Page 1 of 24
E
P I D E M I O L O G Y
A Brief Introduction
Epidemiology – definition
epi – means “on, upon, befall”
epidermis: upon the body, skin
demo – means “people, population, man”
demographics
ology – means study of.
Literally epidemiology: that which befalls man.
Some see epidemiology as science, others see it as a method.
Generally seen as a scientific method to investigate disease.
Def: an investigative method used to detect the cause or source of
diseases, disorders, syndromes, conditions, or perils that cause pain,
injury illness, disability, or death in human populations or groups.
Page 2 of 24
E
P I D E M I O L O G Y
–
W
H A T I S I T
?
The study of the nature, cause, control, and determinants of the
frequency and distribution of disease, disability, and death in human
populations.
Also involves characterizing the distribution of health status,
diseases, or other health problems in terms of age, sex, race,
geography, religion, education, occupation, behaviors, time, place,
person, etc.
This characterization is done in order to explain the distribution of a
disease or health related problems in terms of the causal factors.
Serves as the foundation and logic of interventions made in the
interest of public health and preventive medicine.
It is considered a cornerstone methodology of public health
research, and is highly regarded in evidence-based medicine for
identifying risk factors for disease and determining optimal
treatment approaches to clinical practice.
In the work of communicable and non-communicable diseases, the
work of epidemiologists range from outbreak investigation to study
design, data collection and analysis including the development of
statistical models to test hypotheses and the documentation of
results for submission to peer-reviewed journals.
Epidemiologists may draw on a number of other scientific disciplines
such as biology in understanding disease processes and social
Page 3 of 24
science disciplines including sociology and philosophy in order to
better understand proximate and distal risk factors.
H
I S T O R Y
The Greek physician Hippocrates is sometimes said to be the father of
epidemiology. He is the first person known to have examined the relationships
between the occurrence of disease and environmental influences. He coined the
terms endemic (for diseases usually found in some places but not in others) and
epidemic (for disease that are seen at some times but not others).
One of the earliest theories on the origin of disease was that it was primarily the
fault of human luxury. This was expressed by philosophers such as Plato and
Rousseau, and social critics like Jonathan Swift.
In the medieval Islamic world, physicians discovered the contagious nature of
infectious disease. In particular, the Persian physician Avicenna, considered a
"father of modern medicine," in The Canon of Medicine (1020s), discovered the
Page 4 of 24
contagious nature of tuberculosis and sexually transmitted disease, and the
distribution of disease through water and soil.
Avicenna stated that bodily secretion is contaminated by foul foreign earthly
bodies before being infected. He introduced the method of quarantine as a means
of limiting the spread of contagious disease.
He also used the method of risk factor analysis, and proposed the idea of a
syndrome in the diagnosis of specific diseases.
When the Black Death (bubonic plague) reached Al Andalus in the 14th century,
Ibn Khatima hypothesized that infectious diseases are caused by small "minute
bodies" which enter the human body and cause disease.
Another 14th century Andalusian-Arabian physician, Ibn al-Khatib (1313–1374),
wrote a treatise called On the Plague, in which he stated how infectious disease
can be transmitted through bodily contact and "through garments, vessels and
earrings."
In the middle of the 16th century, a famous Italian doctor from Verona named
Girolamo Fracastoro was the first to propose a theory that these very small,
unseeable, particles that cause disease were alive.
Page 5 of 24
They were considered to be able to spread by air, multiply by themselves and to be
destroyable by fire. In this way he refuted Galen's theory of miasms (poison gas in
sick people).
In 1543 he wrote a book De contagione et contagiosis morbis, in which he was the
first to promote personal and environmental hygiene to prevent disease.
The miasmatic theory of disease held that diseases such as cholera or the Black
Death were caused by a miasma (Greek language: "pollution"), a noxious form of
"bad air". In general, this concept has been supplanted by the more scientifically
founded germ theory of disease.
The development of a sufficiently powerful microscope by Anton van
Leeuwenhoek in 1675 provided visual evidence of living particles consistent with a
germ theory of disease.
John Graunt, a professional haberdasher and serious amateur scientist, published
Natural and Political Observations ... upon the Bills of Mortality in 1662. In it, he
used analysis of the mortality rolls in London before the Great Plague to present
one of the first life tables and report time trends for many diseases, new and old.
Page 6 of 24
He provided statistical evidence for many theories on disease, and also refuted
many widespread ideas on them.
Dr. John Snow is famous for his investigations into the causes of the 19th Century
Cholera epidemics.
He began with a comparison between the death rates from areas supplied by two
adjacent water companies in Southwark.
His identification of the Broad Street pump as the cause of the SoHo epidemic is
considered the classic example of epidemiology.
He used chlorine in an attempt to clean the water and had the handle removed,
thus ending the outbreak. (It has been questioned as to whether the epidemic was
already in decline when Snow took action.)
This has been perceived as a major event in the history of public health and can
be regarded as the founding event of the science of epidemiology.
Map of Cholera
outbreaks in London
Page 7 of 24
Other pioneers include Danish physician P. A. Schleisner, who in 1849 related his
work on the prevention of the epidemic of tetanus neonatorum on the Vestmanna
Islands in Iceland.
Another important pioneer was Hungarian physician Ignaz Semmelweis, who in
1847 brought down infant mortality at a Vienna hospital by instituting a
disinfection procedure.
His findings were published in 1850, but his work was ill received by his
colleagues, who discontinued the procedure.
Disinfection did not become widely practiced until British surgeon Joseph
Lister 'discovered' antiseptics in 1865 in light of the work of Louis Pasteur.
In the early 20th century, mathematical methods were introduced into
epidemiology by Ronald Ross, Anderson Gray McKendrick and others.
Page 8 of 24
P
U R P O S E S O F
E
P I D E M I O L O G Y
To explain the etiology (cause) of a single disease or group of
diseases using information management.
To determine if data are consistent with proposed hypothesis.
To provide a basis for developing control measures and prevention
procedures for groups and at risk populations.
T
E R M S T O K N O W
Disease a pattern of response by a living organism to some form of
invasion by a foreign substance or injury which causes an alteration
of the organisms normal functioning.
also – an abnormal state in which the body is not capable of
responding to or carrying on its normally required functions.
Pathogens organisms or substances such as bacteria, viruses, or
parasites that are capable of producing diseases.
Pathogenesis the development, production, or process of generating
a disease.
Pathogenic means disease causing or producing.
Pathogenicity describes the potential ability and strength of a
pathogenic substance to cause disease.
Page 9 of 24
Infective diseases are those which the pathogen or agent has the
capability to enter, survive, and multiply in the host.
Virulence the extent of pathogenicity or strength of different
organisms.
The ability of the pathogen to grow, thrive, and to develop all
factor into virulence.
The capacity and strength of the disease to produce severe and
fatal cases of illness.
Invasiveness the ability to get into a susceptible host and cause a
disease within the host.
The capacity of a microorganism to enter into and grow in or upon
tissues of a host.
Etiology the factors contributing to the source of or causation of a
disease.
Toxins a poisonous substance that is a specific product of the
metabolic activities of a living organism and is usually very unstable.
notably toxic when introduced into the tissues, and typically
capable of inducing antibody formation.
Antibiotics a substance produced by or a semisynthetic substance
derived from a microorganism and able in dilute solution to inhibit or
kill another microorganism.
endemic: the ongoing, usual level of, or constant presence of a
disease in a given population.
Page 10 of 24
hyperendemic: persistent level of activity beyond or above the
expected prevalence.
holoendemic: a disease that is highly prevalent in a population and
is commonly acquired early in life in most all of the children of the
population.
epidemic: outbreak or occurrence of one specific disease from a
single source, in a group population, community, or geographical
area, in excess of the usual level of expectancy.
pandemic: epidemic that is widespread across a country, continent,
or large populace, possible worldwide.
incidence: the extent that people, within a population who do not
have a disease, develop the disease during a specific time period.
prevalence: the number of people within a population who have a
certain disease at a given point in time.
point prevalence: how many cases of a disease exist in a group of
people at that moment.
prevalence relies on 2 factors:
How many people have had the disease in the past.
Duration of the disease in the population.
Page 11 of 24
7
U
S E S O F
E
P I D E M I O L O G Y
1. To study the history of the disease.
Studies trends of a disease for the prediction of trends
Results of studies are useful in planning for health services and
public health.
2. Community diagnosis.
What diseases, conditions, injuries, disorders, disabilities, defects
causing illness, health problems, or death in a community or
region.
3. Look at risks of individuals as they affect populations.
What are the risk factors, problems, behaviors that affect groups?
Groups are studied by doing risk factor assessments.
4. Assessment, evaluation and research.
How well do public health and health services meet the problems
and needs of the population?
Effectiveness; efficiency; quality; access; availability of services to
treat, control or prevent disease.
5. Completing the clinical picture.
Page 12 of 24
Identification and diagnostic process to establish that a condition
exists or that a person has a specific disease.
Cause effect relationships are determined, e.g. strep throat can
cause rheumatic fever.
6. Identification of syndromes.
Help to establish and set criteria to define syndromes, some
examples are: Down, fetal alcohol, sudden death in infants, etc.
7. Determine the causes and sources of diseases
Findings allow for control prevention, and elimination of the
causes of disease, conditions, injury, disability, or death.
T
H E
E
P I D E M I O L O G Y
T
R I A N G L E
Outbreaks in a population often involve several factor and entities.
Many people, objects, avenues of transmission, and organisms can
be involved in the spread of disease.
Epidemiologists have created a model to help explain the
multifaceted phenomena of disease transmission: the epidemiology
triangle.
Many diseases rely on an agent or single factor for an infectious
disease to occur.
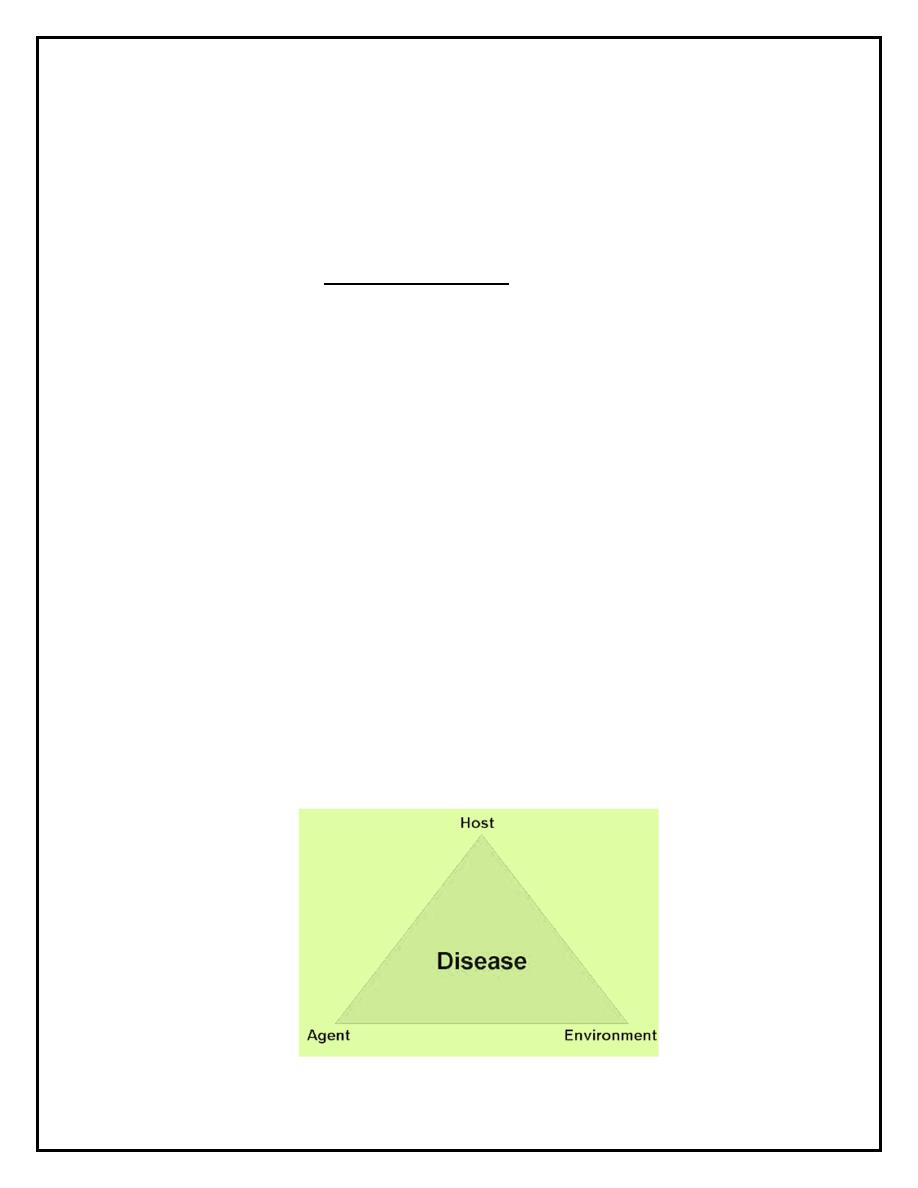
Page 13 of 24
Epidemiologist use an ecological view to assess the interaction of
various elements and factors in the environment and disease-related
implications
When more than a single cause must be present for a disease to
occur, this is called multiple causation
The interrelatedness of 4 factors contributes to the outbreak of a
disease:
1.
Role of the host
2.
Agent
3.
Environmental circumstances
4.
Time
The epidemiology triangle is used to analyze the role and
interrelatedness of each of the four factors in epidemiology of
infectious diseases, that is the influence, reactivity and effect each
factor has on the other three.
Page 14 of 24
The agent is the cause of the disease.
Can be bacteria, virus, parasite, fungus, mold
Chemicals (solvents), Radiation, heat, natural toxins (snake or
spider venom).
The host is an organism, usually human or animal, that harbors the
disease.
Pathogen disease-causing microorganism or related substance.
Offers subsistence and lodging for a pathogen.
Level of immunity, genetic make-up, state of health, and overall
fitness within the host can determine the effect of a disease
organism can have upon it.
The environment is the favorable surroundings and conditions
external to the human or animal that cause or allow the disease or
allow disease transmission.
Environmental factors can include the biological aspects as well as
the social, cultural, and physical aspects of the environment.
Time accounts for incubation periods, life expectancy of the host or
pathogen, duration of the course of illness or condition.
The mission of the epidemiologist is to break one of the legs of the
triangle, which disrupts the connection between environment, host,
and agent, stopping the continuation of an outbreak.
The goals of public health are the control and prevention of disease.
Page 15 of 24
By breaking one of the legs of the triangle, public health intervention
can partially realize these goals and stop epidemics.
An epidemic can be stopped when one of the elements of the
triangle is interfered with, altered, changed or removed from
existence.
D
I S E A S E
T
R A N S M I S S I O N
Fomites: inanimate objects that serve as a role in disease
transmission.
Pencils, pens, doorknobs, infected blankets
Vector: any living non-human carrier of disease that transports and
serves the process of disease transmission.
Insects: fly, flea, mosquito; rodents; deer.
Reservoirs: humans, animals, plants, soils or inanimate organic
matter (feces or food) in which infectious organisms live and multiply
Humans often serve as reservoir and host.
Zoonois: when an animal transmits a disease to a human.
Carrier: one that spreads or harbors an infectious organism.
Some carriers may be infected and not be sick. e.g. Typhoid Mary.
Page 16 of 24
Mary Mallon (1869 – 1938) was the first person in the United
States to be identified as a healthy carrier of typhoid fever. Over
the course of her career as a cook, she infected 47 people, three
of whom died from the disease.
Her notoriety is in part due to her vehement denial of her own
role in spreading the disease, together with her refusal to cease
working as a cook.
She was forcibly quarantined twice by public health authorities
and died in quarantine. It is possible that she was born with the
disease, as her mother had typhoid fever during her pregnancy.
Active carrier: individual exposed to and harbors a disease-causing
organism. May have recovered from the disease.
Convalescent carrier: exposed to and harbors disease-causing
organism (pathogen) and is in the recovery phase but is still
infectious.
Healthy carrier: exposed to an harbors pathogen, has not shown
any symptoms.
Incubatory carrier: exposed to and harbors a disease and is in the
beginning stages of the disease, showing symptoms, and has the
ability to transmit the disease.
Intermittent carrier: exposed to and harbors disease and can
intermittently spread the disease.
Passive carrier: exposed to and harbors disease causing organism,
but has no signs or symptoms.
Page 17 of 24
M
O D E S
D
I S E A S E
T
R A N S M I S S I O N
Methods by which an agent can be passed from one host to the next.
Or can exit the host to infect another susceptible host (either person or
animal).
Two general modes:
direct
indirect
Direct transmission or person to person
Immediate transfer of the pathogen or agent from a
host/reservoir to a susceptible host.
Can occur through direct physical contact or direct personal
contact such as touching contaminated hands, kissing or sex.
Indirect transmission
pathogens or agents are transferred or carried by some
intermediate item or organism, means or process to a
susceptible host.
done in one or more following ways:
Airborne - waterborne - vehicle borne - vector borne.
Indirect transmission
Airborne
- Droplets or dust particles carry the pathogen to the host and
infect it
- Sneezing, coughing, talking all spray microscopic droplets in
the air.
Page 18 of 24
Waterborne
- Carried in drinking water, swimming pool, streams or lakes
used for swimming. Examples: cholera.
Vehicleborne
- Related to fomites
Vectorborne
- A pathogen uses a host (fly, flea, louse, or rat) as a mechanism
for a ride or nourishment this is mechanical transmission.
biological transmission when the pathogen undergoes changes as
part of its life cycle, while within the host/vector and before being
transmitted to the new host.
C
H A I N O F
T
R A N S M I S S I O N
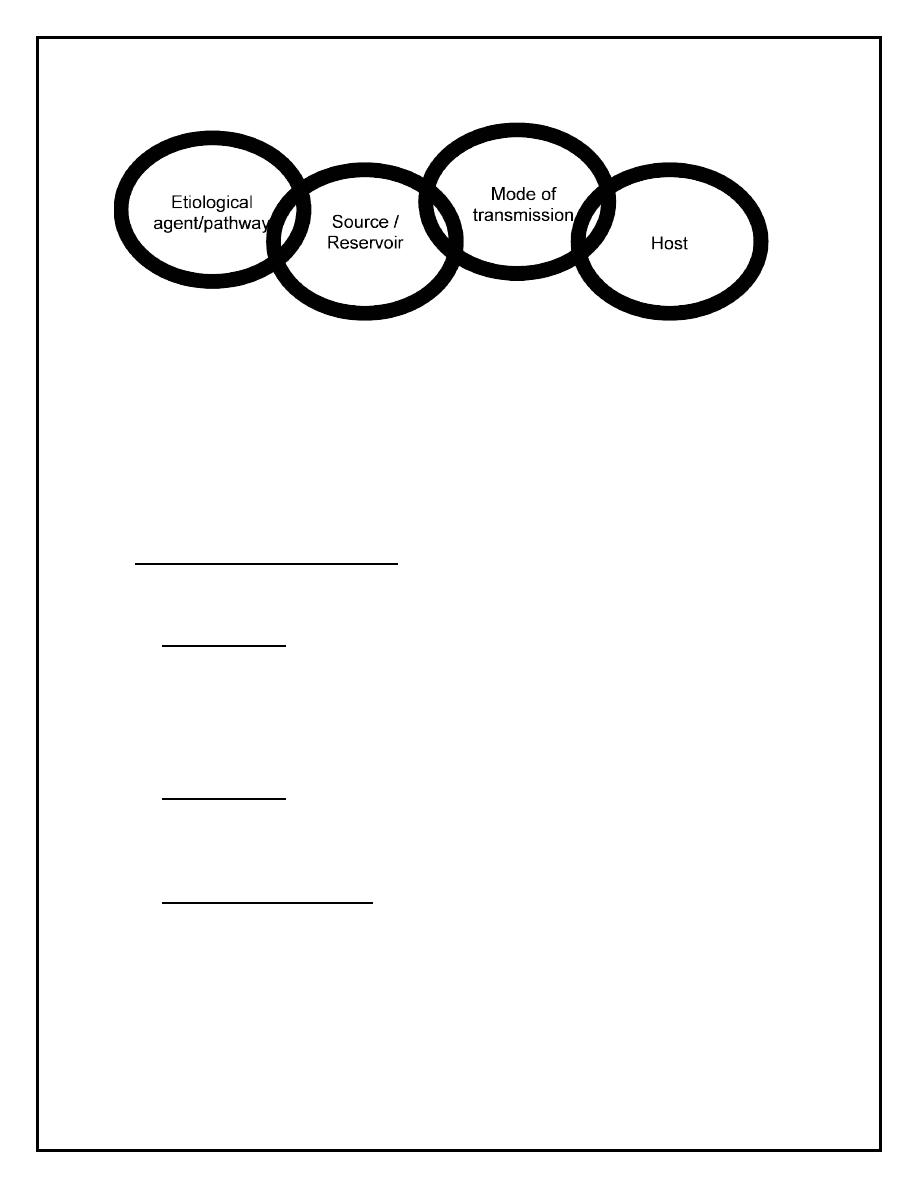
Close association between the triangle of epidemiology and the
chain of transmission.
Disease transmission occurs when the pathogen or agent leaves the
reservoir through a portal or exit and is spread by one of several
modes of transmission.
Breaks in the chain of transmission will stop the spread of disease.
Page 19 of 24
C
L A S S E S O F
E
P I D E M I C S
/
O
U T B R E A K S
Common Source Epidemic – when a group of persons is exposed to
a common infection or source of germs.
Point source from a single source (food)
- Persons exposed in one place at one time and become ill within
the incubation period.
Ex: bad mayonnaise at a picnic
Intermittent irregular and somewhat unpredictable.
- Tuberculosis spread by person to person contact and people
move around and interact with other people.
Continuous epidemic
- When an epidemic spreads through a community or population
at a high level, affecting a large number of people within the
population without diminishing.
Page 20 of 24
Propagated Epidemic
when a single source cannot be identified, yet the epidemic or
diseases continues to spread from person to person.
Usually experiences exponential growth.
Cases occur over and over longer than one incubation period.
Mixed Epidemic a common source epidemic is followed by person-
to-person contact and the disease is spread as a propagated
outbreak.
L
E V E L S O F
D
I S E A S E
Diseases have a range of seriousness, effect, duration, severity, and
extent.
Classified into 3 levels:
Acute relatively severe, of short duration and often treatable
usually the patient either recovers or dies.
Subacute intermediate in severity and duration, having some acute
aspects to the disease but of longer duration and with a degree of
severity that detracts from a complete state of health.
Patient expected to eventually heal.
Page 21 of 24
Chronic less severe but of long and continuous duration, lasting over
a long time periods, if not a lifetime.
Patient may not fully recover and the disease can get worse
overtime.
Life not immediately threatened, but may be over long term
I
M M U N I T Y A N D
I
M M U N I Z A T I O N
History
Before polio vaccine became available in 1955, 58,000 cases of polio
occurred in peak years. ½ of these cases resulted in permanent
paralysis.
Prior to measles vaccine in 1963, 4,000,000 cases per year.
Immunization of 60 million children from 1963-1972 cost $180
million, but saved $1.3 billion.
Mumps used to be the leading cause of child deafness.
10% of children with diphtheria died.
According to CDC, unless 80% or greater of the population is
vaccinated, epidemics can occur.
Page 22 of 24
Three types of immunity possible in humans:
Acquired Immunity obtained by having had a dose of a disease that
stimulates the natural immune system or artificially stimulating
immune system.
Active Immunity body produces its own antibodies
o
can occur through a vaccine or in response to having a similar
disease.
o
Similar to acquired.
Passive Immunity (natural passive) acquired through transplacental
transfer of a mother’s immunity to diseases to the unborn child (also
via breastfeeding)
o
can also come from the introduction of already produced
antibodies into a susceptible case
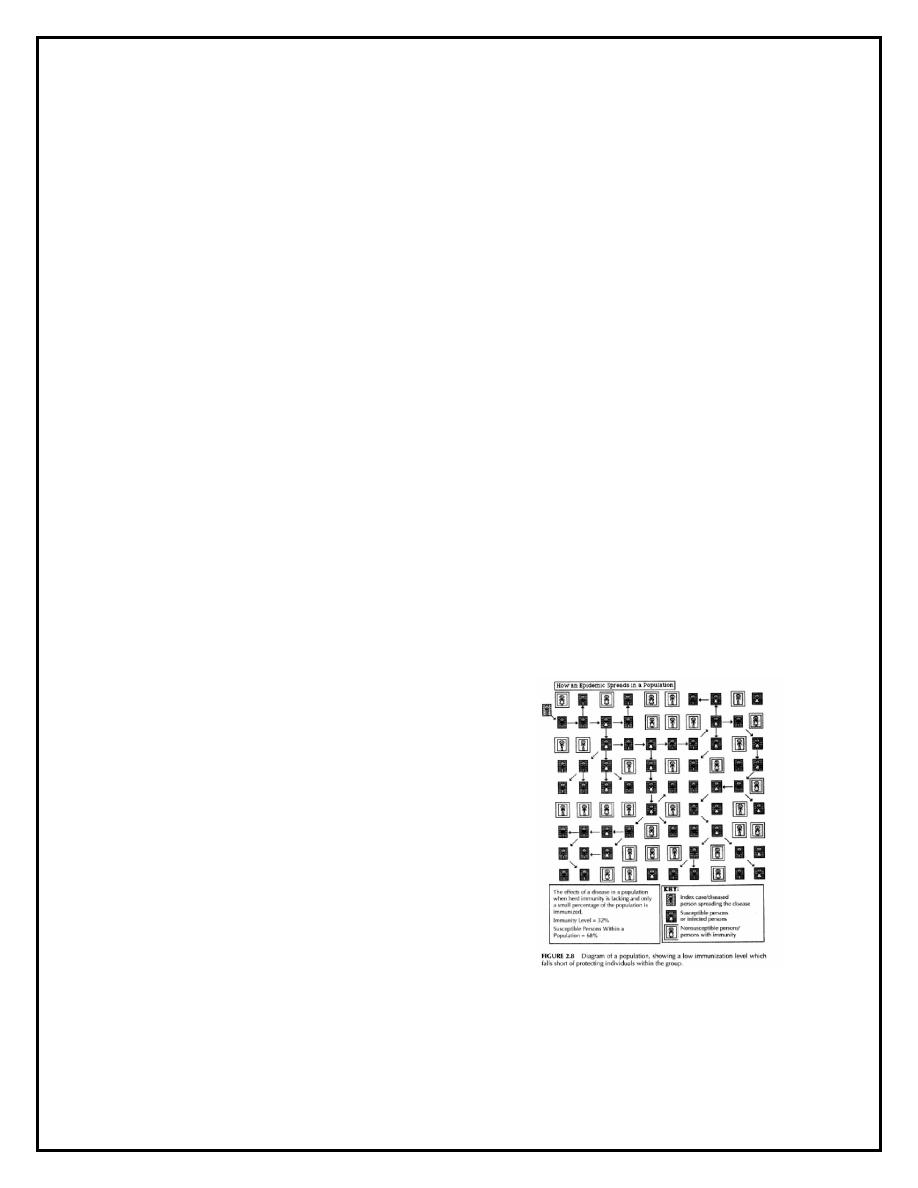
When there is little to
no immunity within a
population, the disease
spreads quickly.
Page 23 of 24
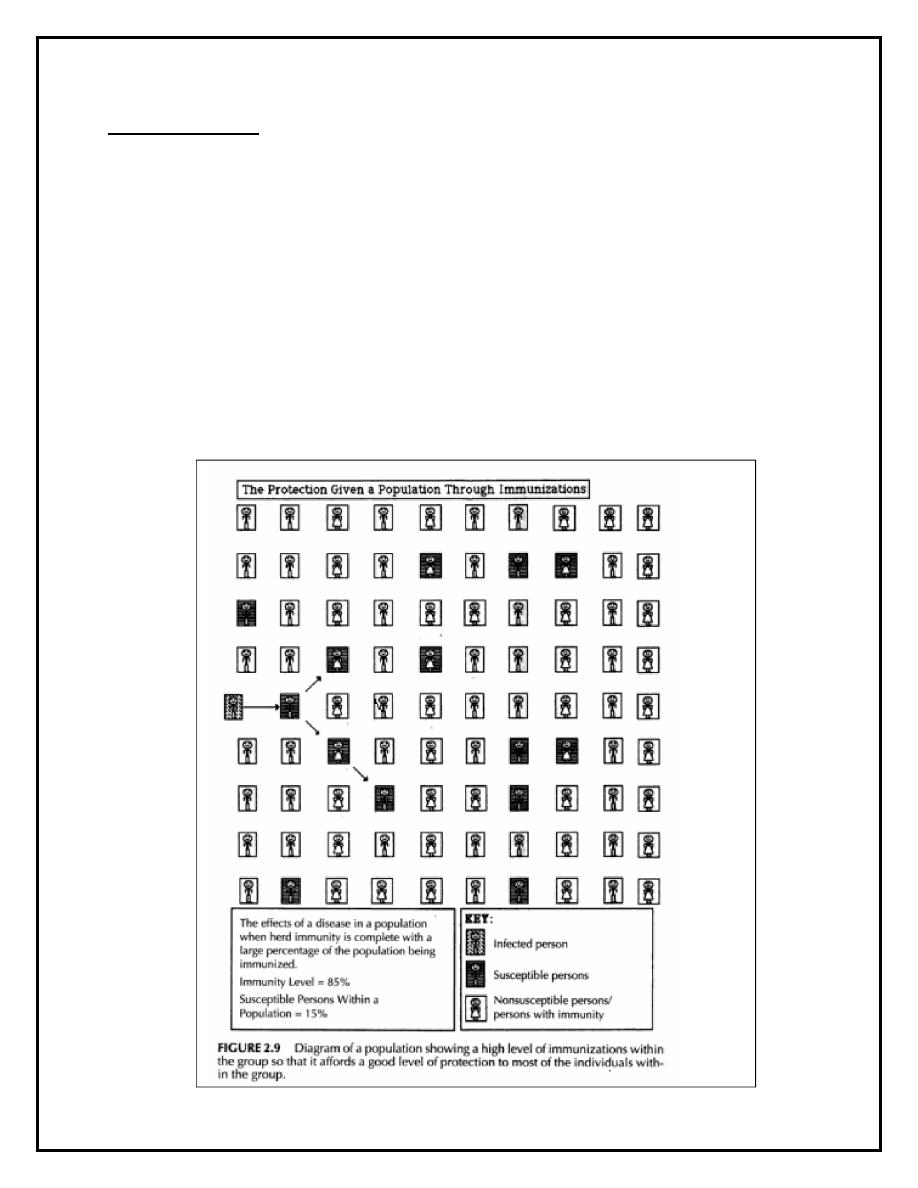
Herd Immunity
The resistance a population
or group (herd) has to the
invasion and spread of an
infectious disease.
Page 24 of 24
D
I S E A S E S F O R W H I C H V A C C I N E S A R E
U S E D
Anthrax
Influenza
Pneumonia
Tuberculosis
Chicken pox
Malaria (in
process)
Polio
Typhoid Fever
Cholera
Measles
Rabies
Typhus
Diphtheria
Meningitis
Small pox
Whooping
Cough
German
measles
(rubella)
Mumps
Spotted fever
Yellow Fever
Hepatitis A & B
Plague
Tetanus
