
Respiratory System
Dr.M.Ali
Chronic obstructive pulmonary disease (COPD)
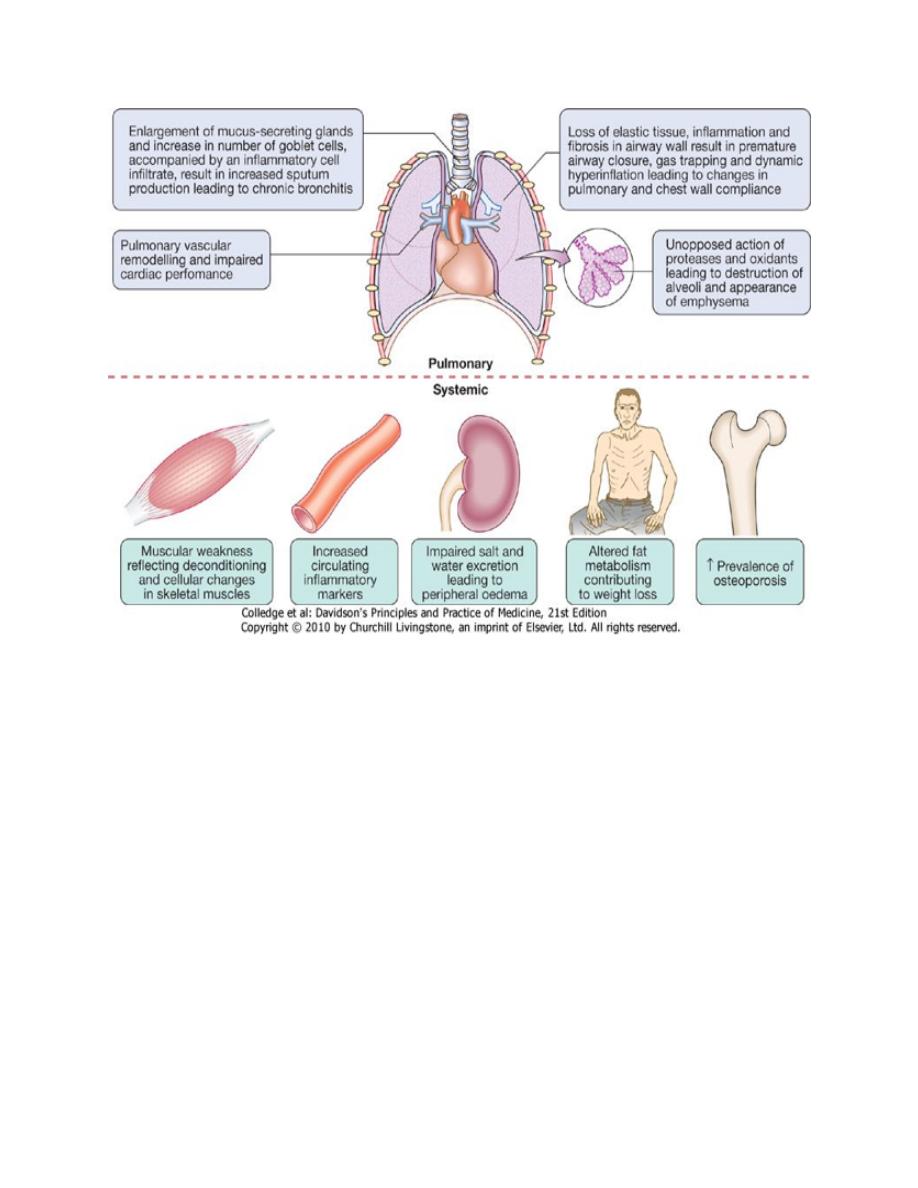
COPD is defined as a preventable and treatable lung disease with some significant
extrapulmonary effects that may contribute to the severity in individual patients.
The pulmonary component is characterised by airflow limitation that is not
fully reversible. The airflow limitation is usually progressive and associated with
an abnormal inflammatory response of the lung to noxious particles or
gases.Related diagnoses include chronic bronchitis (cough and sputum on most
days for at least 3 consecutive months for at least 2 successive years) and
emphysema (abnormal permanent enlargement of the airspaces distal to the
terminal bronchioles, accompanied by destruction of their walls and without
obvious fibrosis). Extrapulmonary manifestations include impaired nutrition,
weight loss and skeletal muscle dysfunction .
Epidemiology
Prevalence is directly related to the prevalence of tobacco smoking and, in low-
and middle-income countries, the use of biomass fuels. Current estimates suggest
that 80 million people world-wide suffer from moderate to severe disease.In 2005,
COPD contributed to more than 3 million deaths (5% of deaths globally), but by
2020 it is forecast to represent the third most important cause of death world-
wide.The anticipated rise in morbidity and mortality from COPD will be greatest in
Asian and African countries as a result of their increasing tobacco consumption.
Aetiology
Cigarette smoking represents the most significant risk factor for COPD and relates
to both the amount and the duration of smoking.It is unusual to develop COPD
with less than 10 pack years (1 pack year = 20 cigarettes/day/year) and not all
smokers develop the condition, suggesting that individual susceptibility factors are
important.

Respiratory System
Dr.M.Ali
Risk factors for development of COPD
a- Exposures
• Tobacco smoke: accounts for 95% of cases in UK
• Biomass solid fuel fires: wood, animal dung, crop residues and coal lead to
high levels of indoor air pollution
• Occupation: coal miners and those who work with cadmium
• Outdoor and indoor air pollution
• Low birth weight: may reduce maximally attained lung function in young
adult life
• Lung growth: childhood infections or maternal smoking may affect growth
of lung during childhood, resulting in a lower maximally attained lung
function in adult life
• Infections: recurrent infection may accelerate decline in FEV
1
; persistence of
adenovirus in lung tissue may alter local inflammatory response
predisposing to lung damage; HIV infection is associated with emphysema
• Low socioeconomic status
• Nutrition: role as independent risk factor unclear
• Cannabis smoking
b-Host factors
• Genetic factors: α
1
-antiproteinase deficiency; other COPD susceptibility
genes are likely to be identified
• Airway hyper-reactivity

Respiratory System
Dr.M.Ali
Pathophysiology
COPD has both pulmonary and systemic components. The changes in pulmonary
and chest wall compliance mean that collapse of intrathoracic airways during
expiration is exacerbated, during exercise as the time available for expiration
shortens, resulting in dynamic hyperinflation. Increased V/Q mismatch increases
the dead space volume and wasted ventilation. Flattening of the diaphragmatic
muscles and an increasingly horizontal alignment of the intercostal muscles place
the respiratory muscles at a mechanical disadvantage. The work of breathing is
therefore markedly increased, first on exercise but, as the disease advances, at rest
too. Emphysema may be classified by the pattern of the enlarged airspaces:
centriacinar, panacinar and periacinar. Bullae form in some individuals. This
results in impaired gas exchange and respiratory failure.
Clinical features
COPD should be suspected in any patient over the age of 40 years who presents
with symptoms of chronic bronchitis and/or breathlessness. Depending on the
presentation, important differential diagnoses include chronic asthma, tuberculosis,
bronchiectasis and congestive cardiac failure.Cough and associated sputum
production are usually the first symptoms, often referred to as a 'smoker's cough'.
Haemoptysis may complicate exacerbations of COPD but should not be attributed
to COPD without thorough investigation.Breathlessness usually brings about the
first presentation to medical attention.the modified Medical Research Council
(MRC) dyspnoea scale may also be useful. In advanced disease, enquiry should be
made as to the presence of oedema (which may be seen for the first time during an
exacerbation) and morning headaches, which may suggest hypercapnia.

Respiratory System
Dr.M.Ali
Modified MRC dyspnoea scale
Grad
e
Degree of breathlessness related to activities
0
No breathlessness except with strenuous exercise
1
Breathlessness when hurrying on the level or walking up a slight hill
2
Walks slower than contemporaries on level ground because of breathlessness or has to stop for breath when walking at
own pace
3
Stops for breath after walking about 100 m or after a few minutes on level ground
4
Too breathless to leave the house, or breathless when dressing or undressing
Physical signs are non-specific, correlate poorly with lung function, and are
seldom obvious until the disease is advanced. Breath sounds are typically quiet;
crackles may accompany infection but if persistent raise the possibility of
bronchiectasis.Finger clubbing is not a feature of COPD and should trigger further
investigation for lung cancer, bronchiectasis or fibrosis. The presence of pitting
oedema should be documented but the frequently used term 'cor pulmonale' is
actually a misnomer, as the right heart seldom 'fails' in COPD and the occurrence
of oedema usually relates to failure of salt and water excretion by the hypoxic,
hypercapnic kidney.The body mass index (BMI) is of prognostic significance and
should be recorded. Two classical phenotypes have been described: 'pink puffers'
and 'blue bloaters'. The former('pink puffers) are typically thin and breathless,
and maintain a normal PaCO
2
until the late stage of disease. The latter ('blue
bloaters')develop (or tolerate) hypercapnia earlier and may develop oedema and
secondary polycythaemia. In practice, these phenotypes often overlap.
Respiratory System
Dr.M.Ali
Investigations
Although there are no reliable radiographic signs that correlate with the severity of
airflow limitation, a chest X-ray is essential to identify alternative diagnoses such
as cardiac failure, other complications of smoking such as lung cancer, and the
presence of bullae.
A full blood count is useful to exclude anaemia or document polycythaemia, and
in younger patients with predominantly basal emphysema, α
1
-antiproteinase
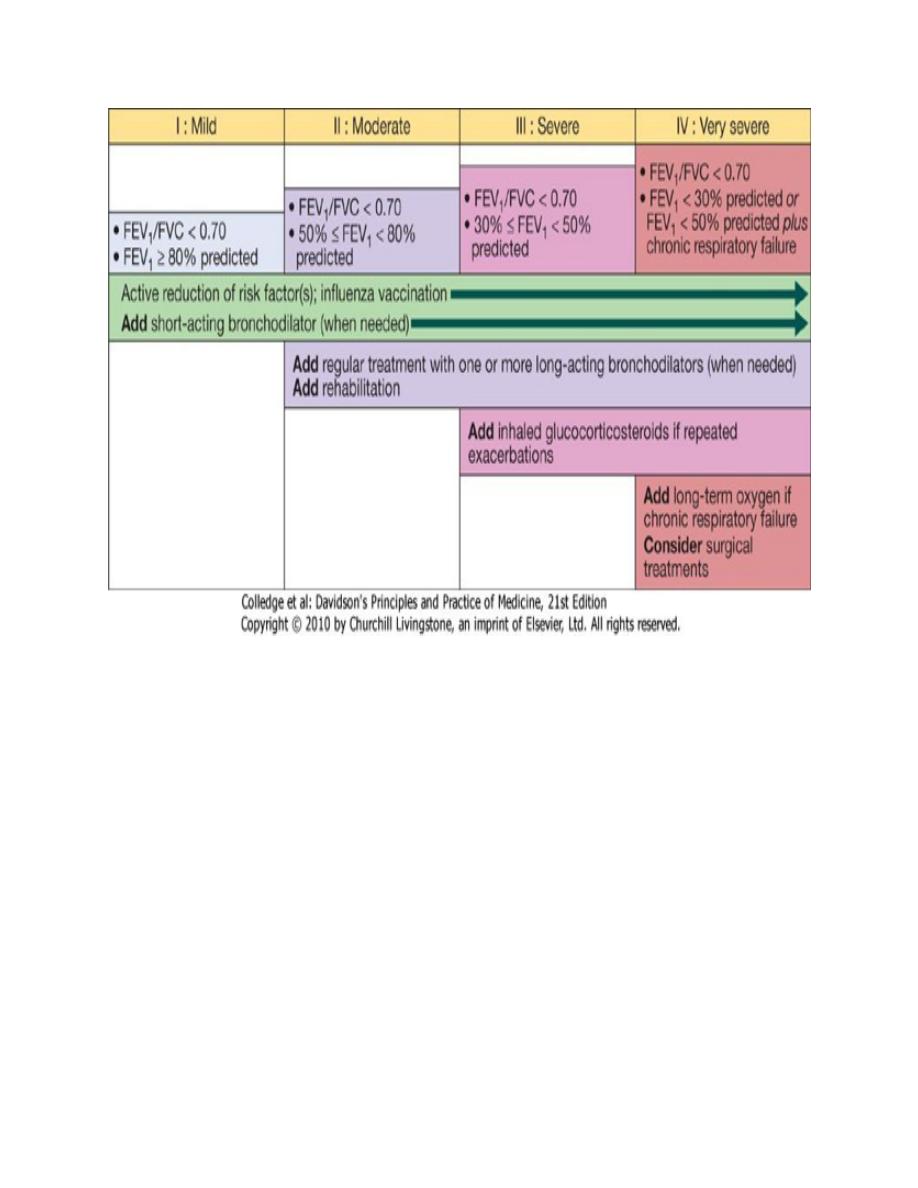
should be assayed. The diagnosis requires objective demonstration of airflow
obstruction by spirometry and is established when the post-bronchodilator
FEV
1
is less than 80% of the predicted value and accompanied by FEV
1
/FVC
< 70%. An FEV
1
/FVC < 70% with an FEV
1
of 80% or more suggests the presence
of mild disease, although this may be a normal finding in older patients. The
severity of COPD may be defined according to the post-bronchodilator FEV
1
as a
percentage of the predicted value for the patient's age . A low peak flow is
Respiratory System
Dr.M.Ali
consistent with COPD but is non-specific, does not discriminate between
obstructive and restrictive disorders, and may underestimate the severity of airflow
limitation.
Spirometric classification of COPD severity based on post-bronchodilator
FEV1
Stag
e
Severity
FEV
1
I
Mild
FEV
1
/FVC < 0.70
FEV
1
≥80% predicted
II
Moderate
FEV
1
/FVC < 0.70
50% ≤ FEV
1
< 80% predicted(50%-80%)
III
Severe
FEV
1
/FVC < 0.70
30% ≤ FEV
1
< 50% predicted(30%-50%)
IV
Very severe
FEV
1
/FVC < 0.70
FEV
1
< 30% predicted or FEV
1
< 50% predicted plus chronic
respiratory failure
Measurement of lung volumes provides an assessment of hyperinflation. This is
generally performed using the helium dilution technique.The presence of
emphysema is suggested by a low gas transfer factor . Exercise tests provide an
objective assessment of exercise tolerance and a baseline on which to judge the
response to bronchodilator therapy or rehabilitation programmes; they may also be
valuable when assessing prognosis.
Pulse oximetry may prompt referral for a domiciliary oxygen assessment if less
than 93%.
Respiratory System
Dr.M.Ali
HRCT is likely to play an increasing role in the assessment of COPD, as it allows
the detection, characterisation and quantification of emphysema and is more
sensitive than a chest X-ray at detecting bullae.
Management
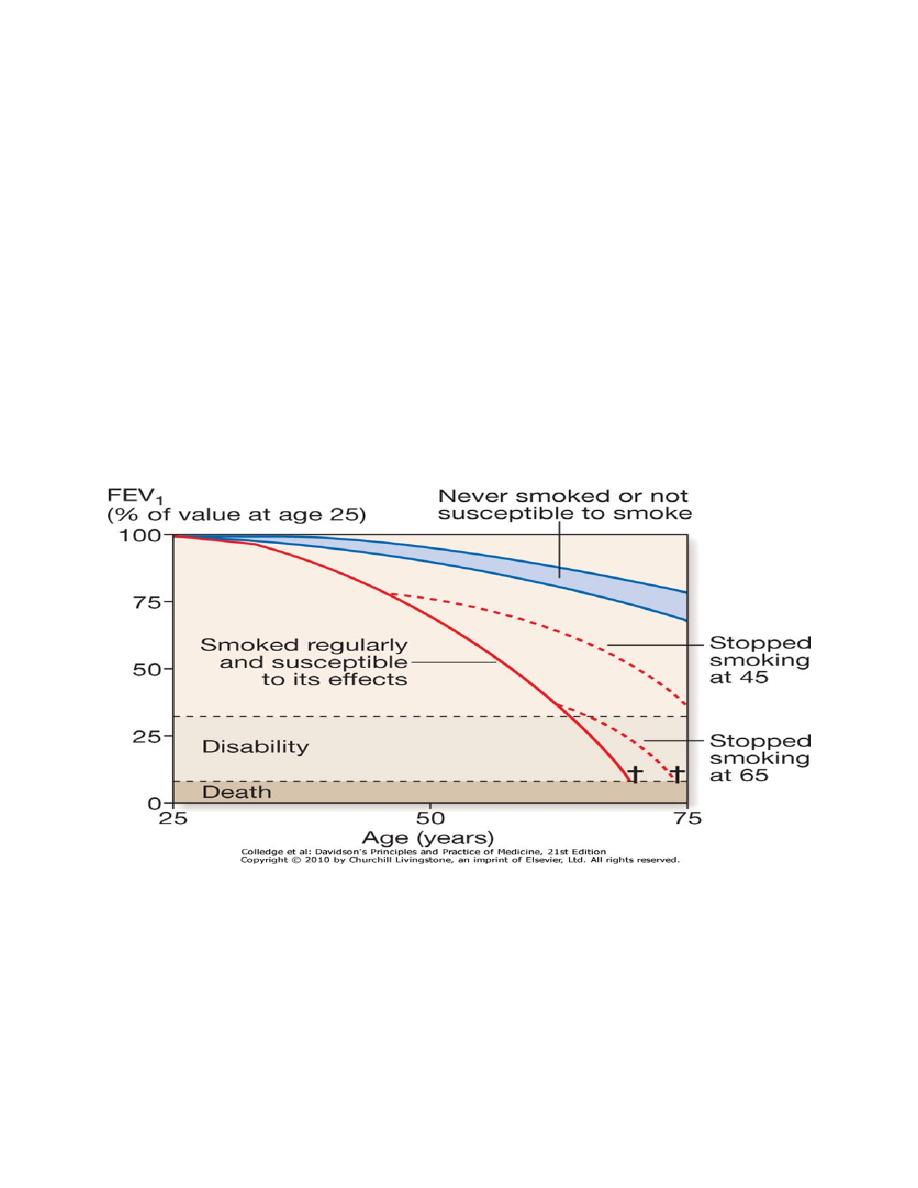
Smoking cessation:
Every attempt should be made to highlight the role of smoking in the development
and progress of COPD, advising and assisting the patient toward smoking
cessation. On cessation patients should be warned to expect an apparent worsening
of chest symptoms and reassured that this is temporary.
Cessation is difficult but highly rewarding and remains the only intervention
proven to decelerate the decline in FEV1.
Smoking cessation and COPD 'Sustained smoking cessation in mild to moderate
COPD is accompanied by a reduced decline in FEV
1
compared to persistent
smokers.' Reducing the number of cigarettes smoked each day has little impact on
the course and prognosis of COPD, but complete cessation is accompanied by an
improvement in lung function and deceleration in the rate of FEV
1
decline.In
regions where the indoor burning of biomass fuels is important, the introduction of
non-smoking cooking devices or the use of alternative fuels should be encouraged.

Respiratory System
Dr.M.Ali
Bronchodilator therapy is central to the management of breathlessness.The
inhaled route is preferred and a number of different agents delivered by a variety of
devices are available. Short-acting bronchodilators, such as the β
2
-agonists
salbutamol and terbutaline, or the anticholinergic, ipratropium bromide, may be
used for patients with mild disease. Longer-acting bronchodilators, such as the β
2
-
agonists salmeterol and formoterol, or the anticholinergic tiotropium bromide, are
more appropriate for patients with moderate to severe disease.Significant
improvements in breathlessness may be reported despite minimal changes in FEV
1
,
probably reflecting improvements in lung emptying that reduce dynamic
hyperinflation and ease the work of breathing. Oral bronchodilator therapy may be
contemplated in patients who cannot use inhaled devices efficiently. Theophylline
preparations improve breathlessness and quality of life, but their use has been
limited
by
side-effects,
unpredictable
metabolism
and
drug
interactions.Bambuterol, a pro-drug of terbutaline, is used on occasion. Orally
active highly selective phosphodiesterase inhibitors are currently under
development.
Corticosteroids
Inhaled corticosteroids (ICS) reduce the frequency and severity of exacerbations;
they are currently recommended in patients with severe disease (FEV
1
< 50%) who
report two or more exacerbations requiring antibiotics or oral steroids per year.
Regular use is associated with a small improvement in FEV
1
, but they do not alter
the natural history of the FEV
1
decline. It is more usual to prescribe a fixed
combination of an ICS with a LABA.Oral corticosteroids are useful during
exacerbations but maintenance therapy contributes to osteoporosis and impaired
skeletal muscle function and should be avoided.
Respiratory System
Dr.M.Ali
Pulmonary rehabilitation
Exercise should be encouraged at all stages and patients should be reassured that
breathlessness, whilst distressing, is not dangerous. Multidisciplinary programmes
that incorporate physical training, disease education and nutritional counselling
reduce symptoms, improve health status and enhance confidence.
Oxygen therapy
Long-term domiciliary oxygen therapy (LTOT) 'Long-term home oxygen
therapy improves survival in selected patients with COPD complicated by severe
hypoxaemia (arterial PaO
2
less than 8.0 kPa (55 mmHg)).'
Prescription of long-term oxygen therapy (LTOT) in COPD Arterial blood
gases measured in clinically stable patients on optimal medical therapy on at least
two occasions 3 weeks apart:

Respiratory System
Dr.M.Ali
1. PaO
2
< 7.3 kPa (55 mmHg) irrespective of PaCO
2
and FEV
1
< 1.5 L
2. PaO
2
7.3-8 kPa (55-60 mmHg) plus pulmonary hypertension, peripheral
oedema or nocturnal hypoxaemia
3. patient stopped smoking.
• Use at least 15 hours/day at 2-4 L/min to achieve a PaO
2
> 8 kPa (60
mmHg) without unacceptable rise in PaCO
2
.
• Surgical intervention:
Young patients in whom large bullae compress surrounding normal lung tissue,
who otherwise have minimal airflow limitation and a lack of generalised
emphysema, may be considered for bullectomy.Patients with predominantly upper
lobe emphysema, with preserved gas transference and no evidence of pulmonary
hypertension, may benefit from lung volume reduction surgery (LVRS), in which
peripheral emphysematous lung tissue is resected with the aim of reducing
hyperinflation and decreasing the work of breathing may lead to
improvements in FEV
1
, lung volumes, exercise tolerance and quality of life.
Both bullectomy and LVRS can be performed thorascopically, minimising
morbidity, and endoscopic techniques for lung volume reduction are also under
development. Lung transplantation may benefit carefully selected patients with
advanced disease but is limited by shortage of donor organs.
Other measures
Patients with COPD should be offered an annual influenza vaccination and, as
appropriate, pneumococcal vaccination. Obesity, poor nutrition, depression and
social isolation should be identified and, if possible, improved. Mucolytic therapy
such as acetylcysteine, or antioxidant agents are occasionally used but with limited
evidence.
Acute exacerbations of COPD
Acute exacerbations of COPD are characterised by an increase in symptoms and
deterioration in lung function and health status. They become more frequent as the

Respiratory System
Dr.M.Ali
disease progresses and are usually triggered by bacteria, viruses or a change in air
quality. They may be accompanied by the development of respiratory failure
and/or fluid retention and represent an important cause of death. Many patients can
be managed at home with the use of increased bronchodilator therapy, a short
course of oral corticosteroids, and if appropriate, antibiotics. The presence of
cyanosis, peripheral oedema or an alteration in consciousness should prompt
referral to hospital.In other patients, consideration of comorbidity and social
circumstances may influence decisions regarding hospital admission.
Management of Acute exacerbations of COPD
Oxygen therapy
In patients with an exacerbation of severe COPD, high concentrations of oxygen
may cause respiratory depression and worsening acidosis . Controlled oxygen at
24% or 28% should be used with the aim of maintaining a PaO
2
> 8 kPa (60 mmHg)
(or an SaO
2
> 90%) without worsening acidosis.
Bronchodilators
Nebulised short-acting β
2
-agonists combined with an anticholinergic agent (e.g.
salbutamol with ipratropium) should be administered. With careful supervision, it
is usually safe to drive nebulisers with oxygen, but if concern exists regarding
oxygen sensitivity, nebulisers may be driven by compressed air and supplemental
oxygen delivered by nasal cannula.
Corticosteroids:
Oral prednisolone reduces symptoms and improves lung function. Currently, doses
of 30 mg for 10 days are recommended but shorter courses may be acceptable.
Prophylaxis against osteoporosis should be considered in patients who receive
repeated courses of steroids .
Antibiotic therapy:
The role of bacteria in exacerbations remains controversial and there is little
evidence for the routine administration of antibiotics. They are currently
recommended for patients reporting an increase in sputum purulence, sputum
volume or breathlessness. In most cases, simple regimens are advised, such as an

Respiratory System
Dr.M.Ali
aminopenicillin or a macrolide. Co-amoxiclav is only required in regions where β-
lactamase-producing organisms are known to be common.
Non-invasive ventilation:
If, despite the above measures, the patient remains tachypnoeic and acidotic (H
+
≥
45/pH < 7.35), then NIV should be commenced .Several studies have demonstrated
its benefit. Mechanical ventilation may be contemplated in those with a reversible
cause for deterioration (e.g. pneumonia), or when no prior history of respiratory
failure has been noted.
Non-invasive ventilation in COPD exacerbations
'Non-invasive ventilation is safe and effective in patients with an acute
exacerbation of COPD complicated by mild to moderate respiratory acidosis and
should be considered early in the course of respiratory failure to reduce the need
for endotracheal intubation, treatment failure and mortality.‘
Additional therapy
Exacerbations may be accompanied by the development of peripheral oedema;
this usually responds to diuretics. There has been a vogue for using an infusion of
intravenous aminophylline but evidence for benefit is limited and there are risks of
inducing arrhythmias and drug interactions. The use of the respiratory stimulant
doxapram has been largely superseded by the development of NIV, but it may be
useful for a limited period in selected patients with a low respiratory rate.
Prognosis
COPD has a variable natural history but is usually progressive. The prognosis is
inversely related to age and directly related to the post-bronchodilator FEV
1
.
Additional poor prognostic indicators include weight loss and pulmonary
hypertension. A recent study has suggested that a composite score (BODE index)
comprising the body mass index (B), the degree of airflow obstruction (O), a
measurement of dyspnoea (D) and exercise capacity (E), may assist in predicting
death from respiratory and other causes . Respiratory failure, cardiac disease and
lung cancer represent common modes of death.

Respiratory System
Dr.M.Ali
Calculation of the BODE index
Points on BODE index
Variable
0
1
2
3
FEV
1
≥ 65
50-64
36-49
≤ 35
Distance walked in
6 min (m)
≥ 350
250-349
150-249
≤ 149
MRC
dyspnoea
scale
0-1
2
3
4
Body mass index
> 21
≤ 21
A patient with a BODE score of 0-2 has a mortality rate of around 10% at 52 months,
whereas a patient with a BODE score of 7-10 has a mortality rate of around 80% at 52
months.
Discharge :
Discharge from hospital may be planned once the patient is clinically stable on his
or her usual maintenance medication. The provision of a nurse-led 'hospital at
home' team providing short-term nebuliser loan improves discharge rates and
provides additional support for the patient.
