1
SURGICAL ANATOMY
The normal thyroid gland weighs 20–25 g. The functioning unit is the lobule supplied by a
single arteriole and consisting of 24–40 follicles lined with cuboidal epithelium. The follicle
contains colloid in which thyroglobulin is stored . The arterial supply is rich, and extensive
anastomoses occur between the main thyroid arteries and branches of the tracheal and
oesophageal arteries . There is an extensive lymphatic network within the gland. Although
some lymph channels pass directly to the deep cervical nodes, the subcapsular plexus drains
principally to the central compartment juxtathyroid nodes – paratracheal nodes (level 7) and
nodes on the superior and inferior thyroid veins, and from there to the deep cervical (levels 2,
3, 4 and 5) and mediastinal groups of nodes. The normal parathyroid gland weighs up to 50
mg with a characteristic orange/brown colour and mobility within the surrounding fat and
thymic tissue.
PHYSIOLOGY
Thyroxine
The hormones tri-iodothyronine (T3) and L-thyroxine (T4) are bound to thyroglobulin
within the colloid. Synthesis within the thyroglobulin complex is controlled by several enzymes,
in distinct steps:
• trapping of inorganic iodide from the blood;
• oxidation of iodide to iodine;
• binding of iodine with tyrosine to form iodotyrosines;
• coupling of monoiodotyrosines and di-iodotyrosines to form T3 and T4.
When hormones are required, the complex is resorbed into the cell and thyroglobulin is
broken down. T3 and T4 are liberated and enter the blood, where they are bound to serum
proteins:
albumin, thyroxine-binding globulin (TBG) and thyroxinebinding prealbumin (TBPA). The small
amount of hormone that remains free in the serum is biologically active.
The metabolic effects of the thyroid hormones are due to unbound free T4 and T3 (0.03% and
0.3% of the total circulating hormones respectively). T3 is the more important physiological
2
hormone and is also produced in the periphery by conversion from T4. T3 is quick acting
(within a few hours), whereas T4 acts more slowly (4–14 days).
The pituitary–thyroid axis
The synthesis and liberation of thyroid hormones from the thyroid is controlled by thyroid-
stimulating hormone (TSH) from the anterior pituitary. Secretion of TSH depends upon the
level of circulating thyroid hormones and is modified in a classic negative feedback manner. In
hyperthyroidism, when hormone levels in the blood are high, TSH production is suppressed
whereas in hypothyroidism it is stimulated. Regulation of TSH secretion also results from the
action of thyrotrophin-releasing hormone (TRH) produced in the hypothalamus.
Calcitonin
The parafollicular C-cells of the thyroid are of neuroendocrine origin and arrive in the thyroid
via the ultimobranchial body . They produce calcitonin, which is a serum marker for recurrence
of medullary thyroid cancer.
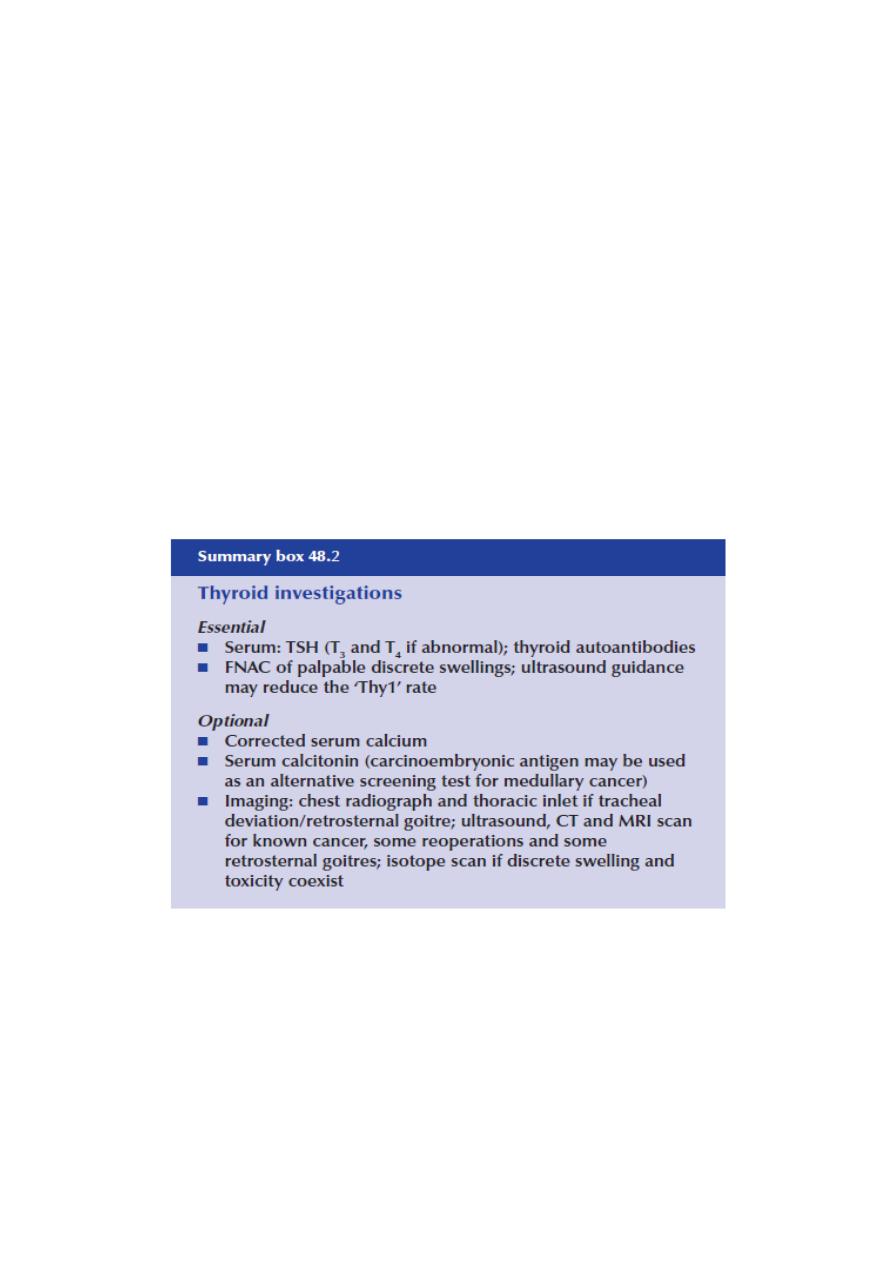
Classification of fine-needle aspiration cytology reports
Thy1 Non-diagnostic
Thy2 Non-neoplastic
Thy3 Follicular
Thy4 Suspicious of malignancy
Thy5 Malignant

3
HYPOTHYROIDISM
Cretinism (fetal or infantile hypothyroidism)
Cretinism is the consequence of inadequate thyroid hormone production during fetal and
neonatal development. ‘Endemic cretinism’ is due to dietary iodine deficiency, whereas
sporadic cases are due to either an inborn error of thyroid metabolism or complete or partial
agenesis of the gland. A hoarse cry, macroglossia and umbilical hernia in a neonate with
features of thyroid failure suggests the diagnosis.
Immediate diagnosis and treatment with thyroxine within a few days of birth are essentialto
prevent damage in utero progressing and if physical and mental development are to be
normal. Women taking anti-thyroid drugs may give birth to a hypothyroid infant and
radioactive iodine must never be given to pregnant women
Adult hypothyroidism
The term myxoedema should be reserved for severe thyroid failure and not applied to the
much commoner mild thyroid deficiency.
The
signs
of thyroid deficiency are:
1) bradycardia;
2) cold extremities;
3) dry skin and hair;

4
4) periorbital puffiness;
5) hoarse voice;
6) bradykinesis, slow movements; 7)delayed relaxation phase of ankle jerks.
The symptoms are:
1) tiredness;
2) mental lethargy;
3) cold intolerance;
4) weight gain;
5) constipation;
6) menstrual disturbance;
7) carpal tunnel syndrome.
Thyroid function tests
These show low T4 and T3 levels with a high TSH (except in the rare event of pituitary failure) .
High serum levels of TPO antibodies are characteristic of autoimmune disease.
Treatment
Oral thyroxine (0.10–0.20 mg) as a single daily dose is curative.
Caution is required in the elderly or those with cardiac disease; in such cases the replacement
dose is commenced at 0.05 mg daily and increased cautiously. If a rapid response is required,
triiodothyronine (20 μg t.d.s.) may be used.
Myxoedema
The signs and symptoms of hypothyroidism are accentuated. The facial appearance is typical;
there is often supraclavicular puffiness, a malar flush and a yellow tinge to the skin.
Myxoedema coma, characterised by altered mental state, hypothermia and a precipitating
medical condition, for example cardiac failure or infection, carries a high mortality rate.
Treatment comprises

5
thyroid replacement, either a bolus of 500 mg of T4 or 10 μg of T3 either intravenously or
orally every 4–6 hours. If the body temperature is less than 30∞C the patient must be warmed
slowly. Intravenous broad-spectrum antibiotics and hydrocortisone (in divided doses) are
recommended.
Primary or atrophic myxoedema is considered to be an autoimmune disease similar to chronic
lymphocytic (Hashimoto’s) thyroiditis (see below) but without goitre formation.
Delay in diagnosis is common and the degree of hypothyroidism is usually more severe than in
goitrous autoimmune thyroiditis.
Dyshormonogenesis
Genetic deficiencies in the enzymes controlling the synthesis of thyroid hormones account for
a minority of cases of neonatal hypothyroidism and goitre. These are usually inherited in an
autosomal recessive pattern and a family history is common.
the biochemical effect is of moderate degree, thyroid enlargement may be the only
manifestation; dyshormonogenesis should be considered in young patients presenting with
euthyroid goitre.
The most common abnormalities affect TPO activity and thyroglobulin synthesis.
A classic example of dyshormonogenesis due to TPO deficiency is Pendred’s syndrome, in
which goitre is associated with severe sensorineural hearing impairment and abnormality of
the bony labyrinth observed on CT examination of the temporal bones.
