-
1
-
LIVER TRAUMA
Dr. Dlair Omer
Liver injuries are fortunately uncommon
–
*position under the diaphragm
*protected by the chest wall.
However, when occurs, it is serious
divided into:
1. Blunt injury: produces contusion, laceration and avulsion
injuries to liver, m.b associated with splenic, mesenteric or
renal injury.
2. Penetrating injuries, such as stab and gunshot wounds, are
often associated with chest or pericardial involvement
At risk patients:
1. Stabbing/gunshot in lower chest or upper abdomen, esp if
severe hypotension
2. Severe Crush injury with multiple rib fractures, haemothorax
and S/S of shock
Diagnosis
1. CT
– scan with oral & iv contrast
2. DPL
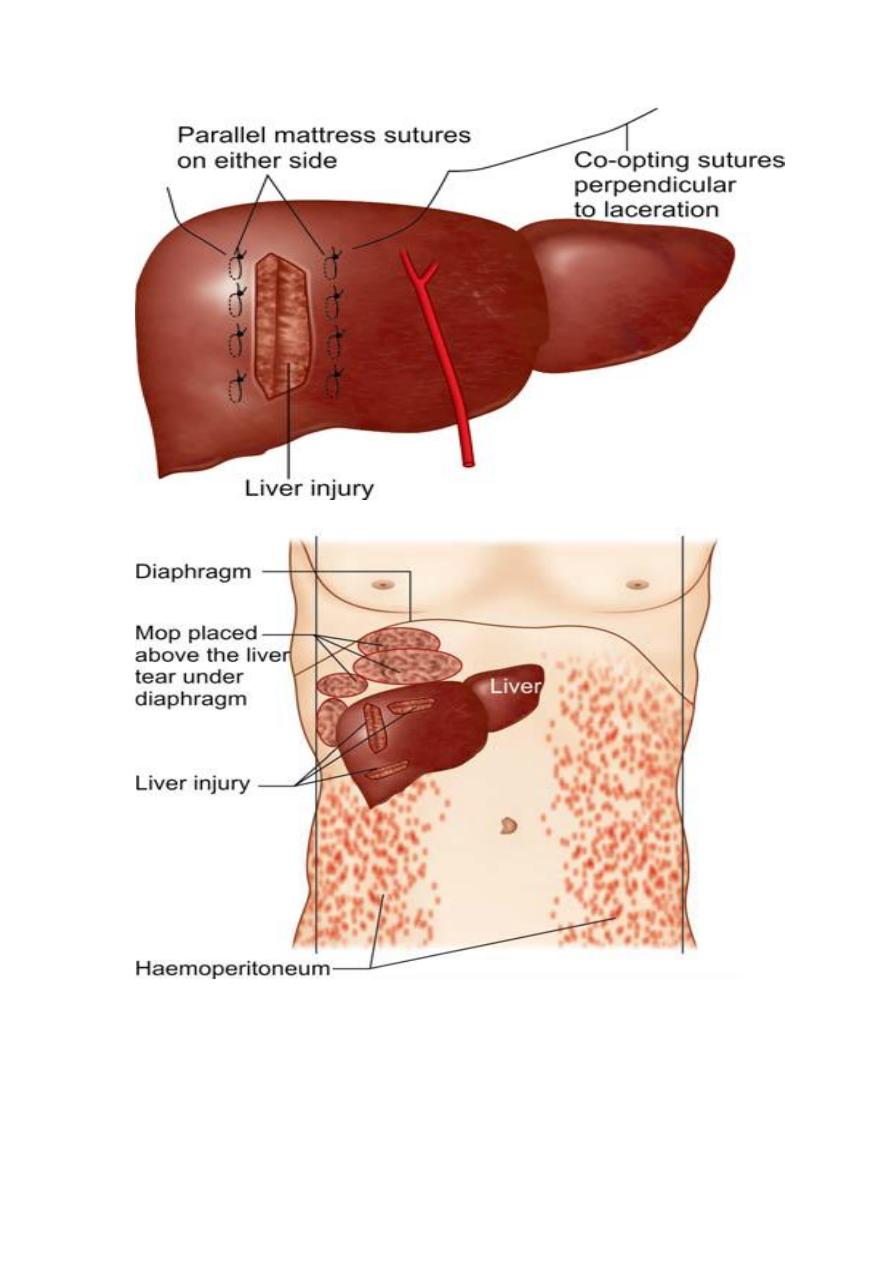
3. FAST: determine haemoperitoneum
4. Laparoscopy:
demonstrate
associated
diaphragmatic
rupture, Damage to the spleen and/or liver.
Hepatic organ injury scale
Grade I:
• hematoma subscapular, nonexpanding <10cm surface area
• Laceration capsular tear, nonbleeding, <1cm parenchymal
depth
Grade II:
• hematoma subscapular, nonexpanding 10-50% surface area
• Intraparenchymal nonexpanding <10cm diameter
• Laceration capsular tear, active bleeding; 1-3cm depth,
<10cm in length
Grade III:
• Hematoma subcapsular, >50% surface area or expanding;
• Ruptured subcapsular hematoma with active bleeding;

-
2
-
• Intraparenchymal hematoma >10cm or expanding;
• Laceration >3cm parenchymal depth
Grade IV:
• Hematoma ruptured intraparenchymal hematoma with active
bleeding;
• Laceration parenchymal disruption involving 25-75% of
hepatic lobe
Grade V:
• Laceration parenchymal disruption involving >75% of hepatic
lobe
• Vascular juxtahepatic venous injuries (vena cava, hepatic
veins)
Grade VI:
• Vascular hepatic avulsion
Management of liver trauma
Haemodynamically stable pts: -- oral and intravenous
contrast-enhanced CT scan of the chest and abdomen. This
will demonstrate evidence of:
1. parenchymal damage to liver or spleen
2. associated traumatic injuries to their feeding vessels.
3. Free fluid
4.
The chest scan: injuries to the great vessels and damage to the
lung parenchyma.
Haemodynamically stable ---- conservative treatment
Pts managed nonoperatively for solid organ injuries, but
when develop: Tachycardia, leukocytosis, hypotension,
metabolic acidosis, chang
es in abdominal examination→
may need surgery
laparotomy and/or thoracotomy indicated in:
1.
Haemodynamically unstable pts
2.
pts with penetrating injuries
3.
Pts with haemodynamic instability & evidence of positive DPL.
Findings on abdominal CT scan
Pelvic collection
Pneumoperitoneum

-
3
-
Focal bowel wall thickening
Mesenteric hematoma
Mesenteric fat streaking
Extravasation of oral & intravenous contrast
Initial management of liver injuries
Penetrating
1. A B C
2. Peripheral venous access: two large-bore cannulae and
blood for cross-match of 10 units of blood,
3. full blood count, urea and electrolytes, liver function tests,
clotting screen, glucose and amylase.
4. Initial volume replacement with colloid or O-negative blood if
necessary.
5. Intercostal chest drains inserted if associated pneumothorax
or haemothorax
6. transferred to the operating theatre,
7. frozen
plasma
and
cryoprecipitate:
rapidly
develop
irreversible coagulopathies due to a lack of fibrinogen and
clotting factors.
Blunt trauma:
1. A B C
2. Conservative Rx
3. Surgery if: evidence of on-going blood loss despite correction
of coagulopathy and the development of signs of generalised
peritonitis.
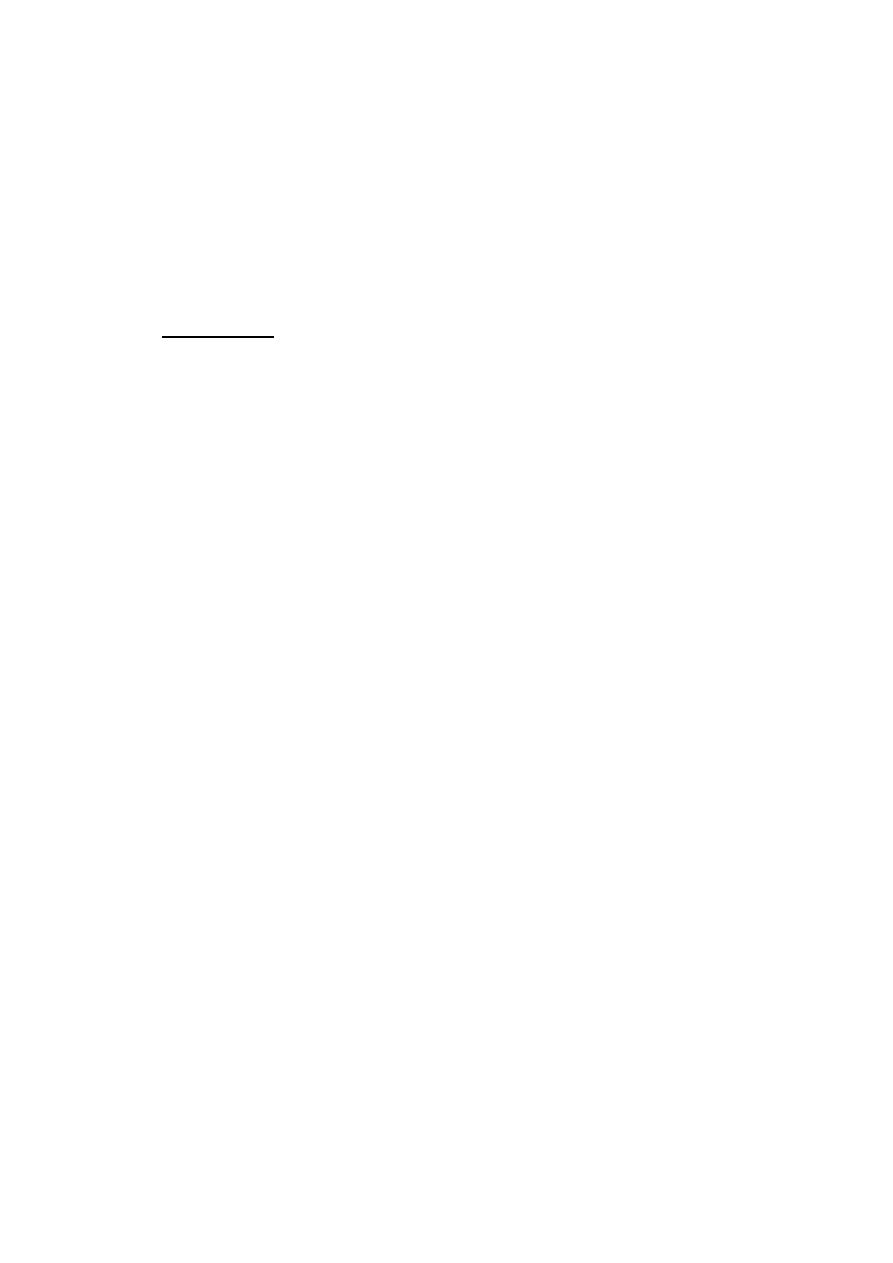
The surgical approach to liver trauma
A rooftop incision
Suturing
atraumatic clamp across the foramen of Winslow (the Pringle
manoeuvre).
abdominal packs
complications of liver trauma
A subcapsular or intrahepatic haematoma requires no
specific treatment
Abscesses as a result of secondary infection of an area
parenchymal ischaemia.
Bile collections, biliary fistulaIf
hepatic artery aneurysm and arteriovenous or arteriobiliary
fistulae
Hepatic failure may occur following extensive liver trauma.

-
4
-
Portal hypertension
Normal portal venous pressure is 80-120mmH2O
Portal HT
– 400mmH2O
Oesoph varices bleeding
– wn reach 250-300mmH2O
Sequelae: pphaematemesis, caput medusa, hypersplenisim
with
pancytopenia,
portal
vein
thrombosis,
ascites,
haemorrhoids,
Causes of PHT
1. Prehepatic: umblical sepsis, polycythemia, malignancy
obstruction, idiopathic
2. Intrahepatic: schisto, cong hepatic fibrosis, sarcoidosis, liver
intoxication, cirrhosis
3. Post-hepatic: hepatic vein obst, constrictive pericarditis
Usually produce no symptoms, But diagnosed following
presentation with chronic liver disease, encephalopathy, ascites or
variceal bleeding
Ix: CXR, Ba.swallow, IVU, Doppler-US, liver biopsy
Absolute indication for elective surgery is bleeding
oesophageal varices
Hypersplenisim & ascites: relative
Emergency Mx of bleeding varices
1. Obtain periph & central venous access
2. Adequate blood (10 units)
3. LFT & coagulation profile
4. Vitamin K (10mg) & FFP
5. Oesoph ballon tamponade
6. Drug Rx vasopressin * octreotide
7. Endoscopic scleotherapy
8. Endoscopic banding
9. TIPSS: pts not responding to druds & endoscopy
10. Surgical shunts
-
5
-
