
Medicine Lec1
Dr. Bilal
INVESTIGATION OF
RESPIRATORY DISEASE
A detailed history, thorough examination and basic haematological
and biochemical tests usually suggest the likely diagnosis and key
differentials. However, a number of further investigations are usually
required to confirm the diagnosis and/or monitor disease activity.
Imaging
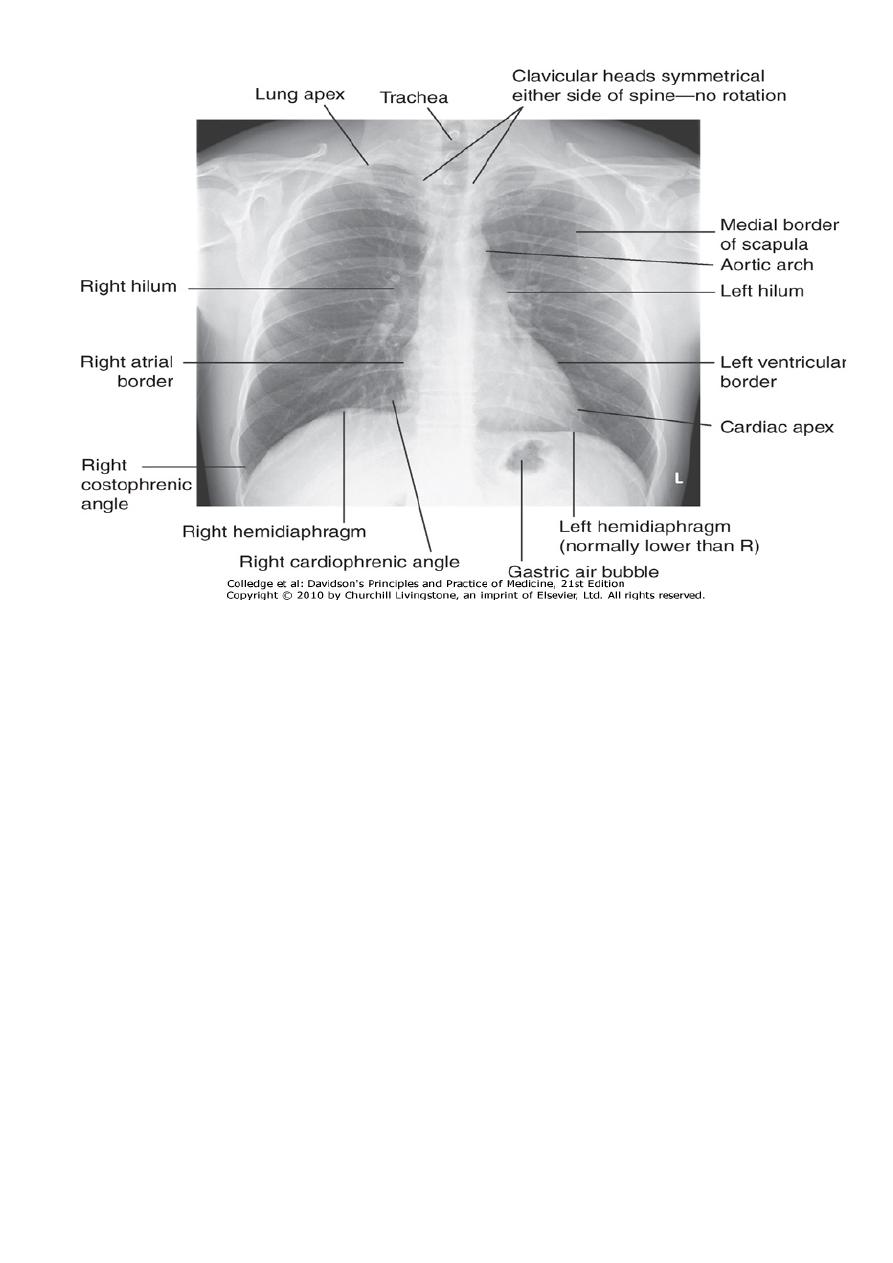
The 'plain' chest X-ray This is performed on the majority of patients
suspected of having chest disease. A postero-anterior (PA) film
provides information on the lung fields, heart, mediastinum, vascular
structures and the thoracic cage .Additional information may be
obtained from a lateral film, particularly if pathology is suspected
behind the heart shadow or deep in the diaphragmatic sulci.
1
Medicine Lec1
Dr. Bilal
Note lung markings consist of branching and tapering lines radiating out from
the hila; where airways and vessels turn towards the film they can appear as
open or filled circles (see upper pole of right hilum). The scapulae may overlie
the lung fields; trace the edge of bony structures to avoid mistaking them for
pleural or pulmonary shadows. To check for hyperinflation, count the ribs; if
more than 10 are visible posteriorly above the diaphragm, the lungs are
hyperinflated.
Upper zone CXR infiltrate favors : TB , Aspergilosis , fibrosis due
to Ankylosing spondylitis.
Lower zone infiltrate: Idiopathic(Cryptogenic) pulmonary
fibrosis ,Asbestosis, Aspiration pneumonia.
Significance of apparently elevated hemidiaphram:
•
Phrenic nerve pulsy
•
Segmental or lobar
collapse or resection
•
Subphrenic collection
•
Massive hepatomegaly
•
Diaphramatic rupt
2
Medicine Lec1
Dr. Bilal
Films are postero-anterior (PA) unless
marked AP to denote antero-posterior
Name, date,
orientation
Equal translucency?
Lung fields
Check horizontal fissure from right hilum to
sixth rib at the anterior axillary line
Masses? Consolidation? Cavitation?
Check behind the clavicles.
Masses? Consolidation? Cavitation?
Lung apices
Central? (Midway between the clavicular
heads). Paratracheal mass? Goitre?
Trachea
Normal shape? Cardiothoracic ratio (should be
< half the intrathoracic diameter)
Heart
Retrocardiac mass?
Left should be higher than right
Hila
Shape? (Should be concave laterally; if
convex, consider mass or lymphadenopathy)
Density?
Right should be higher than left
Diaphragms
Hyperinflation? No more than 10 ribs should
be visible posteriorly above the diaphragm)
Acute and well-defined? (Pleural fluid or
thickening, if not)
Costophrenic
angles
Breast shadows in females
Soft tissues
Chest wall for masses or subcutaneous
emphysema
Ribs, vertebrae, scapulae and clavicles
Bones
Any fracture visible at bone margins or
lucencies?
3

Medicine Lec1
Dr. Bilal
Common chest X-ray abnormalities:-
1.Pulmonary and pleural shadowing
2.Consolidation: infection, infarction, inflammation, and rarely
bronchoalveolar cell carcinoma
3.Lobar collapse: mucus plugging, tumour, compression by lymph
nodes
4.Solitary nodule.Multiple nodules: miliary tuberculosis (TB), dust
inhalation, metastatic malignancy, healed varicella pneumonia,
rheumatoid disease
5.Ring shadows, tramlines and tubular shadows: bronchiectasis
6.Cavitating lesions: tumour(esp.squamous), abscess, infarct,
pneumonia (Staphylococcus/Klebsiella), Wegener's
granulomatosis
7.Reticular, nodular and reticulonodular shadows: diffuse
parenchymal lung disease, infection
8.Pleural abnormalities: fluid, plaques, tumour
9.Increased translucency Bullae
10.Pneumothorax
11.Oligaemia
12.Hilar abnormalities
13.Unilateral hilar enlargement: TB, bronchial carcinoma,
lymphoma
14.Bilateral hilar enlargement: sarcoid, lymphoma, TB, silicosis
15.Other abnormalities Hiatus hernia
16.Surgical emphysema
Increased shadowing may represent accumulation of fluid, lobar collapse
or consolidation. Uncomplicated consolidation should not change the
position of the mediastinum and the presence of an air bronchogram
means that proximal bronchi are patent. Collapse (implying obstruction of
the proximal bronchus) is accompanied by loss of volume and
displacement of the mediastinum towards the affected side .
The presence of ring shadows (diseased bronchi seen end-on), tramline
shadows (diseased bronchi side-on) or tubular shadows (bronchi filled with
4

Medicine Lec1
Dr. Bilal
secretions) suggests bronchiectasis. The presence of pleural fluid is
suggested by a dense basal shadow which, in the erect patient, ascends
towards the axilla. In large pulmonary embolism, relative oligaemia may
cause a lung field to appear abnormally dark.
Computed tomography (CT)
CT provides detailed images of the pulmonary parenchyma,
mediastinum, pleura and bony structures. The displayed range of
densities can be adjusted to highlight different structures such as the
lung parenchyma, the mediastinal vascular structures or bone.
Sophisticated software facilitates three-dimensional reconstruction of
the thorax and virtual bronchoscopy.
CT is superior to chest radiography in determining the position and
size of a pulmonary lesion and whether calcification or cavitation is
present. It is now routinely used in the assessment of patients with
suspected lung cancer and facilitates guided percutaneous needle
biopsy. Information on tumour stage may be gained by examining the
mediastinum, liver and adrenal glands.
CT provides better assessment of the mediastinum and hilar LN,&
section as small as 1mm can be obtained.
High-resolution CT (HRCT) uses thin sections to provide detailed
images of the pulmonary parenchyma and is particularly useful in
assessing diffuse parenchymal lung disease, identifying bronchiectasis
, and it is the best technique to diagnose and follow the type and
extent of emphysema and COPD.
CT pulmonary angiography (CTPA) is used increasingly in the diagnosis
of pulmonary thromboembolism , when it may either confirm the
suspected embolism or highlight an alternative diagnosis.
5

Medicine Lec1
Dr. Bilal
Ultrasound
Ultrasound is sensitive at detecting pleural fluid and may also be
employed to direct and improve the diagnostic yield from pleural
biopsy. It is also used to investigate the anatomy of an empyema
cavity to facilitate directed drainage, and to guide needle biopsy of
superficial lymph node or chest wall masses. Endobronchial
ultrasound is now possible using specialised bronchoscopes, and is
used for imaging and sampling peribronchial lymph nodes.
Positron emission tomography (PET)
PET scanners exploit the avid ability of malignant tissue to absorb
and metabolise glucose. The radiotracer
18
F-fluorodeoxyglucose (FDG)
is administered and rapidly taken up by malignant tissue.
It is then phosphorylated but cannot be metabolised further,
becoming 'trapped' in the cell. PET is useful in the investigation of
pulmonary nodules, and in staging mediastinal lymph nodes and distal
metastatic disease in patients with lung cancer. The negative
predictive value is high; however, the positive predictive value is
poor. Co-registration of PET and CT (PET-CT) enhances localisation
and characterisation of metabolically active deposits
6

Medicine Lec1
Dr. Bilal
CT and positron emission
tomography (PET) combined to
reveal intrathoracic metastases.
A- In a patient with lung cancer, CT
shows some posterior pleural
thickening.
B-PET scanning
reveals FDG uptake in two pleural
lesions (arrows),
C-highlighted in yellow in the
combined PET/CT image .
Ventilation-perfusion imaging
In this technique, the lungs are imaged using a gamma camera that is
able to distinguish two isotopes, inhaled
133
Xe (yielding ventilation
images) and injected macroaggregates of
99m
Tc-albumin (yielding
perfusion images). Pulmonary emboli appear as perfusion defects
with preserved ventilation. However, the utility of this technique is
limited in patients with underlying lung disease, in whom up to 70%
of scans may be indeterminate. It is increasingly being replaced by
CTPA.
7

Medicine Lec1
Dr. Bilal
Pulmonary angiography
Images taken with contrast medium in the main pulmonary artery are
rarely used, particularly now that CTPA is widely available. Right
heart catheterisation remains useful in the investigation of patients
with pulmonary hypertension, providing information on pulmonary
and right heart pressures.
Endoscopic examination
Laryngoscopy
The larynx may be inspected indirectly with a mirror or directly with
a laryngoscope. Fibreoptic instruments allow a magnified view to be
obtained.
Bronchoscopy
The trachea and larger bronchi may be inspected using either a
flexible or a rigid bronchoscope. Flexible bronchoscopy may be
performed under local anaesthesia with sedation on an outpatient
basis. Structural changes, such as distortion or obstruction, can be
seen. Abnormal tissue in the bronchial lumen or wall can be biopsied,
and bronchial brushings, washings or aspirates can be taken for
cytological or bacteriological examination.
Small biopsy specimens of lung tissue, taken by forceps passed
through the bronchial wall (transbronchial biopsies), may reveal
sarcoid granulomas or malignant diseases and may be helpful in
diagnosing certain bronchocentric disorders (e.g. hypersensitivity
pneumonitis, cryptogenic organising pneumonia), but are generally
too small to be of diagnostic value in other diffuse parenchymal
pulmonary disease .
Transbronchial needle aspiration (TBNA) may be used to sample
mediastinal lymph nodes and in the staging of lung cancer.
8
Medicine Lec1
Dr. Bilal
Rigid bronchoscopy requires general anaesthesia and is reserved for
specific situations such as massive haemoptysis or removal of foreign
bodies. Endobronchial laser therapy and endobronchial stenting may
be performed more easily with rigid bronchoscopy.
Assessment of the mediastinum
Lymph nodes down to the main carina can be sampled using a
mediastinoscope passed through a small incision at the suprasternal
notch under general anaesthetic. This procedure is particularly useful
in lung cancer as a means of determining whether nodal disease is
present. Endobronchial ultrasound (EBUS) using a specialised
bronchoscope allows directed needle aspiration from peribronchial
nodes but is not yet widely available. Lymph nodes in the lower
mediastinum may be biopsied via the oesophagus using endoscopic
ultrasound (EUS), an oesophageal endoscope equipped with an
ultrasound transducer and biopsy needle.
Investigation of pleural disease
The traditional method of pleural biopsy using an Abram's needle is
largely being replaced by the use of core biopsy guided by either
ultrasound or CT. Thoracoscopy, which involves the insertion of an
endoscope through the chest wall, facilitates biopsy under direct
vision and is practised by many surgeons and an increasing number of
physicians.
Skin tests
The tuberculin test may be of value in the diagnosis of tuberculosis.
Skin hypersensitivity tests are useful in the investigation of allergic
diseases.
9

Medicine Lec1
Dr. Bilal
Immunological and serological tests
The presence of pneumococcal antigen (
revealed by counter-
immunoelectrophoresis
) in sputum, blood or urine may be of diagnostic
importance in pneumonia. Exfoliated cells colonised by influenza A virus
can be detected by fluorescent antibody techniques. In blood, high or
rising antibody titres to specific organisms (such as Legionella,
Mycoplasma, Chlamydia or viruses) may eventually clinch a diagnosis
suspected on clinical grounds. Precipitating antibodies may be found as a
reaction to fungi such as Aspergillus or to antigens involved in
hypersensitivity pneumonitis .
Microbiological investigations
Sputum, pleural fluid, throat swabs, blood and bronchial washings
and aspirates can be examined for bacteria, fungi and viruses. In
some cases, as when Mycobacterium tuberculosis is isolated, the
information is diagnostically conclusive, but in others the findings
must be interpreted in conjunction with the results of clinical and
radiological examination.
Induced sputum
The use of hypertonic saline to induce expectoration of sputum is
useful in facilitating the collection of specimens for microbiology,
particularly in patients in whom more invasive procedures such as
bronchoscopy are not possible. The technique also allows assessment
of the inflammatory cell constituency of the airway, which is a useful
research tool in many conditions including asthma, COPD and
interstitial lung disease.
Histopathological and cytological examination
Histopathological examination of biopsy material obtained from
pleura, lymph node or lung often allows a 'tissue diagnosis' to be
made. This is of particular importance in suspected malignancy or in
elucidating the pathological changes in interstitial lung disease.
Important causative organisms, such as M. tuberculosis, Pneumocystis
jirovecii or fungi, may be identified in bronchial washings, brushings
or transbronchial biopsies. Cytological examination of exfoliated cells
10

Medicine Lec1
Dr. Bilal
in sputum, pleural fluid or bronchial brushings and washings, or of
fine needle aspirates from lymph nodes or pulmonary lesions can
support a diagnosis of malignancy, but if this is indeterminate a tissue
biopsy is necessary. Cellular patterns in bronchial lavage fluid may
help to distinguish pulmonary changes due to sarcoidosis from those
caused by idiopathic pulmonary fibrosis or hypersensitivity
pneumonitis.
Pulmonary Function Test
Pulmonary Function Testing has been a major step forward in
assessing the functional status of the lungs as it relates to :
•
How much air volume can be moved in and out of the lungs
•
How fast the air in the lungs can be moved in and out
•
How stiff are the lungs and chest wall - a question about
compliance
•
The diffusion characteristics of the membrane through which the
gas moves (determined by special tests)
•
How the lungs respond to chest physical therapy procedures
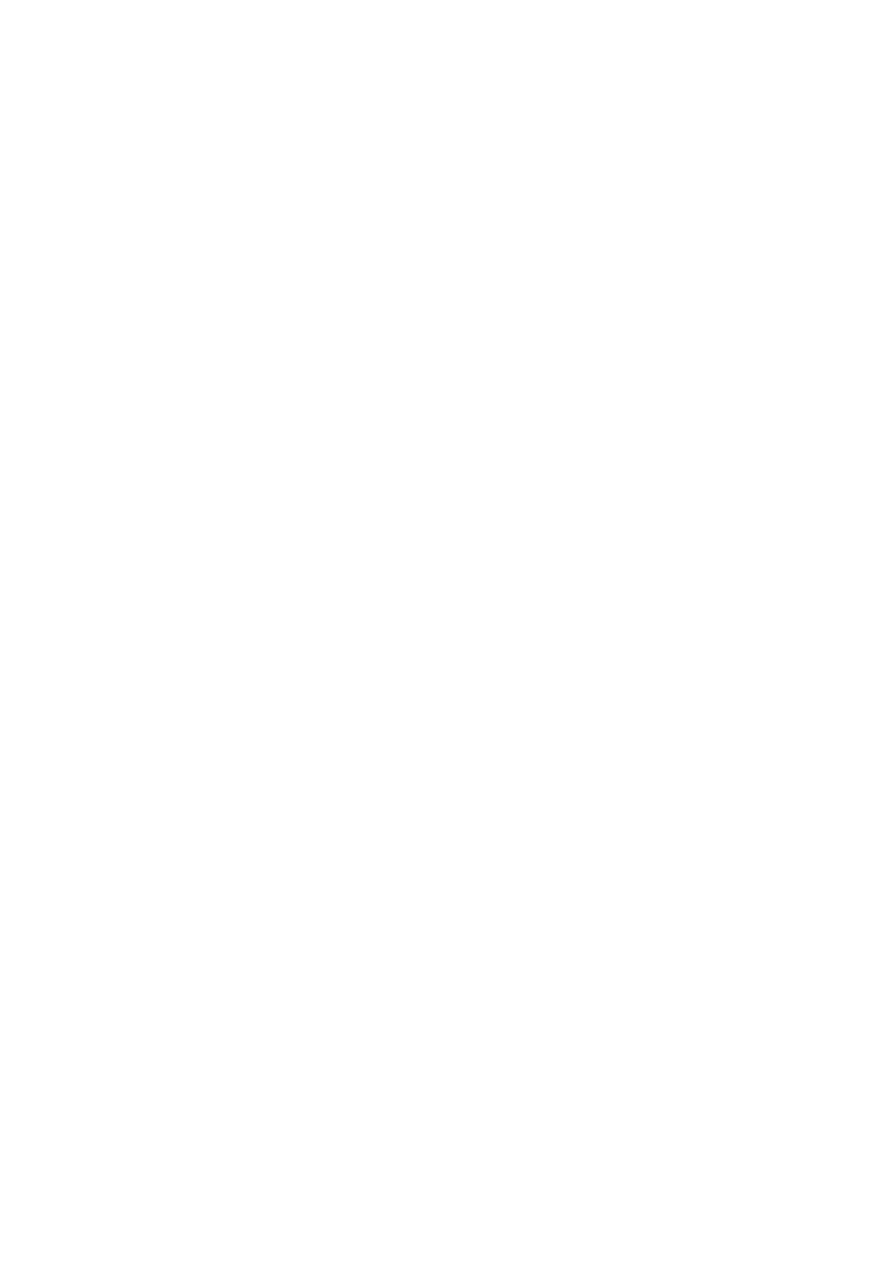
RESPIRATORY FUNCTION TESTING
Respiratory function tests are used to aid diagnosis, assess functional
impairment and monitor treatment or progression of disease.
11
Medicine Lec1
Dr. Bilal
12

Medicine Lec1
Dr. Bilal
ABBREVIATIONS USED IN RESPIRATORY FUNCTION TESTING
Terminology and Definitions
FVC - Forced Vital Capacity - after the patient has taken in the
deepest possible breath, this is the volume of air which can be
forcibly and maximally exhaled out of the lungs until no more can be
expired. FVC is usually expressed in units called liters. This PFT value
is critically important in the diagnosis of obstructive and restrictive
diseases.
FEV1 - Forced Expiratory Volume in One Second - this is the volume
of air which can be forcibly exhaled from the lungs in the first second
of a forced expiratory manuever. It is expressed as liters. This PFT
Stands for
Abbreviatio
n
Forced expiratory volume in 1 second
FEV
1
Forced vital capacity
FVC
Vital capacity (relaxed)
VC
Peak (maximum) expiratory flow
PEF
Total lung capacity
TLC
Functional residual capacity
FRC
Residual volume
RV
Gas transfer factor for carbon
monoxide
TL
CO
Gas transfer per unit lung volume
K
CO
13

Medicine Lec1
Dr. Bilal
value is critically important in the diagnosis of obstructive and
restrictive diseases.
FEV1/FVC - FEV1 Percent (FEV1%) - This number is the ratio of FEV1
to FVC - it indicates what percentage of the total FVC was expelled
from the lungs during the first second of forced exhalation - this
number is called FEV1%, %FEV1 or FEV1/FVC ratio. This PFT value is
critically important in the diagnosis of obstructive and restrictive
diseases.
PEFR - Peak Expiratory Flow Rate - this is maximum flow rate
achieved by the patient during the forced vital capacity maneuver
beginning after full inspiration and starting and ending with maximal
expiration - it can either be measured in L/sec or L/min - this is a
useful measure to see if the treatment is improving obstructive
diseases like bronchoconstriction secondary to asthma.
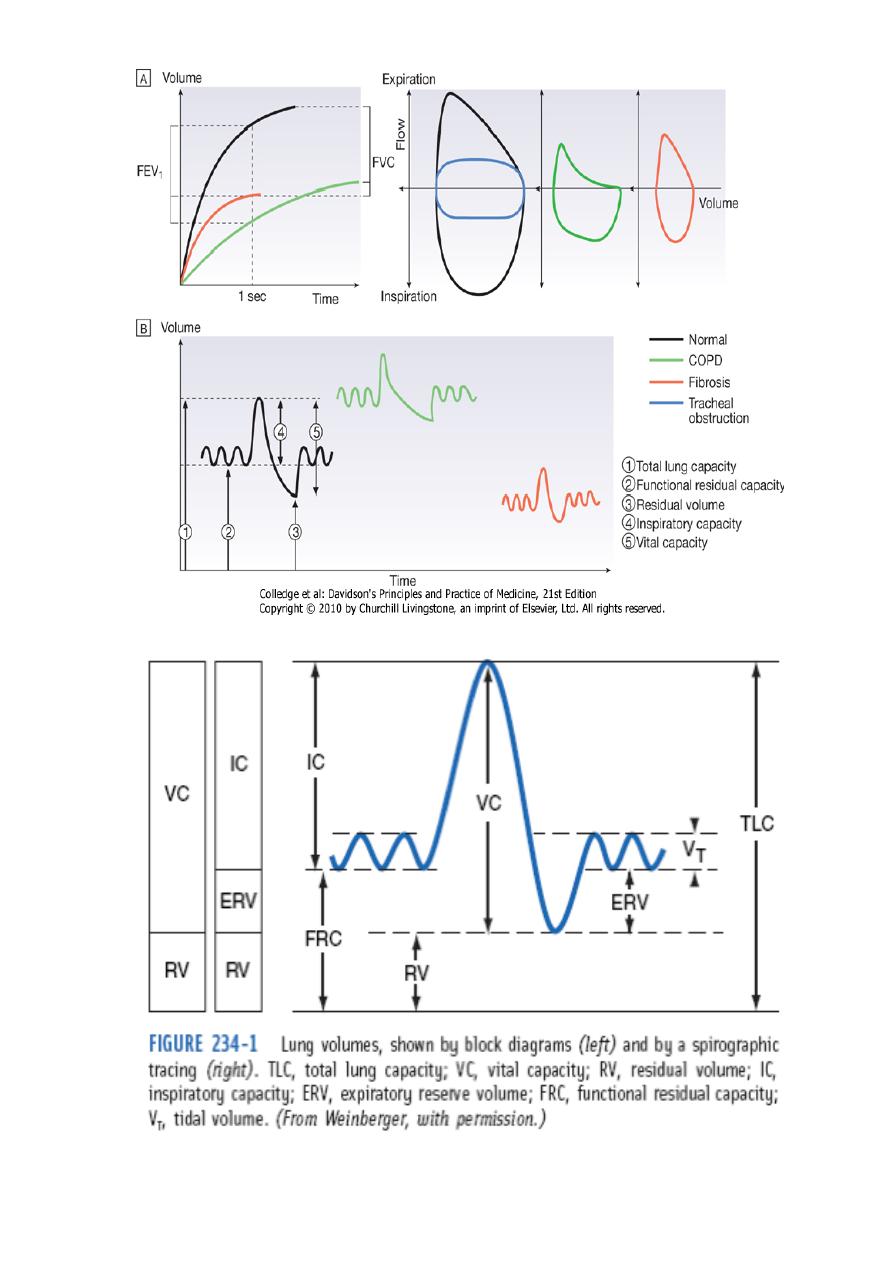
Total lung capacity (TLC). This measures the amount of air in your
lungs after you inhale as deeply as possible.
Functional residual capacity (FRC). This measures the amount of air
in your lungs at the end of a normal exhaled breath.
Residual volume (RV). This measures the amount of air in your lungs
after you have exhaled completely. It can be done by breathing in
helium or nitrogen gas and seeing how much is exhaled.
Vital capacity (VC). This is the total volume of air that can be
exhaled after maximum inspiration.
Inspiratory capacity: The volume of air that can be inhaled after
normal inspiration.
14

Medicine Lec1
Dr. Bilal
Lung volumes
Tidal volume and vital capacity (VC) can be measured by spirometry.
Total lung capacity (TLC) can be measured by asking the patient to
rebreathe an inert non-absorbed gas (usually helium) and recording
the dilution of test gas by lung gas. This measures the volume of
intrathoracic gas which mixes quickly with tidal breaths.
Alternatively, lung volume may be measured by body
plethysmography, which determines the pressure/volume relationship
of the thorax. This method measures total intrathoracic gas volume,
including poorly ventilated areas such as bullae.
In diseases characterised by airway narrowing (e.g. asthma,
bronchitis and emphysema) maximum expiratory flow is limited by
dynamic compression of small intrathoracic airways, some of which
close completely during expiration, limiting the volume which can be
expired.
Hyperinflation of the chest results, and can become extreme if
elastic recoil is also lost due to parenchymal destruction, as in
emphysema.
In contrast, diseases which cause lung inflammation and/or scarring
and fibrosis are characterised by progressive loss of lung volume with
normal expiratory flow rates.
Gas exchange is impaired by both parenchymal destruction
(emphysema) and by interstitial disease, which disrupts the local
matching of ventilation and perfusion.
In respiratory function testing, airway narrowing, lung volume and
gas exchange capacity are quantified and compared with normal
values adjusted for age, gender, height and ethnic origin.
15

Medicine Lec1
Dr. Bilal
Airway narrowing is assessed by forced expiration into a peak flow
meter or a spirometer. Peak flow meters are cheap and convenient
for home monitoring (e.g. detection and monitoring of asthma) but
values are effort-dependent.
The forced expiratory volume in 1 second (FEV1) and vital capacity
(VC) are obtained from maximal forced and relaxed expirations into a
spirometer.
FEV1 is disproportionately reduced in airflow obstruction resulting
in FEV1/VC ratios of less than 70%.
When airflow obstruction is seen, spirometry should be repeated
following inhaled short-acting β2-adrenoceptor agonists (e.g.
salbutamol); reversibility to normal is suggestive of asthma .
Flow/volume loops
To distinguish large airway narrowing (e.g. tracheal stenosis or
compression) from small airway narrowing, flow/volume loops are
recorded using spirometry.
These display flow as it relates to lung volume (rather than time)
during maximum expiration and inspiration, and the pattern of
flow reveals the site of airflow obstruction .
Transfer factor
To measure the capacity of the lungs to exchange gas, patients inhale
a test mixture of 0.3% carbon monoxide, which is avidly bound to
haemoglobin in pulmonary capillaries. After a short breath-hold, the
rate of disappearance of CO into the circulation is calculated from a
sample of expirate, and expressed as the TL
CO
or carbon monoxide
transfer factor. Helium is also included in the test breath to allow
calculation of the volume of lung examined by the test breath.
Transfer factor expressed per unit lung volume is termed K
CO
16
Medicine Lec1
Dr. Bilal
How to interpret respiratory function abnormalities
Arterial blood gases and oximetry
The measurement of hydrogen ion concentration, PaO
2
and PaCO
2
,
and derived bicarbonate concentration in an arterial blood sample is
essential in assessing the degree and type of respiratory failure and
for measuring acid-base status. Interpretation of results is made
easier by blood gas diagrams, which indicate whether any acidosis or
alkalosis is due to acute or chronic respiratory derangements of
PaCO
2
, or to metabolic causes.
Pulse oximeters with finge or ear probes allow non-invasive
continuous assessment of oxygen saturation in patients, in order to
assess hypoxaemia and its response to therapy. They measure the
difference in absorbance of light by oxygenated and deoxygenated
blood to calculate its oxygen saturation (SaO
2
).
Exercise tests
Resting measurements are sometimes unhelpful in early disease or in
patients complaining only of exercise-induced symptoms. Exercise
Pulmonary
fibrosis
Emphysem
a
Chronic
bronchiti
s
Asthm
a
↓
↓↓
↓↓
↓↓
FEV
1
↓↓
↓
↓
↓
VC
↑/→
↓
↓
↓
FEV
1
/VC
↓↓
↓↓
→
→
TL
CO
↓/-
↓
→
↑/→
K
CO
↓
↑↑
↑
↑/→
TLC
↓
↑↑
↑
↑/→
RV
17

Medicine Lec1
Dr. Bilal
testing with spirometry before and after can be helpful in
demonstrating exercise-induced asthma. Walk tests include the self-
paced 6-minute walk and the externally paced incremental 'shuttle'
test, where patients walk at increasing pace between two cones 10 m
apart. These provide simple, repeatable assessments of disability and
response to treatment. Cardiopulmonary bicycle or treadmill exercise
testing with measurement of metabolic gas exchange, ventilation and
cardiac responses is useful for quantifying exercise limitation and for
detecting occult cardiovascular or respiratory limitation in the
breathless patient.
Pleural Fluid Analysis
A pleural effusion is a collection of fluid in the space between the
two linings (pleura) of the lung.
Normal pleural fluid: Normal pleural fluid has the following
characteristics:
•
Clear ultrafiltrate of plasma that originates from the parietal
pleura
•
A pH of 7.60-7.64
•
Protein content of less than 2% (1-2 g/dL)
•
Fewer than 1000 white blood cells (WBCs) per cubic millimeter
•
Glucose content similar to that of plasma
•
Lactate dehydrogenase (LDH) less than 50% of plasma
The initial diagnostic consideration is distinguishing transudates from
exudates. Although a number of chemical tests have been proposed
to differentiate pleural fluid transudates from exudates, the tests
first proposed by Light et al have become the criterion standards.
The fluid is considered an exudate if any of the following applies:
•
Ratio of pleural fluid to serum protein greater than 0.5
•
Ratio of pleural fluid to serum LDH greater than 0.6
•
Pleural fluid LDH greater than two thirds of the upper limits of
normal serum value
18
