Hospital-acquired or
nosocomial pneumonia
dr.bilal
•
Hospital-acquired or nosocomial pneumonia refers to a new episode of pneumonia occurring
at least 2 days after admission to hospital.
•
It is the second most common hospital-acquired infection (HAI) and the leading cause of
HAI-associated death.
•
Older people are particularly at risk, as are patients in intensive care units, especially when
mechanically ventilated, in which case the term ventilator-associated pneumonia (VAP) is
applied.
Health care-associated pneumonia (HCAP):
•
refers to the development of pneumonia in a person who has spent at least 2 days in hospital
within the last 90 days, attended a haemodialysis unit, received intravenous antibiotics, or
been resident in a nursing home or other long-term care facility.
Aetiology
•
When HAP occurs within 4-5 days of admission (early-onset), the organisms involved are
similar to those involved in CAP;
•
however, late-onset HAP is more often attributable to Gram-negative bacteria (e.g.
Escherichia, Pseudomonas and Klebsiella species), Staph. aureus (including methicillin-
resistant Staph. aureus (MRSA)) and anaerobes.
Factors predisposing to hospital-acquired pneumonia
•
Reduced host defences against bacteria
•
Reduced immune defences (e.g. corticosteroid treatment, diabetes, malignancy)
•
Reduced cough reflex (e.g. post-operative)
•
Disordered mucociliary clearance (e.g. anaesthetic agents)
•
Bulbar or vocal cord palsy
•
Aspiration of nasopharyngeal or gastric secretions
•
Immobility or reduced conscious level
•
Vomiting, dysphagia, achalasia or severe reflux
•
Nasogastric intubation
•
Bacteria introduced into lower respiratory tract
•
Endotracheal intubation/tracheostomy
•
Infected ventilators/nebulisers/bronchoscopes
•
Dental or sinus infection
•
Bacteraemia
•
Abdominal sepsis
•
I.v. cannula infection
•
Infected emboli

Clinical features and investigations
•
Universally agreed diagnostic criteria are lacking; however, HAP should be considered in
any hospitalised or ventilated patient who develops:
1. purulent sputum (or endotracheal secretions),
2. new radiological infiltrates,
3. an otherwise unexplained increase in oxygen requirement,
4. a core temperature > 38.3°C,
5. and a leucocytosis or leucopenia. Circulating biomarkers may assist with the
diagnosis but are currently non-specific.
•
Appropriate investigations are similar to those outlined for CAP, although whenever
possible, microbiological confirmation should be sought.
•
In mechanically ventilated patients, bronchoscopy-directed protected brush specimens or
bronchoalveolar lavage (BAL) may be performed.
•
Endotracheal aspirates are easy to obtain but less reliable.
Management
•
The choice of empirical antibiotic therapy should be based on local knowledge of pathogens
and drug resistance patterns, and variables such as length of hospital stay, recent antibiotics
and comorbidity.
•
Adequate Gram-negative cover is usually provided by:
•
a third-generation cephalosporin (e.g. cefotaxime) with an aminoglycoside (e.g. gentamicin)
•
meropenem or
•
a monocyclic β-lactam (e.g. aztreonam) and flucloxacillin.
•
MRSA is treated with intravenous vancomycin, but when appropriate, oral therapy may be
considered with doxycycline, rifampicin or linezolid.
•
The nature and severity of most HAPs dictate that these antibiotics are all given
intravenously, at least initially.
•
Physiotherapy is important in those who are immobile or old.
•
Adequate oxygen therapy, fluid support and monitoring are essential.
Prevention
•
Despite appropriate management, the mortality from HAP is high at approximately 30%,
emphasising the importance of prevention.
•
Good hygiene is paramount, including both hand washing and equipment.
•
Steps should be taken to minimise the chances of aspiration and limit the use of stress ulcer
prophylaxis with proton pump inhibitors.
•
Oral antiseptic (chlorhexidine 2%) may be used to decontaminate the upper airway and some
intensive care units use selective decontamination of the digestive tract when the anticipated
requirement for ventilation will exceed 48 hours.
Suppurative pneumonia, aspiration pneumonia and pulmonary abscess
•
These conditions are considered together, as their aetiology and clinical features overlap.

•
Suppurative pneumonia is characterised by destruction of the lung parenchyma by the
inflammatory process and, although microabscess formation is a characteristic histological
feature,
•
'pulmonary abscess' is usually taken to refer to lesions in which there is a large localised
collection of pus, or a cavity lined by chronic inflammatory tissue, from which pus has
escaped by rupture into a bronchus.
•
Suppurative pneumonia and pulmonary abscess often develop after the inhalation of septic
material during operations on the nose, mouth or throat, under general anaesthesia, or of
vomitus during anaesthesia or coma, particularly if oral hygiene is poor.
•
Additional risk factors for aspiration pneumonia include bulbar or vocal cord palsy, stroke,
achalasia or oesophageal reflux, and alcoholism.
•
Aspiration tends to localise to dependent areas of the lung such as the apical segment of the
lower lobe in a supine patient.
•
Suppurative pneumonia and abscess may also complicate local bronchial obstruction from a
neoplasm or foreign body.
•
Infections are usually due to a mixture of anaerobes and aerobes in common with the typical
flora encountered in the mouth and upper respiratory tract, and isolates of Bacteroides,
Fusobacterium necrophorum, anaerobic or microaerophilic cocci, and Bacteroides fragilis
may be identified.
•
When suppurative pneumonia or pulmonary abscess occurs in a previously healthy lung, the
most likely infecting organisms are Staph. aureus or Klebsiella pneumoniae.
•
Bacterial infection of a pulmonary infarct or a collapsed lobe may also produce a
suppurative pneumonia or lung abscess.
•
The organism(s) isolated from the sputum include Strep. pneumoniae, Staph. aureus, Strep.
pyogenes, H. influenzae and, in some cases, anaerobic bacteria.
•
In many cases, however, no pathogen can be isolated, particularly when antibiotics have
been given.
•
Recently, cases of community-acquired MRSA (CA-MRSA) have been reported.
•
This organism is distinct from MRSA but produces the toxin Panton-Valentine leukocidin,
which causes a rapidly progressive severe necrotising pneumonia.
•
Lemierre's syndrome is a rare cause of pulmonary abscesses. The usual causative agent is the
anaerobe, Fusobacterium necrophorum.
•
It typically commences as a sore throat, painful swollen neck, fever, rigor, haemoptysis and
dyspnoea, and bacterial spread into the jugular veins leads to thrombosis and metastatic
spread of the organisms.
•
Injecting drug-users are at particular risk of developing haematogenous lung abscess, often
in association with endocarditis affecting the pulmonary and tricuspid valves.
•
A non-infective form of aspiration pneumonia-exogenous lipid pneumonia-may follow the
aspiration of animal, vegetable or mineral oils.
Clinical features of suppurative pneumonia
Symptoms
•
Cough productive of large amounts of sputum which is sometimes fetid and blood-stained
•
Pleural pain common
•
Sudden expectoration of copious amounts of foul sputum occurs if abscess ruptures into a
bronchus
Clinical signs
•
High remittent pyrexia
•
Profound systemic upset
•
Digital clubbing may develop quickly (10-14 days)
•
Chest examination usually reveals signs of consolidation; signs of cavitation rarely found
•
Pleural rub common
•
Rapid deterioration in general health with marked weight loss can occur if disease not
adequately treated
Investigations
•
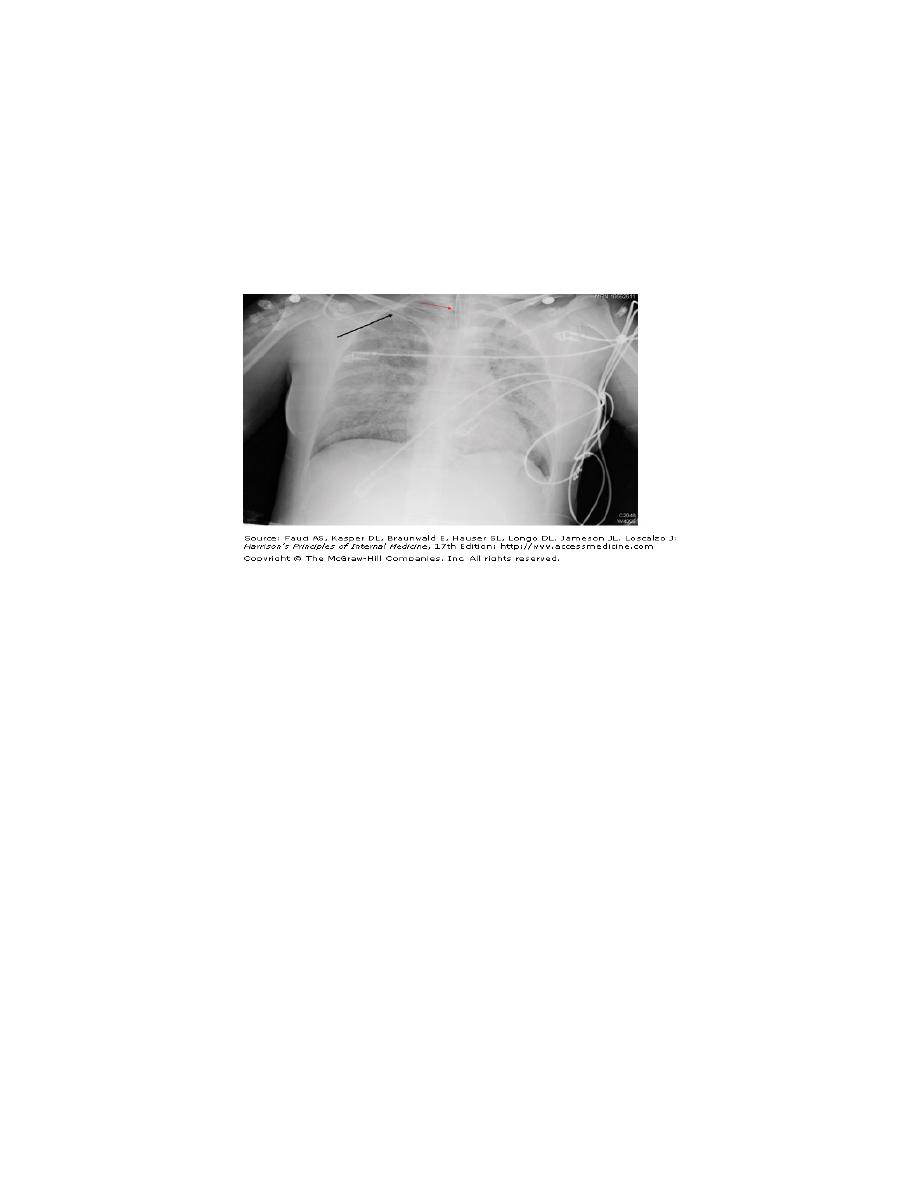
Radiological features of suppurative pneumonia include homogeneous lobar or segmental
opacity consistent with consolidation or collapse.
•
Abscesses are characterised by cavitation and fluid level.
•
Occasionally, a pre-existing emphysematous bulla becomes infected and appears as a cavity
containing an air-fluid level.
•
Sputum and blood should be sent for culture.
"
Management
•
Oral treatment with amoxicillin 500 mg 6-hourly is effective in many patients. Aspiration
pneumonia can be treated with co-amoxiclav 1.2 g 8-hourly.
•
If an anaerobic bacterial infection is suspected (e.g. from fetor of the sputum), oral
metronidazole 400 mg 8-hourly should be added.
•
Further modification of antibiotics should be informed by clinical response and the
microbiological results.
•
CA-MRSA is usually susceptible to a variety of oral non-β-lactam antibiotics, such as
trimethoprim/sulfamethoxazole, clindamycin, tetracyclines and linezolid.
•
Parenteral therapy with vancomycin or daptomycin can also be considered.
•
Fusobacterium necrophorum is highly susceptible to β-lactam antibiotics and to
metronidazole, clindamycin and third-generation cephalosporins.
•
Prolonged treatment for 4-6 weeks may be required in some patients with lung abscess.
•
Physiotherapy is of great value, especially when suppuration is present in the lower lobes or
when a large abscess cavity has formed.
•
In most patients, there is a good response to treatment, and although residual fibrosis and
bronchiectasis are common sequelae, these seldom give rise to serious morbidity.
•
Surgery should be contemplated if no improvement occurs despite optimal medical therapy.
•
Removal or treatment of any obstructing endobronchial lesion is essential.
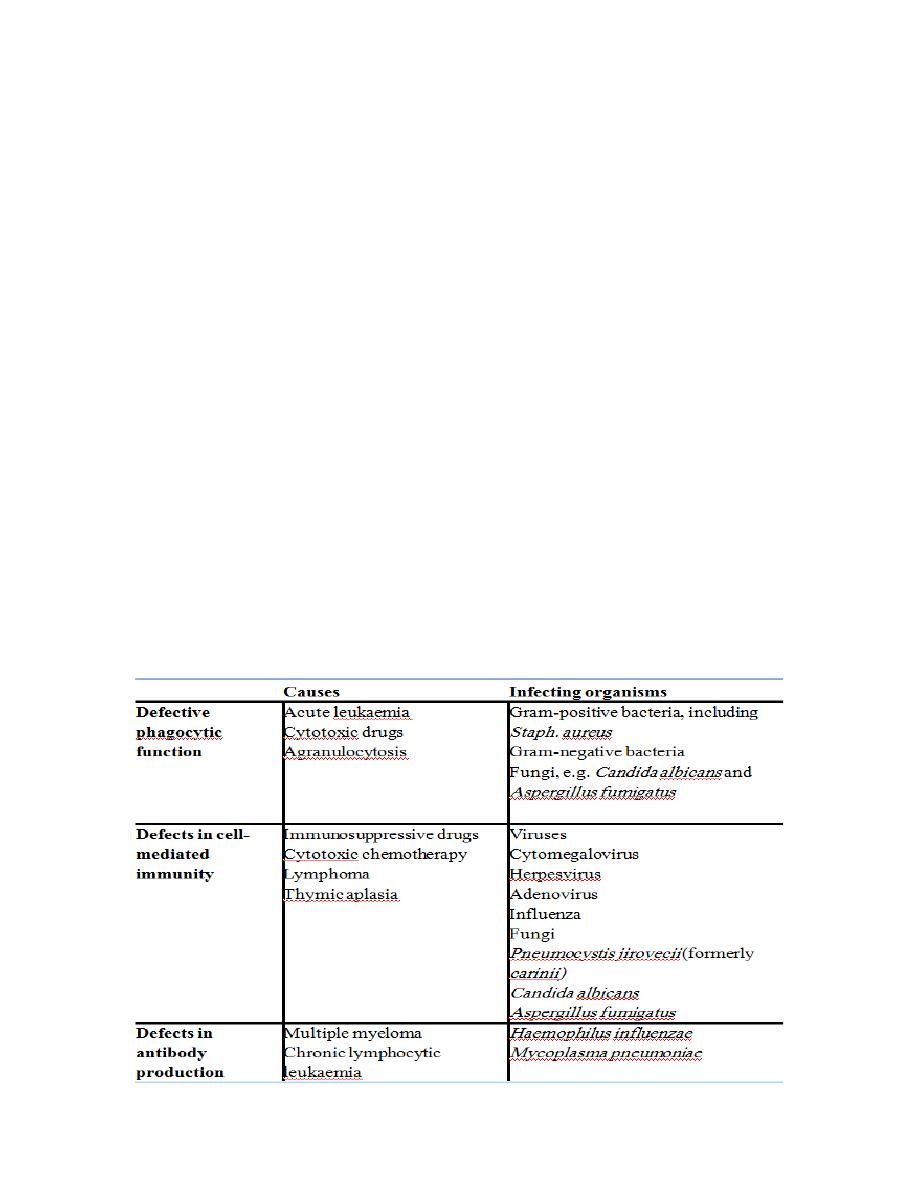
Pneumonia in the immunocompromised patient
•
Patients immunocompromised by drugs or disease (particularly HIV) are at high risk of
pulmonary infection.
•
The majority of infections are caused by the same pathogens that cause pneumonia in non-
immunocompromised individuals, but in patients with more profound immunosuppression,
unusual organisms, or those normally considered to be of low virulence or non-pathogenic,
may become 'opportunistic' pathogens .
•
In addition to the more common agents, the possibility of Gram-negative bacteria, especially
Pseudomonas aeruginosa, viral agents, fungi, mycobacteria, and less common organisms
such as Nocardia asteroides, must be considered.
•
Infection is often due to more than one organism.
"

Clinical features
•
These typically include fever, cough and breathlessness, but are less specific with more
profound degrees of immunosuppression.
•
In general, the onset of symptoms tends to be less rapid when caused by opportunistic
organisms such as Pneumocystis jirovecii and in mycobacterial infections, than with
bacterial infections .
•
In P. jirovecii pneumonia, symptoms of cough and breathlessness can be present several days
or weeks before the onset of systemic symptoms or the appearance of radiographic
abnormality.
Diagnosis
•
The approach to investigation is informed by the clinical context and severity of the illness.
•
Invasive investigations such as bronchoscopy, BAL, transbronchial biopsy or surgical lung
biopsy are often impractical, as many patients are too ill to undergo these safely.
•
However, 'induced sputum' may offer a relatively safe method of obtaining microbiological
samples.
•
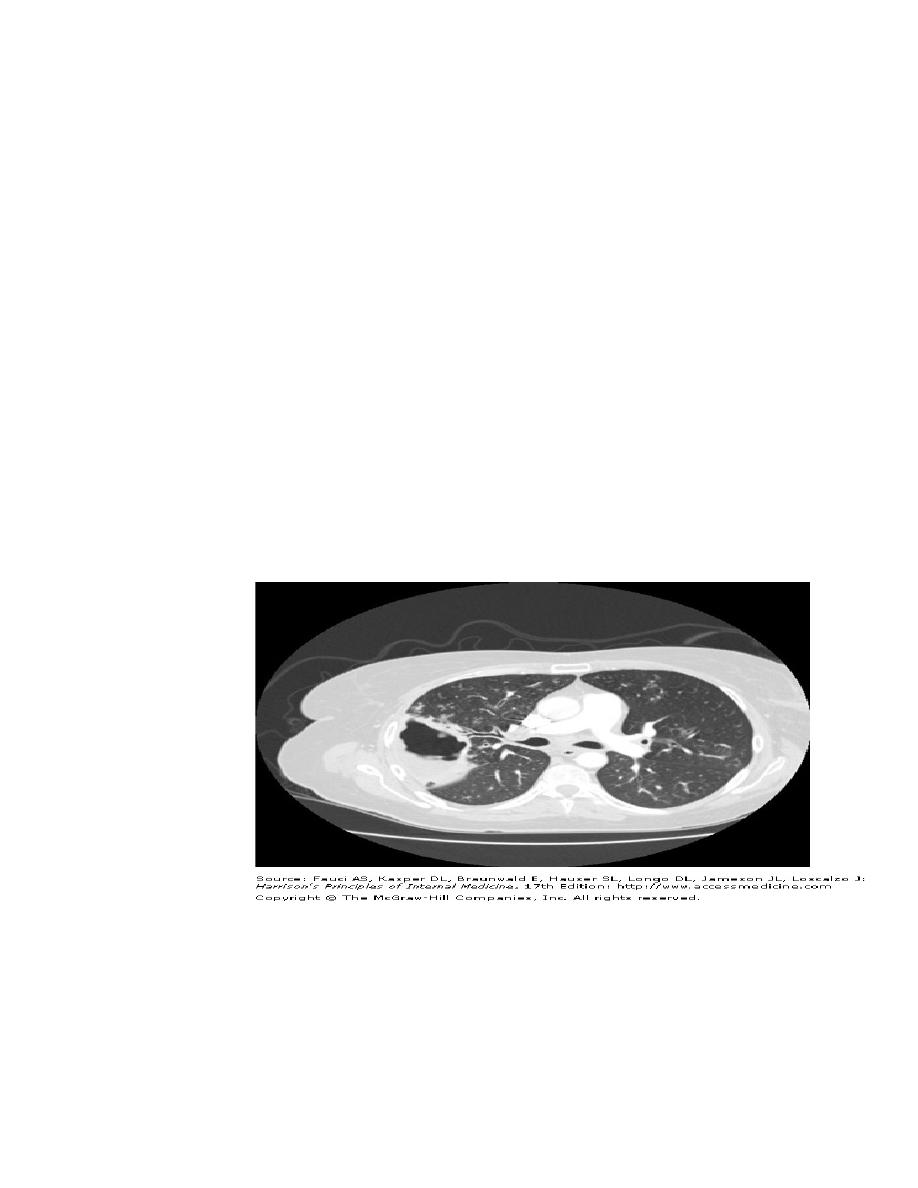
HRCT is useful in differentiating the likely cause:
•
Focal unilateral airspace opacification favours bacterial infection, mycobacteria or nocardia.
•
Bilateral opacification favours P. jirovecii pneumonia, fungi, viruses and unusual bacteria,
e.g. nocardia.
•
Cavitation may be seen with N. asteroides, mycobacteria and fungi.
•
The presence of a 'halo sign' may suggest Aspergillus .
•
Pleural effusions suggest a pyogenic bacterial infection and are uncommon in P. jirovecii
pneumonia.
Management
•
In theory, treatment should be based on an established aetiological diagnosis; in practice, the
causative agent is frequently unknown and broad-spectrum antibiotic therapy is required,
such as:
•
a third-generation cephalosporin, or a quinolone, plus an antistaphylococcal antibiotic, or
•
an antipseudomonal penicillin plus an aminoglycoside.
•
Thereafter treatment may be tailored according to the results of investigations and the
clinical response.
•
Depending on the clinical context and response to treatment, antifungal or antiviral
therapies may be added.
•
Mechanical ventilation increases the risk of nosocomial pneumonia and is associated with a
greater mortality rate.
•
It may be avoided by the early use of NIV.
•
The delivery of NIV via a hood is as effective as a face mask and allows the patient to
expectorate, communicate and feed.
Severe acute respiratory distress syndrome (SARS):
•
SARS rose to prominence in late 2002 when a series of cases in the Guangdong
Province, China, was followed by an international outbreak.
•
The illness is characterised by the presence of a high fever (> 38°C), malaise and
muscle aches and later a dry cough with shortness of breath or difficulty in breathing.
•
A history of travel within 10 days of onset of symptoms to an area with documented
or suspected community transmission of SARS or close contact within 10 days of
onset of symptoms with a person known to be a suspect SARS case is typical.
•
The chest X-ray is usually indicative of pneumonia.
•
SARS has recently been attributed to the Corona virus (Urbani SARS-associated
coronavirus); however, additional viruses, or other factors may be involved.
•
The optimum method of treating SARS remains uncertain and is largely supportive,
including mechanical ventilation.
•
The role of antibacterial, antiviral and immunomodulatory therapy is still under
research.
"
