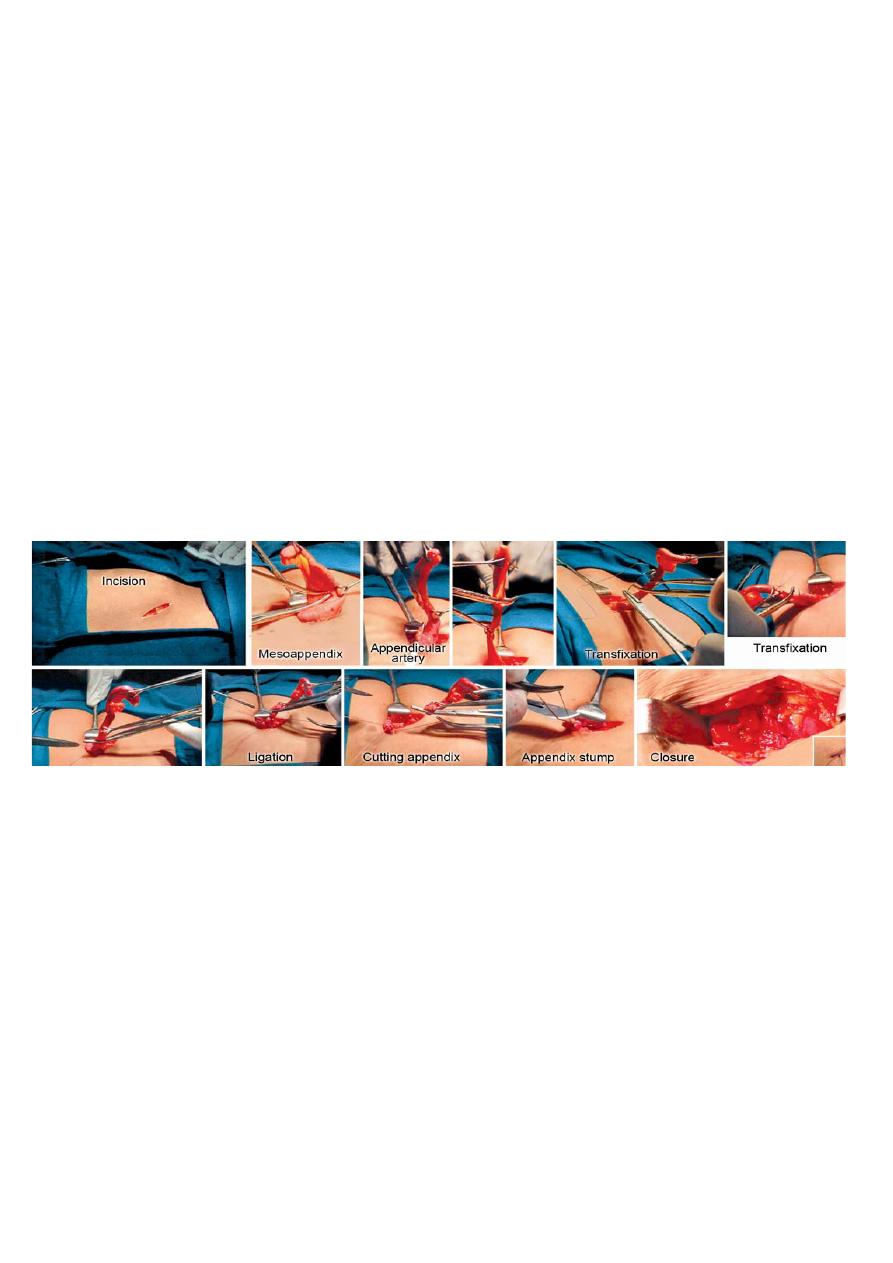
Treatment;- Surgery- Appendicectomy
Approaches
1-Gridiron incision: Incision is placed perpendicular to the right spinoumbilical line at the
McBurney’s point=
(i.e. at the junction of lateral one-third and medial two-third of spinoumbilical line).
2. Rutherford Morison’s muscle cutting incision (Muscles are cut upwards and laterally).
3. Lanz crease incision centering at McBurney’s point—cosmetically better.
4. Right lower paramedian incision/lower midline incision—
when in doubt or when there is diffuse peritonitis.
5. Laparoscopic approach: Becoming popular and better.
6. Fowler-Weir approach by cutting muscle medially over the rectus.
!
Complications after appendicectomy
1- Paralytic ileus.
2- Reactionary haemorrhage due to slipping of ligature of the appendicular artery.
3- Residual abscess (pelvic, paracolic, local, sub diaphragmatic).
4-Adhesions, kinking and intestinal obstruction.
5- Right inguinal hernia (direct)—due to injury to ilioinguinal nerve.
6- Wound sepsis 10%.
7- Faecal fistula.
8- Respiratory problems and DVT.
9- Pylephlebitis (Portal pyaemia).
INCIDENTAL APPENDICECTOMY
* removal of normal appendix is done at laparotomy for other conditions.
* It is done in vague lower abdominal pain of doubtful severity.
* It is a useful procedure to tackle ‘Munchausen syndrome, i.e. the patient is always worried of
pain abdomen and gets relieved after the procedure (psychological benefit).
* It is done along with Ladd’s procedure for malrotation.
* It is also done during on table colonic lavage.
*It is not done in Crohn’s disease (during acute phase of appendicitis), postradiation,
immunosuppression, aortoiliac grafts.
APPENDICULAR MASS -(Periappendicular Phlegmon)
It is the localisation of infection occurring 3 to 5 days after an attack of acute appendicitis.
Inflamed appendix, greater omentum, oedematous caecum, parietal peritoneum
and dilated ileum (Ileus) forms a mass in the right iliac fossa.
This mass is tender, smooth, firm, well localised, not moving with respiration,
not mobile, all borders well made out (well localised) and resonant on percussion.
Patient may have fever and features of toxicity.
Differential diagnosis
Carcinoma caecum Actinomycosis
Crohn’s disease Mesenteric lymphadenitis
Ovarian disease Ruptured ectopic pregnancy
Twisted ovarian cyst Ileocaecal tuberculosis
Investigations
1- Total leucocyte Count is increased.
2- U/S confirms the mass.

!
Treatment ;-
1- Conservative (Ochsner-Sherren Regimen)= Includes observation:
1- Temp, BP, pulse chart.( Marking the mass to identify the progression/regression).
2- Antibiotics (Ampicillin, metronidazole, genta micin, ..)
3- IV fluids. 4- Analgesics. 5- Initial nasogastric aspiration.
Patient usually shows response by 48 to 72 hours and mass reduces in size, temperature and pulse
becomes normal. Appetite is regained.
90% of patients respond to conservative therapy.
Patient is discharged and advised to come for interval appendicectomy after 6 weeks.
Contraindications for Ochsner-Sherren regimen
1. When diagnosis is in doubt. 2. In acute appendicitis in children and
elderly.
3. In burst, gangrenous appendicitis. 4. In patients in whom diffuse peritonitis
sets in.
Criteria to discontinue Ochsner-Sherren regimen
1- Patient becomes more toxic (tachycardia, high fever). 2- Persistent vomiting.
3- Increase or spread of pain abdomen (means onset of diffuse peritonitis).
4- Increased size of the mass 5- Suppuration (abscess formation) in
the mass.
In these patients the regimen is discontinued.
The patient is taken for immediate surgery, either through laparotomy or through classic
approaches

APPENDICULAR ABSCESS
It occurs due to suppuration in an acute appendicitis or suppuration in an already formed
appendicular mass.
Abscess commonly occurs in retrocaecal region but often can occur in subcaecal, preileal lumbar
or postileal regions.
Pelvic abscess is also common after an attack of acute appendicitis.
Clinical Features
High fever, features of toxicity, tender, smooth, dull (to percuss), soft swelling in right iliac
fossa which lies towards right lateral and lower side with clear upper margin but indistinct
lower margin.
U/S confirms the diagnosis.
Treatment ;- Antibiotics are started.
Under G/A, incision is made in the lower lateral aspect of the swelling
above the inguinal ligament. Skin, external oblique muscle is cut.
Abscess cavity is opened and pus is drained extraperitoneally, which is
sent for culture and sensitivity. Wound is closed.
A drain is placed through a separate incision. Antibiotics are continued.
Interval appendicectomy is done after 3 months.
Pelvic abscess is drained per-rectally or through vagina
( posterior colpotomy in females).
MUCOCELE OF APPENDIX
It can be neoplastic or non-neoplastic.
It occurs when proximal end of the lumen of appendix gets slowly and completely
occluded, usually by a fibrous stricture causing collection of sterile fluid (mucus) in the
Lumen. It is a retention cyst.
Appendix is grossly enlarged with features of sub-acute appendicitis.
Mucocele can get infected leading to empyema of appendix.
Rupture of mucocele can lead to pseudomyxoma peritonei.

Neoplastic type causes generalised pseudomyxoma peritonei;
non-neoplastic type causes localised pseudomyxoma peritonei.
Often mucocele of appendix is also caused by a mucus secreting adenocarcinoma and if
it is so right Hemicolectomy is done.
Clinical Features ;- Colicky pain in right iliac fossa.
Tenderness in the right iliac fossa.
Investigations;- U/S abdomen.
Treatment;- Appendicectomy.
Pseudomyxoma peritonei
Jelly like mucoid yellowish-brown substance accumulates in peritoneal cavity.
Due to ruptured adenocarcinoma appendix/mucocele or mucinous carcinoma of ovary.
Common in females.
Painless progressive distension of abdomen with intestinal obstruction occurs eventually
Shifting dullness is absent.
Surgical debulking, oophorectomy, appendicectomy, omentectomy are often done.
Chemotherapy is useful—cisplatin.
Carries poor prognosis.
Pseudomyxoma peritonei is presently considered to be due to neoplastic adenocarcinoma
of appendix with gelatinous fluid collection in the peritoneal cavity.
It is also seen in cystadenocarcinoma of ovary.
Treatment is surgery and chemotherapy.
NEOPLASMS OF THE APPENDIX
It is rare. = It is often postappendicectomy histological diagnosis.
Cystic neoplasms of appendix: Simple cyst (non-neoplastic mucocele); mucinous cystadenoma;
mucinous cystadenocarcinoma (most common form of cystic neoplasms); pseudomyxoma
peritonei.
Simple cyst is non-neoplastic obstruction of the lumen and is less than 2 cm in size which
contains
mucin.
Mucinous cystadenoma attains progressively large size of up to 8 cm with CT showing
calcification
of the wall. Laparoscopic appendicectomy is not used in mucinous cystadenoma.
Treatment ;-Hemicolectomy is done in mucinous cystadenocarcinoma and cystadenoma of large
size and if base is involved.
Carcinoid tumour is the most common type.
It is less aggressive. It is often incidentally found. It is arising from Kulchitsky cells in
crypts of Lieberkuhn (argentaffin tissue).
It is ten times more common than other types (One in 400 ppendices).
Commonly its location is in the tip.
Carcinoid of appendix may be goblet cell type or classical type histologically.
Treatment is appendicec-tomy.
Right hemicolectomy is done if base is involved or size is more than 2 cm or nodes are involved.
Primary adenocarcinoma of the appendix is rare.
It can be mucinous (common) or colonic (less Common) type.
Acute presentation as appendicitis is common in colonic type.
Mucinous type has got better prognosis.
Mucinous type can rupture into the peritoneal cavity and can cause pseudomyxoma peritonei.
