1
Spleen
Embryology;-
Fetal splenic tissue develops from mesoderm in the dorsal mesogastrium.
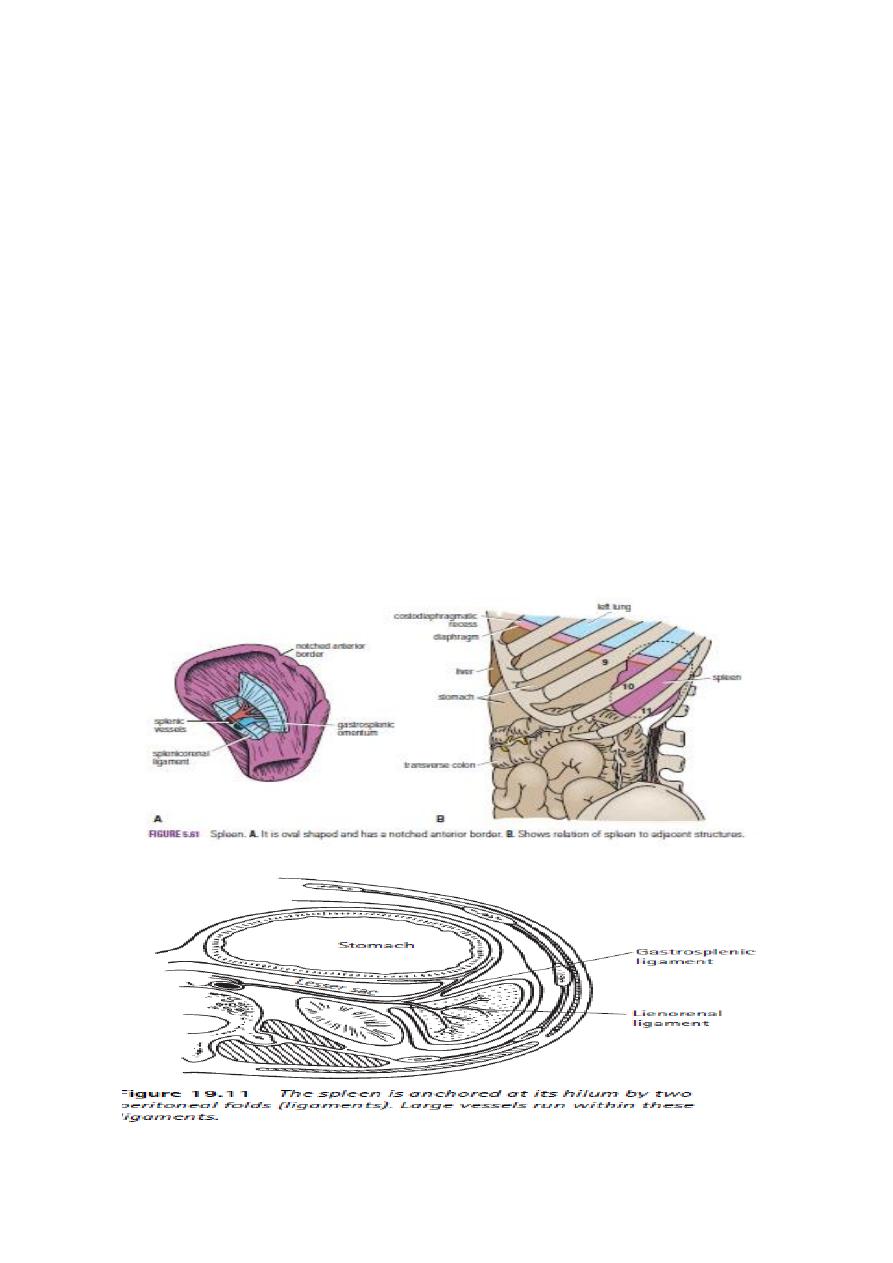
Anatomy
The weight of the normal adult spleen is 75–250 g.
It lies in the left hypochondrium between the gastric fundus and the left
hemidiaphragm, with its long axis lying along the 10th rib.
The tortuous splenic artery arises from the coeliac axis and runs along the upper
border of the body and tail of the pancreas, to which it gives small branches.
The short gastric and left gastroepiploic branches pass between the layers of the
gastrosplenic ligament.
The splenic vein is formed from several tributaries that drain the hilum. The vein runs
behind the pancreas, receiving several small tributaries from the pancreas before
joining the superior mesenteric vein at the neck of the pancreas to form the portal vein.
The lymphatic drainage comprises efferent vessels in the white pulp that run with the
arterioles and emerge from nodes at the hilum. These nodes and lymphatics drain via
retropancreatic nodes to the coeliac nodes.
Sympathetic nerve fibres run from the coeliac plexus and innervate splenic arterial
branches.

2
Functions of the spleen
■ Immune
■ Filter function
■ Pitting■ Reservoir
■ Cytopoiesis
■ Splenectomy harms the patient
•
• It is now recognised that an incidental splenectomy during the
course of another operative procedure increases the risk of complication and death.
The surgeon should normally endeavour to preserve the spleen to maintain the
following functions:
1- Immune function. The spleen processes foreign antigens and is
the major site of specific immunoglobulin M (IgM) production.
The non-specific opsonins, properdin and tuftsin, are synthesised. These
antibodies are of B- and T-cell origin and bind to the specific receptors on the
surface of macrophages and leucocytes, stimulating their phagocytic, bactericidal
and tumoricidal activity.
2- Filter function. Macrophages in the reticulum capture cellular and non-cellular
material from the blood and plasma. This will include the removal of effete
platelets and red blood cells. This process takes place in the sinuses and the
splenic cords by the action of the endothelial macrophages. Iron is removed from
the degraded haemoglobin during red cell breakdown and is returned to the
plasma. Removed non-cellular material may include bacteria and, in particular,
pneumococci.
3- Pitting. Particulate inclusions from red cells are removed, and the repaired red
cells are returned to the circulation.
These include Howell–Jolly and Heinz bodies, which represent nuclear remnants
and precipitated haemoglobin or globin subunits respectively.
4- Reservoir function. This function is less marked than in other species, but the
spleen does contain approximately 8% of the red cell mass. An enlarged spleen
may contain a much larger proportion of the blood volume.
5- Cytopoiesis. From the fourth month of intrauterine life, some degree of
haemopoiesis occurs in the fetal spleen. Stimulation of the white pulp may occur
following antigenic challenge, resulting in the proliferation of T and B cells and
macrophages. This may also occur in myeloproliferative disorders, thalassaemias
and chronic haemolytic anaemias

3
INVESTIGATION OF THE SPLEEN
1-Full blood count, reticulocyte count and tests for haemolysis ( cause of the anaemia).
2- Splenomegaly associated with portal hypertension ; abnormal tests of liver function .
3- Endoscopic evidence of oesophageal varices. Sinistral or segmental portal
hypertension may result from isolated occlusion of the splenic vein by pancreatic
inflammation or tumour.
4- Splenomegaly are associated with lymphadenopathy (Lymph node biopsy).
Radiological imaging
1-Plain radiology is rarely used ( incidental finding of calcification of the splenic artery
or spleen may raise the possible diagnosis of a splenic artery aneurysm, an old
infarct, a benign cyst or hydatid disease. Multiple areas of calcification may
suggest splenic tuberculosis.
2-Ultrasonography ; (size and consistency of the spleen, and whether a cyst is present.
3-Computerised tomography (CT) scan with contrast enhancement( the nature of the
suspected splenic pathology and to exclude other intra-abdominal pathology).
4- Magnetic resonance image (MRI) scanning may be similarly useful.
5-Radioisotope scanning is used occasionally to provide information about the spleen.
(The use of technetium-99m (99mTc)-labelled colloid is normally restricted to
determining whether the spleen is a significant site of destruction of red blood
cells)
CONGENITAL ABNORMALITIES OF THE SPLEEN
1-Splenic agenesis is rare
but is present in 10% of children with congenital heart
disease.
2-Polysplenia is a rare
condition resulting from failure of splenic fusion.
3-Splenunculi
are single or multiple accessory spleens that are found in 10–30% of the
population.
They are located near the hilum of the spleen in 50% of cases and are related to the
splenic vessels or behind the tail of the pancreas in 30%. The remainder are
located in the mesocolon or the splenic ligaments. Their significance lies in the fact
that failure to identify and remove these at the time of splenectomy may give rise
to persistent disease.
4-Hamartomas
are rarely found in life and vary in size from 1 cm in diameter to masses
large enough to produce an abdominal swelling.
5-Non-parasitic splenic cysts are rare
. True cysts form from embryonal rests and include
dermoid and mesenchymal inclusion cysts .
These are lined by flattened epithelium and should be differentiated from false cysts
that may result from trauma and contain serous or haemorrhagic fluid. The walls
of such degenerative cysts may be calcified and therefore resemble the radiological
appearances of a hydatid cyst.

4
The spleen is also a common site for pseudocyst development following a
severe attack of pancreatitis .
Pseudocysts can easily be diagnosed on scanning, and intervention is
normally required for symptomatic lesions that persist following a
period of observation.
Splenic artery aneurysm
*They are twice as common in the female and are usually situated in the
main arterial trunk.
*They are more likely to be associated with arteriosclerosis in elderly
patients.
CLINICALLY ;-The aneurysm is
1- symptomless ( detected on a plain abdominal radiograph or scan).
It is unlikely to be palpable, although a bruit may be present.
2-Rupture into the peritoneal cavity, the symptoms mimic those of splenic
rupture.
Almost half the cases of rupture occur in patients younger than 45 years of
age, and a quarter are in pregnant women, usually in the third trimester
of pregnancy or at labour.
The treatment ;-
1- splenectomy and removal of the diseased artery.
2-Embolisation or endovascular stenting following selective splenic artery
angiography .
In the younger patient with an asymptomatic splenic artery aneurysm,
surgery or interventional radiology is indicated depending on local
expertise after CT scan, MRI or selective coeliac angiography has
confirmed the diagnosis.
In the elderly patient with a calcified aneurysm, there is less risk of rupture,
and observation may be preferred.
In patients with pancreatic necrosis, the treatment will include drainage of
the septic focus.
5
Splenic infarction;
commonly occurs in patients with a massively enlarged spleen from myeloproliferative
syndrome, portal hypertension or vascular occlusion produced by pancreatic
disease, splenic vein thrombosis or sickle cell disease.
clinically ;- 1- asymptomatic.
2- left upper quadrant and left shoulder tip pain.
Diagnosis ;- A contrast-enhanced CT scan .
Treatment ;-is conservative, and splenectomy should be considered only when a septic
infarct causes an abscess.
Splenic rupture; causes ;-
1- blunt abdominal trauma, particularly (left upper quadrant of the abdomen).
2- Iatrogenic injury to the spleen (complication of any surgical procedure,) .
Rupture of a malarial spleen
Common in tropical countries, and following ‘trivial’ injury is not infrequent.
treatment ;- splenectomy .
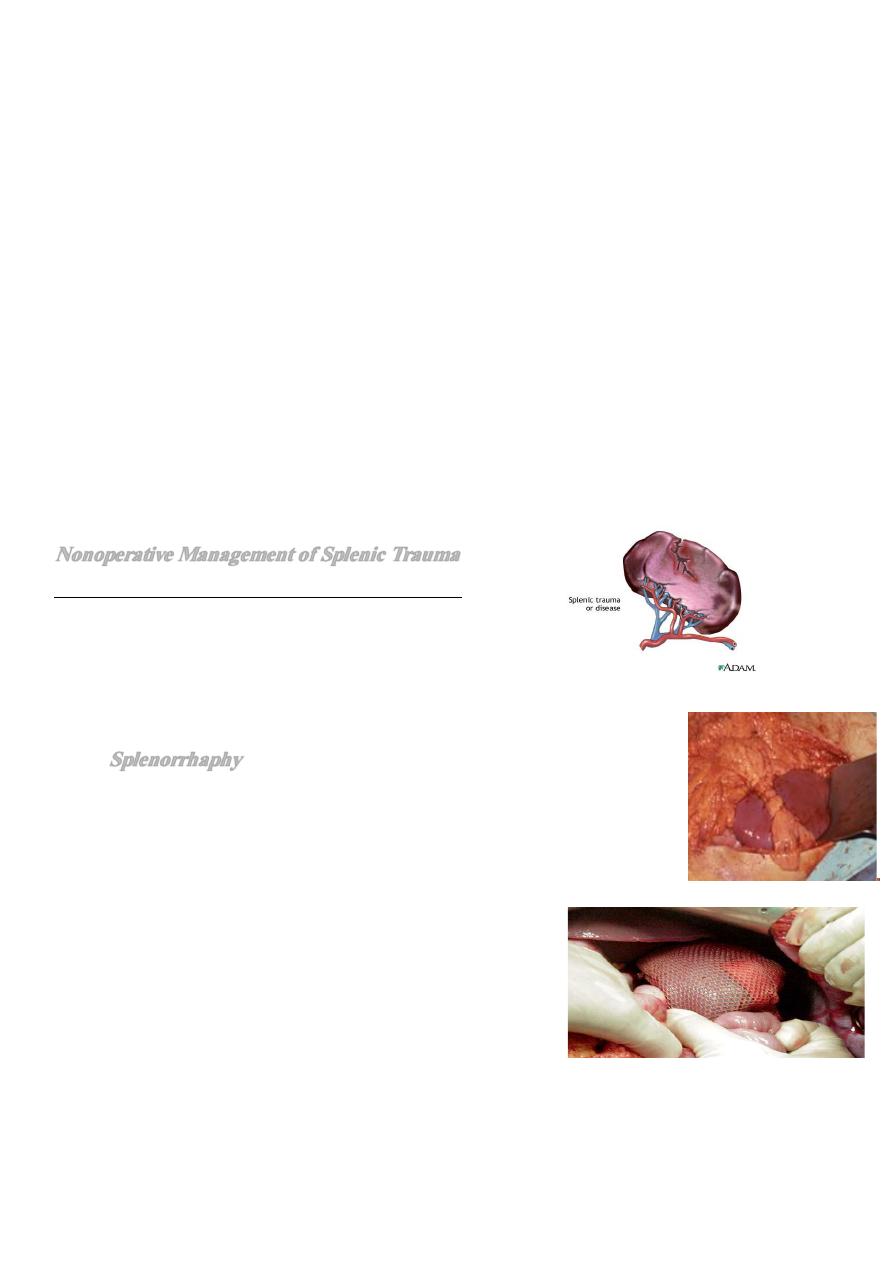
Nonoperative Management of Splenic Trauma
Indications for initial nonoperative management
• hemodynamic stability
• absence of peritonitis
• CT scan
– No contrast extravasation
– absence of other injuries
• Transfusions - >2 Packed RBC’s
•
Splenorrhaphy
• Topical Hemostasis for Small injuries (I & II)
• Bovie electrocautery / Argon beam
• Gelfoam / Surgicel / Avitene
• Suture Repair & Partial Resection
– Segmental blood supply
– Monofilament sutures
• Pledgeted horizontal mattress sutures
• Mesh Splenorrhaphy
– Delaney (1982)
• Autotransplantation
– controversial

6
SPLENOMEGALY AND HYPERSPLENISM
Hypersplenism is an indefinite clinical syndrome that is characterised by;-
( splenic enlargement, any combination of anaemia, leucopenia or thrombocytopenia,
compensatory bone marrow hyperplasia and improvement after splenectomy).
******************************************************************
Splenic abscess
Causes ;-
1-Splenic abscess may arise from an infected splenic embolus or
2- in association with typhoid and paratyphoid fever, osteomyelitis, otitis media and
puerperal sepsis.
3-It may be associated with pancreatic necrosis or other intra-abdominal infection.
Complications ;-
1- left subphrenic abscess .
2- peritonitis.
treatment ;-
1- Treat the underlying cause .
2-drainage of the splenic abscess by percutaneous means under radiological guidance.
NEOPLASMS
** Haemangioma
is the most common benign tumour of the spleen and may rarely
develop into a haemangiosarcoma that is managed by splenectomy.
The spleen is rarely the site of metastatic disease.
Lymphoma
is the most common cause of neoplastic enlargement, and splenectomy may
play a part in its management.
Splenectomy
may be required to achieve a diagnosis in the absence of palpable lymph
nodes or to relieve the symptoms of gross splenomegaly.
Myelofibrosis
results from an abnormal proliferation of mesenchymal elements in the
bone marrow, spleen, liver and lymph nodes.
Most patients present over the age of 50 years, and the spleen may produce pain owing
to its gross enlargement or from splenic infarcts.
Splenectomy reduces the need for transfusion and may relieve the discomfort resulting
from the splenomegaly.
Indications for splenectomy
Trauma;-
■ Accidental
■ Operative
Oncological;-
■ Part of en bloc resection
■ Diagnostic
■ Therapeutic

7
Haematological;-
■ Spherocytosis
■ Purpura (ITP)
■ Hypersplenism
Portal hypertension;-
■ Variceal surgery
Preoperative preparation
1-In the presence of a bleeding tendency, transfusion of blood, fresh-frozen plasma,
cryoprecipitate or platelets may be required.
Coagulation profiles should be as near normal as possible at operation, and platelets
should be available for patients with thrombocytopenia at operation and in the
early postoperative period.
2-Antibiotic prophylaxis appropriate to the operative procedure should be given, and
consideration should be given to the risk of post-splenectomy sepsis.
Technique of open splenectomy
Incision ;-
*midline or *transverse left subcostal incision for open splenectomy.
*Rarely, a thoracoabdominal incision may be necessary for a massive spleen that is
adherent to the diaphragm.
*Passage of a nasogastric tube following induction of the anaesthetic enables the
stomach to be emptied.
In elective splenectomy
, the gastrosplenic ligament is opened up, and the short gastric
vessels are divided.
The splenic vessels at the superior border of the pancreas are suture-ligated.
Accessory splenic tissue in the splenic hilum or omentum should be excluded by a
careful search at operation. There is no need to drain the wound if haemostasis is
secured adequately.
Postoperative complications
1-Immediate;- haemorrhage resulting from a slipped ligature.
2-Haematemesis from gastric mucosal damage and gastric dilatation is uncommon.
3- Left basal atelectasis is common, and a pleural effusion may be present.
4-Adjacent structures at risk during the procedure include the stomach and pancreas.
A fistula may result from damage to the greater curvature of the stomach during
ligation of the short gastric vessels. Damage to the tail of the pancreas may result
in pancreatitis, a localised abscess or a pancreatic fistula.
5-The blood platelet count may rise and, if this exceeds 1 × 106ml–1, prophylactic
aspirin is recommended to prevent axillary or other venous thrombosis.
6-Post-splenectomy septicaemia may result from Streptococcus pneumoniae, Neisseria
meningitides, Haemophilus influenzae and Escherichia coli.
The risk is greater in the young patient, in splenectomised patients treated with
chemoradiotherapy and in patients who have undergone splenectomy for
hemolytic anemias.or thrombocytopenia.

8
Opportunist post-splenectomy infection (OPSI) is a major concern.
Prophylaxis ;-
1- Appropriate and timely immunization,
2-Antibiotic prophylaxis, education and prompt treatment of infection.
It is thought that children who have undergone splenectomy before the age of 5 years
should be treated with a daily dose of penicillin until the age of 10 years.
However, all patients with compromised immune function should receive prophylaxis.
Satisfactory oral prophylaxis can be obtained with penicillin, erythromycin or
amoxicillin, or co-amoxiclav. Suspected infection can be treated intravenously with
these same antibiotics and cefotaxime, ceftriaxone or chloramphenicol in patients
allergic to penicillin and cephalosporins.
If elective splenectomy
vaccinating against pneumococcus, meningococcus
(both repeated every 5 years) and H. influenzae (repeated every 10 years).
Yearly influenza vaccination has been recommended as there is some
evidence that it may reduce the risk of secondary bacterial infection.
Pneumococcal vaccination is recommended in those patients aged over 2
years.
Haemophilus influenzae type b vaccination is recommended irrespective of
age.
In the trauma victim,
vaccination can be given in the postoperative period,
and the resulting antibody levels will be protective in the majority of
cases.
Patients who have undergone splenectomy and are travelling to countries
where malaria is present are strongly advised to use all physical anti-
mosquito barriers as well as antimalarial therapy.
OPSI
– Incidence ≈1% (up to 5%); 50% Mortality
– Encapsulated gram-positive bacteria = Streptococcus
– Risk factors
• Children < 15 yrs old
• Immunosupression
• Hematologic dz (thalassemia, SCD, etc)
• Highest within the first 2 yrs post splenectomy
–
Pnemococcus, H.influenza, meningococcus
• vaccination 7-14 days prior to splenectomy
– Pneumovax booster Q5yrs and annual H.influenza immunizations
– Abx prophylaxis for children x2 yrs post splenectomy
– Lower incidence of OPSI in adults (vs children) and after trauma
