
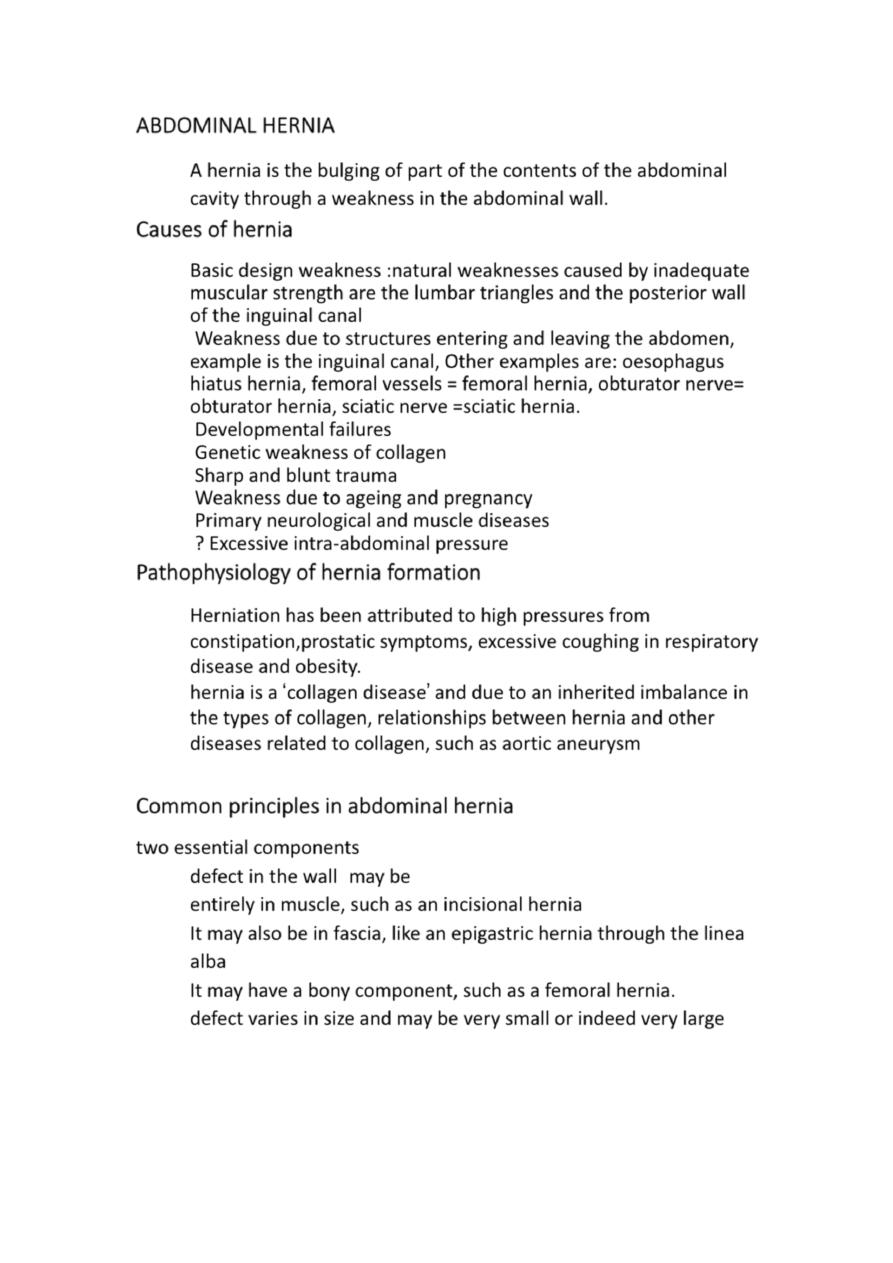
Abdominal wall hernia
Basic anatomy
Posteriorly the muscles are strong, further supported by the
vertebral column, ribs and pelvis Erector spinae, Psoas Major ,
Quadratus lumborum, Latissimus dorsi.
Laterally there are three thin muscle layers
whose fibres criss-cross for strength and flexibility, External oblique,
Internal oblique Transversus abdominis.
Anteriorly the two powerful rectus abdominus muscles extend
vertically from ribs to pelvis
ABDOMINAL HERNIA
A hernia is the bulging of part of the contents of the abdominal
cavity through a weakness in the abdominal wall.
Causes of hernia
Basic design weakness :natural weaknesses caused by inadequate
muscular strength are the lumbar triangles and the posterior wall
of the inguinal canal
Weakness due to structures entering and leaving the abdomen,
example is the inguinal canal, Other examples are: oesophagus
hiatus hernia, femoral vessels = femoral hernia, obturator nerve=
obturator hernia, sciatic nerve =sciatic hernia.
Developmental failures
Genetic weakness of collagen
Sharp and blunt trauma
Weakness due to ageing and pregnancy
Primary neurological and muscle diseases
? Excessive intra-abdominal pressure
Pathophysiology of hernia formation
Herniation has been attributed to high pressures from
constipation,prostatic symptoms, excessive coughing in respiratory
disease and obesity.
hernia is a ‘collagen disease’ and due to an inherited imbalance in
the types of collagen, relationships between hernia and other
diseases related to collagen, such as aortic aneurysm
Common principles in abdominal hernia
two essential components
1.
defect in the wall may be
entirely in muscle, such as an incisional hernia
It may also be in fascia, like an epigastric hernia through the linea
alba
It may have a bony component, such as a femoral hernia.
defect varies in size and may be very small or indeed very large
2. The content of the hernia
fat within an epigastric hernia
urinary bladder in a direct inguinal hernia
intraperitoneal structures such as bowel or omentum
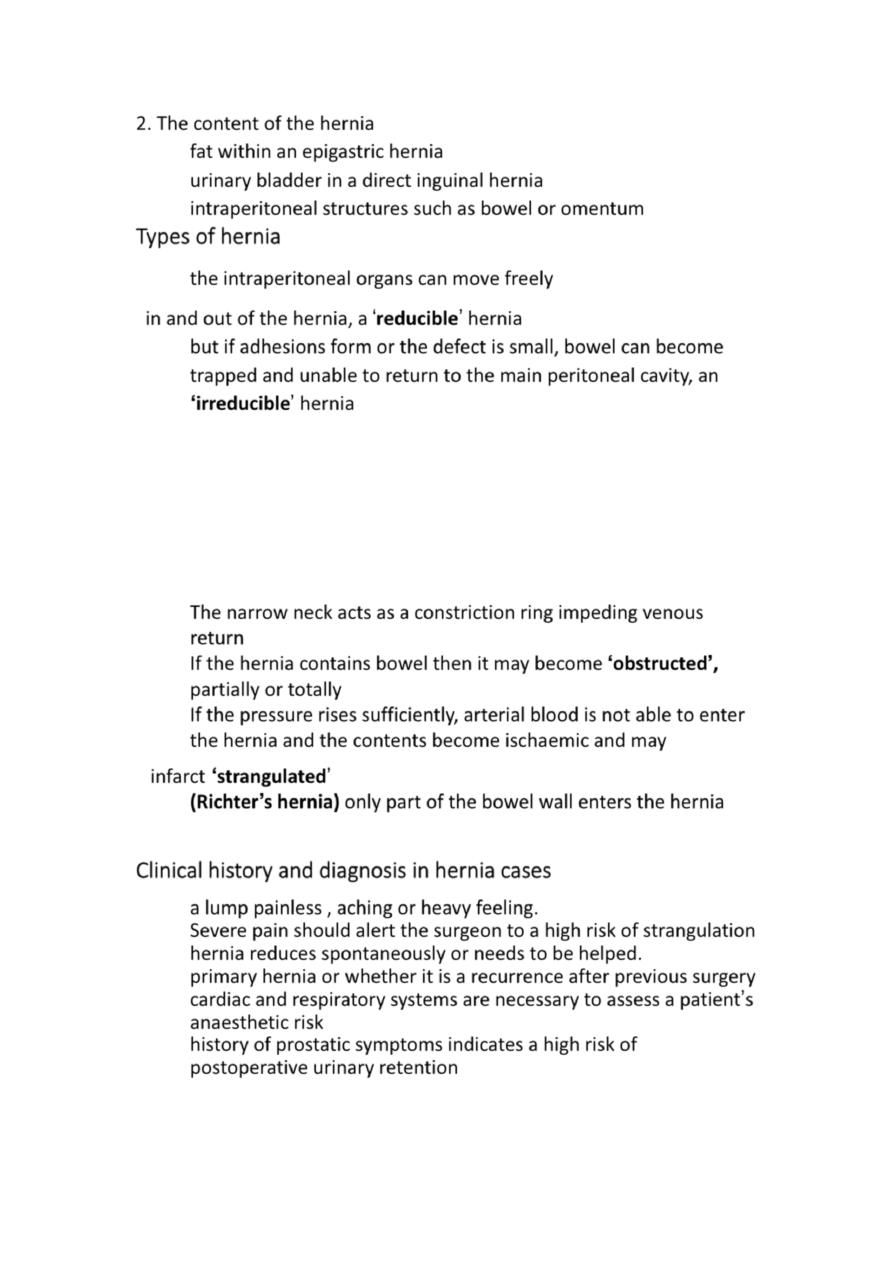
Types of hernia
the intraperitoneal organs can move freely
in and out of the hernia, a ‘reducible’ hernia
but if adhesions form or the defect is small, bowel can become
trapped and unable to return to the main peritoneal cavity, an
‘irreducible’ hernia
Interstitial hernia occurs when the hernia extends
between the layers of muscle and not directly through
them.This is typical of a Spigelian hernia.
Internal hernia bowel can enter and become trapped into
abnormal pockets of adhesions form within the peritoneal
cavity
The narrow neck acts as a constriction ring impeding venous
return
If the hernia contains bowel then it may become ‘obstructed’,
partially or totally
If the pressure rises sufficiently, arterial blood is not able to enter
the hernia and the contents become ischaemic and may
infarct ‘strangulated’
(Richter’s hernia) only part of the bowel wall enters the hernia
Clinical history and diagnosis in hernia cases
a lump painless , aching or heavy feeling.
Severe pain should alert the surgeon to a high risk of strangulation
hernia reduces spontaneously or needs to be helped.
primary hernia or whether it is a recurrence after previous surgery
cardiac and respiratory systems are necessary to assess a patient’s
anaesthetic risk
history of prostatic symptoms indicates a high risk of
postoperative urinary retention
Examination for hernia
The patient should be examined lying down initially and
then standing as this will usually increase hernia size
The patient is asked to cough,
If bruising is present this may suggest venous engorgement of the
content
if cellulitis then hernia content is strangulating
cough impulse is felt
In cases where the neck is tight and the hernia irreducible
there may be no cough impulse
Checks
Reducibility
Cough impulse
Tenderness
Overlying skin colour changes
Multiple defects/contralateral side
Signs of previous repair
Scrotal content for groin hernia
Associated pathology
A swelling with a cough impulse is not necessarily a hernia
(saphena varix)
A swelling with no cough impulse may still be a hernia
(femoral hernia)
Investigations for hernia
For most hernias, no specific investigation is required, the
diagnosis being made on clinical examination.
Plain x-ray – of little value
Ultrasound scan – mass or fluid collection, hernia content is in
doubt, haematoma or seroma/early recurrence
CT scan – incisional hernia number and size of muscle
defects, identifying the content
MRI scan – good in sportsman’s groin with pain
Contrast radiology ( herniagram)– especially for inguinal hernia
Laparoscopy – useful to identify occult contra lateral
inguinal hernia
20
%
Management
In reality, most patients with a hernia should be offered repair.
‘watchful waiting’ policy if the hernia is asymptomatic, small in
size,can be reduced easily and is not causing anxiety then
observation alone should be sufficient
Small hernias can be more dangerous than large
Pain, tenderness and skin colour changes imply high risk of
strangulation
Femoral hernia should always be repaired
Operative approaches to hernia
All surgical repairs follow the same basic principles:
1 reduction of the hernia content into the abdominal cavity
with removal of any non-viable tissue and bowel repair if
necessary;
2 excision and closure of a peritoneal sac if present or replac in it deep to
the muscles;
3 reapproximation of the walls of the neck of the hernia if possible;
4 permanent reinforcement of the abdominal wall defect with sutures or
mesh
Mesh in hernia repair
The term ‘mesh’ refers to prosthetic material, either a net or a flat
sheet which is used to strengthen a hernia repair. Mesh can
be used:
• to bridge a defect: the mesh is simply fixed over the defect as a
tension-free patch;
• to plug a defect: a plug of mesh is pushed into the defect;
• to augment a repair: the defect is closed with sutures and the
mesh added for reinforcement.
Mesh types
Woven, knitted or sheet
Synthetic or biological – mainly synthetic (synthetic polymers of
polypropylene, polyester or polytetrafluoroethylene (PTFE
biological meshes’ which are sheets of sterilised,decellularised,
non-immunogenic connective tissue. They derive from human or
animal dermis, bovine pericardium or porcine intestinal
submucosa.

Light, medium or heavyweight – lightweight becoming more
popular
Large pore, small pore – large pore causes less fibrosis and pain
Intraperitoneal use or not – non-adhesive mesh on one side
Non-absorbable or absorbable – mainly non-absorbable
Positioning the mesh
• just outside of the muscle in the subcutaneous space (onlay);
• within the defect (inlay) – only applies to mesh plugs in small
defects;
between fascial layers in the abdominal wall (intraparietal or
sublay);
• immediately extraperitoneally, against muscle or fascia (also
sublay);
• intraperitoneally.
