Statistics in Screening/Diagnosis
Annie HerbertResearch & Development Department
Salford Royal Hospitals NHS Foundation Trust
annie.herbert@manchester.ac.uk
0161 2064567
Outline
Intro: Design, recording resultsSensitivity
SpecificityContinuous variables: ROC curves
Predictive valuesLikelihood ratio
Bias
Introduction: diagnostic testIntroduction: assessing a diagnostic test
All participantsIndex test
Reference test2 x 2 Table of results
+-
+
-
90
10
60
240
2 x 2 Table of results
Reference test
Index test
Introduction: 2x2 table of results
• ‘TRUTH’• (by Reference test
• – Gold standard)
• Total
• +• -
• TEST RESULT
• (by Index test)• +
• True
• Positive
• False
• Positive
• Total said to have disease
• -
• False Negative
• True Negative
• Total said not to have disease
• Total
• Total with disease
• Total without diseaseHypothetical example – Breast cancer screening study
Gold standard:Mammography
Cheaper/more convenient option:
GP examinationBreast cancer screening results
• ‘TRUTH’• (by mammography)
• Total
• +
• -• TEST RESULT (by GP Exam)
• +• 95
• 45
• 140
• -
• 5• 855
• 860
• Total
• 100
• 900• 1000
Sensitivity - Definition
What proportion of people who have the condition are identified as positive by the test?
If a test has a high sensitivity, most people with the condition are picked up by the test.
+ve test
Have conditionSensitivity - Calculation
• ‘TRUTH’• (by gold standard)
• +
• -• TEST RESULT
• +
• a
• b
• -
• c• d
• Total
• a+c
• b+d
Sensitivity = a/(a+c)
Sensitivity - Example• Mammography
• +• -
• GP Exam
• +
• 95
• 45
• -
• 5• 855
• Total
• 100
• 900
Sensitivity = 95/100 = 0.95
I.e. 95% of patients diagnosed as having breast cancer by the mammogram are picked up by GP examination.Specificity - Definition
What proportion of people who don’t have the condition are identified as negative by the test?If a test has a high specificity, most people without the condition are ruled out by the test.
-ve test
Don’t have conditionSpecificity - Calculation
• ‘TRUTH’• (by gold standard)
• +
• -• TEST RESULT
• +
• a
• b
• -
• c
• d
• Total
• a+c
• b+dSpecificity = d/(b+d)
Specificity - Example• Mammography
• +• -
• GP Exam
• +
• 95
• 45
• -
• 5
• 855
• Total
• 100
• 900Specificity = 855/900 = 0.95
I.e. 95% of patients diagnosed as not having breast cancer by the mammogram are ruled out by GP examination.Sensitivity & Specificity - Notes
It is essential to have a confirmed ‘true’ diagnosis (+ve or -ve). The accuracies of sensitivity and specificity are only as good as that of the gold standard.Sensitivity and specificity are estimated from a sample, and so should be accompanied by confidence intervals to convey amount of uncertainty.
(StatsDirect: Analysis -> Proportions -> Single)
Tests based on continuous variables (1)
One or more continuous variables can be a marker for a condition, where a very low/high level indicates a low/high likelihood of having the condition.A cut-off level can be determined where having higher/lower than that cut-off indicates a positive test result.
Different cut-off points will give different sensitivity/specificity values.
Tests based on continuous variables (2)
E.g. Creatinekinase in patients with unstable angina or acute myocardial infarctionData of Frances Boa, from ‘An introduction to Medical Statistics’ by Martin Bland
Tests based on continuous variables (3)
Sensitivity= 27/27
= 1.0
• Truth
• +• -
• Test
• +
• 27
• 54
• -
• 0
• 39
• Total
• 27
• 93Specificity
= 39/93= 0.42
Cut-off level at 80
Tests based on continuous variables (4)Sensitivity
= 26/27= 0.96
• Truth
• +
• -
• Test
• +
• 26
• 35
• -
• 1• 58
• Total
• 27
• 93Specificity
= 58/93= 0.62
Cut-off level at 100
The trade-off
Plot sensitivity against (1-specificity) to get the ROC (‘receiver operating characteristic’) curve.
Ideally want high sensitivity and high specificity (but increase in one is at expense of the other).
Also requires some clinical judgement,
e.g. Likely considered better to send women without breast cancer to have a mammogram than give those with breast cancer the all clear.Check sensitivity and specificity values in a new sample.
ROC curveROC plot for MI data
0.000.25
0.500.75
1.00
0.00
0.250.50
0.751.00
Sensitivity1-Specificity
The diagonal line represents
sensitivity = specificity,i.e. taking the test is as good as flipping a coin.
Sensitivity = 1.0
Specificity = 1.0Sensitivity = 0.0
Specificity = 0.0
Optimum cut-off
MI data:‘Optimum’ cut-off point selected = 302
Sensitivity (95% CI) = 0.93 (0.76 to 0.99)Specificity (95% CI) = 0.97 (0.91 to 0.99)
Note: ‘optimum’ assumes sensitivity and specificityof equal concern.
Area under the ROC curve
Area under the ROC curve can be between 0 (sensitivity and specificity always 0.0) and 1 (sensitivity and specificity always 1.0).Can be useful for comparing two tests.
MI data: Area under curve is an estimate of ‘probability that creatinekinase of random person with MI will be higher than for random person with angina’.The difference between sensitivity & specificity and predictive values…
Sensitivity & Specificity: How good is the test at making the right diagnosis?
Predictive Values: Once diagnosis has been made, how reliable is it?
Positive Predictive Value - DefinitionProportion of those with a positive test result that actually have the condition.
If a test has a high positive predictive value, if someone tests positive for the condition, there is a high probability that they have it.
Have condition
Test positivePositive Predictive Value - Calculation
PPV= a/(a+b)
• ‘TRUTH’
• Total
• +
• -• TEST RESULT
• +• a
• b
• a+b
• -
• c• d
• c+d
Positive Predictive Value - Example
PPV= 95/140
= 0.68
• ‘TRUTH’
• (by mammogram)• Total
• +• -
• TEST RESULT (by GP Exam)
• +• 95
• 45
• 140
• -
• 5• 855
• 860
I.e. 68% of patients who test positive for breast cancer by GP examination could be expected to test positive by mammogram.
Negative Predictive Value - Definition
Proportion of those with a negative test result that really don’t have the condition.
If a test has a high negative predictive value, if someone tests negative for the condition, there is a high probability that they don’t have it.
Don’t have condition
Test negativeNegative Predictive Value - Calculation
NPV= d/(c+d)
• ‘TRUTH’
• Total• +
• -• TEST RESULT
• +
• a
• b
• a+b
• -
• c• d
• c+d
Negative Predictive Value - Example
NPV= 855/860
= 0.99
• ‘TRUTH’
• (by mammogram)• Total
• +
• -• TEST RESULT (by GP Exam)
• +• 95
• 45
• 140
• -
• 5• 855
• 860
I.e. 99% of patients who test negative for breast cancer by GP examination would be expected to test negative by mammogram.
Prevalence
What proportion of people in a cohort have the disease? E.g. “The prevalence of breast cancer in females over 40 years of age is approximately 1.5%”.‘Prevalence’ is not the same as ‘incidence’.
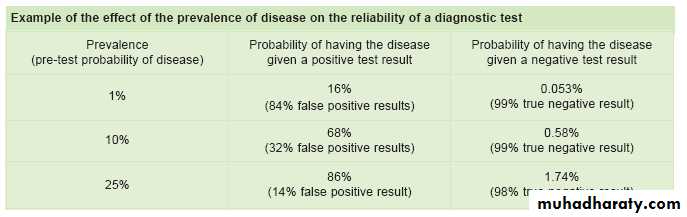
Sensitivity & specificity values are unaffected by prevalence, though predictive values are.
E.g. Test with 95% sensitivity and 95% specificity:
MeReC Briefing: supplement to issue 30Example: Self administered cognitive screening test (TYM) for detection of Alzheimer’s disease: cross sectional study, Brown et al, June 2009
“A score of 42/50 had a sensitivity of 93% and specificity of 86% in the diagnosis of Alzheimer’s disease. The TYM was more sensitive in detection of Alzheimer’s disease than the mini-mental examination, detecting 93% of patients compared with 52% for the mini-mental state examination. The negative and positive predictive values of the TYM with the cut off of 42 were 99% and 42% with a prevalence of Alzheimer’s disease of 10%.”
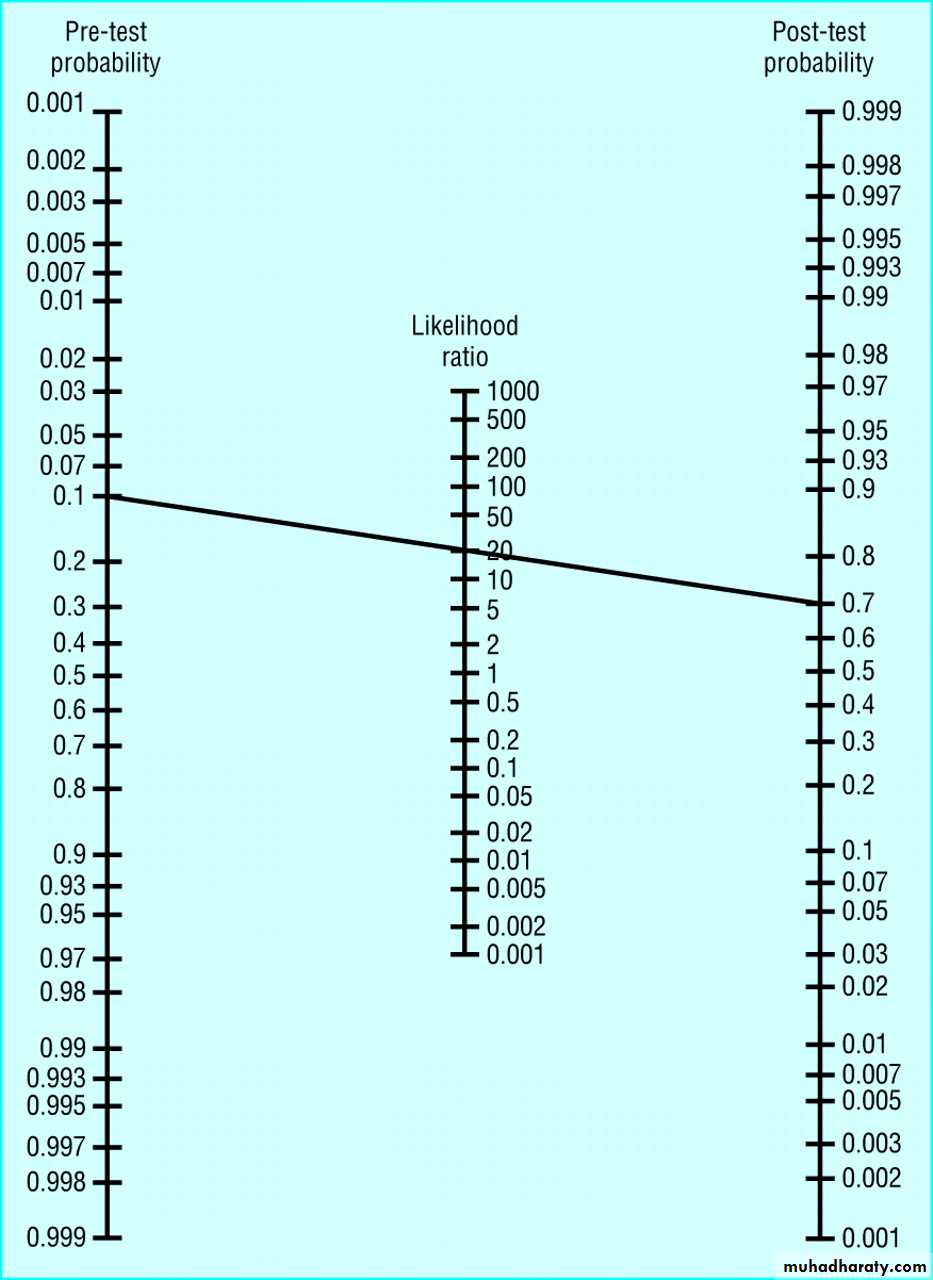
Likelihood Ratio - Definition
How many times more (or less) a patient with the condition is likely to have that particular result than a patient without the disease.Can be used to calculate the probability of individual patient having condition based on test results.
Copyright ©2004 BMJ Publishing Group Ltd.
Deeks, J. J et al. BMJ 2004;329:168-169Use of Fagan's nomogram for calculating post-test probabilities:
Bias in studies:
Is the reference appropriate?
Was the same reference used for all patients (verification bias)?
Were assessors blind to case details?Was it a ‘diagnostic case-control study’?
Which population was the test tested in?Summary
All patients must have both new test & reference test (gold standard).Report 2x2 table and give sensitivity, specificity with precision.
A good screening test is not necessarily a good diagnostic test.Test cut-offs in an independent sample.
Predictive values vary according to prevalence.Consider all potential sources of bias.
Recommended Texts
BMJ Statistics Notes:1) Sensitivity & Specificity
2) Predictive Values
3) ROC Curves
4) Likelihood Ratios