1
Gastric anatomy & physiology
Dr.Luay
Function of Stomach
Reservoir
Mix food
Digestion of
Protein
Fats
Activates some enzymes (Pepinogen into pepsin)
Destroy some bacteria by HCl
Makes intrinsic factor – Vit. B 12 absorption
In adult life, stomach located T10 and L3 vertebral segment
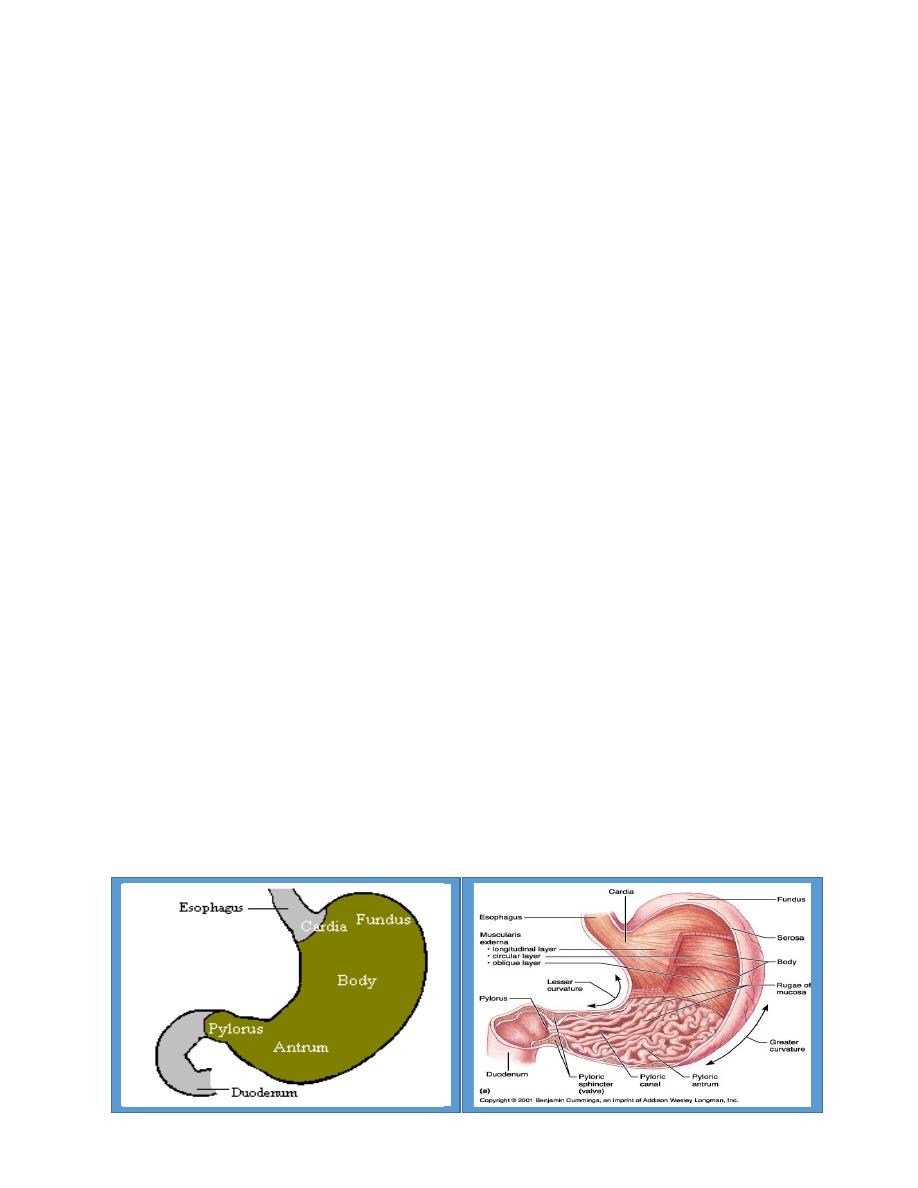
Can be divided into anatomic regions based on external landmarks
4 regions:-
Cardia
Fundus
Corpus (body)
Antrum

2
Position of the stomach varies with body habitus
In general- it is fixed at two points
Proximally at the GE juction
Distally by the retroperitoneal duodenum
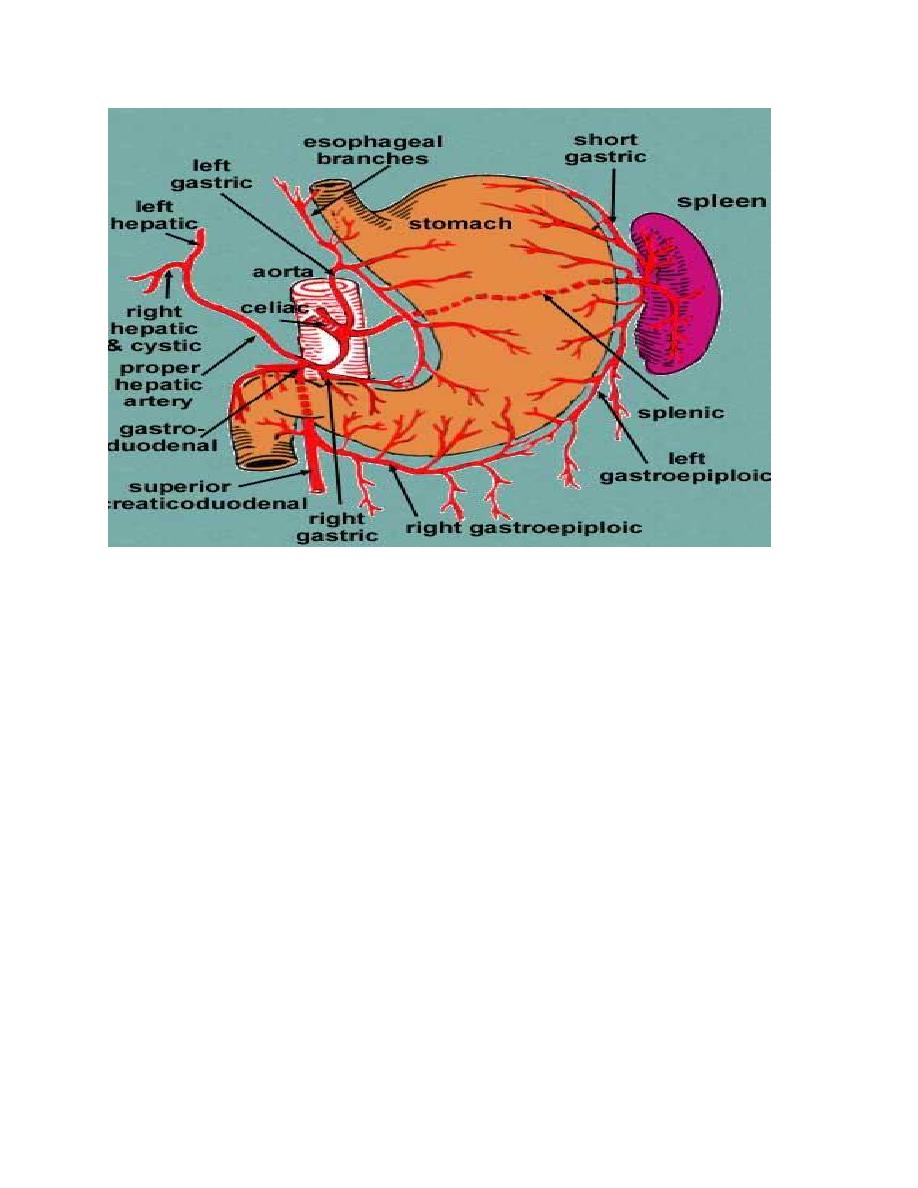
Vasculature
Well vascularized organ
Arterial flow mainly derived from Celiac Artery
3 Branches:
Left Gastric Artery
Supplies the cardia of the stomach and distal esophagus
Splenic Artery
Gives rise to 2 branches which help supply the greater curvature of the stomach
Left Gastroepiploic
Short Gastric Arteries
Common Hepatic or Proper Hepatic Artery
2 major branches
Right Gastric- supples a portion of the lesser curvature
Gastroduodenal artery
-Gives rise to Right Gastroepiploic artery
-helps supply greater curvature in conjunction with Left Gastroepiploic Artery
3
Venous Drainage
Parallels arterial supply
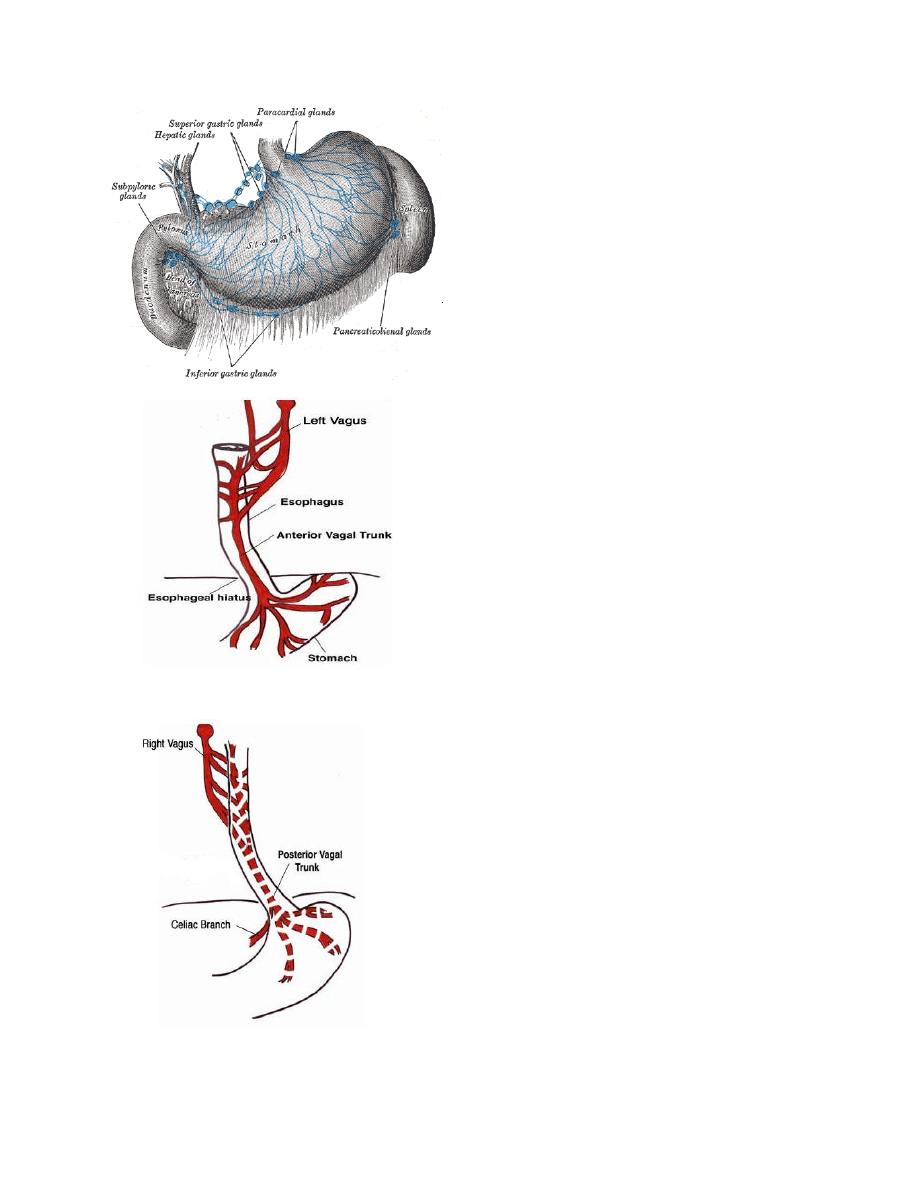
Lymphatic drainage
Lymph from the proximal portion of the stomach drains along the lesser curvature
first drains into superior gastric lymph nodes surrounding the Left Gastric Artery
Distal portion of lesser curvature drains through the supra pyloric nodes
Proximal portion of the greater curvature is supplied by the lymphatic vessels that
traverse the pancreaticosplenic nodes
Antral portion of the greater curvature drains into the subpyloric and omental nodal
groups
In general- The lymphatic drainage of the human stomach, like its blood supply, exhibits
extensive intramural ramifications and a number of extramural communications. Therefore
spread beyond is often beyond region of origin at a distance from the primary lymphatic.
4
Nerve Supply
– Left and Right Vagus Nerves descend
parallel to the esophagus within the
thorax before forming a peri-esophageal
plexus between the tracheal bifurcation
and the diaphragm
– From this plexus, two vagal trunks
coalesce before passing through the
esophageal hiatus of the diaphragm
Left (anterior) Vagus Nerve
Left of the esophagus
Branches
Hepatic Branch
Supplies liver and Biliary Tract
Anterior gastric or Ant. Nerve of Latarget.
Right (posterior) Vagus Nerve
Right of the esophagus
Branches
Celiac
Posterior Latarget
Innervates posterior gastric wall
5
the stomach and duodenum possess both
intrinsic and extrinsic nerve supplies:
The intrinsic nerves exist principally in two plexuses, the myenteric plexus of Auerbach
and the submucosal plexus of Meissner
The extrinsic supply is derived mainly from the vagus nerves, fibres of whichoriginate in
the brainstem.
Parasympathetic innervation of Stomach- Vagus Nerve
– 90% of fiber in vagal trunk is afferent (sensory)from stomach to CNS
The efferent fibres are involved in the
– receptive relaxation of stomach
– stimulation of gastric motility,
– secretory function.
Sympathetic innervation of Stomach- Splanchnic Nerve(coeliac ganglia)
Derived from spinal segement T5-T10
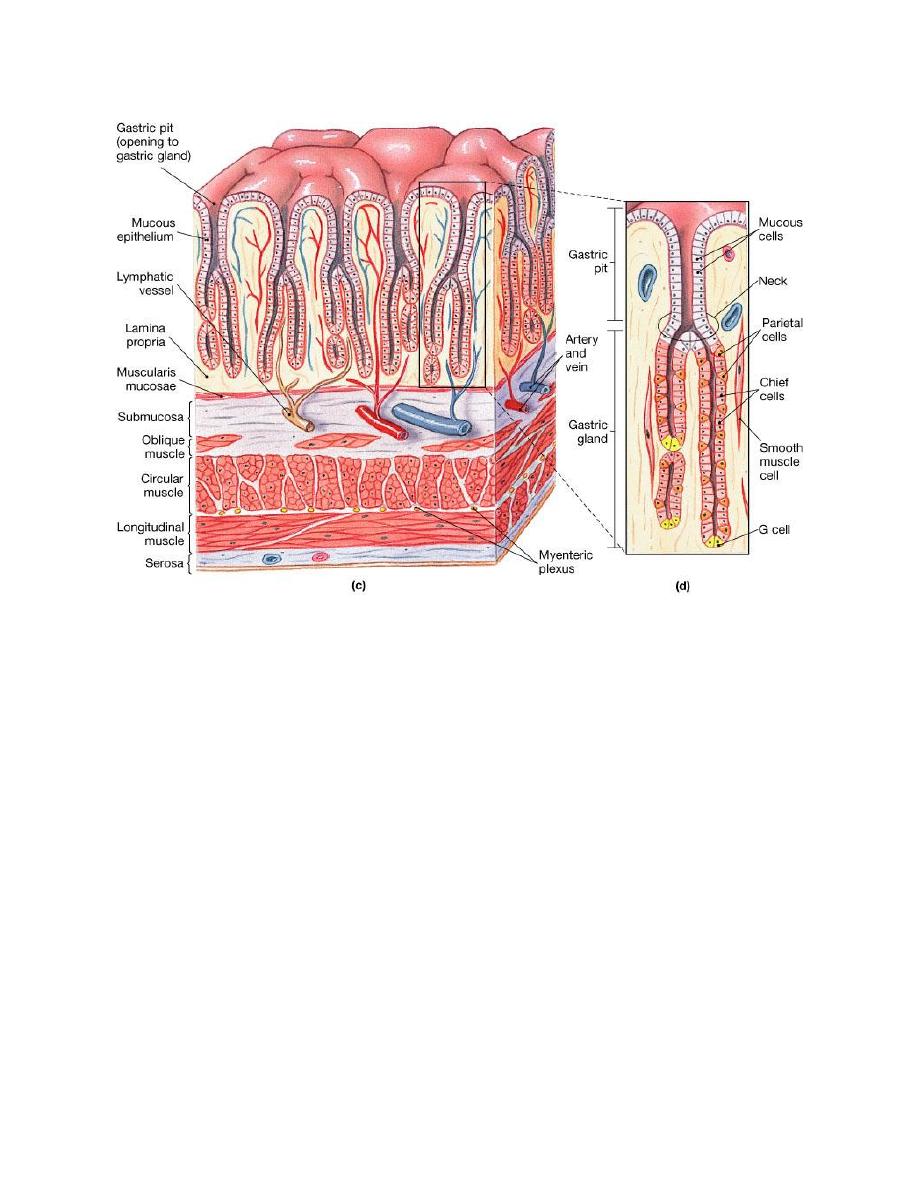
MICROSCOPIC ANATOMY OF THE STOMACH AND DUODENUM
The gastric epithelial cells are mucus producing and are turned over rapidly
Specialised cells of the stomach (parietal and chief cells) are found in the gastric crypts
endocrine cells. G cells (gastrin),
D cell(somatostatin), enterochromaffin-like (ECL) cells (histamin)
– Parietal cells
Location- neck of gastric pit
Stimulated by Ach, Histamine and Gastrin
Secretes HCl + Intrinsic Factor
The hydrogen ions are actively pumped by theproton pump,
a hydrogen–potassium-ATPase

6
Chief Cells
Location- base of gastric pit
Stimulus- Vagal
Secretes Pepsinogen (eventually leads to pepsin- digestive enzyme)
– Antral Glands
– Gastrin cells
Location- mucosa of distal stomach
Stimulus- amino acids
Secretion- Gastrin (stimulates HCl production by way of parietal cells)
– Somatostatin
Location- mucosa of distal stomach + Duodenum
Stimulus- HCl or low pH in duodenum
Actions- Inhibits gastric emptying, Pancreatic secretions, and gallbladder
contraction
7
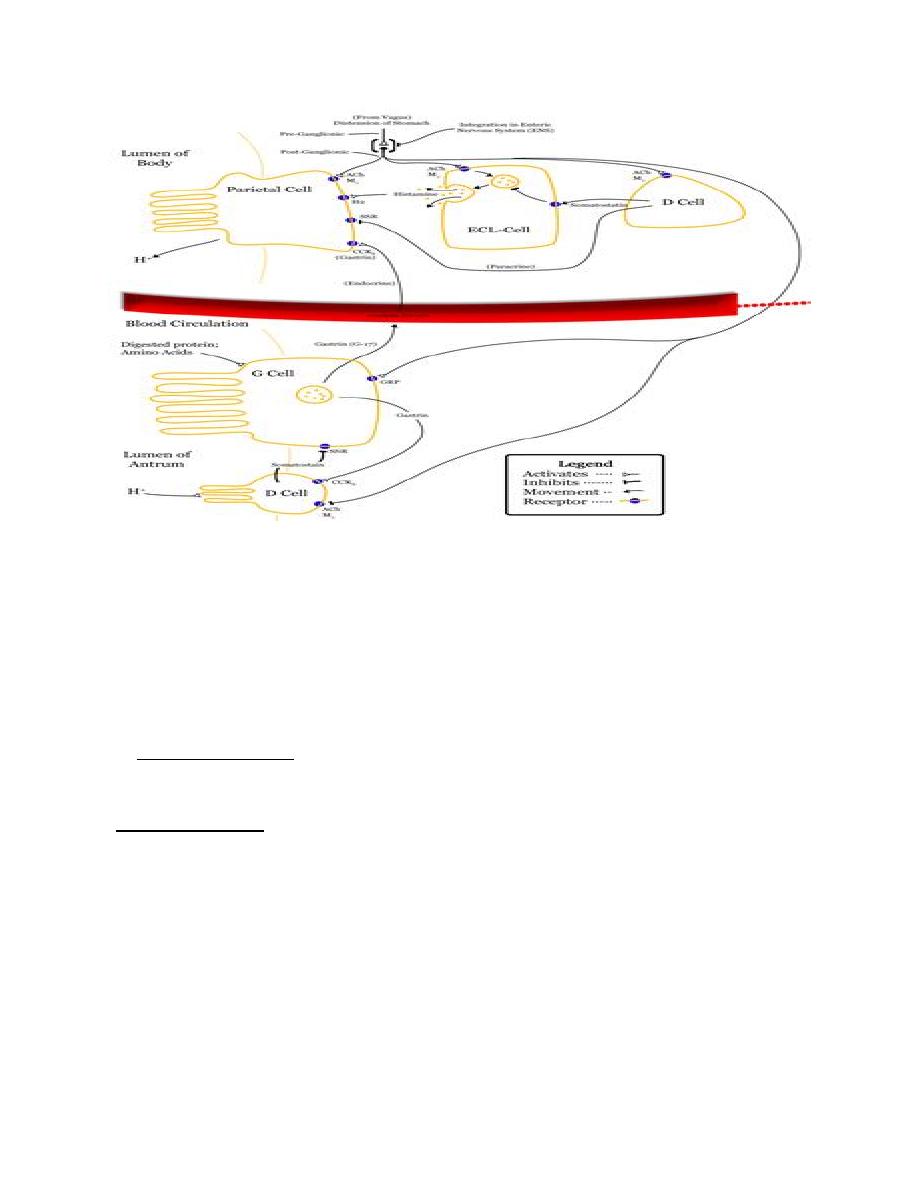
Gastric Acid Secretion
Stimulated acid secretion begins with
– Cephalic phase
– Thought, sight or smell of food stimulates acid secretion
– Mediated by Vagal stimulation
Vagal discharge
– Directs the cholinergic mechanism for stimulation
Can be inhibited by Atropine (anticholinergic)
– Inhibits release of somatostatin
Vagal effects inhibit tonic inhibition that is provided by
somatostatin

8
Gastric Phase
Begins when food enters the stomach
– The following are responsible for stimulation of acid secretion
Presence of partially hydrolyzed food constituents
Gastric distention
– Gastrin is the most important mediator of this phase
Ends when Antral muscosa is exposed to acid
– When luminal pH is <2.0 in the antrum, gastrin release stops
– Somatostatin release is increased
– Entry of digestive products into the intestine begins the intestinal-phase
inhibition of gastric acid secretion
– Intestinal Phase
The presence of chyme in the duodenum and small bowel inhibits gastric
emptying and theacidification of the duodenum
Releases secretin to inhibit Gastrin which ultimately decreases Acid
production.
9
Gastric mucus and the gastric mucosal barrier
The gastric mucus layer is essential to the integrity of the gastric mucosa. As barrier
against acid and pepsin, buffering capacity
breakdown of this gastric mucous barrier by NSAIDs, ischaemia following a
hypovolaemic insult
Gastroduodenal motor activity
Receptive Relaxation
Vagally mediated relaxation of fundus (proximal stomach) when degluttination occurs
Adaptive relaxation Allows the proximal stomach to act as a storage site for ingested food in
the immediate postprandial period
Meal is accepted without a significant increase in intra-gastric pressure
Most of the peristaltic activity is found in the distal stomach
proximal stomach demonstrates only tonic activity
10
The investigation of gastric disorders
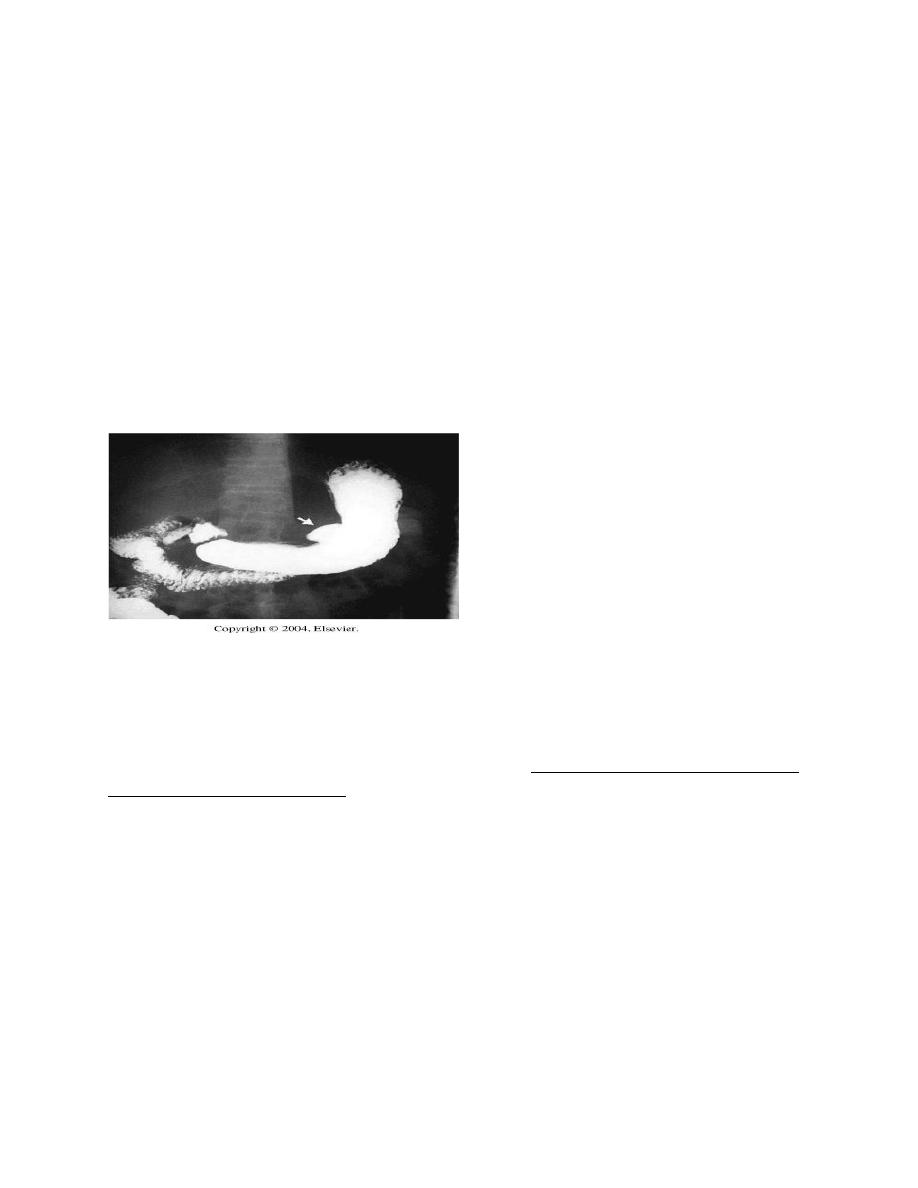
1.Flexible endoscopy
the ‘gold standard’
more sensitive than conventional radiology
Diagnostic&therapeutic
Great care is necessary in performing endoscopy to avoid complications and missing
important pathology
2. Contrast radiology
now less frequently used
3. Ultrasonography
conventionally it is less sensitive
endoluminal ultrasound and laparoscopic
ultrasound are probably the most sensitive techniques depth of invasion of a tumour can be
assessed with exquisite accuracy
assessment of gastric emptying
Liver metastasis
Computerised tomography scanning and magnetic resonance imaging
lacks sensitivity in detecting smaller and curable lesions. It is much less accurate in‘T’
staging than endoluminal ultrasound
it is possible to be reasonably accurate in detecting nodal involvement with tumour

11
Axial imaging, particularly multislice CT, is useful in the staging of gastric cancer,
although it may be less sensitive in the detection of liver metastases than other
modalities
Computerised tomography/positron emission tomography
Fluorodeoxyglucose most commonly used tracer
used in the preoperative staging of gastro-oesophageal cancer
demonstrate occult spread
Laparoscopy l
Laparoscopy is sensitive in detecting peritoneal metastases
laparoscopic ultrasound provides an
Accurate evaluation of lymph node and liver metastases
Gastric emptying studies
useful for studying gastric dys motility problems, particularly those that follow gastric
surgery
radioisotope-labelled liquid and solid meal is ingested and the emptying of the stomach
is followed on a gamma camera.
Angiography
most commonly in the investigation of upper gastrointestinal bleeding that is not
identified using endoscopy
Therapeutic embolisation for unfit patients
By:-Mohammed Kamal Jalal
