1
Community Dr.Suhyla
Epidemiology of Healthcare Associated
Infections
Healthcare Associated Infection:
Any infection that was not present or incubating at the time that the patient was
admitted to the hospital.
Healthcare-associated Infections Background:
Emerging as important public health problem throughout the world
Affect both developed and resource-limited countries
Significant burden for both the patient and for public health
Particular problem in countries
a. with rapid development of health care services
b. increasing invasive devices and procedures
c. introduction of new technology
d. infection control is not a well recognized discipline
Healthcare-associated Infections Impact:
HAIs rank among the most important causes of death in the developing world
High cost of healthcare
- Length of stay, increased use of antibiotics,
- Need for isolation, additional laboratory investigations
Organisms may be transmitted to the community (patients, staff, visitors)
Increase in antimicrobial resistance
Cost of HAI …..
2
HAI makes the news:
• Public Concern
• Quality Issues
Hospital Infections
Bacterial
• Klebsiella,
• S. aureus,
• Acinitobacter,
• Enterobacter,
• Mycobacterium Tuberculosis ….
Viral
• HCV, HIV, HBV
• Measles, influenza, Rubella
• Rotavirus, norwalk ….
Parasitic: Malaria
Fungal
3
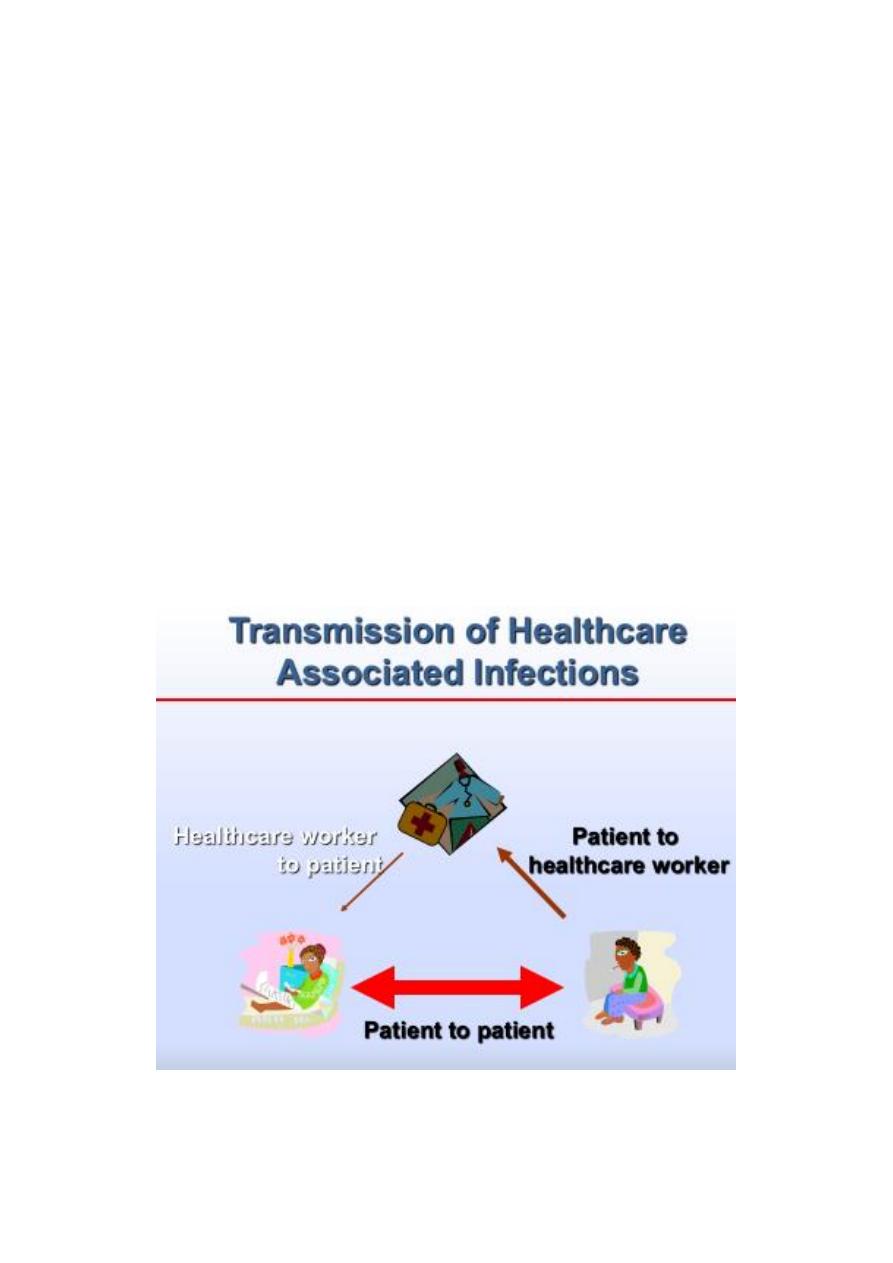
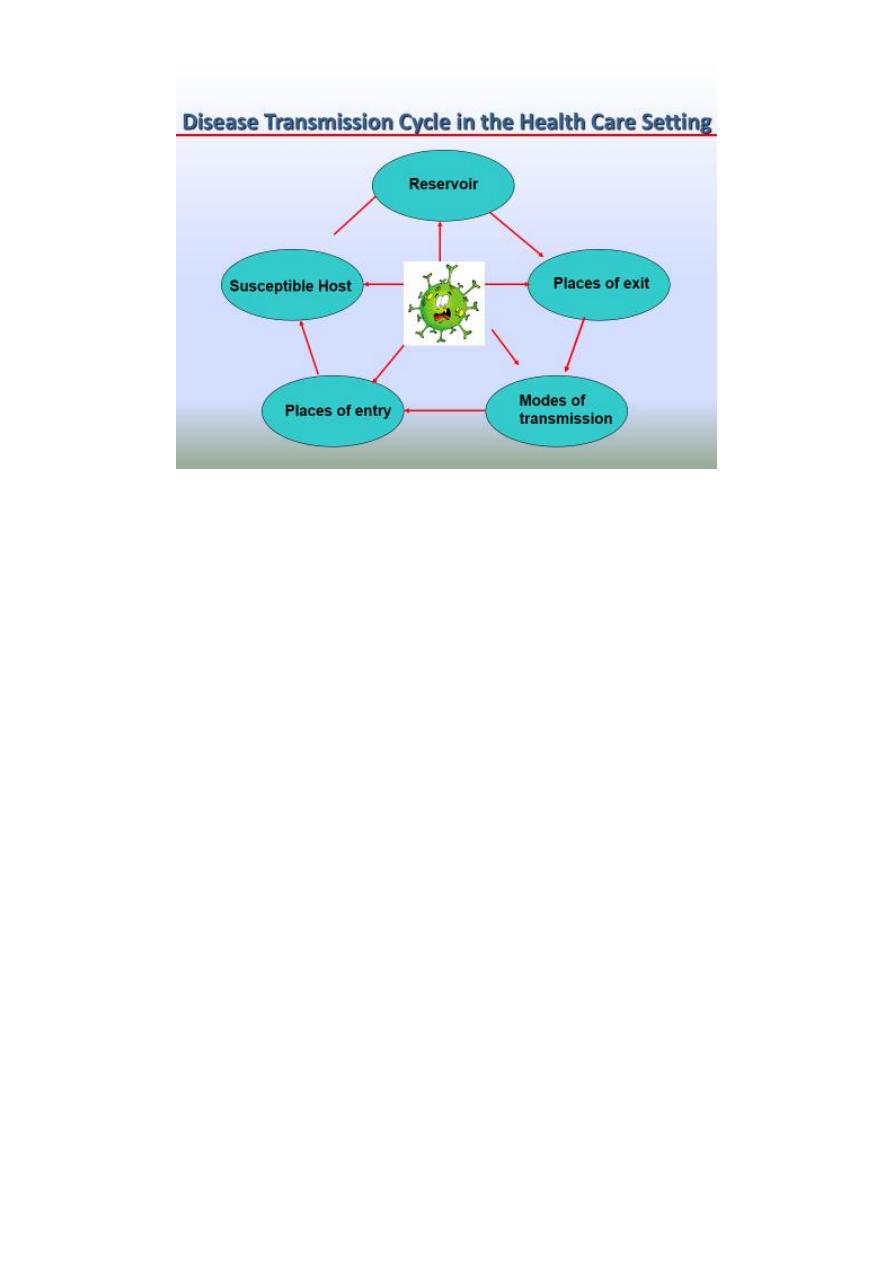
Sources of infectious Disease Transmission in the Health Care Setting
Endogenous source
A. Agent is present at the time of admission as part of
patient’s normal flora
B. Infection develops as a result of altered resistance or
introduction of microbes into normally sterile areas
4
Exogenous source
Infection occurs from introduction of microbes into or on the patient from an outside
source.
Natural Barriers to Prevent Infection
1. Skin
2. Mucous membranes
3. Humoral immunity
4. Cellular immunity.
Characterization of Healthcare Associated Infections
Conventional
Conditional
Opportunistic
Cause disease in healthy
persons
Disease in persons with
reduced immunity or when
introduced into sterile site
Generalized disease in
persons with severe
immune impairment
Staphylococcus, Salmonella,
shigella C. diphtheriae,
Mycobacterium tuberculosis,
B. pertussis,
hepatitis A, B, C, HIV …
S. agalactiae, Enterococcus
spp., C. tetani, E. coli,
Klebsiella spp., S.
marcescens, Acinetobacter
baumanii, …
Atypical mycobacteria,
N. asteroides, P. carinii,
Cryptococcus,
Cryptosporidium, ….
Transition from Colonization to Infection
Interaction between the contaminating organism and the host.
Not all colonized individuals develop infection.
Persons who have progressed from colonization to infection may represent only the
“tip of the iceberg” of persons carrying a particular pathogen
5
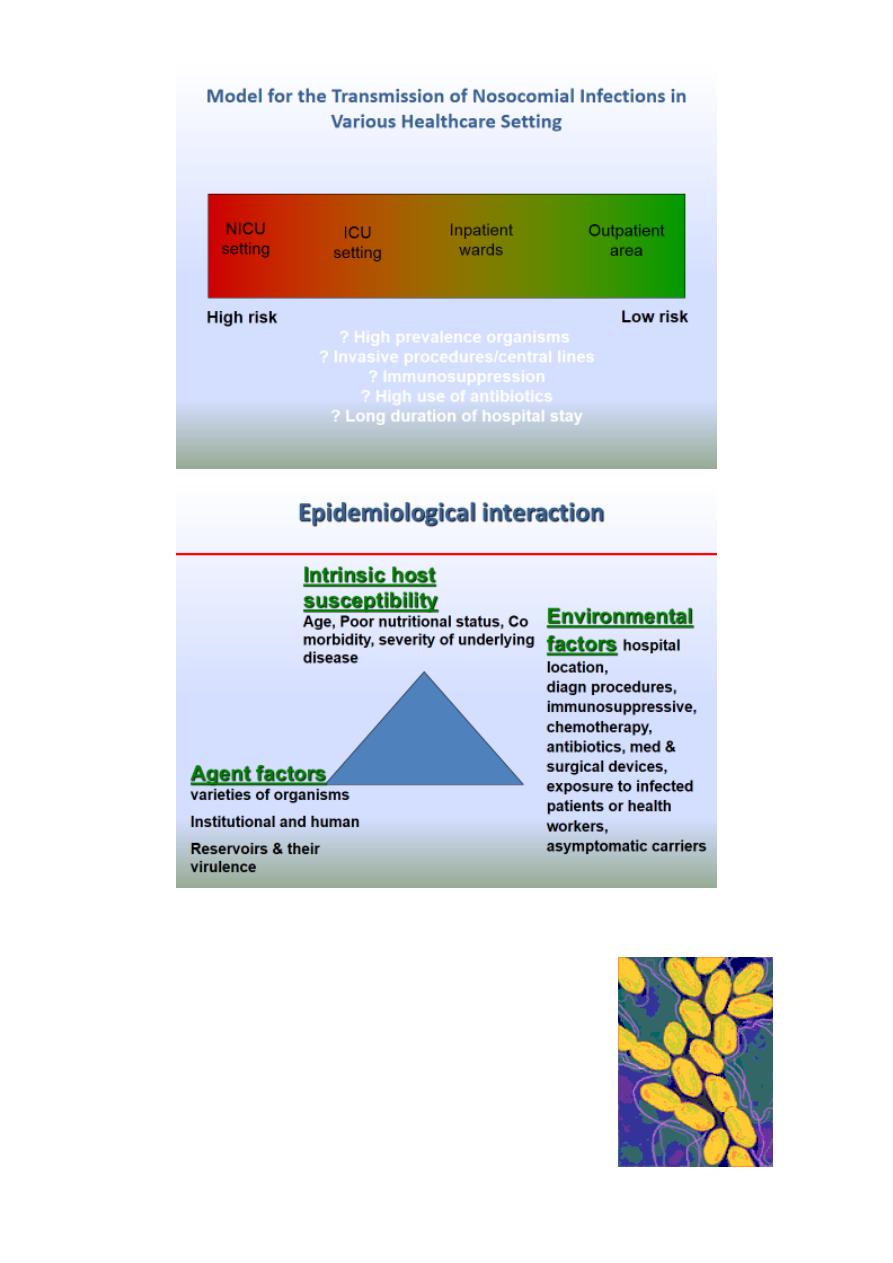
Agent Factors Related to the Development of Healthcare Associated
Infections:
D Virulence : (S. aureus, seudomonas)
D Antimicrobial resistance highly influenced by usage patterns
D Resiliency
• ability to survive in the environment
• resistance to disinfectants
Patient Factors Related to the Development of Healthcare Associated
Infections
1. Underlying disease(DM, burns, immuno-suppression)
2. Invasive procedures(urinary catheter, intravenous lines, ventilation)
3. Age
4. Nutritional status
5. Alteration of normal flora
Reservoirs Related to the Development of Healthcare Associated Infections:
1) Patients and staff
2) Air (tuberculosis, measles…)
3) Water (Acinitobacter, Klebsiella)
4) Environmental surfaces and inanimate objects(VRE, MRSA)
5) Contaminated supplies and equipment (HBV)
6
Places of Exit for Healthcare Associated Pathogens:
1. Respiratory
2. Gastrointestinal
3. Genitourinary
4. Skin, mucous membranes
5. Blood and infectious body fluids
Modes of Infectious Disease Transmission in the Healthcare Setting:
1) Contact
• Direct contact: direct contact and physical transfer.
• Indirect contact: through a contaminated object
2) Droplet transmission: Droplets generated by coughing, sneezing, or talking or by
respiratory tract procedures such as suctioning or bronchoscopy
3) Airborne transmission: Tiny droplet nuclei (< 5 microns) that remain suspended in the
air
4) Common Vehicle transmission: Transmitted indirectly by material contaminated with
the infectious agent. (eg. Contaminated food, blood products, water, or contaminated
instruments and other items).
5) Vector transmission: Transmitted through insects and other invertebrate animals
(e.g., mosquitoes can transmit malaria and yellow fever; fleas can transmit plague).
Places of Entry in the Development of Healthcare Associated Infections
A. Portals of entry
- Percutaneous
- Mucous membrane
- Surgical site
B. Contributing factors
- Equipment
- Invasive devices
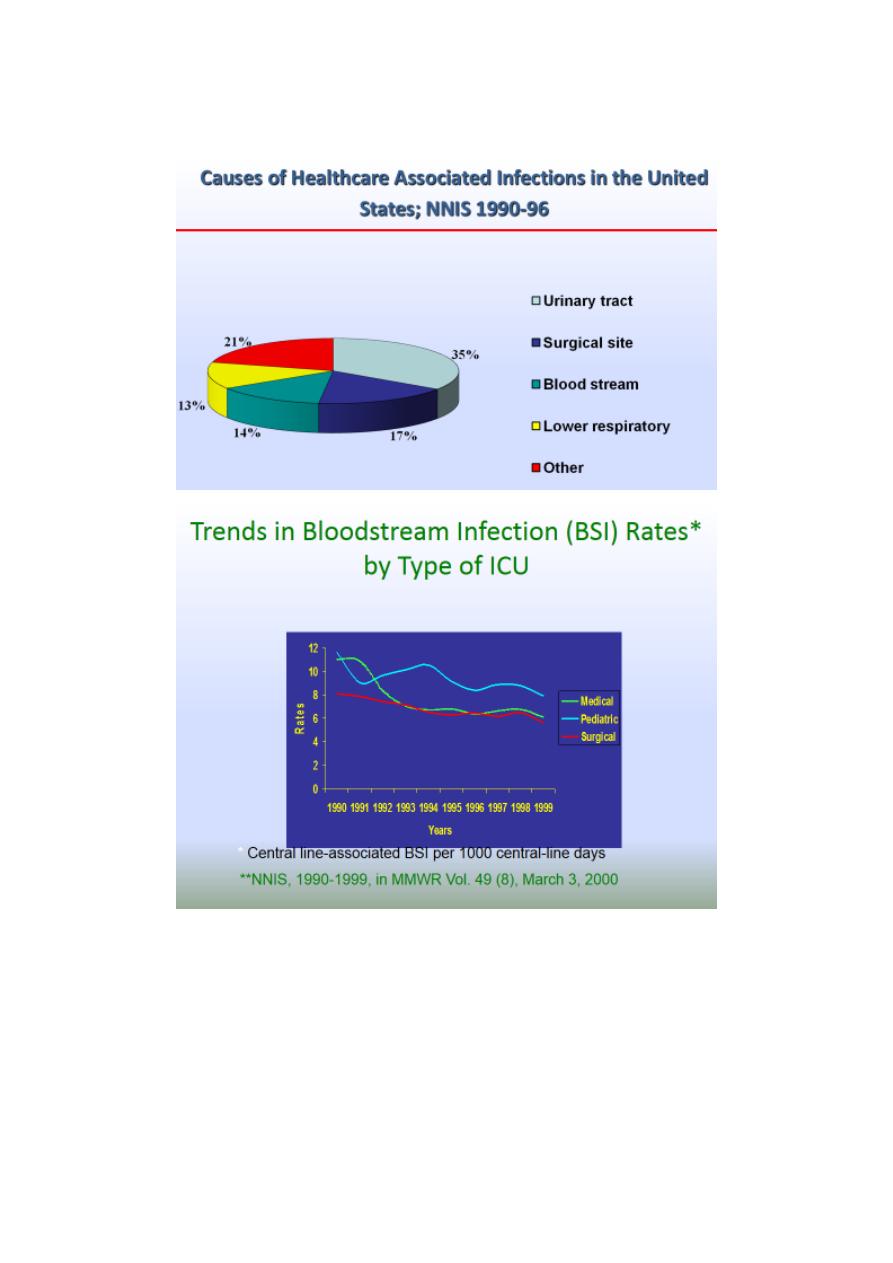
The National Nosocomial Infections Surveillance (NNIS) system in the
United States:
Begun in 1970 with 62 hospitals now >300 hospitals in 42 states
-
mandatory reporting
Focus
-
Initial, hospital-wide infection surveillance
-
Now, infections critical care and surgery
7
Current participants
hospitals with at least 100 occupied beds
inpatients only
Burden of Healthcare-associated Infections
• Europe 7.7
• Western Pacific 9
• South-East-Asia 10
• EMR 11.8
• Total 8.7%
WHO prevalence survey of 55 hospitals in 14 countries

8
Evidence that Nosocomial Infections are an Important Health Problems in
Middle East:
Z Sepsis is a leading cause of death in ICU patients
Z HIV transmission reported due to poor infection control practices
Z Many studies suggest HCB transmission is related to poor infection control practices
and unsafe injections
Importance of IC program in JordanWhy do we need IC in Jordan?
Drug use in outpatient settings
o High antibiotic use (every 3
rd
patient )
o High frequency of injections prescribed ( every 5
th
patient )
Health Care Worker Survey
• Lack of training on infection control
• Low Hepatitis B vaccination coverage
High frequency of needle stick and sharp injuries (41 per 100 HCW per year )
What is Infection Control all About? Importance of IC programs?
1. Reducing patient morbidity and mortality
2. Reducing health care costs
3. Improving the quality of health care services and patient safety
4. Required for hospital accreditation
5. Based on risk assessment and risk management
Infection Control Standard Precautions:
1) Hand hygiene
2) equipment (PPersonal protective PE)
3) Aseptic techniques
4) Reprocessing of instruments/ Sterile services
5) Aseptic techniques
6) Environmental cleaning
7) Proper sharps and waste disposal
8) Occupational safety
9) Environmental cleaning
10) Integrated Public Health Train
9
Infection Control in Special Care Settings:
1. Dentistry
2. Dialysis
3. Intensive Care
4. Operating Room
5. Obstetrics
6. Neonatal Care Unit
7. Endoscopy
8. Pre-hospital care and transport
9. Laboratory safety
