NEOPLASMS OF THE THYROID
Classification of thyroid neoplasms
-Benign
a) Follicular adenoma
-Malignant
a)Primary b)Secondary
1)Follicular epithelium – differentiated Metastatic
i) Follicular Local infiltration
ii) Papillary
2) Follicular epithelium – undifferentiated ---- Anaplastic
3) Parafollicular cells --------- Medullary
4) Lymphoid cells ---------- Lymphoma
Benign tumours
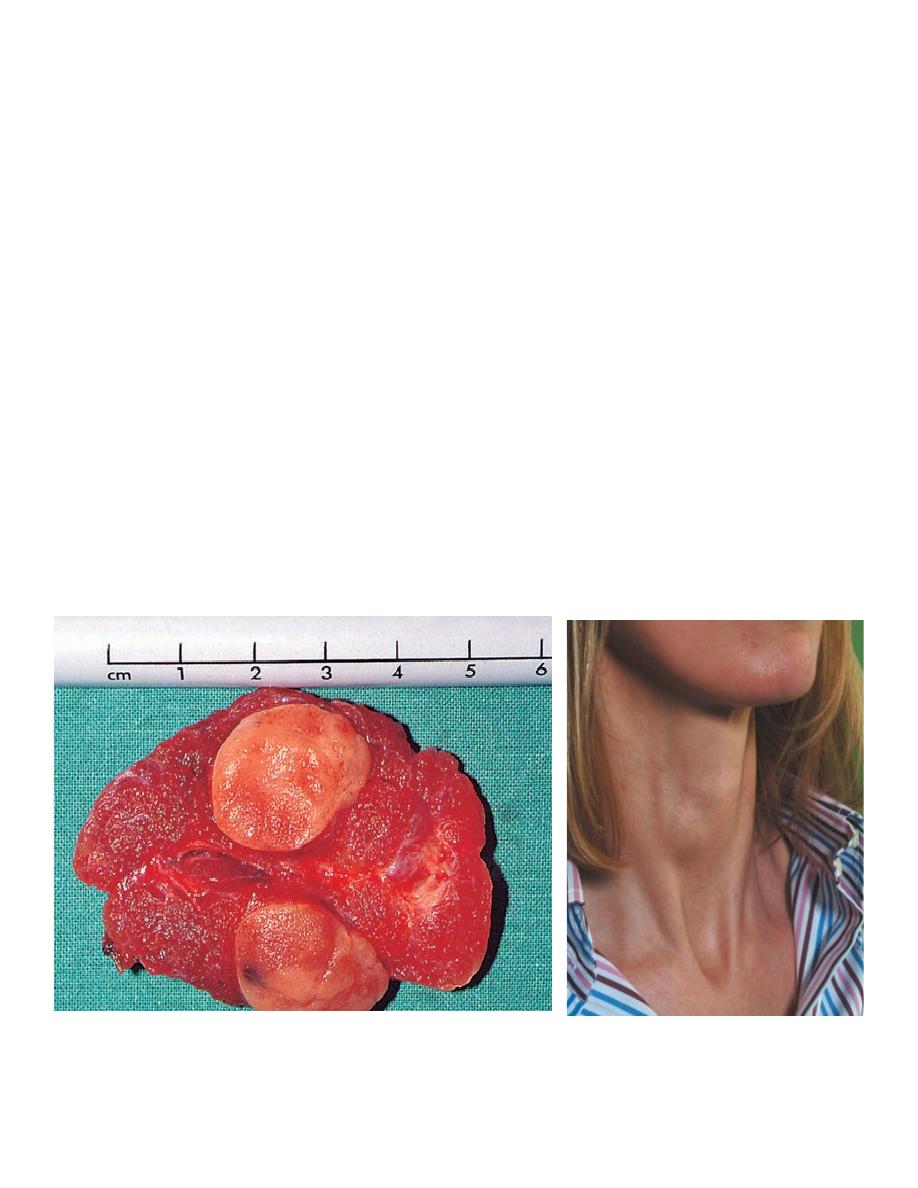
Follicular adenomas present as clinically solitary nodules and the distinction between a follicular
carcinoma and an adenoma can only be made by histological examination; in the adenoma there is no
invasion of the capsule or of pericapsular blood vessels. Treatment is therefore by wide excision, i.e.
lobectomy.
The remaining thyroid tissue is normal so that prolonged follow-up is unnecessary. All papillary
tumours should be considered as malignant, even if encapsulated.
Isolated swelling
Follicular neoplasmas an isolated swelling.
Malignant tumours
The vast majority of primary malignancies are carcinomas derived from follicular cells .
Lymphoma makes up the remainder of primary malignancies.
Metastases to the thyroid account for < 5% of malignancies.
Secondary disease should be considered when there is a history of malignancy, particularly kidney and
breast cancer, and when the cytology of a thyroid swelling is atypical. Direct invasion by upper
aerodigestive squamous cancer is a rare but lethal event. Lymph node and blood-borne metastases to
bone and lung occur and may be the mode of presentation
Aetiology of malignant thyroid tumours
The single most important aetiological factor in differentiated
thyroid carcinoma, particularly papillary carcinoma, is
irradiation of the thyroid under 5 years of age.
Short-latency aggressive papillary cancer is associated with the
ret/PTC3 oncogene and later-developing, possibly less
aggressive, cancers are associated with ret/PTC1. The incidence
of follicular carcinoma is high in endemic goitrous areas,
possibly as a result of TSH stimulation. Malignant lymphomas
sometimes develop in autoimmune thyroiditis, and the
lymphocytic infiltration in the autoimmune process may be an
aetiological factor.
Clinical features of thyroid cancers
The most common presenting symptom is a thyroid swelling
and a 5-year history is not uncommon in differentiated growths.
Enlarged cervical lymph nodes may be the presentation of
papillary carcinoma. Recurrent laryngeal nerve paralysis is very
suggestive of locally advanced disease.
Anaplastic growths are usually hard, irregular and infiltrating.
A differentiated carcinoma may be suspiciously firm and
irregular but is often indistinguishable from a benign swelling.
Small papillary tumours may be impalpable, even when
lymphatic metastases are present. Pain, often referred to the ear,
is frequent in infiltrating growths.
Diagnosis of thyroid neoplasms
Diagnosis is obvious on clinical examination in most cases of
anaplastic carcinoma, although Riedel’s thyroiditis is
indistinguishable. The localised forms of granulomatous
thyroiditis and lymphadenoid goitre may simulate carcinoma. It
is not always easy to exclude a carcinoma in a multinodular
goitre, and solitary nodules, particularly in a young male patient,
are always suspect.
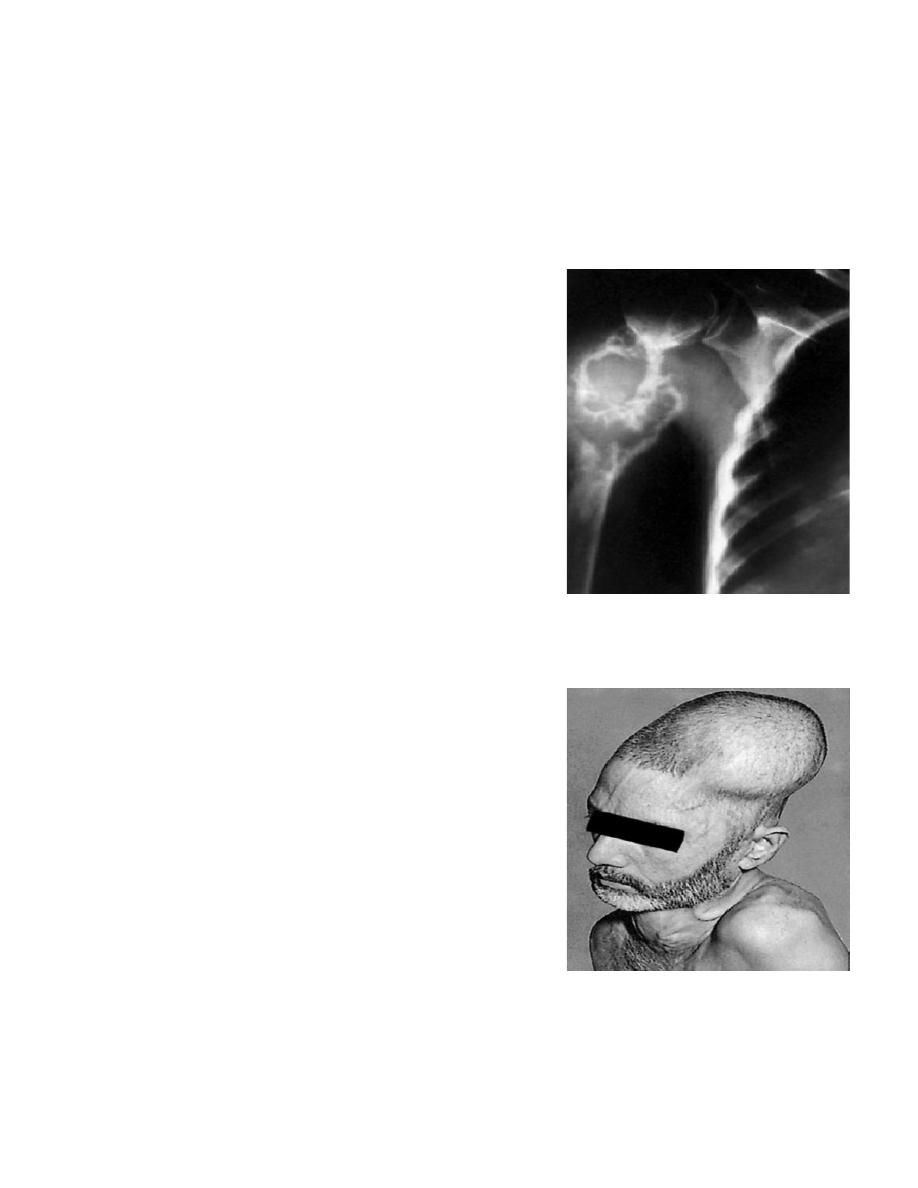
Metastasis in the humerus
from a carcinoma of the
thyroid
Metastasis in the left
parietal bone from a
carcinoma of
the thyroid
Failure to take up radioiodine is characteristic of almost all thyroid carcinomas [only very rarely will
differentiated carcinoma (primary or secondary) take up 123I in the presence of normal thyroid tissue],
but this also occurs in degenerating nodules and all forms of thyroiditis.
TSH levels are often raised in carcinoma but this may be clouded by simultaneous elevation of anti-
thyroid antibodies. Regarding FNAC there is a false-negative rate with all investigations, and lobectomy
is appropriate when there is a strong clinical suspicion. Incisional biopsy may cause seeding of cells and
local recurrence and is not advised in a resectable carcinoma. In an anaplastic and obviously
irremovable carcinoma, however, incisional or core needle biopsy is justified.
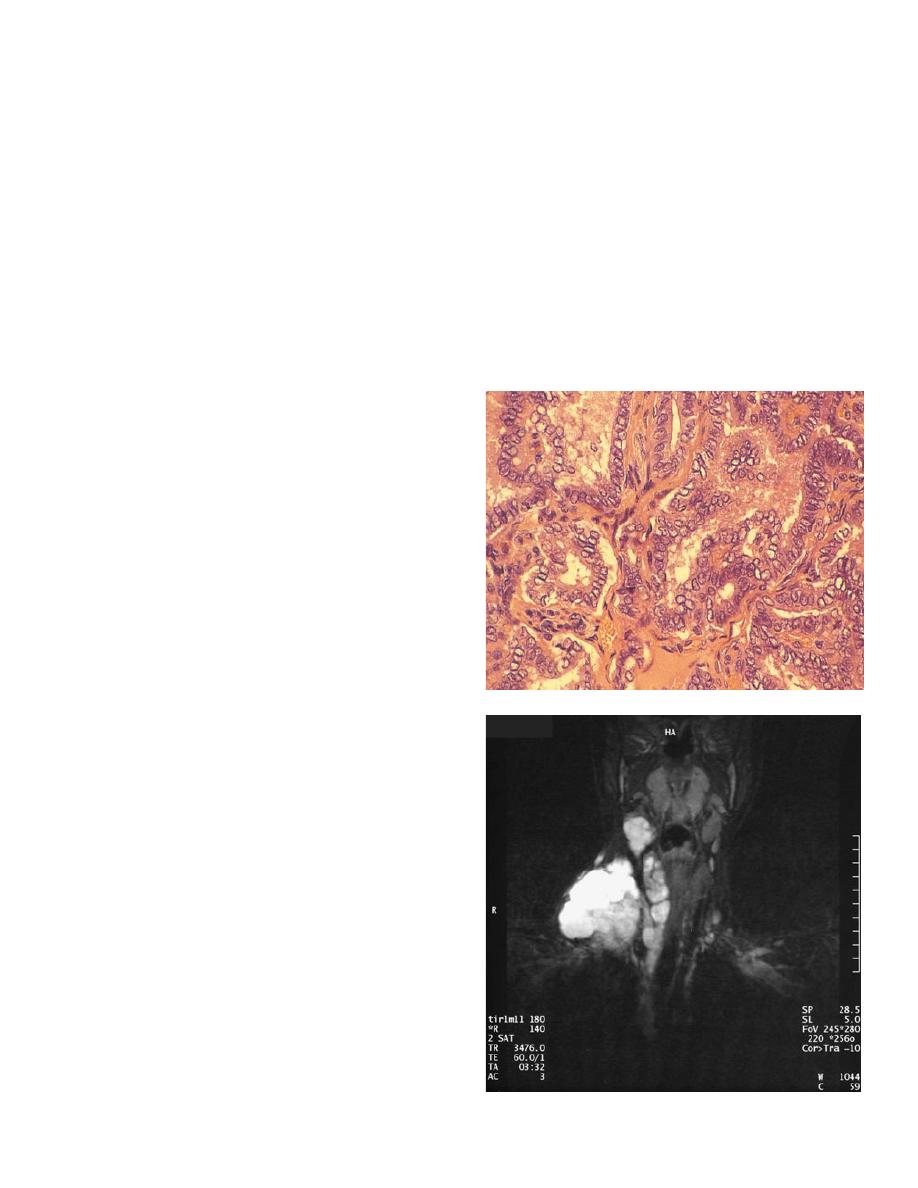
When a preoperative diagnosis is made, imaging with ultrasound, MRI or CT is required. As well as
additional information on the extent of the primary tumour, imaging provides valuable information on
nodal involvement, which permits preoperative planning for nodal dissection.
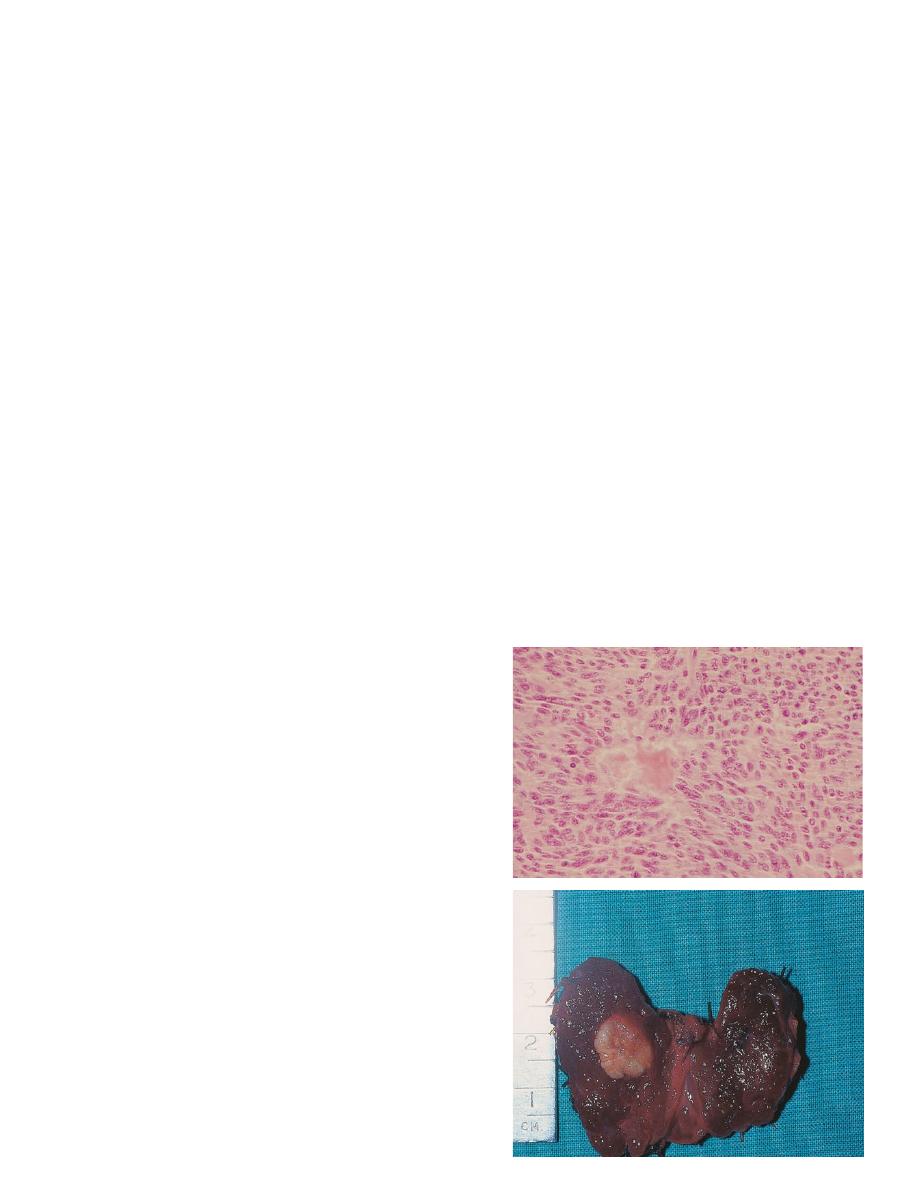
Papillary carcinoma
Most papillary tumours contain a mixture of papillary
and colloid- filled follicles and, in some, the follicular
structure predominates. Histologically the tumour
shows papillary projections and characteristic pale
empty nuclei (Orphan Annie-eyed nuclei) . Papillary
carcinomas are very seldom encapsulated.
Multiple foci may occur in the same lobe as the
primary tumour or, less commonly, in both lobes.
They may be due to lymphatic spread in the rich
intrathyroidal lymph plexus or to multicentric growth.
Spread to the lymph nodes is common but blood-
borne metastases are unusual unless the tumour is
extrathyroidal.
Microcarcinoma (occult carcinoma)
Clearly the majority of such tumours never progress
to become a clinically significant entity. A small
percentage of cancers present with enlarged lymph
nodes in the jugular chain or pulmonary metastases
with no palpable abnormality of the thyroid.
The primary tumour may be no more than a few
millimetres in size and is often termed occult. Foci of
papillary carcinoma may also be discovered in thyroid
tissue resected for other reasons, for example Graves’
disease.
Microcarcinoma applied for cancers less than
1 cm in diameter. These have a uniformly excellent
prognosis although those presenting with nodal or
distant metastases justify more aggressive therapy.
Follicular carcinoma
These appear to be macroscopically encapsulated but, microscopically, there is invasion of the capsule
and of the vascular spaces in the capsular region. Multiple foci are seldom seen and lymph node
involvement is much less common than in papillary carcinoma. Blood-borne metastases are more
common and the eventual mortality rate is twice that of papillary cancer.
Hürthle cell tumours are a variant of follicular neoplasm in which oxyphil (Hürthle, Askanazy) cells
predominate histologically. Hürthle cell cancers are associated with a poorer prognosis and some hold
that all Hürthle cell neoplasms are malignant.
Major differences between papillary and follicular
carcinoma (after Cady)
Papillary (%) Follicular (%)
Male incidence 22 35
Lymph node metastases 35 13
Blood vessel invasion 40 60
Recurrence rate 19 29
Overall mortality rate 11 24
Location of recurrent carcinoma
Distant metastases 45 75
Nodal metastases 34 12
Local recurrence 20 12
Surgical treatment of differentiated thyroid carcinoma
There is agreement that patients with large, locally aggressive or
metastatic DTC require total thyroidectomy, with excision of adjacent involved structures if necessary,
and appropriate nodal surgery followed by radioiodine ablation with long-term TSH suppression.
The conservative approach reserves total thyroidectomy for specific indications (namely those in which
there is a preoperative diagnosis of high-risk cancer, bilateral disease or when there is a clear indication
for postoperative radioiodine therapy). ‘Small’ cancers confined to one lobe can be managed by
lobectomy and TSH suppression.
Additional measures
Thyroxine
Thyroxine (0.1–0.2 mg daily) for all patients after operation for differentiated thyroid carcinoma to
suppress endogenous TSH production Failure of suppression to a level of < 0.1 mU l–1 may indicate an
inadequate dose of thyroxine or, more usually, that the patient is non-compliant..
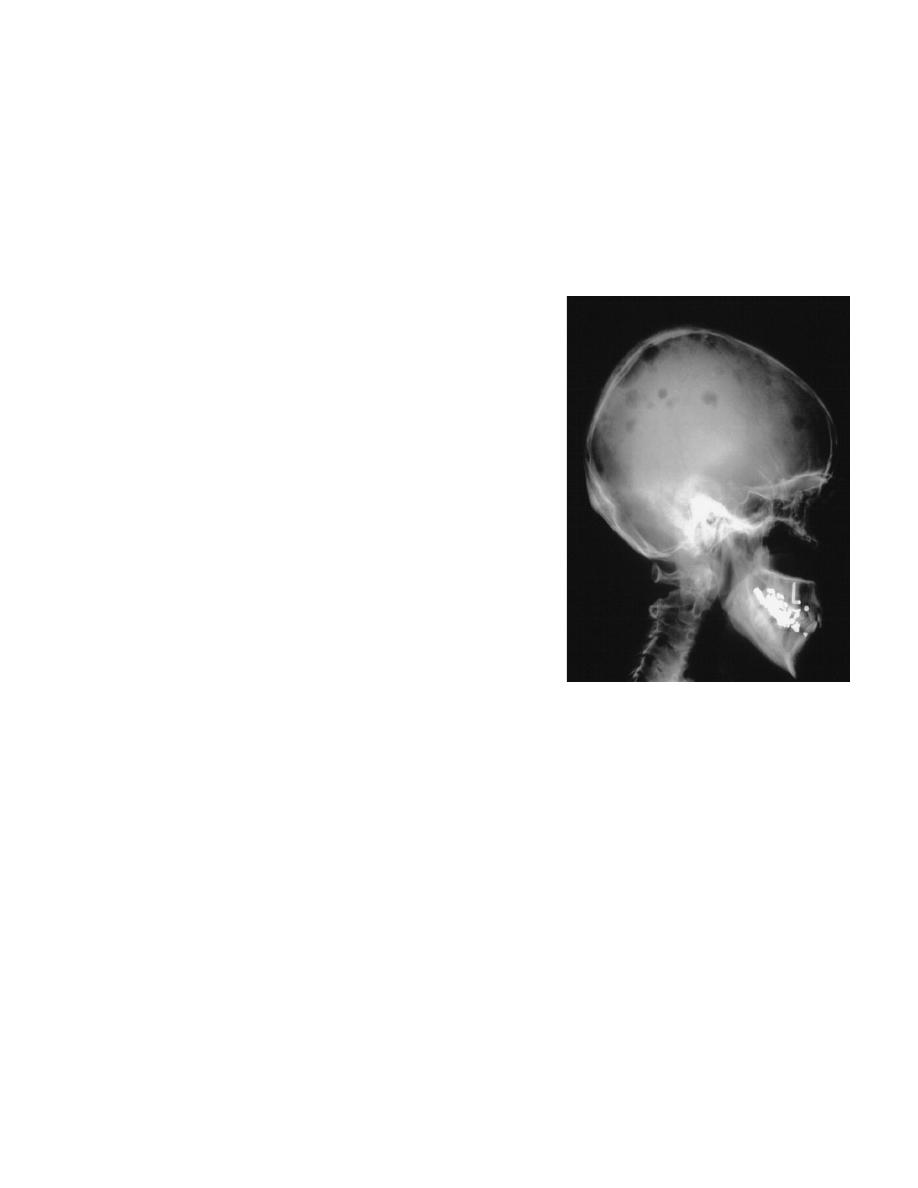
skull secondaries.
Radioiodine
If metastases take up radioiodine they may be detected by scanning and treated with large doses of
radioiodine. Radioactive iodine is indicated in patients with unresectable disease, local recurrence or
metastatic disease, high-risk patients and in those with a rising serum thyroglobulin level.
Thyroglobulin
The measurement of serum thyroglobulin is of value in the follow-up and detection of metastatic
disease in patients who have undergone surgery for DTC.
Undifferentiated (anaplastic) carcinoma
Local infiltration is an early feature of these tumours, with spread by lymphatics and by the
bloodstream. They are extremely lethal tumours and survival is calculated in months. Complete
resection is justified if the disease appears confined to the thyroid and possibly the strap muscles and is
only possible in a minority of patients.
Some of these aggressive lesions present in an advanced stage with tracheal obstruction and they
require urgent tracheal decompression. The trachea may be decompressed and tissue obtained for
histology by isthmusectomy. Tracheostomy is best avoided. Radiotherapy should be given in all cases
and may provide a worthwhile period of palliation, but there is little evidence to support the use of
chemotherapy.
Medullary carcinoma
These are tumours of the parafollicular cells (C cells) derived from the neural crest and not of cells of
the thyroid follicle. The cells are not unlike those of a carcinoid tumour and there is a characteristic
amyloid stroma.
High levels of serum calcitonin and carcinoembryonic
antigen are produced by many medullary tumours. Levels
fall after resection and rise again with recurrence making
it a valuable tumour marker in the follow-up of patients
with this disease.
Diarrhoea is a feature in 30% of cases and this may be
due to 5-hydroxytryptamine or prostaglandins produced
by the tumour cells. Some tumours are familial, possibly
accounting for 10–20% of all cases.
Medullary carcinoma may occur in combination with
adrenal phaeochromocytoma and hyperparathyroidism
(HPT) (usually due to hyperplasia) in the syndrome
known as multiple endocrine neoplasia type 2A (MEN-
2A). The familial form of the disease frequently affects
children and young adults, whereas sporadic cases occur
at any age with no sex predominance.
When the familial form is associated with prominent
mucosal neuromas involving the lips, tongue and inner

aspect of the eyelids, with a marfanoid habitus, the syndrome is referred to as MEN type 2B.
Involvement of lymph nodes occurs in 50–60% of cases of medullary carcinoma and blood-borne
metastases are common.
Treatment
Treatment is by total thyroidectomy and either prophylactic or therapeutic resection of the central and
bilateral cervical lymph nodes.
Malignant lymphoma
The response to irradiation is good and radical surgery is unnecessary once the diagnosis is established
by biopsy. Although the diagnosis may be made or suspected on FNAC, sufficient material is seldom
available for immunocytochemical classification and large-bore needle (Truecut) or open biopsy is
usually necessary.
In patients with tracheal compression, isthmusectomy is the most appropriate form of biopsy, although
the response to therapy is so rapid that this should rarely be necessary unless there has been difficulty
in making a histological diagnosis. The prognosis is good if there is no involvement of cervical lymph
nodes. Rarely, the tumour is part of widespread malignant lymphoma disease, and the prognosis in
these cases is worse. Most lymphomas occur against a background of lymphocytic thyroiditis.
THYROIDITIS
Chronic lymphocytic (autoimmune) thyroiditis
This common condition is usually associated with raised titres of thyroid antibodies. Not infrequently
there is a family history of other autoimmune disease. It commonly presents as a goitre, which may be
diffuse or nodular with a characteristic ‘bosselated’ feel, or with established or subclinical thyroid
failure.
The diagnosis often follows investigation of a discrete swelling. Features of chronic lymphocytic (focal)
thyroiditis are commonly present on histological examination in association with other thyroid
diseases, notably toxic goitre. Primary myxoedema without detectable thyroid enlargement represents
the end-stage of the pathological process.
Clinical features
The onset, thyroid status and type of goitre vary profoundly from case to case. The onset may be
insidious and asymptomatic or so sudden and painful that it resembles the acute form of
granulomatous thyroiditis. Mild hyperthyroidism may be present initially, but hypothyroidism is
inevitable and may develop rapidly or extremely slowly.
The goitre is usually lobulated and may be diffuse or localised to one lobe. It may be large or small, and
soft, rubbery or firm in consistency, depending on the cellularity and degree of fibrosis. The disease is
most common in women at the menopause but may occur at any age. Papillary carcinoma and
malignant lymphoma are occasionally associated with autoimmune thyroiditis.

Diagnosis
-Biochemical tests of thyroid function
- Thyroid antibodies
-FNAC is the most appropriate investigation
-Diagnostic lobectomy
Treatment
Full replacement dosage of thyroxine should be given for hypothyroidism and if the goitre is large or
symptomatic because some (under TSH stimulation) may subside with hormone therapy. Occasionally,
the goitre increases in size despite hormone treatment and, in these circumstances, there may be a
favourable response to steroid therapy
Thyroidectomy may be necessary if the goitre is large and causes discomfort. An increase in size of a
longstanding lymphocytic goitre should be assessed urgently because of the possibility of the
development of malignant lymphoma.
Granulomatous thyroiditis (subacute thyroiditis, de Quervain’s
thyroiditis)
Granulomatous thyroiditis is caused by a viral infection. In a typical subacute presentation there is pain
in the neck, fever, malaise and a firm irregular enlargement of one or both thyroid lobes. In 10% of
cases the onset is acute, the goitre is very painful and tender and there may be symptoms of
hyperthyroidism. One-third of cases are asymptomatic but for the presence of the goitre.
There is a raised erythrocyte sedimentation rate and absent thyroid antibodies, the serum T4 is high
normal or slightly raised and the 123I uptake of the gland is low. The condition is self-limiting and after
a few months the goitre subsides and there may be a period of months of hypothyroidism before
eventual recovery.
If diagnosis is in doubt it may be confirmed by FNAC, radioactive iodine uptake and a rapid
symptomatic response to prednisone.
The specific treatment for the acute case with severe pain is to give prednisone l0–20 mg daily for 7
days, with the dose gradually reduced over the next month. If thyroid failure is prominent, treatment
with thyroxine may be required until function recovers.
Riedel’s thyroiditis
Riedel’s thyroiditis is very rare, accounting for 0.5% of goitres. Thyroid tissue is replaced by cellular
fibrous tissue, which infiltrates through the capsule into muscles and adjacent structures, including the
parathyroids, recurrent nerves and carotid sheath.
It may occur in association with retroperitoneal and mediastinal fibrosis and is most probably a
collagen disease. The goitre may be unilateral or bilateral and is very hard and fixed. The differential
diagnosis from anaplastic carcinoma can be made with certainty only by biopsy, when a wedge of the

isthmus should also be removed to free the trachea. If the condition is unilateral the other lobe is
usually involved later and subsequent hypothyroidism is common.
Treatment is with high-dose steroids and thyroxine replacement.
BY
Muhammed Shakir Yashar M. Shakir
