1
•
1/3
of the world (2 billion people) infected
•
1 person infected/second resulting in >30 million new infections, 8
million new cases
•
Left untreated 1/3 die, 1/3 self-cure, 1/3 remain infectious
•
TB kills 1 person every 10 seconds = 5000/day = 2-3 million each year
Clinical Features:
•
TB is caused by Mycobacterium tuberculosis
•
TB can affect any organ system: bone, kidney, CNS; 80% are pulmonary
•
Classic pulmonary systems of active disease: cough > 3 weeks
duration, chest pain, bloody sputum
•
Classic systemic symptoms: fever, night sweats, weight loss, malaise
•
Treated for many years with long hospitalization, surgery, myriad of
drugs leading to belief that TB is not treatable or treatment worse
than disease.
Infection vs TB Disease:
•
TB infection – organism is present, but dormant, cannot infect others
•
TB disease – person is sick and can transmit disease to others if in lungs
TB: A Global Emergency
22 High Burden Countries
•
India
•
China
•
Indonesia
•
Bangladesh
•
Pakistan
•
Nigeria
•
Philippines
•
South Africa
•
Ethiopia
•
Vietnam
•
Congo
•
Brazil
•
Tanzania
•
Kenya
•
Thailand
•
Myanmar
•
Afghanistan
•
Uganda
•
Peru
•
Zimbabwe
•
Cambodia
2
•
10%
of individuals with TB infection will develop TB disease
•
Each individual with active TB can infect 10-15 people/year
When does TB infection become disease?:
•
Most likely to occur in first two years after infection
•
If person becomes immunocompromised
✦ HIV
✦ Cancer
✦ Chemotherapy
✦ Poorly controlled diabetes
✦ Malnutrition
The 5 Essential Components of the DOTS Strategy:
✦ Government commitment to a National TB Program
✦ Priority to detect infectious cases by sputum smear microscopy
✦ Standardized regimens of short-course chemotherapy, given under direct
observation for , at least, the intensive phase
✦ Regular, uninterrupted supply of anti-TB meds
✦ Monitoring system for program supervision and evaluation
3
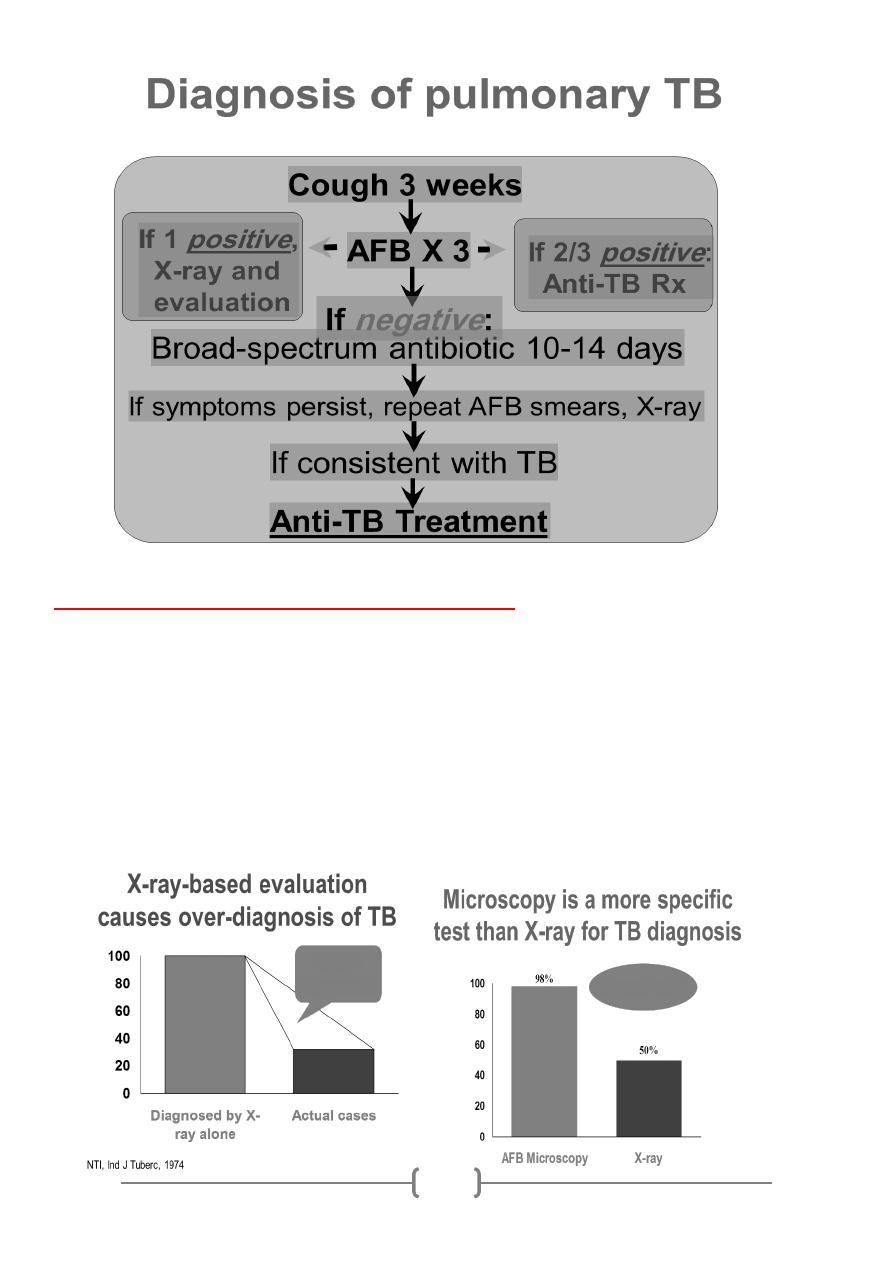
Chest X-ray (CXR) as Diagnostic Tool:
✦ No CXR pattern is typical
✦ Many TB cases are missed (10-15% culture+s(
✦ Many non-TB cases misdiagnosed (40% diagnosed by CXR alone do not have
active TB
✦ Previous MD training emphasized CXR as best diagnostic tool
✦ Often reaction to poor, inaccurate, or unavailable lab services
4
5
6
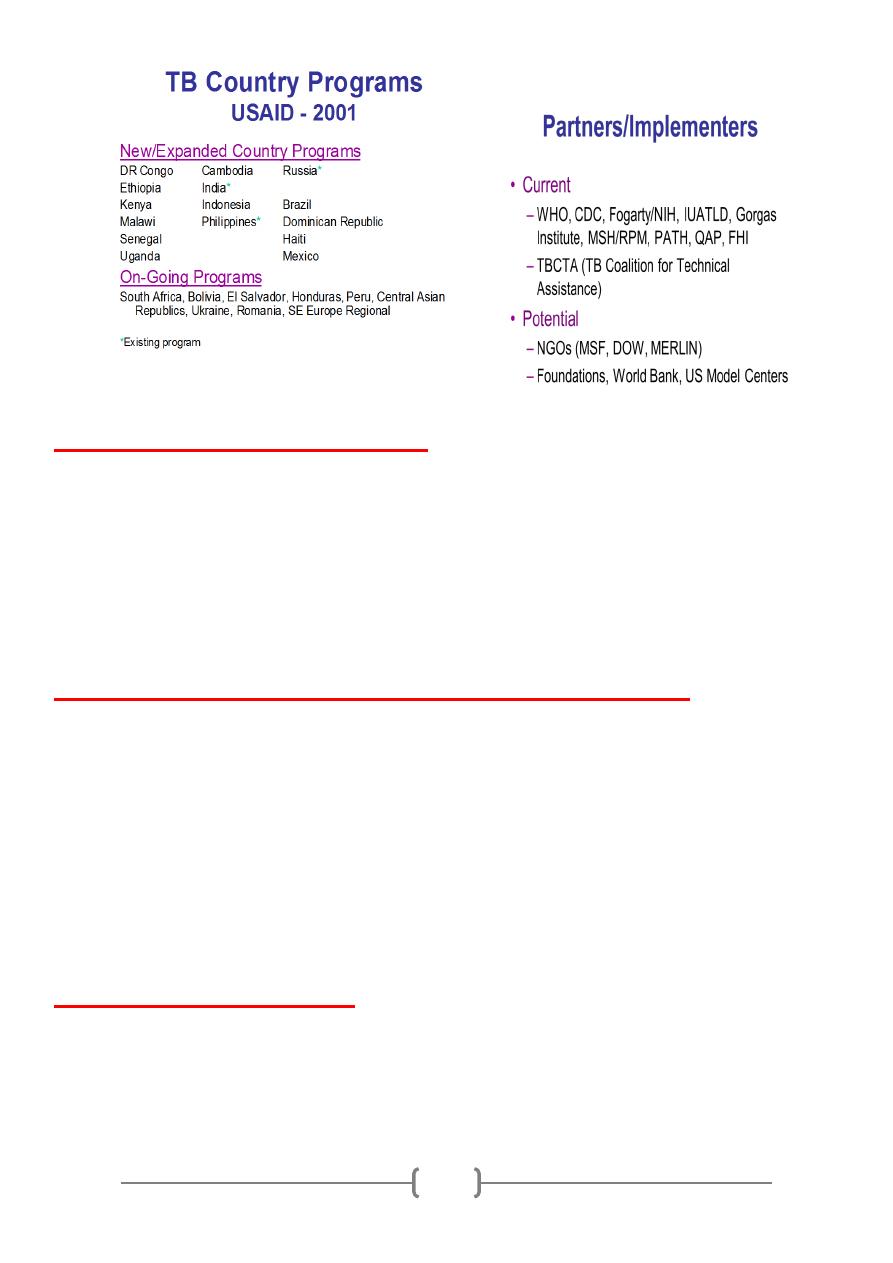
USAID TB Strategy:
✦ Support for the STOP TB Initiative
✦ Establishment of field sites/programs to serve as models for innovative
wide-scale TB control
✦ Investigation/implementation of potential technologies and
methodologies for TB prophylaxis, diagnosis, and treatment
✦ Support for surveillance to monitor TB trends and identify MDRTB
strains before they become widespread
7
USAID’s strategy to address the global TB problem was developed with the
assistance of our partners and other experts in public health and TB to maximize
the use of initial and subsequent funding levels. These consultations helped shape
the USAID TB portfolio to use funds effectively and in ways which worked to
support pre-existing programs of other donors, technical agencies, and
government programs.
USAID Expanded Response:
Continued investments in global and regional partnerships:
✦ support for the Stop TB initiative
✦ continued work with other USG agencies
✦ Global partnership to develop new anti-TB drugs
✦ Global Drug Facility
✦ New International coalition of organizations and agencies including
KNCV, IUATLD, WHO, CDC, ALA/ATS to provide TA/develop TB expertise
✦ Continued support for coordinated research to optimize diagnostics
and treatment regimens
Expanded research investments:
✦ rapid and sensitive TB diagnostic tests
✦ increase funding, work with our partners to mobilize efforts and
expertise of PH workers, industry, academic researchers, donors, other
partners in lab/OR components
✦ Target collaborative efforts to develop cost-effective TB drugs and
combination therapies
✦ Potential expansion to vaccine development
Focused, expanded programs in key countries, targeting:
✦ countries of greatest need, defined by TB burden
✦ countries with high HIV/AIDS prevalence
✦ countries at risk of escalating MDR epidemics
8
Global Programs/Mechanisms:
✦ Global/Bureau umbrella agreements with WHO and CDC
✦ Multiple agreements to address technical areas: RPM, PATH, TBCTA
✦ New interagency alliances under development for drug procurement/
management/development
✦ Standard indicators already developed
Common Health Assumptions not applicable to TB:
✦ Access is necessary but NOT sufficient
✦ Drugs
✦ Services
✦ Not every health center/NGO site appropriate as TB care center
✦ Poor program is worse than no program at all
Priorities of TB Control:
✦ Make sure the person completes TB treatment!
✦ Do not cause drug resistance; a poor TB program is worse than no TB
program!
9
✦ Treating non-pulmonary cases and those infected without active
disease are of lesser public health importance
With TB, treatment is more than treatment, treatment is prevention
Diagnosis of pulmonary TB:
✦ Patients with TB feel ill and seek care promptly
✦ Active case finding is unnecessary and unproductive
✦ Microscopy is appropriate technology, indicating infectiousness, risk of
death, and priority for treatment
✦ X-ray is non-specific for TB diagnosis
10
✦ Serological and amplification technologies (PCR, etc.) currently of no
proven value in TB control
Prompt treatment of infectious cases reduces spread of TB:
✦ Smear-positive patients usually seek care
✦ Smear-positive patients are 4-20 times more infectious
✦ Untreated, a smear-positive patient may infect 10-15 persons/year
✦ Smear-positive patients are much more likely to die if untreated
11
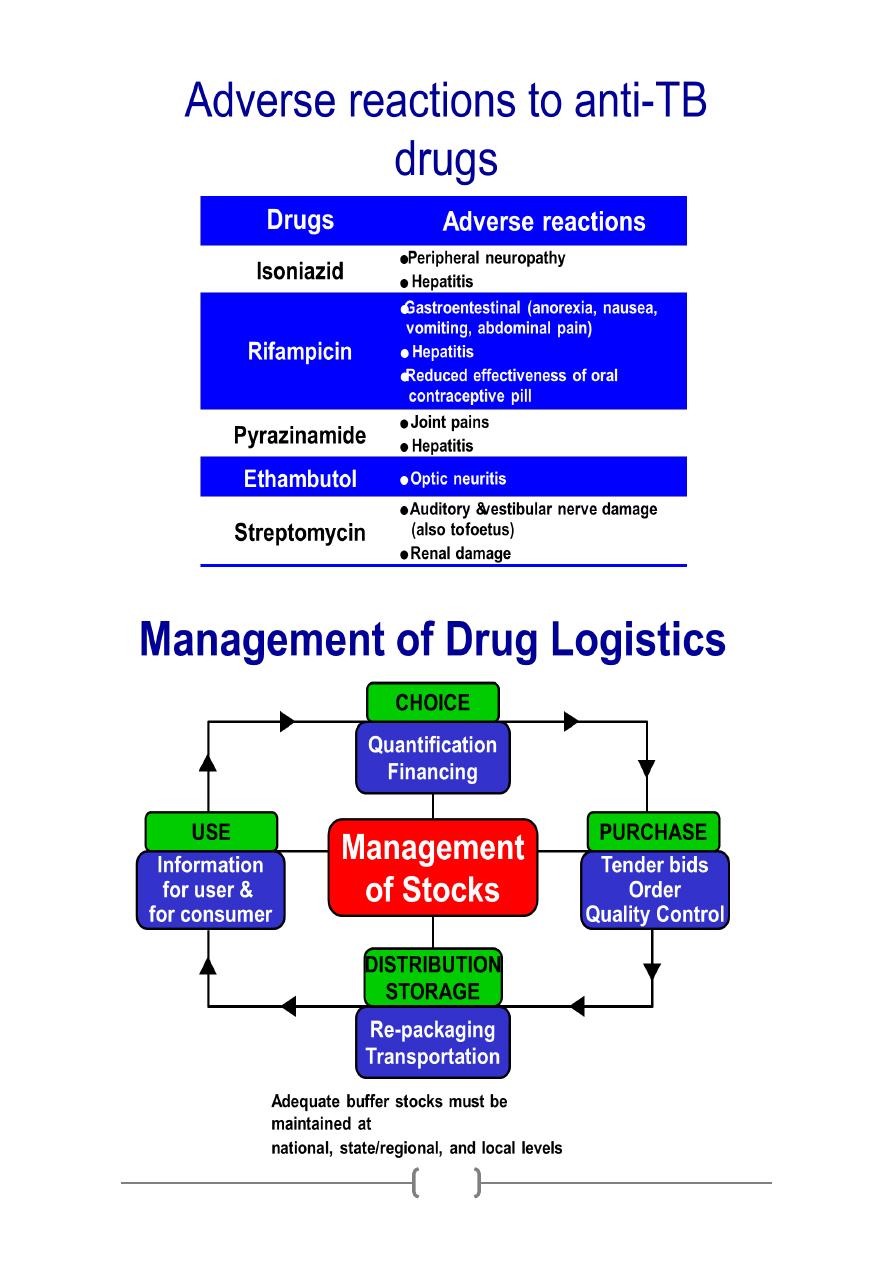
Role of Ethambutol/ Streptomycin:
✦ Prevent emergence of resistance to other drugs given
✦ Hasten sputum conversion
✦ Bacteriostatic or weakly bactericidal against rapidly dividing organisms
12
