DyslipidemiaPHCL 442
Hadeel Al-KofideTopics to be covered today
Lipid metabolismWhat is dyslipidemia?
Classification of dyslipidemia
Secondary causes of lipoprotein abnormalities
Rationale for treating dyslipidemia
Diagnosis
Risk assessment
Setting your Goals
Treatment modalities
• Therapeutic life style changes
• Drug therapy
Summary of the effect of drugs on lipid profile
Which agent to use for which patient?
Patient counseling
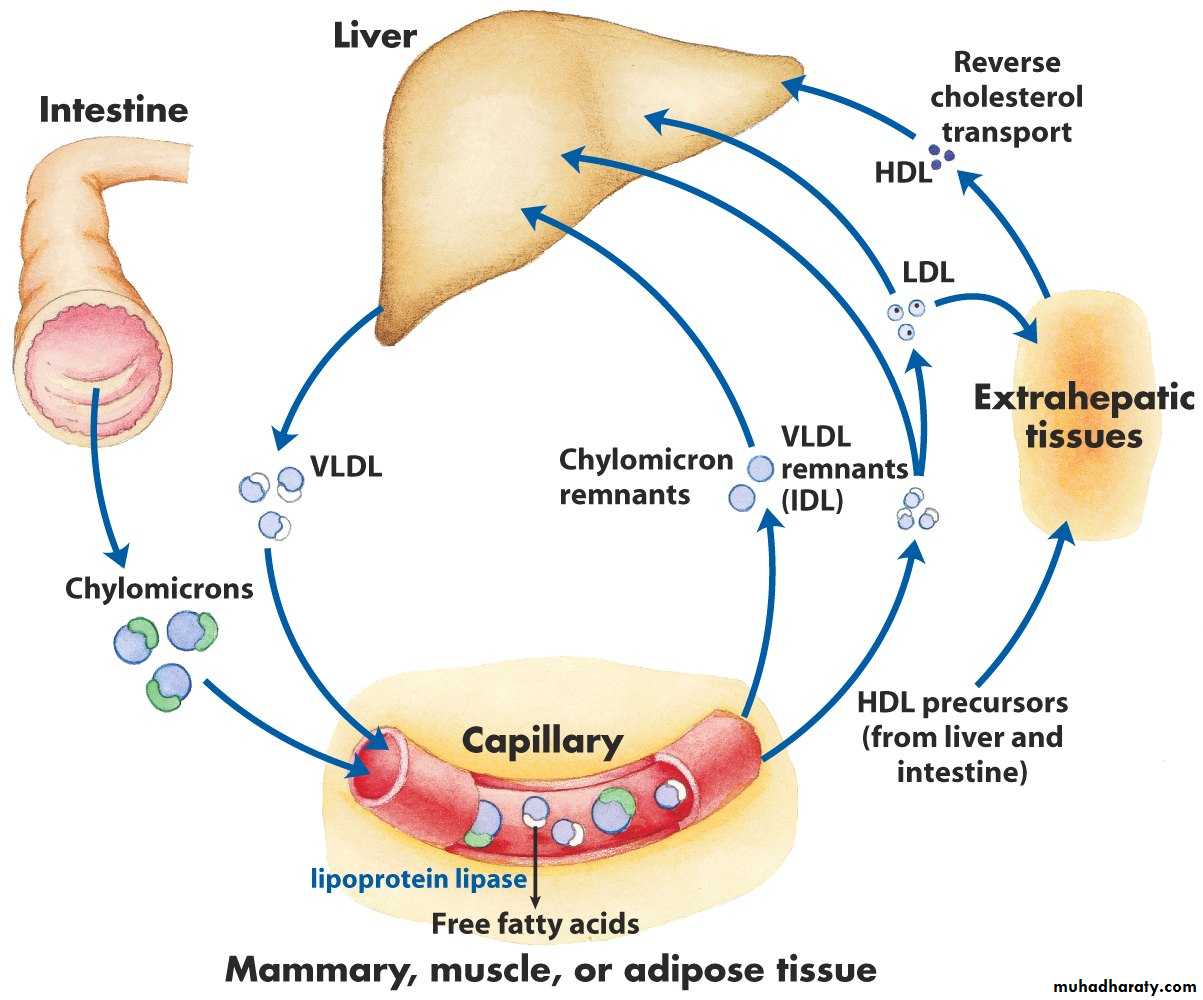
Lipid Metabolism
Cholesterol synthesis
Lipoproteins:
VLDL
LDL
HDL
Chylomicrons
Apolipoproteins
LDL receptor
What is Dyslipidemia?
Dyslipidemias are disorders of lipoprotein metabolismIncluding lipoprotein overproduction & deficiency
They may manifest as one or more of the following: Elevated total cholesterol, low-density lipoprotein cholesterol (LDL), & triglyceride levels or as decreased high-density lipoprotein cholesterol (HDL) level
Classification of Dyslipidemia
Fredrickson ClassificationType
Elevated particles
Associated clinical disorders
Serum TC
Serum TG
I
Chylomicrons
Lipoprotein lipase deficiency, apolipoprotein C-II deficiency
↔
↑↑
IIa
LDL
Familial hypercholesterolemia, polygenic hypercholeterolemia, nephrosis, hypothyroidism, familial combined hyperlipidemia
↑↑
• ↔
IIb
LDL, VLDL
Familial combined hyperlipidemia
↑↑
↑
Fredrickson Classification
TypeElevated particles
Associated clinical disorders
Serum TC
Serum TG
III
IDL
Dysbetalipoproteinemia
↑
↑
IV
VLDL
Familial hypertriglyceridemia, familial combined hyperlipidemia, sporadic hypertriglyceridemia, diabetes
↔↑
• ↑↑
V
Chylomicrons, VLDL
Diabetes
↑
↑↑
Secondary Causes of Lipoprotein Abnormalities
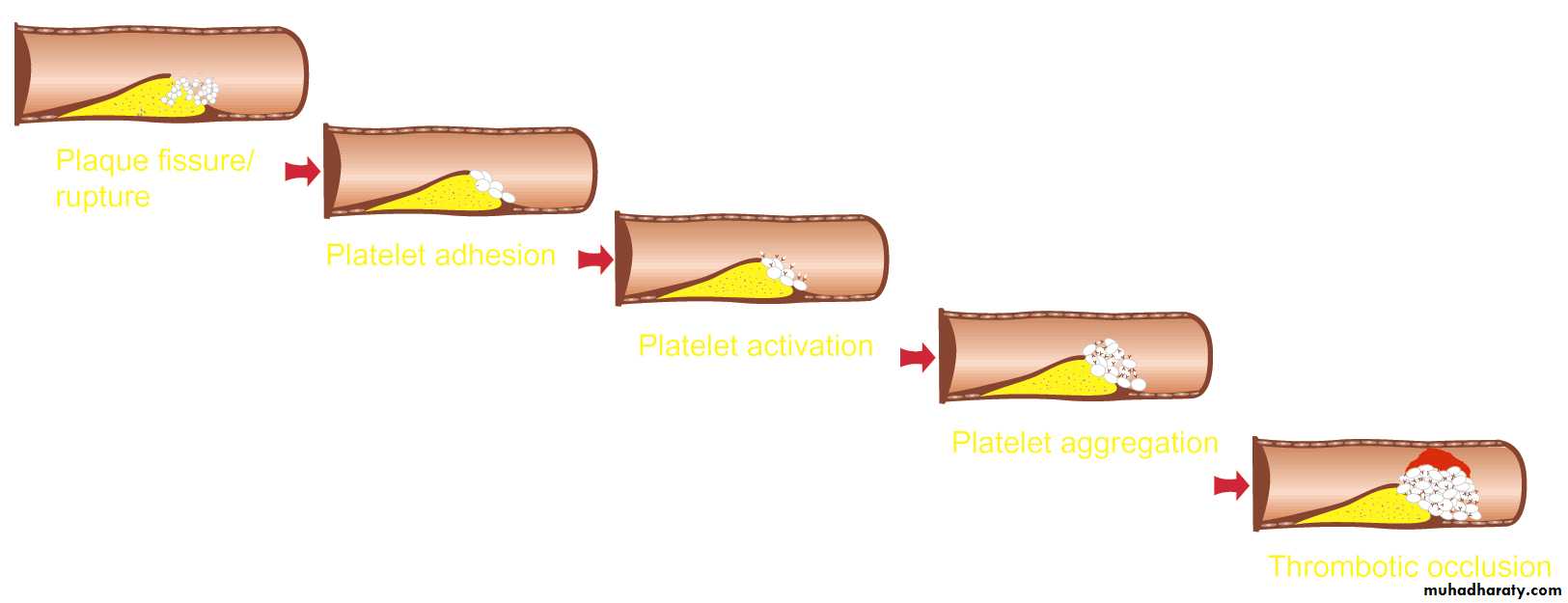
Rationale for Treating DyslipidemiaPathogenesis of atherosclerosis
Epidemiological studies
Clinical trials
LDL cholesterol as a primary target of therapy
Pathogenesis of Atherosclerosis
Rationale for Treating DyslipidemiaEpidemiological Studies
For every 1% increase in cholesterol level there is 1-2% increase in the incidence of CHD
There is a gender difference in relation to age: male at higher risk in 50-60s while female in 60s-70s
CHD cause death in female more than all cancer combined
Rationale for Treating Dyslipidemia
Clinical Trials
TrialIntervention
Initial LDL
Change in LDL
CHD event reduction
CHD & CHD risk equivalent
4S
Simvastatin
188-117
↓ 35%
↓ 34%
LIPID
Pravastatin
150-112
↓ 25%
↓ 24%
CARE
Pravastatin
139-98
↓ 32%
↓ 24%
Post-CABG
Lovastatin/Resin
136-98
↓ 39%
↓ 24%
Rationale for Treating Dyslipidemia
Clinical Trials
Trial
Intervention
Initial LDL
Change in LDL
CHD event reduction
Acute coronary syndrome patients
MIRACL
Atorvastatin124-72
↓ 42%
↓ 26%
AVERT
• Atorvastatin
145-77
↓ 42%
↓ 36%
Rationale for Treating Dyslipidemia
Clinical Trials
TrialIntervention
Initial LDL
Change in LDL
CHD event reduction
Patients without evidence of CHD
LRC-CPPT
Resin
205-175
↓ 15%
↓ 19%
WOSCOPS
Pravastatin
192-142
↓ 26%
↓ 31%
Tex/AFCAPS
Lovastatin
150-115
↓ 25%
↓ 40%
ASCOT
Atorvastatin
132-85
↓ 31%
↓ 50%
Rationale for Treating Dyslipidemia
LDL as a Primary Target of Therapy
Epidemiological studies supported that the increase in LDL is associated with increase in CHD
Studies showed that it is the most abundant & clearly evident atherogenic lipoprotein
The ultimate proof was in in clinical trials
Rationale for Treating Dyslipidemia
Diagnosis
Classification of Lipid LevelsTotal cholesterol mg/dl
LDL cholesterol mg/dl
< 200Desirable
< 100
Optimal
200-239
Border line high
100-129
Near optima/Above optimal
≥ 240
High
130-159
Borderline high
160-189
High
≥ 190
Very highNCEP ATP III Classification of Blood Lipids
Diagnosis
Classification of Lipid Levels
Triglycerides mg/dlHDL cholesterol mg/dl
< 150Normal
< 40
Low
150-199
Border line high
200-400
High• ≥ 60
• High
• ≥ 500
Very high
NCEP ATP III Classification of Blood Lipids
Diagnosis
How to Calculate LDL Cholesterol?
HDL & TGs are measured directly in the labLDL can be calculated using a specific equation
If TG is > 400 mg/dl then this formula is not accurate & LDL must be measured directly in the lab
LDL-C = Total Cholesterol – (HDL-C + TG/5)
Diagnosis
Risk Assessment
Non Lipid Risk Factors for CHDModifiable Risk Factors
Non Modifiable Risk Factors
Hypertension
Age
Cigarette smoking
Male
Thrombogenic/ hemostatic state
Family history of premature CHD
Diabetes
Obesity
Physical inactivity
Atherogenic DietRisk Assessment
How to Assess Risk?Why is it important?
The decision on how aggressive to treat depends on the assessment of global CHD risk
How?
Risk Assessment
How to Assess Risk?
• Assess risk factors:• CHD or CHD risk equivalent (regardless of number of risk factors) using NCEP ATP III definition of CHD & CHD risk equivalent
• ≥ 2 risk factors with no CHD & no CHD risk equivalent using NECP ATP III major risk factors that modify LDL goals
• If ≥ 2 risk factors & no CHD or CHD risk equivalent:
• Assess global CHD risk by Framingham Point Score
Risk Assessment
CHD & CHD Risk Equivalent
Clinical CHD
Carotid artery disease
Peripheral arterial disease
• Abnormal aortic aneurysm
DM
Myocardial ischemia (angina)
Stroke history
Claudication
Present
Present
Myocardial infarction
Transient ischemic attack history
ABI > 0.9
Coronary angiography &/or stent replacement
Carotid stenosis > 50%CABG
Prior unstable anginaAny of these present?
Yes -------------------------------------------- CHD or CHD risk equivalent
No ----- See if the patient has major risk factors that modify LDL goals
NCEP ATP III Definition of CHD & CHD Risk Equivalent
Risk Assessment
Major Risk Factors That Modify LDL Goals
Positive risk factors (↑ risk)Negative risk factors (↓ risk)
Age: Male ≥ 45 yr
Female ≥ 55 yr
High HDL (≥ 60 mg/dl)
Family history of premature CHD (definite MI or sudden death before 55 yr in father or other male first degree relative OR before 65 yr in mother or other female relative)
Current cigarette smoking
Hypertension (≥ 140/90 mm Hg or on antihypertensive drugs)Low HDL (< 40 mg/dl)
NCEP ATP III Major Risk Factors That Modify LDL GoalsCheck if your patient has ≥ 2 risk factors
Risk Assessment
Framingham Point Score
When to use it?
If the patient has CHD or CHD risk equivalent
≥ 2 risk factors & no CHD or CHD risk equivalent
< 2 risk factorsNO
Yes
NO
Risk Assessment
Framingham Point Score
It defines the 10 year risk of developing CHDFramingham Point Score Male
Framingham Point Score Female
Risk Assessment
So… How to Assess?!
Your patient must fall in one of 3 categories:If the patient has CHD or CHD risk equivalent
≥ 2 risk factors & no CHD or CHD risk equivalent
< 2 risk factors
No need to use Framingham score because these patients already have ≥ 20% risk of CHD in 10 years without any calculation
Use to Framingham score to assess their 10 year risk
No need to use Framingham score because they already have low risk for CHD
Risk Assessment
Now Chose your Goals of Therapy
LDL Goals & Cut Points for TLC & Drug TherapyRisk Category
LDL Goal
LDL at which to initiate TLC
LDL at which to consider drug therapy
CHD or CHD risk equivalent
(10 yr risk > 20%)
< 100
≥ 100
≥ 130 (100-129, drug is optional)
≥ 2 risk factors
(10 yr risk ≤ 20%)
< 130
≥ 130
With 10 yr risk 10-20% ≥ 130
With 10 yr risk ≤ 10% ≥ 160
< 2 risk factors
< 160
≥ 160
190 (160-189, drug therapy is optional)
TLC = Therapeutic Life Style Changes
Treatment Modalities
Treatment Modalities
Therapeutic Life Style ChangesNutrient
Recommended intake
Total fat
25-35% of total calories
Saturated fate
< 7% of total calories
Polyunsaturated fat
Up to 10% of total calories
Monounsaturated fat
Up to 20% of total calories
Carbohydrates
50-60% of total calories
Fiber
20-30 g/day
Cholesterol
< 200 mg/day
Protein
15% of total calories
Therapeutic Life Style Changes
When restricting saturated fat by < 10% of calories blood cholesterol reduces by 3-14%
Response to diet is variable
Patients who adhere to a low fat diet also response to a lower doses of lipid-lowering drugs
Therapeutic Life Style Changes
Other life style changes include:Weight reduction specially in overweight patients (reduce 10% in the first 6 months)
Increase physical activity
Smoking cessation
Drug Therapy for Dyslipidemia
Bile acid resinsEzetimibe
Niacin
Statins
Fibric acid derivatives
Fish oil
Postmenopausal drug therapy
Bile Acid Resins
Bile acid sequestrants: cholestyramine, colestipol, colesevelamAvailable as powder & tablet
Reduces LDL by 15-18%
Advantage: a strong safety record (not absorbed from GI so lack of systemic toxicity)
Disadvantages: unpleasant granulated texture of powder old resins
New resins (colesvelam) less GI side effects, present as tablet but large
Drug Therapy
Bile Acid Resins
Mechanism of action:
They bind bile acids in the intestine through anion exchange; this reduces the enterohepatic recirculation of bile acids, which releases feedback regulation on conversion of cholesterol to bile acids in the liver
The resulting decrease in hepatocyte cholesterol content enhances LDL-receptor expression, which in turn lowers serum LDL-cholesterol concentrations
Drug Therapy
Bile Acid Resins
Adverse effects:GI: constipation, bloating, epigastric fullness, nausea & flatulence (specially with old ones)
Increase TGs (old resins)
To overcome GI s.e: mix resin powder in noncarbonated pulpy juice, swallow it without engulfing air (use straw) & maintain adequate intake of fluid & fiber in diet
Drug Therapy
Bile Acid Resins
Drug interactions:GI binding can reduce absorption of anionic drugs (warfarin, thyroxin, digitoxin, beta-blockers & thiazide diuretics)
Can reduce this drug interactions by administration 1 hour before or 4 hours after the resin
Colesevelam have higher specificity to binding to bile acid so less drug interactions
Drug Therapy
Ezetimibe
Cholesterol absorption inhibitorNew agent, came to the market at 2003
It reduces LDL by 18-22%
Little effect on TG or HDL
LDL effect enhanced when adding a statin by 10-20%
It has the advantage of minimum systemic absorption
Drug Therapy
Ezetimibe
Mechanism of action:
It interferes with the active absorption of cholesterol from the intestininal lumen into the enterocyte
About 50% less cholesterol is transported from intestine to the liver, leading to reduction in hepatic cholesterol stores & increase in the clearance of cholesterol from the blood
Drug Therapy
Ezetimibe
Adverse effects:Diahhrea, arthralgia, cough & fatigue
Drug Therapy
Niacin
Water soluble B vitamin that improves all lipidsHas been used for a long time
Comes in 3 forms:
• Immediate release crystalline form: Causes flushing
• Sustained release: less flushing but maximum dose 2 gm to prevent liver toxicity
• Extended release: New drug, Niaspan is extended release formula better than other forms due to less side effects
Drug Therapy
Niacin
Decreases LDL by 15-25%
Decreases TGs by 30-40%
Increases HDL by 20-30%
The strongest in increasing HDL
Also useful in hypertriglyceridemia
Drug Therapy
Niacin
Mechanism of action:Inhibit the mobilization of free fatty acids from peripheral adipose tissue to the liver which reduces synthesis & secretion of VLDL particles by the liver
Because LDL is a product of VLDL degradation reducing VLDL will reduce LDL
Drug Therapy
Niacin
Adverse effects:Flushing & headache: with immediate release, can be reduced by giving aspirin
Increase blood glucose by 10-20%
Hepatotoxicity: sustained release formulation, defined as 3 times the upper limit of liver enzymes & could be associated with symptoms as fatigue, anorexia, malaise & nausea
Niasepam: is the best, less flushing but more GI effects like nausea, dyspepsia & activation of peptic ulcer, can reduce these side effect if given with food. Less hepatic toxicity in doses ≤ 2gm/day
Drug Therapy
Statins
HMG-CoA reductase inhibitorsMost potent cholesterol lowering drugs
6 different agents:
Rosuvastatin
Atorvastatin
Simvastatin
Lovastatin
Pravastatin
Fluvastatin
They are all powerful in decreasing LDL levels but some have greater effect on LDL than others
Drug Therapy
Statins
AgentDose (mg)
LDL lowering (↓)
Atorvastatin
10
39%
20
43%
40
50%
80
60%
Rosuvastatin
10
46%
20
52%
40
55%
5
26%
Simvastatin
10
30%
20
38%
40
41%
80
47%
Drug Therapy
↑ dose
↑ LDL lowering effectStatins
Mechanism of actions:Statins act by inhibiting the enzyme HMG-CoA reductase, the enzyme controlling the first committed step of cholesterol synthesis in the liver
Reducing hepatocellular cholesterol promotes an up-regulation of LDL receptors & increases LDL clearance
They reduce TGs by reducing secretion of VLDL particles & increase clearance of VLDL
Drug Therapy
Statins
Adverse effects:Headache
Myalgias (with no CPK changes)
GI symptoms: dyspepsia, constipations & abdominal pain
These adverse effects reduced with continued therapy
Drug Therapy
Statins
Adverse effects:
Hepatotoxicity:
Increases liver enzymes 3 times the upper normal limit in 1-1.5% of patients in a dose dependent manner
Levels may return to normal whether DC or if still on therapy
Rechallenge, how?
Drug Therapy
Statins
Adverse effects:Muscle toxicity (myositis):
Increases CPK > 10 times upper normal limit with the presence of muscle aches, soreness or weakness (myalgia)
Happens in 0.1-1% of patients in a dose dependent manner
Does not require routine monitoring but if symptoms occur check CPK
Once occur, DC then after symptoms subside start with a different statin
Rarely causes rhabdomyolysis
Drug Therapy
Statins
Drug interactions:With gemfibrozil increase risk of rhabdomyolysis
Increase muscular toxicity with drugs that compete or inhibit CYP450 3A4 system (cyclosporine, erythromycin, calcium blockers, niacin, ketoconazole)
What to do when using these drugs?
Lovastatin & rosuvastatin may prolong bleeding time with warfarin
Drug Therapy
Statins
Contraindications:
Active liver disease
Patient pregnant or planning to get pregnant
Drug Therapy
Fibric Acid Derivatives
Fibrates: gemfibrozil & fenofibrateAgent of choice in hypertriglyceridemia
Decrease TG by 20-50%
Increase HDL by 10-15%
Decreases LDL by 10-25%
In patients with combined hyperlipidemia gemfibrozil may increase LDL, while fenofibrate may not increase but has lower effect in LDL reduction (around 10% only)
Drug Therapy
Fibric Acid Derivatives
Mechanism of action:Increases activity of Peroxisome proliferator-activated receptor-alpha (PPARα), a receptor which is involved in metabolism of carbohydrates & fats, as well as adipose tissue differentiation
This increases synthesis of lipoprotein lipase therefore increasing clearance of triglycerides
Drug Therapy
Fibric Acid Derivatives
Adverse effects:
GI symptoms like nausea, dyspepsia & abdominal pain
Myositis & rhabdomyolysis: more common with gemfibrozil specially combination with statins
Gallstones
Drug Therapy
Fish Oils
It contains polyunsaturated (omega-3) fatty acidsIt lowers TG levels by 30-60%
Little value in LDL reduction
Supplemental fish oils have been demonstrated by clinical trials to reduce CHD events
Most useful in patients with hypertriglyceridemia not adequately controlled by drugs (niacin & fibrates)
Drug Therapy
Postmenopausal Drug Therapy
Postmenopausal women have increased risk of CHDEstrogen is known to improve lipid & liporprotein profile
Due to high incidence of side effects (Thromboembolism, breast cancer) they are not recommended for treatment of dyslipidemia in postmenopausal women
These women are candidate for previous modalities for lowering lipid level
Drug Therapy
Summary of the Effect of Drugs on Lipid Profile
Drug
LDL
HDL
TG
Resin
↓ 15-30%
± 3%
↑ 3-10%
Ezitimibe
↓ 18-22%
↑ 0-2%
↓ 0-5%
Niacin
↓ 15-30%
↑ 20-35%
↓ 30-60%
Statin
↓ 25-60%
↑ 5-15%
↓ 10-45%
Fibrates
± 10-25%
↑ 10-30%
↓ 30-60%
What Agent(s) for What Patient?
Drugs of Choice for Dyslipidemia
Elevated LDL cholesterol value:Drug of choice: Statin
Alternative therapy: Niacin, resins or ezetimibe
Combination: statin + niacin; statin + ezetimibe; or statin + resin
According to clinical trials & guidelines Statins are the most effective treatment for high LDL levels
If patients can not tolerate statins, or used statin but with no effect (rare)
If patients did not achieve goal of LDL with maximum statin dose
Drugs of Choice for Dyslipidemia
Elevated LDL & TG values:Drug of choice: Statin
Combination: statin + niacin; statin + ezetimibe; or statin + resin
It decreases LDL & TG but require higher doses for TG
For many patients with mixed hyperlipidemia can use a moderate dose of statin (to avoid side effects of higher doses) with combination of either niacin, resin, ezetimibe or fibratesDrugs of Choice for Dyslipidemia
Normal LDL value but Low HDL:Drug of choice: Niacin or fibrates
If patient have normal LDL OR patient within LDL goal on statin therapy but still HDL high add niacin or fibrates
Drugs of Choice for Dyslipidemia
Elevated TGs value:Drug of choice: Fibrates & niacin
Can add fish oil
If only TG level is high
Patient Instructions & Counseling
StatinsUsually administered in the evening because most hepatic cholesterol production occurs during the night
Atorvastatin may be given any time of the day because of its longer half-life
You may take this medicine with or without food
Patient Instructions & Counseling
Bile acid resisn:Cholestyramin: take it with the largest meal
Titrate dose slowly to avoid GI side effect
The powder cannot be used in dry form. It can be mixed with water, fruit juice, milk, & with food such as thin soup or with milk in breakfast cereal until completely dissolved. The patient must drink this mixture right away
Counsel patient to rinse the glass with liquid to ensure ingestion of all resin
Increase fluid intake
Dose other drugs 1 hour before or 4 hours after resin
Patient Instructions & Counseling
Fibrates:
Gemfibrozil should be taken twice daily 30 minutes before meals
Fenofibrate can be taken with food once daily
Monitor muscle toxicity, especially when used with statins