Page
1
of
11
MALIGNANT NEOPLASMS OF THE STOMACH
The three most common primary malignant gastric neoplasms are :-
• Adenocarcinoma(95 percent),
• Lymphoma (4 percent)
• Malignant gastrointestinal stromal tumor (GIST) (1 percent)
Adenocarcinoma (Gastric Cancer)
Epidemiology:
• · Second leading cause of cancer-related death world-wide
• · USA 2-5 deaths/100,000 people, Japan 90 deaths/100,000 people
• · Steady decline in incidence since 1930 - improved living conditions
• · Incidence of proximal tumors increasing, incidence of distal tumors
decreasing
• · Japan and Korea - 40% detected by early screening programs leading to
improved survival
• increase in the incidence of carcinoma in the proximal stomach,
particularly oesophagogastric junction
• Carcinoma of the distal stomach and body of the stomach is most common
in low socioeconomic groups
• whereas the increase in proximal gastric cancer seems to affect principally
higher socioeconomic groups
• Proximal gastric cancer does not seem to be associated with H. pylori
infection, in contrast withcarcinoma of the body and distal stomach
• Upper oesophagus 2%
• Mid-oesophagus 6%
• Lower oesophagus 22% ,OG junction 18%
Cardia 17%(Approximately 60%)
• Body 15%
• Pylorus 7%
• Antrum 13%
Page
2
of
11
Etiology
• Gastric cancer is a multifactorial disease
• Diet
• H. Pylori :distal and body of stomach more
• Previous stomach surgery:
• Pernicious anemia
• Polyps
• Atrophic gastritis
• Radiation
• genetics
Helicobacter
• Implicated as precursor of gastric cancer.
• H. Pylori associated with atrophic gastritis, and patients with a history of
prolonged gastritis have a 6-fold increase in risk.
• Particularly true of tumors of antrum, body, and fundus of stomach, but
not in cardia.
Diet
• Spirits may induce gastritis and, in the long term, cancer.
• Excessive salt intake,
• Deficiency of antioxidants and
• Exposure to N-nitroso compounds
• Smoked meats
Previous stomach surgery
• The risk is controversial, but the phenomenon is real
• drainage procedures such as Billroth II or P َlya gastrectomy,
gastroenterostomy or pyloroplasty,are at approximately four times the
average risk
• duodenogastric reflux and reflux gastritis
• Intestinal metaplasia, dysplasia.
• Patients with pernicious anaemia and gastric atrophy are at increased risk
Page
3
of
11
Polyps.
• There are five types of gastric epithelial polyps: inflammatory,
hamartomatous,
• Heterotopic, hyperplastic, and adenoma. The first three types
have negligible malignant potential.
• Adenomas can lead to carcinoma,10%of polyps
Genetic/familial
•
Deletion/suppression p53 60–70%
•
Amplification/overexpression COX-2 70%
•
Microsatellite instability 25–40%
•
DNA aneuploidy 60–75%
•
First degree relatives of patients with gastric cancer havean
increased risk of 2 to 3 fold.
•
Patients with hereditary non polyposis colorectal cancer
(HNPCC) have a 10 percent risk of developing gastric cancer
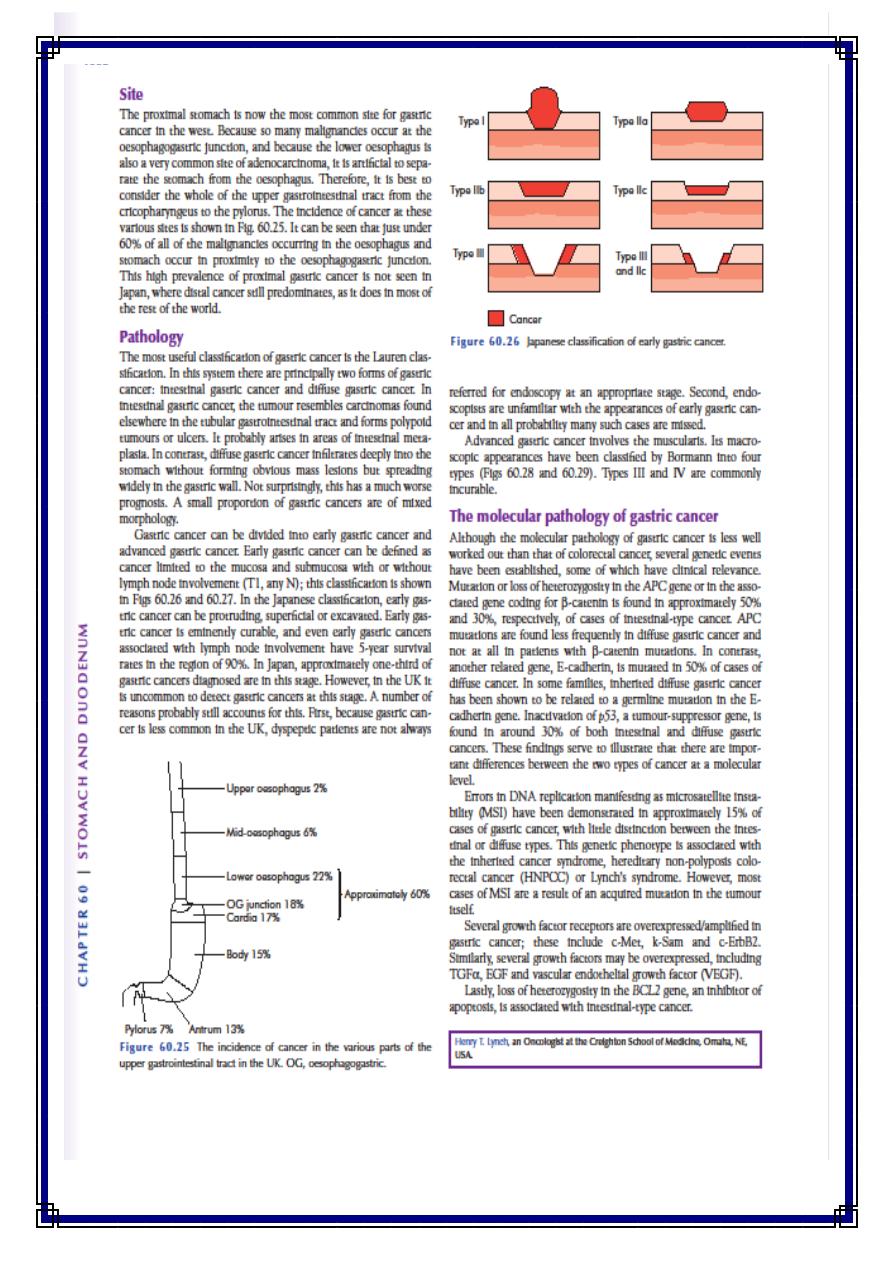
Pathology of Stomach Cancer
Classification of gastric cancer is by the
Lauren classification:
1.intestinal gastric cancer =polyploidy tumors or ulcers, arises in
areas of intestinal metaplasia associated with atrophic gastritis,
retained glandular structure, little invasiveness, carries better
prognosis, shows no family history
2. Diffuse gastric cancer =infiltrates deeply into the
Stomach without forming obvious mass lesions but spreading
widely in the gastric wall, endemic,
Younger patients, genetic factors, blood groups, and family history,
poor prognosis
Page
4
of
11
Borrmann Classification
1.
5 categories
2.
Type I: polypoid or fungating
3.
Type II: ulcerating lesions with elevated borders
4.
Type III: ulceration with invasion of wall
5.
Type IV: diffuse infiltration
6.
Type V: cannot be classified
Types مهم
• Gastric cancer can be divided into :-
1.
early gastric cancer
2.
Advanced gastric cancer.
• Early gastric cancer can be defined as cancer limited to the
mucosa and submucosa with or without lymph node involvement
(T1, any N)
• 10 %of patients with EGC will have lymph node metastases.70%
well diff.,95%cure rate with adequate resection
• EGCs are endoscopically divided into three types, protruded,
superficial, and excavated. 80% of EGCs are of the superficial type,
which are further subdivided into elevated type, flat type, and
depressed type, the latter being the most common
Page
5
of
11
Page
6
of
11
Page
7
of
11
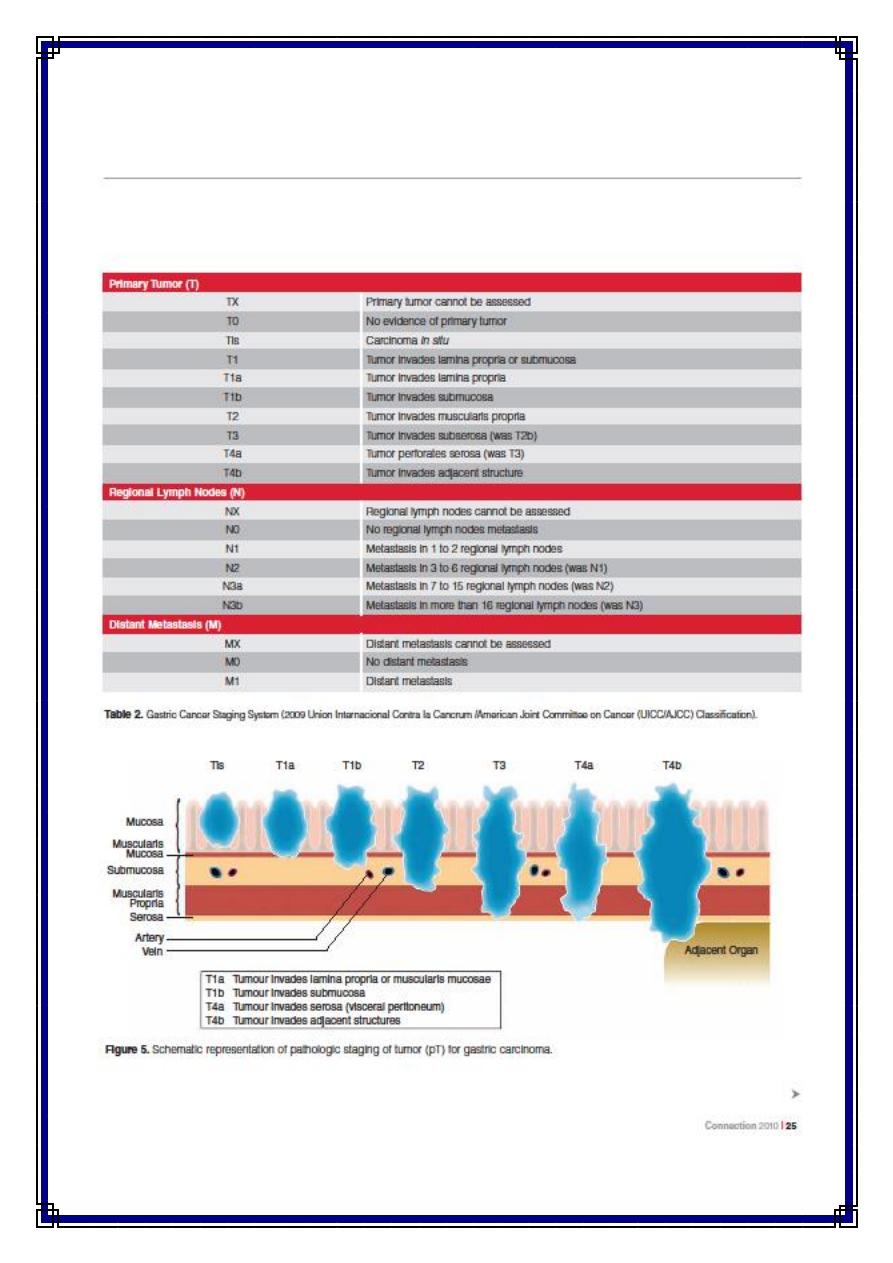
International Union against Cancer (UICC)
staging of gastric cancer
• T1 Tumor involves lamina propria, submucosa
• T1a lamina propria
• T1b submucosa
• T2 Tumor invades muscularis propria
• T3 Tumor involves subserosa
• T4a Tumor perforates serosa
• T4b Tumor invades adjacent organs
• N0 No lymph nodes
• N1 Metastasis in 1–2 regional nodes
• N2 Metastasis in 3–6 regional nodes
• N3a Metastasis in 7–15 regional nodes
• N3b Metastasis in more than 15 regional nodes
• M0 No distant metastasis
• M1 Distant metastasis (this includes peritoneum and distant
• lymph nodes)
Staging
IA T1 N0 M0
IB T1 N1 M0
• T2 N0 M0
IIA T1 N2 M0
• T2 N1 M0
• T3 N0 M0
IIB T1 N3 M0
• T2 N2 M0
• T3 N1 M0
• T4a N0 M0
IIIA T2 N3 M0
• T3 N2 M0
• T4a N1 M0
IIIB T3 N3 M0
• T4a N2 M0
• T4b N0–1 M0
IIIC T4a N3 M0
• T4b N2–3 M0
IV Any T Any N M1
Page
8
of
11
Spread of carcinoma of the stomach
• The diffuse type spreads via the submucosal and subserosal
lymphatic plexus
• It penetrates the gastric wall at an early stage.
Direct spread:-
The tumour penetrates the muscularis, serosa and ultimately
adjacent organs such as the pancreas, colon and liver.
Lymphatic spread:-
• This is by both permeation and emboli to the affected tiers of
nodes.
• Unlike malignancies such as breast cancer, nodal involvement does
not imply systemic dissemination.
• Supraclavicular nodes (Troisier’s sign).
Blood-borne metastases
• These occur first to the liver and subsequently to other organs,
including lung and bone.
Trans peritoneal spread
• This is a common mode of spread once the tumor has reached the
serosa of the stomach and indicates incurability
• Ascites
• Palpated either abdominally or rectally as a tumor ‘shelf’.
• Ovaries may sometimes be the sole site of transcoelomic spread
(Krukenberg’s tumours)
• Spread via the abdominal cavity to the umbilicus (Sister Joseph’s
nodule)
Page
9
of
11
Lymphatic drainage of the stomach
• The lymphatics of the antrum drain into the right gastric lymph node
superiorly, and right gastroepiploic and subpyloric lymph nodes inferiorly.
• The lymphatics of the pylorus drain into the right gastric suprapyloric nodes
superiorly and the subpyloric lymph nodes situated around the
gastroduodenal artery inferiorly
• The efferent lymphatics from suprapyloric lymph nodes converge on the
para-aortic nodes around the coeliac axis, whereas the
• Efferent lymphatics from the subpyloric lymph nodes pass up to the main
superior mesenteric lymph nodes situated around the origin of the superior
mesenteric artery.
• The lymphatic vessels related to the cardiac orifice of the stomach
communicate freely with those of the oesophagus.
• The prognosis of operable cases carcinoma of the stomach depends on
whether or not there is histological evidence of regional lymph node
involvement
• the Japanese Research Society for Gastric Cancer has assigned a number to
each lymph node station to aid the pathological staging
Operability:-
• It is important that patients with incurable disease are not
subjected to radical surgery that cannot help them
Evidence of incurability is
1.
haematogenous metastases,
2.
involvement of the distant peritoneum,
3.
N4 nodal disease and
4.
Disease beyond the N4 nodes, and
5.
fixation to structures that cannot be removed.
Total gastrectomy:-
In general, a D1 resection involves the removal of the perigastric
nodes and
A D2 resection involves the clearance of the major arterial trunks.
Page
11
of
11
In practice, the majorityof specialist centres will perform a radical
total gastrectomy, conserving the spleen and pancreas, with D2
lymphadenectomy sparing station 10 lymph nodes.
Subtotal gastrectomy:-
• For tumors distally placed in the stomach, it appears unnecessary
to remove the whole stomach.
Palliative surgery:-
• In patients suffering from significant symptoms of either
obstruction or bleeding, palliative resection is appropriate
Other treatment modalities:-
•
Radiotherapy
has a role in the palliative
• Treatment of painful bony metastases.
•
Chemotherapy
Gastric cancer may respond well to combination
cytotoxic
Chemotherapy and
neoadjuvant chemotherapy improves the outcome following
surgery
• combination of epirubacin, cis-platinum and in fusional 5-FU or an
oral analogue such as capecitabine
Done by: #MOHDZ Dr.Loay – Surgery
