Fluid and electrolytes
Blood transfusion
Surgical drains
And Others topics
Anwar Qais Sa'adoon
تمت الطباعة في البصرة
–
ناحية الشهيد عز الدين سليم
New surgical booklet Anwar Qais Saadoon Basrah medical college 2
بسم اهلل الرمحن الرحيم
احلمد هلل رب العاملني وصلى اهلل
تعاىل
على
خري خلقه أمج
عني
حممد
األمني
و
على آله
الطيبني الطاهرين
.
ّيسر
ني
أ
ن
أضع
هذا اجلهد امل
وتااضع
بني ايديكم
إخاتي
وأخااتي
والوتمس منكم العذر عن أي
خطأ
أو نقص
ًسائال
اهلل تعاىل ان ي
افقنا
وإياكم اىل ما حيب ويرضى وأ
َّن مين
عليكم و
علينا بالصحة والعافية
ٌانه مسيع
ُجميب
الدعاء
.
أنار قيس سعدون
02
/
8
/
0224
New surgical booklet Anwar Qais Saadoon Basrah medical college 3
Contents
Chapter I :
Fluid and electrolytes
Chapter II :
Blood transfusion
Chapter III :
Post operative
complication
Chapter IV :
Surgical drains
Chapter V :
Suture types
Chapter VI :
Shock
Chapter VII :
Wounds, tissue repair
Chapter VIII :
Nutrition in surgery
Chapter IX :
Stomas
Chapter X :
History of common
surgical cases
4
24
33
41
46
51
63
69
75
80
New surgical booklet Anwar Qais Saadoon Basrah medical college 4
Chapter I
Fluid and electrolytes
Topics
Body fluid compartments
Water Homeostasis
Effective circulating volume
Daily water requirements
Daily electrolyte requirements
Intravenous fluids
Types of Intravenous fluids
Maintenance fluid
Which Fluid to Choose?
The fluid balance chart
Sizes of the I.V cannulae
Electrolyte balance
Sodium balance
Hyponatremia
Hypernatremia
Potassium balance
Hypokalemia
Hyperkalemia
Calcium balance
Hypocalcemia
hypercalcemia
Acid-Base homeostasis
5
5
5
6
6
7
7
11
11
13
14
15
15
15
17
18
19
20
21
21
22
23
New surgical booklet Anwar Qais Saadoon Basrah medical college 5
Body fluid compartments
The TBW is distributed in various locations throughout the body, known as
fluid compartments. These vary somewhat by age, but on average:
Intracellular Fluid Compartment: 2/3 of TBW, 40% of body weight
Extracellular Fluid Compartment: 1/3 of TBW, 20% of body weight
ECF compartment is further divided:
Interstitial Fluid 3/4 of ECF, 15% of body weight
Plasma Water 1/4 of ECF, 5% of body weight
Water Homeostasis
1. Total Body Water ( TBW ) – about 40L
-water intake (food and drink - 2300ml; cell metabolism- 200ml
total- 2500)
-water output (kidneys – 1500ml; skin- 600ml; lungs- 300ml;
GI tract-100ml; total – 2500ml)
2. Disturbances of Water Homeostasis
-hypervolemia (infusion of isotonic i.v. fluid)
-hypovolemia (blood loss)
-overhydration (drinking too much water)
-dehydration (sweating)
3. Four Primary Mechanisms Regulate Fluid Homeostasis
-ADH
-thirst mechanism
-aldosterone
-sympathetic nervous system
Effective circulating volume
That portion of the extracellular vascular space that is perfusing the tissues.
Adequate effective circulating
volume MUST be maintained at ALL TIMES. Decreased effective
circulating volume can be seen in:
• Volume loss (vomiting, diarrhea, hemorrhage, burns, surgical drainage)
• Normal or increased volume (cardiac dysfunction, liver disease)
Effective circulating volume is regulated by:
Sympathetic nerves via baroreceptors
Circulating catecholamines
Renin-angiotensin-aldosterone system ADH
New surgical booklet Anwar Qais Saadoon Basrah medical college 6
Daily water requirements
Historically, daily water needs have been estimated based on energy
expenditure:
1 kcal expended/day = 1 ml H2O required
Based on computed energy expenditure of the average hospitalized patient:
First 10 kg = 100ml/kg/day H2O
Second 10 kg = 50 ml/kg/day H2O
Weight over 20 kg = 20 ml/kg/day H2O
Therefore, for a 25kg child, the daily fluid requirement based on this scheme
would
1000ml/day for the first 10kg (10kg X 100ml/kg/day)
500ml/day for the second 10kg (10kg X 50ml/kg/day)
+ 100ml/day for the 5kg over 20kg (5kg X 20ml/kg/day)
TOTAL:1600ml/day for 25kg child
We also can calculate maintance fluid by using “4-2-1” rule and as the
following:
First 10 kg = 4 ml/kg/hr H2O
Second 10 kg = 2 ml/kg/hr H2O
Weight over 20 kg = 1 ml/kg/hr H2O
Therefore, for the same 25kg child used in the example above, IV fluids
based on this method would be:
40ml/hr for the first 10kg (10kg X 4 ml/kg/hr)
20ml/hr for the second 10kg (10kg X 2 ml/kg/hr)
+ 5ml/hr for the 5kg over 20kg (5kg X 1 ml/kg/hr)
TOTAL: 65ml/hr for 25kg child, or
1560ml/day (65ml/hr X 24 hrs/day), pretty close to the 1600ml/day
calculated by the long method, above.
Daily electrolyte requirements
Estimates for daily electrolytes can be based on metabolic demands or, by
extension, on daily water needs:
• Sodium 2 - 3 mEq/100ml H2O /day
• Potassium 1 - 2 mEq/100ml H2O /day
• Chloride 2 - 3 mEq/100ml H2O /day
New surgical booklet Anwar Qais Saadoon Basrah medical college 7
Intravenous fluids
Intravenous fluids may be divided into:
1- Crystalloid solutions - clear fluids made up of water and
electrolyte solutions; Will cross a semi-permeable membrane
e.g Normal, hypo and hypertonic saline solutions; Dextrose solutions;
Ringer’s lactate and Hartmann’s solution.
2- Colloid solutions – Gelatinous solutions containing particles
suspended in solution. These particles will not form a sediment
under the influence of gravity and are largely unable to cross a
semi-permeable membrane. e.g. Albumin, Dextrans, Hydroxyethyl
starch [HES]; Haemaccel and Gelofusine
Crystalloid solutions:
A- Saline Solutions
(1) 0.9% Normal Saline – Think of it as ‘Salt and water’
• Principal fluid used for intravascular resuscitation and replacement of
salt loss e.g diarrhoea and vomiting
• Contains: Na+ 154 mmol/l, K+ - Nil, Cl
-
- 154 mmol/l; But K+ is often
added
• IsoOsmolar compared to normal plasma
• Distribution: Stays almost entirely in the Extracellular space
Of 1 litre – 750ml Extra cellular fluid; 250ml
intravacular fluid
• So for 100ml blood loss – need to give 400ml N.saline [only 25%
remains intravascular]
(2) 0.45% Normal saline = ‘Half’ Normal Saline = HYPOtonic saline
• Reserved for severe hyperosmolar states severe dehydration
• Leads to HYPOnatraemia if plasma sodium is normal
• May cause rapid reduction in serum sodium if used in excess or
infused too rapidly. This may lead to cerebral oedema and rarely,
central pontine demyelinosis ; Use with caution!
New surgical booklet Anwar Qais Saadoon Basrah medical college 8
(3) 1.8, 3.0, 7.0, 7.5 and 10% Saline = HYPERtonic saline
• Reserved for plasma expansion with colloids
• In practice rarely used in general wards; Reserved for high
dependency, specialist areas
• Distributed almost entirely in the ECF and intravascular space. This
leads to an osmotic gradient between the ECF and ICF, causing
passage of fluid into the EC space. This fluid distributes itself evenly
across the ECF and intravascualr space, in turn leading to intravascular
repletion.
• Large volumes will cause HYPERnatraemia and IC dehydration.
B- Dextrose solutions:
(1) 5% Dextrose (often written D5W) – Think of it as ‘Sugar and
Water’
• Primarily used to maintain water balance in patients who are not able
to take anything by mouth; Commonly used post-operatively in
conjuction with salt retaining fluids ie saline; Often prescribed as 2L
D5W: 1L N.Saline [‘Physiological replacement’ of water and Na+
losses]
• Provides some calories [ approximately 10% of daily requirements]
• Regarded as ‘electrolyte free’ – contains NO Sodium, Potassium,
Chloride or Calcium
• Distribution: <10% Intravascular; > 66% intracellular
• When infused is rapidly redistributed into the intracellular space; Less
than 10% stays in the intravascular space therefore it is of limited use
in fluid resuscitation.
• For every 100ml blood loss – need 1000ml dextrose replacement [10%
retained in intravascular space
• Common cause of iatrogenic hyponatraemia in surgical patient
(2) Dextrose saline – Think of it as ‘a bit of salt and sugar’
• Similar indications to 5% dextrose; Provides Na+ 30mmol/l and Cl
-
30mmol/l Ie a sprinkling of salt and sugar!
• Primarily used to replace water losses post-operatively
• Limited indications outside of post-operative replacement – ‘Neither
really saline or dextrose; Advantage – doesn’t commonly cause water
or salt overload.
New surgical booklet Anwar Qais Saadoon Basrah medical college 9
Colloid solutions:
• The colloid solutions contain particles which do not readily cross
semi-permeable membranes such as the capillary membrane
• Thus the volume infused stays (initially) almost entirely within the
intravascular space
• Stay intravascular for a prolonged period compared to crystalloids
• However they leak out of the intravascular space when the capillary
permeability significantly changes e.g. Severe trauma or sepsis
• Until recently they were regarded as the gold standard for
intravascular resuscitation
• Because of their gelatinous properties they cause platelet dysfunction
and interfere with fibrinolysis and coagulation factors (factor VIII) –
thus they can cause significant coagulopathy in large volumes.
Questions to ask before prescribing fluid:
1. Is my patient Euvolaemic, Hypovolaemic or
Hypervolaemic?
Assess the patient
Euvolaemic: veins are well flled, extremities are warm,
blood pressure and heart rate are normal (depending on
other pathology).
Hypovolaemic:The patient may have cold hands and feet,
absent veins, hypotension, tachycardia, oliguria and confu-
sion. History of fluid loss or low intake.
Hypervolaemic: Patient is oedematous, may have inspira-
tory crackles; history of poor urine output or fluid overload.
2. Does my patient need IV fluid? Why?
NO:
he may be drinking adequately, may be receiving
adequate fluid via NG feed or TPN, or may be receiving
large volumes with drugs or drug infusions (or a
combination of these). ALLOW PATIENTS TO DRINK IF
AT ALL POSSIBLE.
Hypervolaemic: may need fluid restriction or gentle
diuresis.
YES:
not drinking, has lost, or is losing fluid
So WHY does the patient need fluid?
Maintenance fluid only – patient does not have excess
losses above insensible loss. If no other intake he needs
New surgical booklet Anwar Qais Saadoon Basrah medical college 10
approximately 30ml/kg/24hrs. He may only need part of
this if receiving other fluid. Patients having to fast for over
8-12 hours should be started on IV maintenance fluid.
Replacement of losses, either previous or current. If
losses are predicted it is best to replace these later rather
than give extra fluid in anticipation of losses which may not
occur. This fluid is in addition to maintenance fluid. Check
blood gases.
Resuscitation: The patient is hypovolaemic as a result of
dehydration, blood loss or sepsis and requires urgent
correction of intravascular depletion to correct the defcit
3. How much?
a. Obtain weight (estimate if required). Maintenance fluid
requirement approximately 30ml/kg/24hours.
b. Review recent U&Es, other electrolytes and Hb.
c. Recent events – e.g. fasting, intake, losses, sepsis,
operations, fluid overload. Check fluid balance charts.
Calculate how much loss has to be replaced and work
out which type of fluid has been lost: e.g. GI secretions,
blood, infammatory losses.
Note urine does not need to be replaced unless excessive
(diabetes insipidus, recovering renal failure). Post-op: high
urine output may be due to excess fluid;
low urine output is common and may be normal due to anti-
diuretic hormone release.
Assess fully before giving extra fluid.
4. What type(s) of fluid does my patient need?
New surgical booklet Anwar Qais Saadoon Basrah medical college 11
Maintenance fluid
IV fluid should be given via volumetric pump if a patient is
on fluids for over 6 hours or if the fluid contains
potassium. Always prescribe as ml/hr not ‘x hourly’
bags.
Never give maintenance fluids at more than 100ml/hour.
Table 1: correct fluid rate according to body weight
Weight kg Fluid Requirement in mls/day Rate in ml/hour
35-44 1200 50
45-54 1500 65
55-64 1800 75
65-74 2100 85
≥75 2400 100 (max)
Preferred maintenance fluids: 0.18%saline/4%dextrose
with or without added potassium (KCl 10/ 20 mmol) in
500ml. 1 litre bags are available. This fluid if given at
the correct rate provides all water and Na
/K requirements until the patient can eat and drink or be
fed. Excess volumes of this fluid (or any) fluid may cause
hyponatraemia.
Alternatively 5% dextrose 500ml and 0.9% NaCl 500ml
may be used in a ratio of 2 bags of 5% dextrose to 1 bag
of 0.9% NaCl. Prescribe each bag with added potassium
(KCl 20mmol) if patient has normal or low potassium.
Which Fluid to Choose?
Hypovolemia: primary goal is volume
expansion.
Use the fluid that will put the most volume into
the intravascular space. NS or LR.
Dehydration (= hyperosmolality): primary
goal is free water replacement. Note that
this is not synonymous with hypovolemia.
Use a hypotonic fluid usually 0.45% saline or
D5W.
New surgical booklet Anwar Qais Saadoon Basrah medical college 12
Post-operative patients:
Pain and narcotics can be powerful stimulants
of inappropriate ADH secretion (SIADH)
Giving hypotonic fluids in this setting can (but
usually does not) cause dangerous
hyponatremia.
This makes 0.9 % saline a safer fluid but
realize that it will also deliver free water in the
setting of SIADH.
Crystalloid Resuscitation - what should you do?
Recommendations:
• Colloid should NOT be used as the sole fluid replacement in
resuscitation; Volumes infused should be limited because of side
effects and lack of evidence for their continued use in the acutely ill.
• In severely ill patients – principally use crystalloid and blood products;
Colloid may be used in limited volume to reduce volume of fluids
required or until blood products are available
• In elective surgical patients – replace fluid loss with ‘physiological
Hartmann’s and Ringer’s solutions; Blood products and colloid may
be needed to replace intravascular volume acutely
• Don’t get in between an anaesthetist and a surgeon when the words
colloid and crystalloid are mentioned!
New surgical booklet Anwar Qais Saadoon Basrah medical college 13
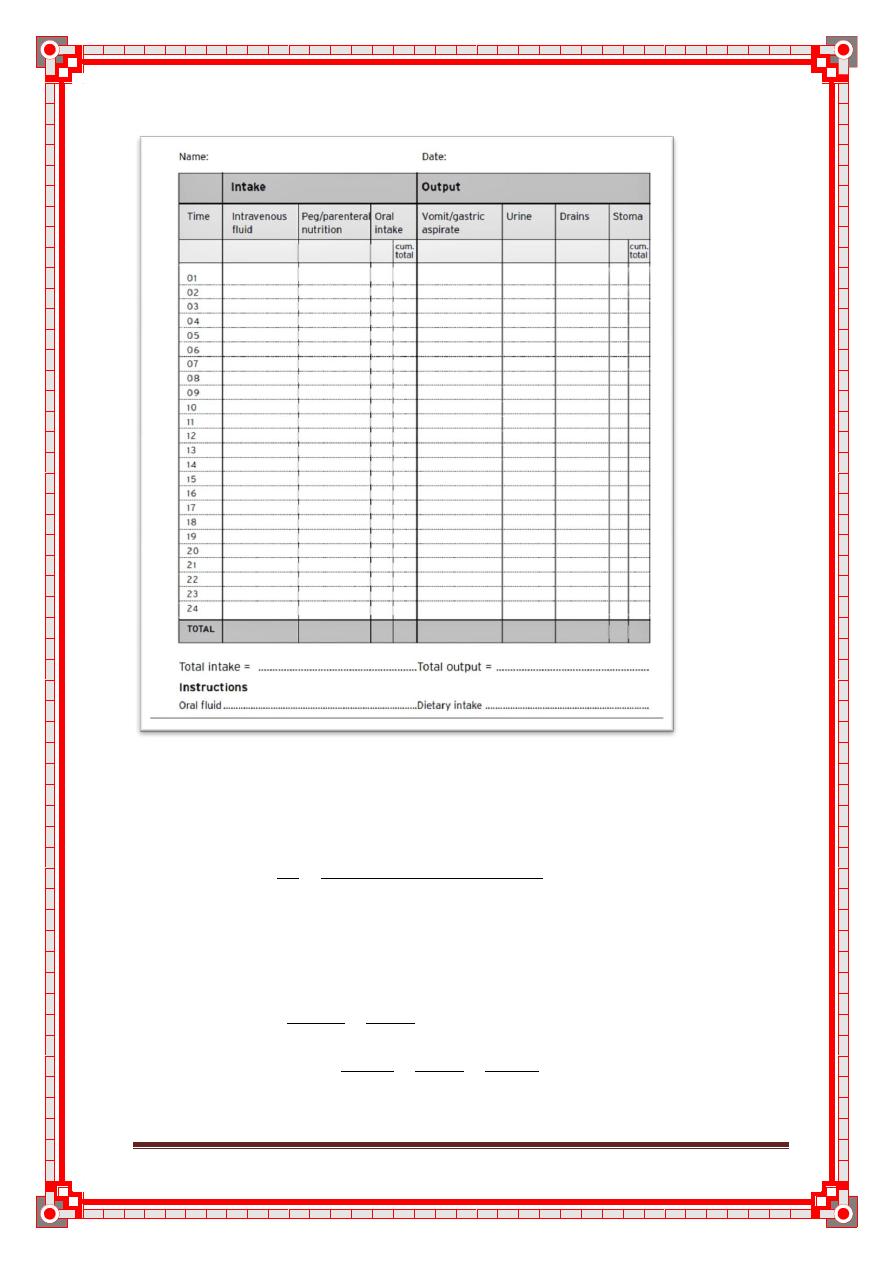
Figure 1: The fluid balance chart
To calculate drip rates / transfusion rates:
To calculate the drip rate (drops / minute)
Drip Rate gtt = Volume to be infused (ml) x Drop Factor (gtt/ml)
min Time (minutes)
1 unit of blood is approximately 400ml in volume
E.g. A unit of blood is prescribed to run over 4 hours; The giving set has a
drop factor of 20 gtt /ml. What is the drip rate (drops /min) ?
Drip rate = 400 ml x 20 gtt ; Drip Rate is drops / minute
4 hour 1ml
Thus Drip Rate = 400ml x 20 gtt x 1 hour
4 hour 1 ml 60 minutes
By multidimensional analysis units are correct (drops / minute)
New surgical booklet Anwar Qais Saadoon Basrah medical college 14
Drip Rate = 100 / 3 = 33 drops / minute
• Drop rate is rounded up or down to the nearest drop
• In the clinical setting to be able to count drops / minute it is sensible to
have a number divisable by 4 - Thus you would set this drip at 32
drops per minute
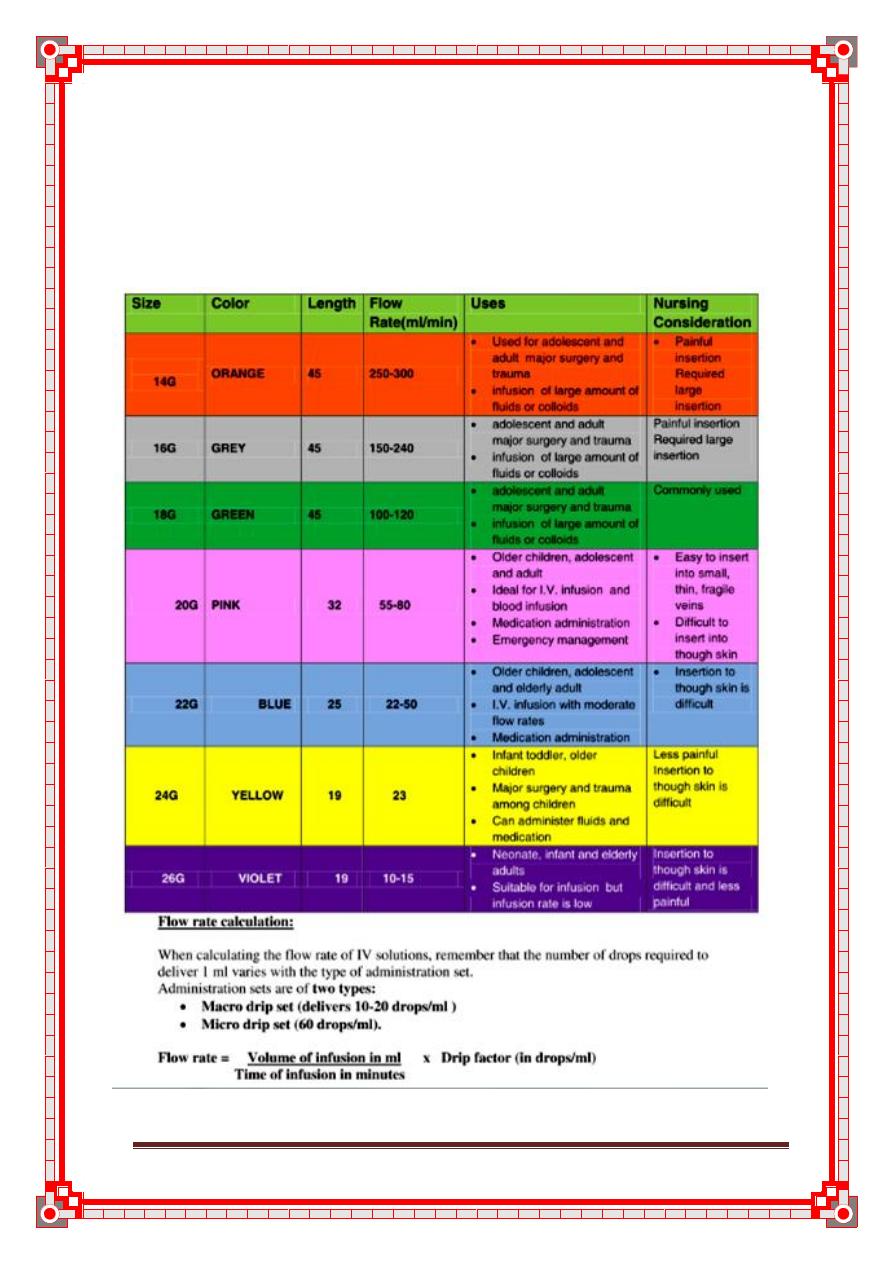
Table 2: sizes of the I.V cannula
New surgical booklet Anwar Qais Saadoon Basrah medical college 15
Electrolyte balance
Sodium balance
Alterations in sodium balance cause fl uid shifts between compartments. The
clinical picture is most often neurologic, due to fl uid shifts within the brain.
Hyponatremia
DEFINITION
< 130 mEq/L.
First steps in hyponatremia: Determine volume status clinically, then
determine plasma osmolality!
Step 1: Determine Plasma Osmolality
Normal osmolality—pseudohyponatremia: Lab artifact due to increased
lipids or plasma proteins → next step; check lipid profi le or possible
multiple myeloma.
High osmolality —pseudohyponatremia: Due to increase of osmolality
active molecules—glucose or mannitol.
Low osmolality—true hyponatremia.
Step 2: Assess Volume Status
Hypovolemia
Euvolemia
Hypervolemia
See below for discussion of each.
HYPONATREMIA WITH HIGH PLASMA OSMOLALITY
(PSEUDOHYPONATREMIA)
CAUSES
Hyperglycemia, either physiologic or due to rapid infusion of glucose or
mannitol will cause increased osmotic pressure that shifts fl uid from the ICF
to the ECF. The total body sodium in this case is normal but has become di-
luted due to the fluid shift.
The expected Na concentration can be calculated as follows: For every 100
mg/dL that glucose is increased over 100 mg/dL, the Na concentration falls
1.6 mEq/L. Remember “sweet 16.”
For example, a patient with a glucose concentration of 500 mg/dL is ex-
pected to have a hyponatremia of around 133.6 mEq/L (4 × 1.6 = 6.4, 140 –
6.4 = 133.6).
New surgical booklet Anwar Qais Saadoon Basrah medical college 16
HYPONATREMIA WITH HYPOTONICITY (TRUE
HYPONATREMIA)
True hyponatremia refl ects excess ingestion of water that overwhelms the
kidneys (either normal or diseased) or due to increased ADH. Hyponatremia
is not due to increased excretion of sodium.
Hypovolemia (dehydration)
Renal cause: Diuretics.
Extrarenal cause: Vomiting, diarrhea, burns, pancreatitis.
Differentiate using urine Na: Urine Na < 20 mEq/L indicates expected
renal retention in the face of hypovolemia, suspect an extrarenal cause.
Urine Na > 20 mEq/L indicates a renal cause.
Hypervolemia
May be from CHF, cirrhosis, or nephrotic syndrome.
Increased thirst and vasopressin.
Edematous state.
Euvolemia
SIADH: Most common cause of normovolemic hyponatremia.
Increased vasopressin release from posterior pituitary or ectopic source
causes decreased renal free water excretion.
Signs and symptoms:
Hypo-osmotic hyponatremia (hyponatremia with hypotonicity).
Inappropriately concentrated urine (urine osmolality > 100 mOsm/
kg).
Normal renal, adrenal, and thyroid function.
Causes:
Neuropsychiatric disorders, malignancies (especially lung), and head
trauma.
Glucocorticoid defi ciency (Addison’s disease)—cortisol defi ciency
causes hypersecretion of vasopressin.
Hypothyroidism—causes decreased CO and glomerular fi ltration rate
(GFR), which leads to increased vasopressin secretion.
Primary polydipsia—usually seen in psychiatric patients who compulsively
drink massive volumes of water.
New surgical booklet Anwar Qais Saadoon Basrah medical college 17
SIGNS AND SYMPTOMS OF (TRUE) HYPONATREMIA
Signs: Decreased reflexes, respiratory depression, seizures, coma.
Symptoms: Nausea/vomiting, headache, lethargy, muscle cramps.
Hypovolemic hyponatremia: Give 0.9% NaCl. Na repletion with saline
isotonic to the patient, in order to avoid rapid changes in ICF volume.
Major complication from rapid correction of chronic hyponatremia is central
pontine myelinolysis.
Hypervolemic hyponatremia: Correct underlying disorder—CHF, liver
or renal failure.
Euvolemic hyponatremia: Raise plasma Na (lower ICF volume)—restrict
water intake.
Hypernatremia
DEFINITION
> 145 mEq/L.
Hypernatremia is always associated with hyperosmolarity. (Note that in the
plasma osmolality equation, Na is the major factor).
CAUSES
Loss of water (dehydration!): Diabetes insipidus, diuretics, sweating, GI
loss, burns, fistulas.
Gain of sodium due to excess mineralocorticoid activity: Primary hyper-
aldosteronism, Cushing’s, renal artery stenosis (hyperreninism), congen-
ital adrenal hyperplasia (will cause concomitant hypokalemia).
If thirst mechanism is intact and water is available, hypernatremia will
not persist. Suspect hypernatremia in the young, elderly, and patients
with altered mental status who may not have access to water.
SYMPTOMS
Thirst.
Restlessness, weakness, delirium.
Hypotension and tachycardia.
Decreased saliva and tears.
Red, swollen tongue.
Oliguria.
New surgical booklet Anwar Qais Saadoon Basrah medical college 18
TREATMENT
Calculate free water defi cit.
If euvolemic: Replace water defi cit with D5W.
If hypovolemic: Use normal saline. Correct one half of water defi cit in
fi rst 24 hours; remaining water defi cit over next 1–2 days.
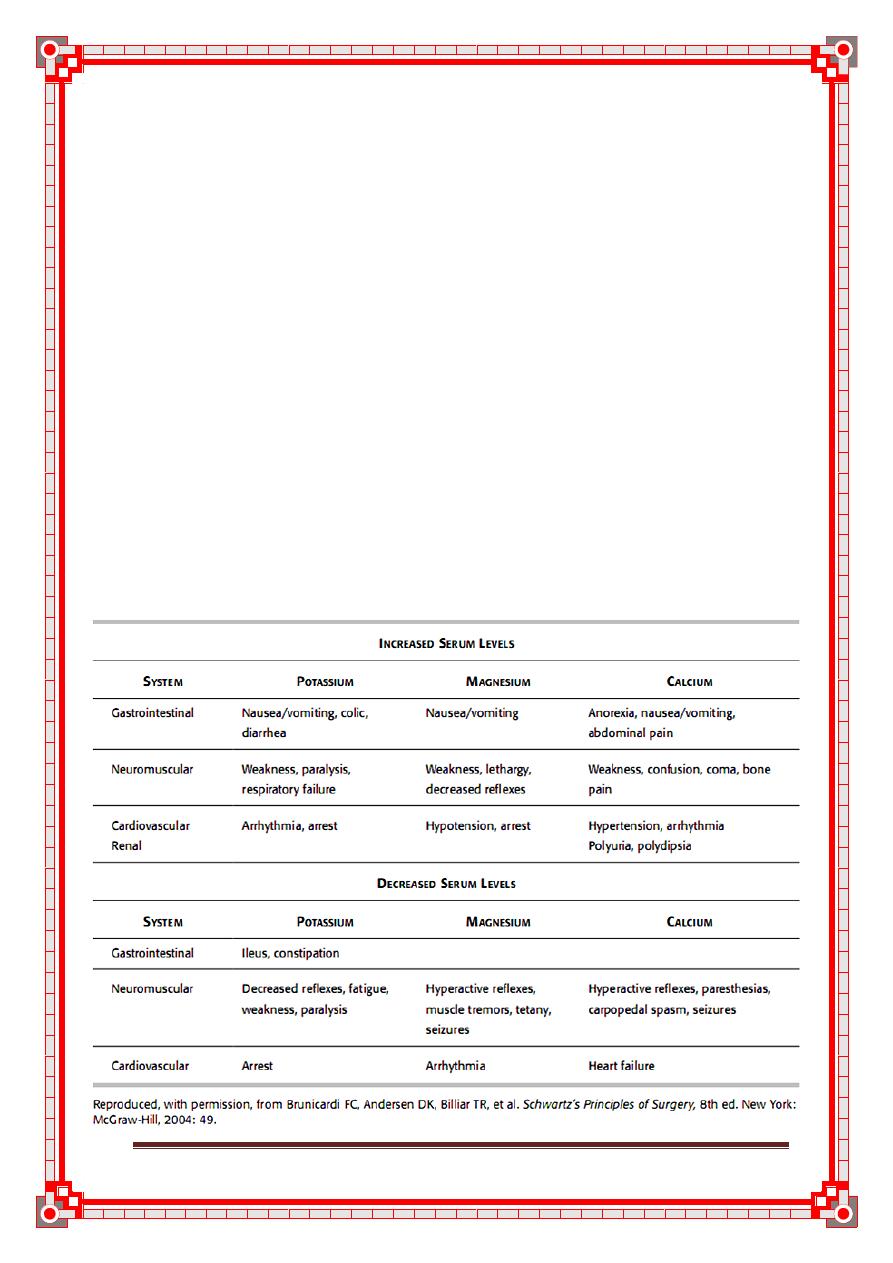
Potassium balance
Ninety-nine percent of K is in ICF. Therefore, small alterations in ex-
tracellular K balance can have signifi cant clinical effects, particularly
impaired electrical signaling in the heart, muscle, and nerve (see Table
3). Proper proportions of K+ and Ca+ must exist for their exchange
across membrane channels that allow electrical conduction to occur.
Cells act as a rapid potassium buffer. Kidney regulates long-term potas-
sium control.
Table 3: Clinical Manifestations of Abnormalities in Potassium, Magnesium,
and Calcium
New surgical booklet Anwar Qais Saadoon Basrah medical college 19
Hypokalemia
DEFINITION
< 3.5 mEq/L.
CAUSES
Most commonly due to excessive renal secretion.
Loss of potassium due to excess mineralocorticoid activity: Primary
hyperaldosteronism, Cushing’s, renal artery stenosis (hyperreninism),
congenital adrenal hyperplasia (will cause concomitant
hypernatremia).
Movement of K into cells due to insulin, catecholamines, alkalemia.
Prolonged administration of K-free parenteral fluids.
Total parenteral hyperalimentation with inadequate K replacement.
Loss in excessive lower GI secretions such as diarrhea, colonic fi
stulas,
VIPoma.
Diuretics.
Signs & symptoms
Electrocardiogram (ECG) Flattened T waves, ST depression, U wave.
Arrhythmias, signs of low voltage.
Treatment
Check Mg level first as hypomagnesemia is commonly associated with
hypokalemia and must be corrected before/along with hypokalemia.
Amount of K to be replaced can be conservatively estimated as: (4.0 –
current K) × 100, in mEq.
Example: if current K is 3.1, give 90 mEq (total, not all at once!!!)
In asymptomatic patient with K > 3.0 mEq/L, oral K replacement may
be sufficient.
No more than 40 mEq should be added to a liter of IV fluid since rapid
K administration can cause fatal arrhythmias.
Rate should not exceed 40 mEq/hr.
May cause a burning sensation if given in peripheral IV. Using low
flow rate of 10 mEq/hr or adding a small amount of lidocaine to the
solution can decrease discomfort.
New surgical booklet Anwar Qais Saadoon Basrah medical college 20
Hyperkalemia
DEFINITION
> 5 mEq/L.
CAUSES
Commonly due to renal failure.
Rarely found when renal function is normal and usually causes a tran-
sient hyperkalemia, due to cellular shifts: Potassium spillage from cells
in severe injury; cells take up hydrogen ions in exchange for intracellu-
lar potassium, acting as a buffer in states of acidosis.
Drugs: Angiotensin-converting enzyme (ACE) inhibitors, potassium-
sparing diuretics.
Iatrogenic causes: Penicillin G contains 1.7 mEq K per one million
units, KCl added to maintenance fl uids, blood transfusion with old
batch of packed red blood cells (RBCs) where K may have leaked out of
cells, overtreatment of hypokalemia.
Digoxin toxicity can cause severe hyperkalemia by blocking the so-
dium–potassium–adenosine triphosphatase (ATPase) pump.
Hypoaldosteronism.
Pseudohyperkalemia: Can result when RBCs lyse in the test tube and
release potassium. This is a lab error: Repeat test before treating!
SIGNS AND SYMPTOMS
Cardiac effects are most signifi cant. Confirm hyperkalemia and obtain an
ECG.
ECG:
Early: Peaked T waves wide QRS, ST depression.
Late: Disappearance of T waves, heart block, sine wave ominous for
impending fatal arrhythmia, cardiac arrest.
GI: Nausea, vomiting, intermittent intestinal colic, diarrhea.
TREATMENT (IN ORDER OF IMPORTANCE)
Ten percent calcium gluconate 1 g IV—monitor ECG. Calcium tem-
porarily suppresses cardiac arrhythmias by stabilizing the cardiac mem-
brane and should be administered fi rst. Does not affect potassium load.
Lower extracellular K+ (acute treatment): Albuterol, insulin with glu-
cose or sodium bicarbonate promote cellular reuptake of K—transient
relief of hyperkalemia.
Kayexalate—cation exchange resin. As opposed to above measures,
which immediately protect against dangers of high potassium, this actu-
ally removes the potassium from the body.
Dialysis (last resort).
New surgical booklet Anwar Qais Saadoon Basrah medical college 21
How does Ca+ help with hyperkalemia?
It stabilizes the membrane potential of cardiac muscle, which would
abnormally fi re in the presence of high potassium. It does not actually have
any effect on the amount of K+ present.
Calcium balance
Normal: 1,000–1,200 mg—most is in the bone in the form of phosphate
and carbonate.
Normal daily intake: 1–3 g.
Most excreted via stool (–200 mg via urine).
Normal serum level: 8.5–10.5 mg/dL (total calcium).
Half of this is nonionized and bound to plasma protein.
If hypocalcemia is seen on laboratory report, fi rst correct for low albumin:
Corrected Calcium = 0.8 (Normal Albumin – Observed Albumin) +
Observed Calcium
If corrected calcium falls within normal range, no action is required.
Ionized calcium is the most accurate measure of calcium, but labs re-
port total calcium.
An additional nonionized fraction (5%) is bound to other substances in
the ECF.
Ratio of ionized to nonionized Ca is related to pH:
Acidosis causes increase in ionized fraction.
Alkalosis causes decrease in ionized fraction.
Hypocalcemia
DEFINITION
< 8 mg/dL.
CAUSES
Acute pancreatitis.
Massive soft-tissue infections (necrotizing fasciitis).
Acute/chronic renal failure.
Pancreatic/small bowel fistulas.
Hypoparathyroidism (common after parathyroid or thyroid surgery).
Hypoproteinemia (often asymptomatic, corrected calcium will fall
within normal range).
Severe depletion of magnesium.
Severe alkalosis may elicit symptoms in patient with normal serum
levels because there is a decrease in the ionized fraction of total serum
calcium.
New surgical booklet Anwar Qais Saadoon Basrah medical college 22
SIGNS AND SYMPTOMS
Numbness and tingling of fingers, toes, and around mouth.
Increased refl exes.
Chvostek’s sign: Tapping over the facial nerve in front of the tragus of
the ear causes ipsilateral twitching.
Trousseau’s sign: Carpopedal spasm following inflation of
sphygmomanometer cuff to above systolic blood pressure for several
minutes.
Muscle and abdominal cramps.
Convulsions.
ECG—prolonged QT interval.
TREATMENT
IV Ca gluconate or Ca chloride.
Monitor QT interval on ECG.
Hypercalcemia
DEFINITION
> 15 mg/dL.
CAUSES
Hyperparathyroidism.
Cancer (especially breast, multiple myeloma).
Drugs (e.g., thiazides).
SIGNS AND SYMPTOMS
Fatigue, weakness, anorexia, weight loss, nausea, vomiting.
Somnambulism, stupor, coma.
Severe headache, pain in the back and extremities, thirst,
polydipsia, polyuria.
Death.
TREATMENT
Vigorous volume repletion with salt solution—dilutes Ca and
increases urinary Ca excretion:
May be augmented with furosemide.
Definitive treatment of acute hypercalcemic crisis in patients
with hyperparathyroidism is immediate surgery.
Treat underlying cause.
New surgical booklet Anwar Qais Saadoon Basrah medical college 23
Acid-Base homeostasis
1. pH of body fluids:
-arterial blood- pH 7, 35-7, 45
-venous blood-pH 7, 35
-intracellular fluid-pH 7, 0
-gastric juice- pH 2, 0
-small intestine juice- pH 8, 0
-urine- pH 4, 5-8 ,0 based on diet and metabolic state
2. The body has 3 ways of maintaining a normal pH range:
-chemical buffer system (acts within seconds)
a) carbonic acid / bicarbonate
b) phosphate buffer
c) protein buffer
-respiratory controls
a) acts within minutes
b) important in compensating for metabolic acidosis or alkalosis
c) permits elimination of the volatile acid ( bicarbonate acid )
-renal mechanisms
a) acts within hours or days
b) compensate for respiratory acidosis or alkalosis
c) eliminate fixed acids from the body (metabolic acids generated in
the body that are eliminated only in the urine).
New surgical booklet Anwar Qais Saadoon Basrah medical college 24
Chapter II
Blood transfusion and
blood transfusion reaction
Topics
Introduction
Blood and blood products
Whole blood
Packed red cells
Fresh-frozen plasma
Cryoprecipitate
Platelets
Prothrombin complex concentrates
Autologous blood
Indications for blood transfusion
Transfusion trigger
Blood groups and cross-matching
ABO system
Rhesus system
Transfusion reactions
Complications of blood transfusion
Complications from a single transfusion
Complications from massive transfusion
Management of transfusion reactions
Transfusion reactions algorithm
25
25
25
25
26
26
26
26
27
27
27
27
27
28
28
29
29
29
30
32
New surgical booklet Anwar Qais Saadoon Basrah medical college 25
Introduction
The transfusion of blood and blood products has become commonplace
since the first successful transfusion in 1829
Although the incidence of severe transfusion reactions and
infections is now very low, in recent years it has become apparent
hat there is an immunological price to be paid for the transfusion
of heterologous blood, which leads to increased morbidity and
decreased survival in certain population groups (trauma, malignancy).
Supplies are also limited and, therefore, the use of blood
and blood products must always be judicious and justifiable in
terms of clinical need.
Blood and blood products
Blood is collected from donors who have been previously
screened to exclude any donor whose blood may have the poten-
tial to harm the patient or to prevent possible harm that donat-
ing a unit of blood may have on the donor. In the UK, up to
450ml of blood is drawn, a maximum of three times a year. Each
unit is tested for evidence of hepatitis B, hepatitis C, human
immunodeficiency virus (HIV)-1, HIV-2 and syphilis. Donations
are leucodepleted as a precaution against variant Creutzfeldt–
jakob disease (this may also reduce the immunogenicity of the
transfusion). The ABO and Rhesus D blood group is determined,
as well as the presence of irregular red cell antibodies. The blood
is then processed into sub-components.
Whole blood
Whole blood is now rarely available in civilian practice as it is an
ineffective use of the limited resource; however, whole blood
transfusion has significant advantages over packed cells as it is
coagulation factor rich and, if fresh, more metabolically active
than stored blood.
Packed red cells
Packed red blood cells are cells that are spun down and concentrated.
Each unit is approximately 330ml and has a haematocrit
of 50–70%. Packed cells are stored in a SAG-M solution
(saline–adenine–glucose–mannitol) to increase their shelf-life to
5 weeks at 2–6∞C. (Older storage regimens included storage in
CPD – citrate–phosphate–dextrose solutions – giving cells a
shelf-life of 2–3 weeks).
New surgical booklet Anwar Qais Saadoon Basrah medical college 26
Fresh-frozen plasma
Fresh-frozen plasma (FFP) is rich in coagulation factors; it is
removed from fresh blood and stored at –40 to –50∞C with a 2-
year shelf-life. It is the first-line therapy in the treatment of
coagulopathic haemorrhage (see below). Rhesus D-positive FFP
may be given to a Rhesus D-negative woman.
Cryoprecipitate
Cryoprecipitate is a supernatant precipitate of FFP and is rich in
factor VIII and fibrinogen. It is stored at –30∞C with a 2-year
shelf-life. It is given in low-fibrinogen states or in cases of factor
VIII deficiency.
Platelets
Platelets are supplied as a pooled platelet concentrate contain-
ing about 250 × 109
cells per litre. Platelets are stored on a
special agitator at 20–24∞C and have a shelf-life of only 5 days.
Platelet transfusions are given to patients with thrombocyto-
penia or with platelet dysfunction who are bleeding or under-
going surgery.
Patients are increasingly presenting on anti-platelet therapy
such as aspirin or clopidogrel for reduction of cardiovascular risk.
Aspirin therapy rarely poses a problem but control of haemor-
rhage on the more potent platelet inhibitors can be extremely dif-
ficult. Patients on clopidogrel who are actively bleeding and
undergoing major surgery may require almost continuous infusion
of platelets during the course of the procedure. Arginine vaso-
pressin or its analogues [e.g. desmopressin acetate (DDAVP)]
have also been used in this patient group, although with limited
success.
Prothrombin complex concentrates
Prothrombin complex concentrates (PCCs) are highly purified
concentrates prepared from pooled plasma. They contain factors
II, IX and X; factor VII may be included or produced separately.
PCCs are indicated for the emergency reversal of anti-coagulant
(warfarin) therapy in uncontrolled haemorrhage.
New surgical booklet Anwar Qais Saadoon Basrah medical college 27
Autologous blood
It is possible for patients undergoing elective surgery to pre-
donate their own blood up to 3 weeks before surgery for retrans-
fusion during the operation. Similarly, during surgery blood can
be collected in a cell saver; this washes and collects red blood
cells, which can then be returned to the patient.
Indications for blood transfusion
Blood transfusions should be avoided if possible and many
previous uses of blood and blood products are now no longer
considered appropriate. The indications for blood transfusion are
as follows:
1-
acute blood loss, to replace circulating volume and maintain
oxygen delivery;
2-
perioperative anaemia, to ensure adequate oxygen delivery
during the perioperative phase;
3-
symptomatic chronic anaemia without haemorrhage or
impending surgery.
Transfusion trigger
Historically, patients were transfused to achieve a haemoglobin
level of >10gdl
–1
. This has now been shown to be not only
unnecessary but also associated with increased morbidity and
mortality compared with lower target values. A haemoglobin level of 6gdl
–1
is acceptable in patients who are not bleeding, not about to undergo major
surgery and not symptomatic. There is some controversy as to the optimal
haemoglobin level in some patient groups such as those with cardiovascular
disease, sepsis and traumatic brain injury. Although conceptually a high-
er haemoglobin level improves oxygen delivery, there is little clinical
evidence at this stage to support higher levels in these groups.
Blood groups and cross-matching
Human red blood cells have many different antigens on their cell
surface. Two groups of antigens are of major importance in surgi-
cal practice – the ABO and Rhesus systems.
ABO system
These are strongly antigenic and are associated with naturally
occurring antibodies in the serum. The system consists of three
allelic genes – A, B and O – which control the synthesis of
enzymes that add carbohydrate residues to cell surface glycopro-
teins. Expression of the A and B genes results in specific residues
being added whereas the O gene is an amorph and does not trans-
New surgical booklet Anwar Qais Saadoon Basrah medical college 28
form the glycoprotein.
The system allows for six possible genotypes although there
are only four phenotypes . Naturally occurring
antibodies are found in the serum of those lacking the corres-
ponding antigen.Blood group O is the universal donor type as it
contains no antigens to provoke a reaction. Conversely, group AB
individuals are ‘universal recipients’ and can receive any ABO
blood type as they have no circulating antibodies.
Rhesus system
The Rhesus D [Rh(D)] antigen is strongly antigenic and is
present in approximately 85% of the population in the UK.
Antibodies to the D antigen are not naturally present in the
serum of the remaining 15% of individuals but their formation
may be stimulated by the transfusion of Rh-positive red cells or
they may be acquired during delivery of a Rh(D)-positive baby.
Table 4:
Perioperative red blood cell transfusion criteria
Haemoglobin level (gdl
–1
) Indication
<6 Probably will benefit from transfusion
6–8 Transfusion unlikely to be of benefit in the
absence of bleeding or impending surgery
>8 No indication for transfusion
Acquired antibodies are capable of crossing the placenta
during pregnancy and, if present in a Rh(D)-negative mother,
they may cause severe haemolytic anaemia and even death
(hydrops fetalis) in a Rh(D)-positive fetus in utero.
The other minor blood group antigens may be associated with
naturally occurring antibodies or they may stimulate the forma-
tion of antibodies on relatively rare occasions.
Transfusion reactions
If antibodies present in the recipient’s serum are incompatible with
the donor’s cells, a transfusion reaction will result. This usually
takes the form of an acute haemolytic reaction. Severe immune-
related transfusion reactions caused by ABO incompatibility result
in severe and potentially fatal complement-mediated intravascular
haemolysis and multiple organ failure. Transfusion reactions from
New surgical booklet Anwar Qais Saadoon Basrah medical college 29
other antigen systems are usually milder and self-limiting.
Febrile transfusion reactions are non-haemolytic and are
usually caused by a graft-versus-host response from leucocytes in
transfused components. There is fever, chills or rigors. The blood
transfusion should be stopped immediately. This form of transfu-
sion reaction is rare with leuco-depleted blood.
Complications of blood transfusion
Complications from blood transfusion can be categorised as those
arising from a single transfusion and those related to massive
transfusion.
Complications from a single transfusion
Complications from a single transfusion include:
1- incompatibility haemolytic transfusion reaction;
2- febrile transfusion reaction
3- allergic reaction;
4- infection:
A- bacterial infection (usually as a result of faulty storage);
B- hepatitis;
C- HIV;
D- malaria;
5- air embolism;
6- thrombophlebitis;
7- transfusion-related acute lung injury (usually from FFP).
Complications from massive transfusion
Complications from massive transfusion include:
1- coagulopathy;
2- hypocalcaemia;
3- hyperkalaemia;
4- hypokalaemia;
5- hypothermia.
Additionally, patients who receive repeated transfusions over
long periods of time (e.g. patients with thalassaemia) may
developiron overload. (Each transfused unit of red blood cells
contains approximately 250mg of elemental iron.)
New surgical booklet Anwar Qais Saadoon Basrah medical college 30
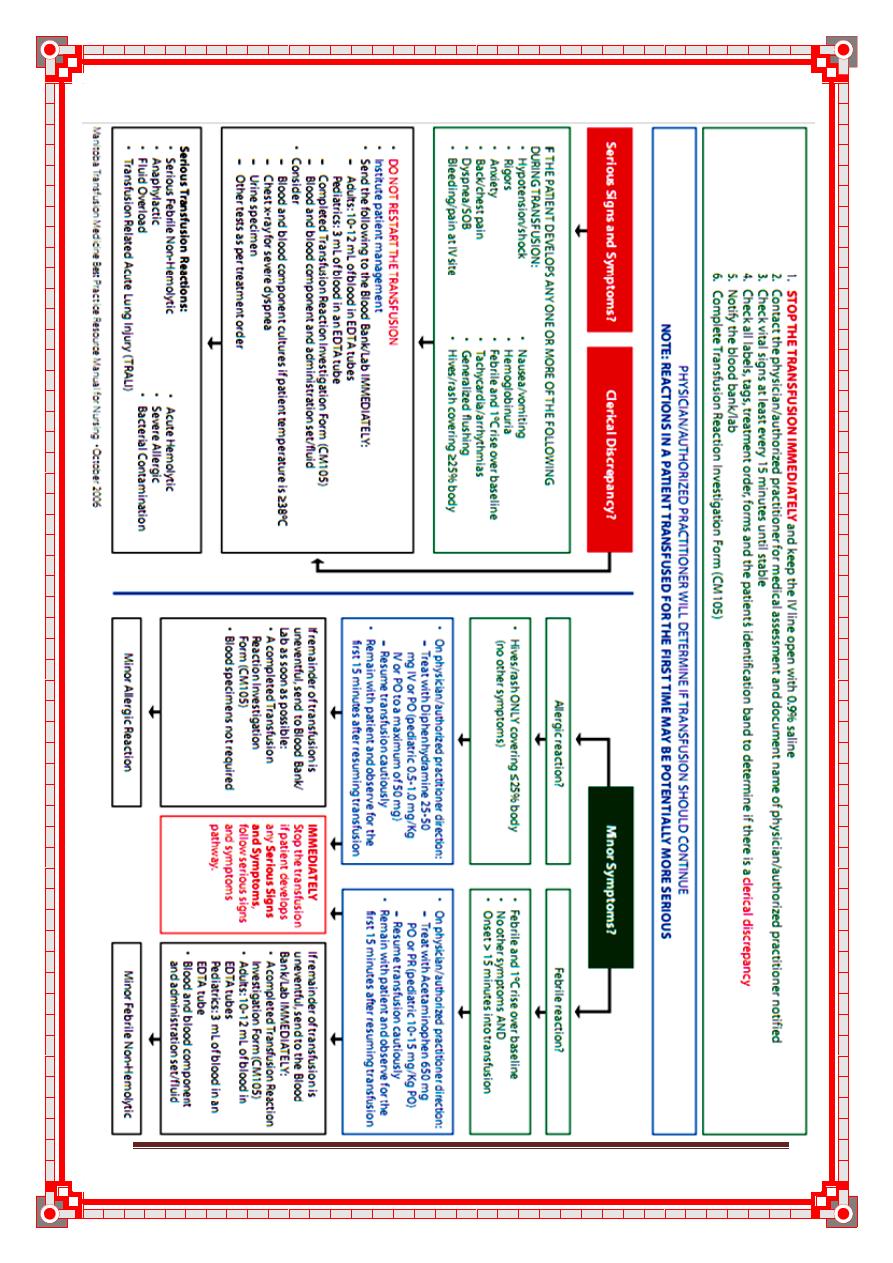
Management of transfusion reactions:
Continuous monitoring of vital signs during generalized anesthesia may
prevent acute circulatory (volume) overload, but it may not detect early signs
of other reactions (eg, acute hemolytic transfusion reactions).
The onset of red-colored urine in a transfused patient should raise the
question of a hemolytic transfusion reaction. When performing checks to
confirm that the correct blood was transfused to the correct patient,
centrifuge a urine sample to determine whether the red color represents
hematuria or hemoglobinuria Rapid test to distinguish hematuria from
hemoglobinuria. The onset of red urine during or shortly after a blood
transfusion may represent hemoglobinuria In addition, the onset of abnormal
bleeding/generalized oozing during surgery in a transfused patient should
raise the question of a hemolytic transfusion reaction with DIC.
Acute hemolytic reactions (antibody mediated)
Immediately discontinue the transfusion while maintaining venous access for
emergency management.
Anticipate hypotension, renal failure, and DIC. Prophylactic measures to
reduce the risk of renal failure may include low-dose dopamine (1-5
mcg/kg/min), vigorous hydration with crystalloid solutions (3000 mL/m2/24
h), and osmotic diuresis with 20% mannitol (100 mL/m2/bolus, followed by
30 mL/m2/h for 12 h). If DIC is documented and bleeding requires
treatment, transfusions of frozen plasma, pooled cryoprecipitates for
fibrinogen, and/or platelet concentrates may be indicated.
Acute hemolytic reactions (nonantibody mediated)
The transfusion of serologically compatible, although damaged, RBCs
usually does not require rigorous management. Diuresis induced by an
infusion of 500 mL of 0.9% sodium chloride per hour, or as tolerated by the
patient, until the intense red color of hemoglobinuria ceases is usually
adequate treatment.
Febrile, nonhemolytic reactions:
Usually, fever resolves in 15-30 minutes without specific treatment. If fever
causes discomfort, oral acetaminophen (325-500 mg) may be administered.
Avoid aspirin because of its prolonged adverse effect on platelet function.
Allergic reactions:
Diphenhydramine is usually effective for relieving pruritus that is associated
with hives or a rash. The route (oral or intravenous) and the dose (25-100
mg) depend on the severity of the reaction and the weight of the patient.
New surgical booklet Anwar Qais Saadoon Basrah medical college 31
Anaphylactic reactions
A subcutaneous injection of epinephrine (0.3-0.5 mL of a 1:1000 aqueous
solution) is standard treatment. If the patient is sufficiently hypotensive to
raise the question of the efficacy of the subcutaneous route, epinephrine (0.5
mL of a 1:10,000 aqueous solution) may be administered intravenously.
Although no documented evidence exists that intravenous corticosteroids are
beneficial for the management of acute anaphylactic transfusion reactions,
theoretical considerations cause most clinicians to include an infusion of
hydrocortisone or prednisolone if an immediate response to epinephrine does
not occur.
TRALI (Transfusion Related Acute Lung Injury)
Immediately discontinue the transfusion while preserving venous access.
Patients with mild episodes should respond to oxygen administered by nasal
catheter or mask. If shortness of breath persists after oxygen administration,
transfer the patient to an intensive care setting where mechanical ventilation
can be administered. In the absence of signs of acute volume overload or
cardiogenic pulmonary edema, diuretics are not indicated.No evidence exists
that corticosteroids or antihistamines are beneficial.
Treat complications with specific supportive measures.
Circulatory (volume) overload
Move the patient to a sitting position, and administer oxygen to facilitate
breathing.The most specific treatment is discontinuing the transfusion and
removing the excessive fluid.If practical, the unit of blood component being
transfused may be lowered to reverse the flow and to decrease intravascular
volume by a controlled phlebotomy.Less urgent situations may be managed
by a parenteral or oral diuretic (eg, furosemide).If the patient has
symptomatic anemia requiring additional transfusions of RBCs, select
concentrated (ie, CPDA-1-anticoagulated) red cells (hematocrit = 80-85%).
Avoid red cell components diluted with saline additives (ie, AS-1).
Bacterial contamination (sepsis)
Immediately discontinue the transfusion, including all tubing, filters, and
administration sets, and save the transfusion materials for cultures, while
preserving venous access. After appropriate blood cultures have been
obtained, initiate treatment with intravenous broad-spectrum antibiotics. If a
microbiologic stain or a culture of the contents of the transfused product
identifies an organism, the initial broad-spectrum antibacterial approach may
be modified accordingly.
New surgical booklet Anwar Qais Saadoon Basrah medical college 32
Transfusion reactions algorithm
New surgical booklet Anwar Qais Saadoon Basrah medical college 33
Chapter III
Post Operative complication
Topics
Common Post-operative Complications
General post -operative complications
Post-operative fever
Haemorrhage
Infection
Disordered wound healing
Surgical injury
Respiratory complication
Common urinary problems
Thrombo-embolism
34
34
35
36
36
37
37
38
39
40
New surgical booklet Anwar Qais Saadoon Basrah medical college 34
Common Post-operative Complications
Post-operative complications may either be general or specific to the type of
surgery undertaken.
The highest incidence of post-operative complications is between 1 and 3
days after the operation. However, specific complications occur in the
following distinct temporal patterns: early post-operative, several days
after the operation, throughout the post-operative period, and in the late
post-operative period
General post -operative complications
A- Immediate:
Primary haemorrhage: either starting during surgery or
following post-operative increase in blood pressure - replace
blood loss and may require return to theatre to re-explore
wound.
Basal atelectasis: minor lung collapse.
Shock: blood loss, acute myocardial infarction,
pulmonary embolism or septicaemia.
Low urine output: inadequate fluid replacement intra- and
post-operatively.
B- Early:
Acute confusion: exclude dehydration and sepsis
Nausea and vomiting: analgesia or anaesthetic-related;
paralytic ileus
Fever
Secondary haemorrhage: often as a result of infection
Pneumonia
Wound or anastomosis dehiscence
Deep vein thrombosis (DVT)
Acute urinary retention
Urinary tract infection (UTI)
Post-operative wound infection
Bowel obstruction due to fibrinous adhesions
Paralytic Ileus
New surgical booklet Anwar Qais Saadoon Basrah medical college 35
C- Late:
Bowel obstruction due to fibrous adhesions
Incisional hernia
Persistent sinus
Recurrence of reason for surgery, e.g. malignancy
o Post-operative fever
In total, 40% of patients develop pyrexia after major
surgery; however, in 80% of cases no particular cause is
found. Pyrexia does not necessarily imply sepsis. The
inflammatory response to surgical trauma may manifest as
temperature. In spite of this, a focus of infection must
always be sought if a patient develops anything more than a
slight pyrexia.
Days 0 to 2:
Mild fever (T <38 °C) (Common)
Atelectasis of microalveoli : the collapsed lung may
become secondarily infected
Tissue damage and necrosis at operation site
Haematoma
Persistent fever (T >38 °C)
Specific infections related to the surgery, e.g. biliary
infection post biliary surgery, UTI post-urological surgery
Blood transfusion or drug reaction
Days 3-5:
superficial and deep wound infection
Bronchopneumonia
Sepsis
Drip site infection or phlebitis
Abscess formation, e.g. subphrenic or pelvic, depending on
the surgery involved
DVT
Day 5: chest infection including viral respiratory tract infec-
tion, urinary tract infection and thrombophlebitis;
New surgical booklet Anwar Qais Saadoon Basrah medical college 36
After 5 days:
Specific complications related to surgery, e.g. bowel
anastomosis breakdown, fistula formation, wound infection,
, intracavitary collections and abscesses;
• infected intravenous cannula sites, DVTs,
transfusion reactions, wound haematomas, atelectasis and
drug reactions,which may also cause pyrexia of non-
infective origin. Patients with persistent pyrexia need a
thorough review.
Relevant investigations include full blood count, urine
culture if urinary tract infection is suspected, sputum
microscopy, chest radiography if indicated and blood
cultures
After the first week
Wound infection
Distant sites of infection, e.g. UTI
DVT, pulmonary embolus (PE)
o Haemorrhage :
It is classified into :
1-Primary :occurs during surgery or immediately after it .
2-Reactionaly :occurs within 24 hr after surgery .
3-Secondary hemorrhage :occur 7days postoperatively. It is mainly
caused by infection.
o Infection
Infectious complications are the main causes of post-operative
morbidity in abdominal surgery.
Wound infection: most common form is superficial wound infection
occurring within the first week presenting as localised pain, redness and
slight discharge usually caused by skin staphylococci.
Cellulitis and abscesses:
Usually occur after bowel-related surgery
Most present within first week but can be seen as late as
third post-operative week, even after leaving hospital
Present with pyrexia and spreading cellulitis or abscess
New surgical booklet Anwar Qais Saadoon Basrah medical college 37
Cellulitis is treated with antibiotics
Abscess requires suture removal and probing of wound but
deeper abscess may require surgical re-exploration. The
wound is left open in both cases to heal by secondary
intention
Gas gangrene is uncommon and life-threatening.
Wound sinus is a late infectious complication from a deep chronic
abscess that can occur after apparently normal healing. Usually needs
re-exploration to remove non-absorbable suture or mesh, which is often
the underlying cause.
o Disordered wound healing
Most wounds heal without complications and healing is not impaired in
the elderly unless there are specific adverse factors or complications.
Factors which may affect healing rate are:
A- Poor blood supply.
B- Excess suture tension.
C- Long term steroids.
D- Immunosuppressive therapy.
E- Radiotherapy.
F- Severe rheumatoid disease.
G- Malnutrition and vitamin deficiency.
D
D
i
i
s
s
o
o
r
r
d
d
e
e
r
r
w
w
o
o
u
u
n
n
d
d
s
s
h
h
e
e
a
a
l
l
i
i
n
n
g
g
i
i
n
n
c
c
l
l
u
u
d
d
e
e
:
:
1- Wound dehiscence and burst abdomen.
2-Incisional hernia
3-Stretched or ragged scar.
4-Hypertrophic scar .
5-Keloid .
o Surgical injury
Unavoidable tissue damage to nerves may occur during many
types of surgery, e.g. facial nerve damage during total
parotidectomy, impotence following prostate surgery or recurrent
laryngeal nerve damage during thyroidectomy.
New surgical booklet Anwar Qais Saadoon Basrah medical college 38
o Respiratory complications
Occur in up to 15% of general anaesthetic and major surgery and
include:
1- Atelectasis (alveolar collapse):
Caused when airways become obstructed, usually by
bronchial secretions. Most cases are mild and may go
unnoticed
Symptoms are slow recovery from operations, poor colour,
mild tachypnoea, tachycardia and low-grade fever
Prevention is by pre-and post-operative physiotherapy
In severe cases, positive pressure ventilation may be
required
2- Pneumonia:
requires antibiotics, physiotherapy.
3- Aspiration pneumonitis:
Sterile inflammation of the lungs from inhaling gastric
contents
Presents with history of vomiting or regurgitation with rapid
onset of breathlessness and wheezing. Non-starved patient
undergoing emergency surgery is particularly at risk
May help avoid this by crash induction technique and use of
oral antacids or metoclopramide
Mortality is nearly 50% and requires urgent treatment with bronchial
suction, positive pressure ventilation, prophylactic antibiotics and
IV steroids
4- Acute respiratory distress syndrome
New surgical booklet Anwar Qais Saadoon Basrah medical college 39
o Common urinary problems :
A- Urinary retention: common immediate post-operative
complication that can often be dealt with conservatively with
adequate analgesia. If this fails may need catheterisation.
B- UTI: very common, especially in women, and may not present
with typical symptoms. Treat with antibiotics and adequate fluid
intake.
C- Acute renal failure
o Complications of bowel surgery
A- Delayed return of function:
Temporary disruption of peristalsis: may complain of
nausea, anorexia and vomiting and usually appears with the
re-introduction of fluids. Often described as ileus
More prolonged extensive form with vomiting and
intolerance to oral intake called adynamic obstruction and
needs to be distinguished from mechanical obstruction. If
involves large bowel usually described as pseudo-
obstruction. Diagnosed by instant barium enema
B- Early mechanical obstruction: may be caused by twisted or
trapped loop of bowel or adhesions occurring approximately 1
week after surgery. May settle with nasogastric aspiration plus IV
fluids or progress and require surgery.
C- Late mechanical obstruction: adhesions can organise and persist,
commonly causing isolated episodes of small bowel obstruction
months or years after surgery. Treat as for early form.
D- Anastomotic leakage or breakdown:
Small leaks are common causing small localised abscesses with
delayed recovery of bowel function. Usually resolves with IV
fluids and delayed oral intake but may need surgery.
New surgical booklet Anwar Qais Saadoon Basrah medical college 40
Major breakdown causes generalised peritonitis and progressive
sepsis needing surgery for peritoneal toilet, and antibiotics. Local
abscess can develop into a fistula.
o Thrombo-embolism
Major cause of complications and death after surgery. DVT is very
commonly related to grade of surgery.
Many cases are silent but present as swelling of leg, tenderness of calf
muscle and increased warmth with calf pain on passive dorsiflexion of
foot.
Diagnosis is by venography or Doppler ultrasound.
Pulmonary embolism:
Classically presents with sudden dyspnoea and
cardiovascular collapse with pleuritic chest pain, pleural rub
and haemoptysis. However, smaller PEs are more common
and present with confusion, breathlessness and chest pain
Diagnosis is by ventilation/perfusion scanning and/or
pulmonary angiography or dynamic CT
Management: intravenous heparin or subcutaneous low molecular
weight heparin for 5 days plus oral warfarin.
New surgical booklet Anwar Qais Saadoon Basrah medical college 41
Chapter IV
Surgical Drains
Topics
Indication of surgical drain
Principles of drains
Complications of surgical drain
Types of drains
Open passive drains
Closed passive drains
Closed active drains
Advantages of the closed drains
General guidance
Removal of surgical drain
42
42
42
43
43
43
44
44
44
45
New surgical booklet Anwar Qais Saadoon Basrah medical college 42
Indication of surgical drain
Drains may be used for several reasons:
of fluid, blood, pus, air
(e.g.drainage of a subphrenic abscess, removal of a pneumothorax).
surgery to the bile duct) or potential abnormal fluids or air (e.g. bloody
fluid in the pelvis after rectal surgery).
-
threatening complications (e.g. neck drains after thyroid surgery, chest
drains after chest trauma in patients undergoing general anaesthesia).
Principles of drains
1) Must not be too rigid
2) Must not be too soft
3) Not of irritant material
4) Wide bore enough to function
5) Left for sufficient time so that when drain removed there is minimal
drainage
6) When used prophylactically e.g. duodenal stump or anastomotic
leak, the drain should be left in situ as long as the danger of perforation
exists, i.e. for 10 days, until a fibrous track is formed which will act as
an external fistula (with a safety-valve action).
7) To minimize the infection rate: drain from a separate wound, use
closed system and the shortest duration used.
The complications associated with abdominal drains include:
• trauma during insertion;
• failure to drain because of incorrect placement or blockage;
• complications caused by disconnection;
• sepsis at drain sites;
• drain site metastases;
• erosion by the drain of adjacent tissue and perforation of
abdominal viscera
• Drains do not always drain the substance required as expected and
may give a false sense of security, e.g. failure to drain bleeding after
thyroid surgery or failure to drain faecal fluid after anastomotic leakage
in rectal surgery. There is no place for outline use of drains after surgery
unless there is a clear indication.
New surgical booklet Anwar Qais Saadoon Basrah medical college 43
The quantity and character of drain fluid can be used to identify
any abdominal complication resulting in fluid leakage (e.g. bile or
pancreatic fluid) or bleeding. The excess loss of body fluids
through the drain should be replaced by additional intravenous
fluids. Blood loss through the drain should be investigated for the
source. Any underlying coagulopathy should be excluded by
checking the coagulation profile and platelet count. Angiography
may be useful to identify the source of blood loss.
The absence of blood in the drain does not exclude heavy
postoperative bleeding. If the patient’s blood pressure and urine
output are lower than expected the wound needs checking for a
collection. Inspection, palpation and ultrasound can all help
identify a developing haematoma.
Types of drains
Materials used include latex rubber (e.g. T tubes), silastic rubber (e.g.
long-term urinary catheters), polypropylene (e.g. abdominal drains),
polyurethane (e.g. nasogastric tubes).
Open passive drains
These provide a conduit around which secretions may flow
Closed passive drains
These drain fluid by gravity (siphon effect) or by capillary flow
New surgical booklet Anwar Qais Saadoon Basrah medical college 44
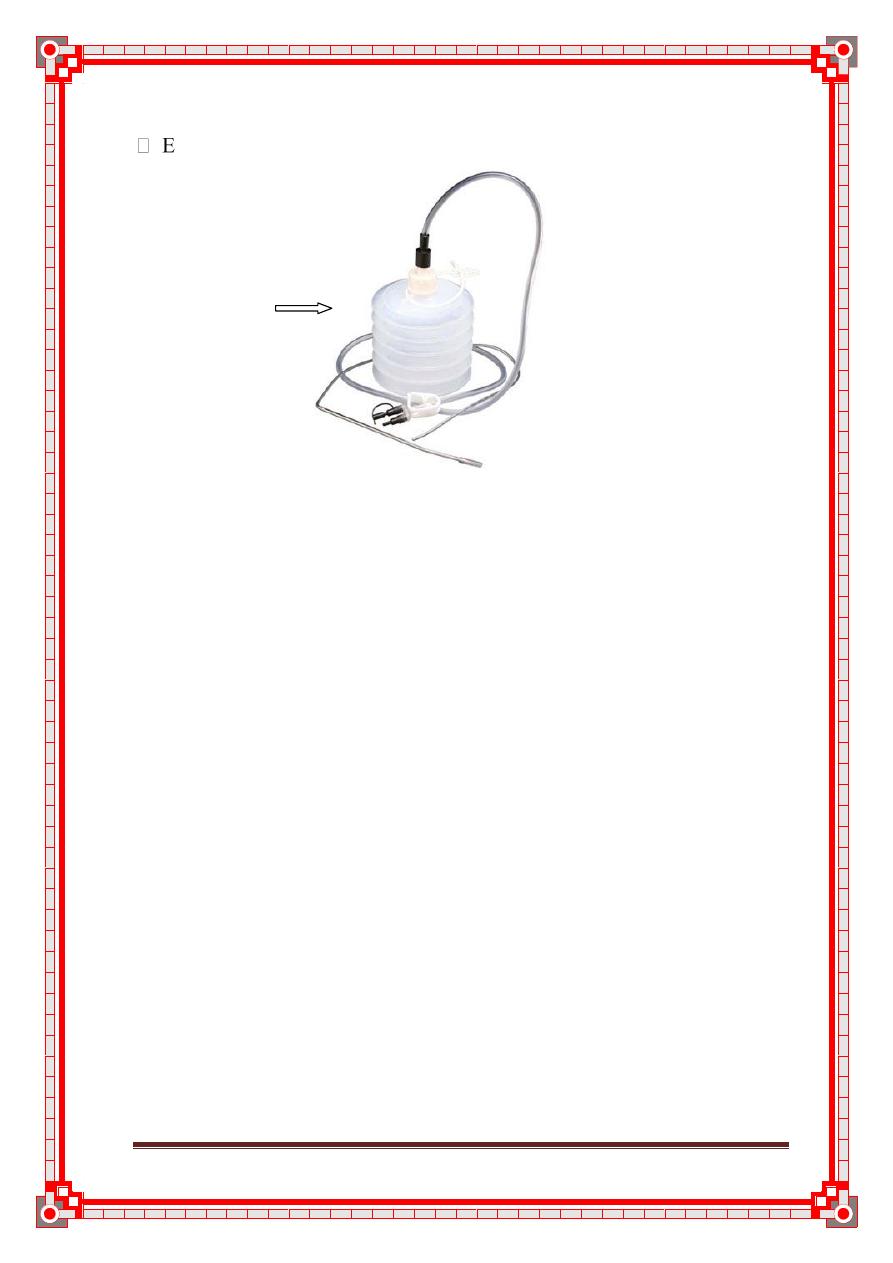
Closed active drains
These generate active suction (low or high pressure)
xudrains®,Redivac drains ®, Minivac ®, Jackson Pratt drains (after
pelvic or breast surgery)
Redivac drains
Advantages of the closed drains
Can calculate the amount.
No risk of infections.
No need for frequent dressing.
General guidance
If active, the drain can be attached to a suction source (and set at a prescribed
pressure).
Ensure the drain is secured (dislodgement is likely to occur when transferring
patients after anaesthesia).
Dislodgement can increase the risk of infection and irritation to the
surrounding skin.
Accurately measure and record drainage output.
Monitor changes in character or volume of fluid. Identify any complications
resulting in leaking fluid (particularly, for example, bile or pancreatic
secretions) or blood.
Use measurements of fluid loss to assist intravenous replacement of fluids.
Drains are used to drain purulent collections, to prevent accumulation of
blood or to indicate the possibility of leaking surgical anastomoses.
In clean surgery, such as joint replacement, blood
collected in drains can be transfused back into the patient pro-
vided that an adequate volume (>150ml) is collected rapidly
(<12 hours) and that a specifically designed drain and filter
system is used.
New surgical booklet Anwar Qais Saadoon Basrah medical college 45
The use of surgical drains has decreased in recent years as the
evidence for their benefits has been questioned. They can result
in complications and so should be used carefully.
Removal of surgical drain:
Generally, drains should be removed once the drainage has stopped or
becomes less than about 25 ml/day. as they are a potential track for
contamination and infection into a wound. Drainage of bile or
faecal matter indicates disruption of a biliary or intestinal anastomosis.
Drains can be 'shortened' by withdrawing them gradually (typically by
2 cm per day) and so, in theory, allowing the site to heal gradually.
Usually drains that protect postoperative sites from leakage form a
tract and are kept in place longer (usually for about a week).
Warn the patient that there may be some discomfort when the drain is
pulled out.
Consider the need for pain relief prior to removal.
Place a dry dressing
New surgical booklet Anwar Qais Saadoon Basrah medical college 46
Chapter V
Suture types
Topics
Suture types
Suture sizes
Surgical needles
Surgical instrument
47
49
49
49
New surgical booklet Anwar Qais Saadoon Basrah medical college 47
Suture types
Sutures come either as monofilament or braided:
* Monofilament sutures cause less reaction than do braided sutures, but
require more ties to assure an adequate maintenance of the knot compared to
braided suture. Monofilament sutures are usually non- absorbable.
* Braided suture usually incites a greater inflammatory response but,
requires fewer ties to maintain the knot
integrity. These include silk, cotton and Mersilene.
The strength of the sutures varies according to their size, which can be
determined by a uniformly applied number. For example, a 6-0 suture is
more delicate and has less strength than a 4-0 suture.
Sutures come as either absorbable or non absorbable:
Absorbable sutures are made of materials which are broken down in tissue
after a given period of time, which depending on the material can be from ten
days to eight weeks. They are used therefore in many of the internal tissues
of the body. In most cases, three weeks is sufficient for the wound to close
firmly. The suture is not needed any more, and the fact that it disappears is an
advantage, as there is no foreign material left inside the body and no need for
the patient to have the sutures removed.
Absorbable sutures were originally made of the intestines of sheep, the so
called catgut. However, the majority of absorbable sutures are now made of
synthetic polymer fibers, which may be braided or monofilament; these offer
numerous advantages over gut sutures, notably ease of handling, low cost,
low tissue reaction, consistent performance and guaranteed non-toxicity.
Natural Absorbable Sutures
1. Catgut Sutures- Plain catgut and Chromic catgut sutures
Synthetic Absorbable Sutures
2. Polyglycolic Acid Sutures (Vicryl) (PGA sutures)- coated and braided
suture
3. Polyglactin 910 Sutures (PGLA sutures)- coated and braided suture
4. Poliglecaprone Sutures (Monocryl) (PGCL sutures)- monofilament suture
5. Polydioxanone Sutures (PDS)- monofilament suture
New surgical booklet Anwar Qais Saadoon Basrah medical college 48
Non absorbable sutures
are made of materials which are not metabolized by the body, and are used
therefore either on skin wound closure, where the sutures can be removed
after a few weeks, or in some inner tissues in which absorbable sutures are
not adequate. This is the case, for example, in the heart and in blood vessels,
whose rhythmic movement requires a suture which stays longer than three
weeks, to give the wound enough time to close. Other organs, like the
bladder, contain fluids which make absorbable sutures disappear in only a
few days, too early for the wound to heal. There are several materials used
for non absorbable sutures. The most common is a natural fiber, silk, which
undergoes a special manufacturing process to make it adequate for its use in
surgery. Other non-absorbable sutures are made of artificial fibers, like
polypropylene, polyester or nylon; these may or may not have coatings to
enhance their performance characteristics. Finally, stainless steel wires are
commonly used in orthopedic surgery and for sternal closure in cardiac
surgery.
Non-Absorbable Sutures:
1. Silk Sutures – Black Braided suture
2. Polypropylene sutures (Prolene)- monofilament suture
3. Nylon suture or Polyamide sutures- monofilament suture
4. Polyester sutures- coated and braided suture
New surgical booklet Anwar Qais Saadoon Basrah medical college 49
SUTURE SIZES:
The size of suture material is measured by its width or diameter and is vital
to proper wound closure. As a guide the following are specific areas of their
usage:
1. 1-0 and 2-0: Used for high stress areas requiring strong retention, i.e. deep
fascia repair
2. 3-0: Used in areas requiring good retention, i.e. scalp, torso, and hands
3. 4-0: Used in areas requiring minimal retention, i.e. extremities. Is the
most common size utilized for
superficial wound closure.
4. 5-0: Used for areas involving the face, nose, ears, eyebrows, and eyelids.
5. 6-0: Used on areas requiring little or no retention. Primarily used for
cosmetic effects.
SURGICAL NEEDLES:
There are a variety of needles for wound closure. Curved needles have two
basic configurations; tapered and cutting. For wound and laceration care, the
reverse cutting needle is used almost exclusively. It is made in such a way
that the outer edge is sharp so as to allow for smooth and atraumatic
penetration of tough skin and fascia. Tapered needles are used on soft tissue,
such as bowel and subcutaneous tissue, or when the smallest diameter hole is
desired.
SURGICAL INSTRUMENTS:
It is not necessary to have large numbers of instruments for emergency
wound care. Wounds and lacerations can be managed with the following
instruments:
1.
NEEDLE HOLDERS:
Needle holders come in various sizes and shapes, but
for most lacerations a
standard size 4" will complete the task. For larger, deeper wound closures a
larger needle and needle holder may be required.
2.
FORCEPS:
Grasping and controlling tissue with forceps is essential to
proper suture placement. However, whenever force is applied to skin or other
tissues, inadvertent damage to cells can occur if an improper instrument or
New surgical booklet Anwar Qais Saadoon Basrah medical college 50
technique is used. Be gentle when grasping tissue, and never fully close the
jaws on the skin.
3.
SCISSORS:
There are three types of scissors that are useful in minor
wound care.
a.
IRIS SCISSORS
: Iris scissors are predominantly used to assist in wound
debridement and revision. These scissors are very sharp and are appropriate
in situations that require very fine control. They are very delicate and are not
recommended for cutting sutures. However, when very small sutures require
removal they can be use.
b.
DISSECTION SCISSORS
: Used for heavier tissue revision as necessary for
wound undermining.
c.
SUTURE REMOVAL SCISSORS:
Standard 6-inch, single blunt-tip, suture
scissors are most useful for cutting sutures, adhesive tape, and other dressing
materials. Because of their size and bulk, these scissors are very durable and
practical.
4.
HEMOSTATS
: Hemostats have three functions in minor wound care:
clamping small blood vessels for
hemorrhage control, grasping and securing fascia during debridement, and
are an excellent tool for
exposing, exploring and visualizing deeper areas of the wound.
5.
KNIFE HANDLES AND BLADES:
The knife handle holds the blade and is
used in the debridement
and excisions during wound revision. Common blades are the #10 blade
(used for large excisions), #15 blade (small, versatile and well suited for
precise debridement and wound revision), and the #11 blade (ideal for
incision and drainage of superficial abscesses and the removal of very small
sutures).
New surgical booklet Anwar Qais Saadoon Basrah medical college 51
Chapter VI
Shock
Topics
Introduction
Classification of shock
Severity of shock
pitfalls
Consequence of shock
Resuscitation of shock
Fluid therapy
Vasopressor and Inotropic support
Monitoring
52
52
54
56
57
58
58
60
60
New surgical booklet Anwar Qais Saadoon Basrah medical college 52
Introduction
Shock is a systemic state of low tissue perfusion, which is inade-
quate for normal cellular respiration. With insufficient delivery of
oxygen and glucose, cells switch from aerobic to anaerobic
metabolism. If perfusion is not restored in a timely fashion, cell
death ensues.
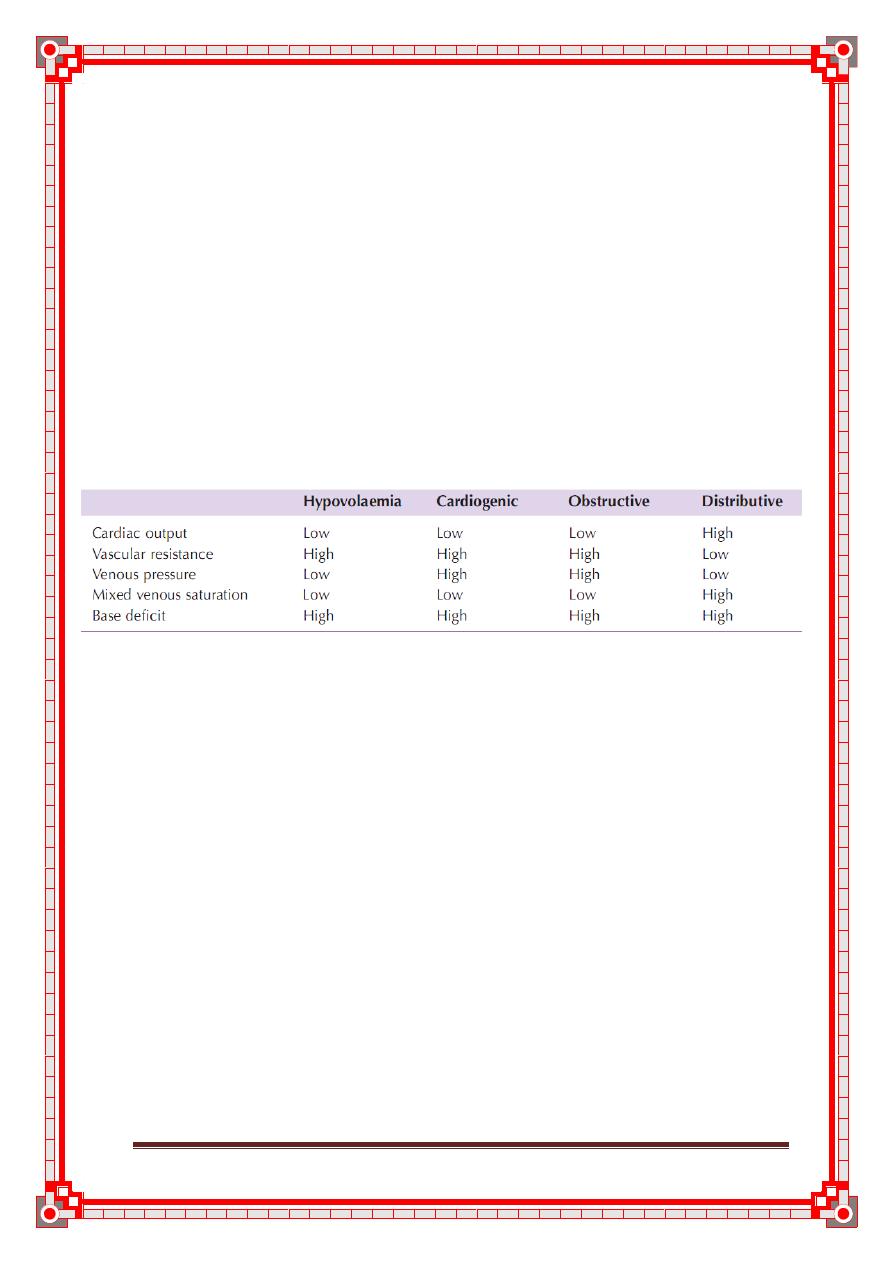
Classification of shock
There are numerous ways to classify shock but the most common
and clinically applicable way is that based on the initiating mechanism .
All states are characterised by systemic tissue hypoperfusion
and different states may coexist within the same patient.
Hypovolaemic shock
Hypovolaemic shock is caused by a reduced circulating volume.
Hypovolaemia may be due to haemorrhagic or non-haemorrhagic causes.
Non-haemorrhagic causes include poor fluid intake (dehydration) and
excessive fluid loss because of vomiting, diarrhoea, urinary loss (e.g.
diabetes), evaporation and ‘third-spacing’,in which fluid is lost into the
gastrointestinal tract and interstitial spaces, as for example in bowel
obstruction or pancreatitis.Hypovolaemia is probably the most common form
of shock and is to some degree a component of all other forms of shock.
Absolute or relative hypovolaemia must be excluded or treated in the
management of the shocked state, regardless of cause.
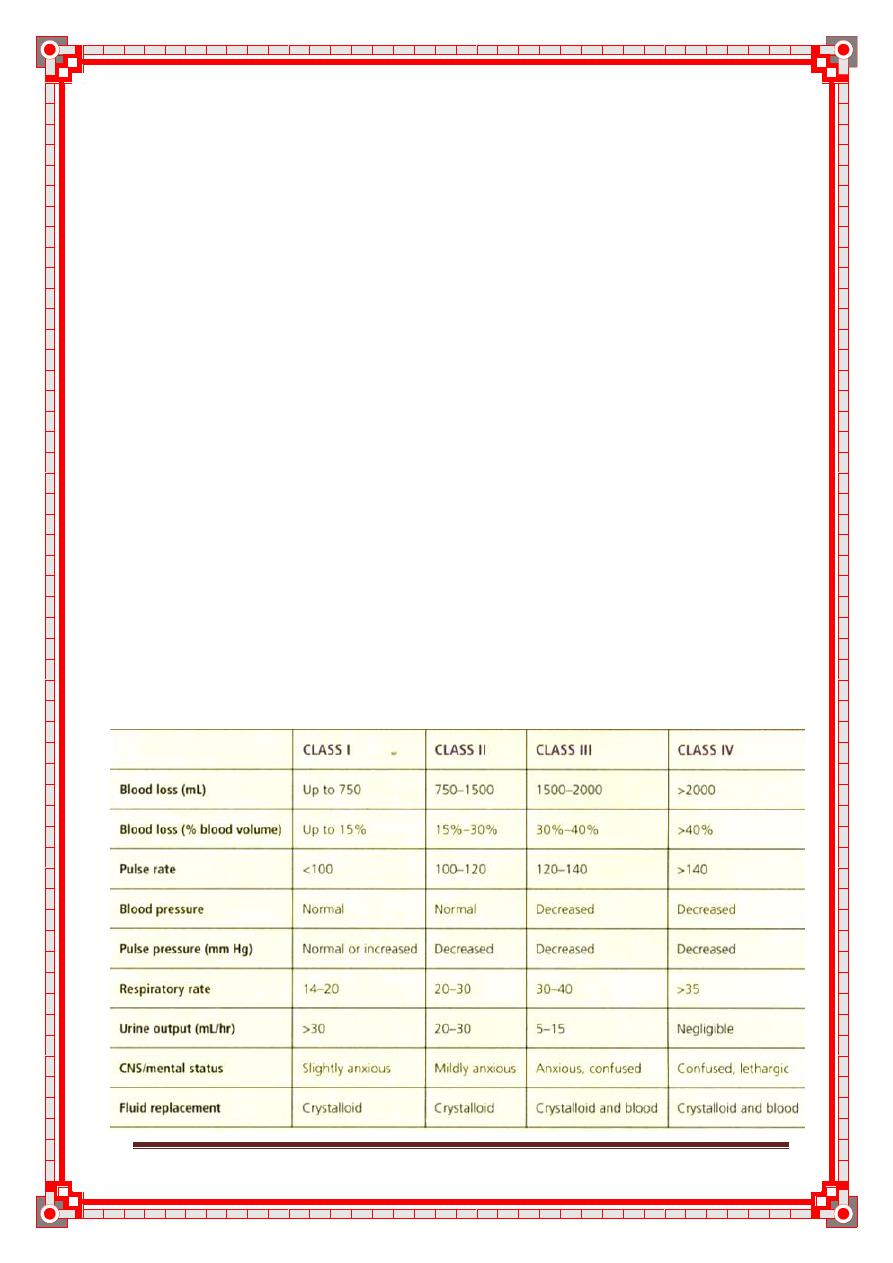
Table 5: Estimated blood loss based on initial patient presentation
New surgical booklet Anwar Qais Saadoon Basrah medical college 53
Cardiogenic shock
Cardiogenic shock is due to primary failure of the heart to pump
blood to the tissues. Causes of cardiogenic shock include myocar-
dial infarction, cardiac dysrhythmias, valvular heart disease, blunt
myocardial injury and cardiomyopathy. Cardiac insufficiency may
also be caused by myocardial depression resulting from endogenous factors
(e.g. bacterial and humoral agents released in
sepsis) or exogenous factors, such as pharmaceutical agents or
drug abuse. Evidence of venous hypertension with pulmonary or
systemic oedema may coexist with the classic signs of shock.
Obstructive shock
In obstructive shock there is a reduction in preload because of
mechanical obstruction of cardiac filling. Common causes of
obstructive shock include cardiac tamponade, tension pneu-
mothorax, massive pulmonary embolus and air embolus. In each
case there is reduced filling of the left and/or right sides of the
heart leading to reduced preload and a fall in cardiac output.
Distributive shock
Distributive shock describes the pattern of cardiovascular
responses characterising a variety of conditions including septic
shock, anaphylaxis and spinal cord injury. Inadequate organ per-
fusion is accompanied by vascular dilatation with hypotension,
low systemic vascular resistance, inadequate afterload and a
resulting abnormally high cardiac output.
In anaphylaxis, vasodilatation is caused by histamine release,
whereas in high spinal cord injury there is failure of sympathetic
outflow and adequate vascular tone (neurogenic shock). The
cause in sepsis is less clear but is related to the release of bacterial
products (endotoxins) and the activation of cellular and humoral
components of the immune system. There is maldistribution of
blood flow at a microvascular level with arteriovenous shunting
and dysfunction of the cellular utilisation of oxygen.
In the later phases of septic shock there is hypovolaemia from
fluid loss into the interstitial spaces and there may be concomi-
tant myocardial depression, which complicates the clinical
picture .
New surgical booklet Anwar Qais Saadoon Basrah medical college 54
Endocrine shock
Endocrine shock may present as a combination of hypovolaemic,
cardiogenic and distributive shock. Causes of endocrine shock
include hypo- and hyperthyroidism and adrenal insufficiency.
Hypothyroidism causes a shock state similar to that of neurogenic
shock as a result of disordered vascular and cardiac responsive-
ness to circulating catecholamines. Cardiac output falls because
of low inotropy and bradycardia. There may also be an associated
cardiomyopathy. Thyrotoxicosis may cause a high-output cardiac failure.
Adrenal insufficiency leads to shock as a result of hypo-
volaemia and a poor response to circulating and exogenous cate-
cholamines. Adrenal insufficiency may result from pre-existing
Addison’s disease or it may be a relative insufficiency caused by a
pathological disease state such as systemic sepsis.
Table 6: cardiovascular and metabolic charachterstic of shock
Severity of shock
Compensated shock
As shock progresses the body’s cardiovascular and endocrine
compensatory responses reduce flow to non-essential organs to
preserve preload and flow to the lungs and brain. In compensated
shock there is adequate compensation to maintain the central
blood volume and preserve flow to the kidneys, lungs and brain.
Apart from a tachycardia and cool peripheries (vasoconstriction,
circulating catecholamines) there may be no other clinical signs
of hypovolaemia.
However, this cardiovascular state is only maintained by
reducing perfusion to the skin, muscle and gastrointestinal tract.
There is a systemic metabolic acidosis and activation of humoral
and cellular elements within the underperfused organs. Although
clinically occult, this state will lead to multiple organ failure and
death if prolonged because of the ischaemia–reperfusion effect
described above. Patients with occult hypoperfusion (metabolic
New surgical booklet Anwar Qais Saadoon Basrah medical college 55
acidosis despite normal urine output and cardiorespiratory vital
signs) for more than 12 hours have a significantly higher mortality rate,
infection rate and incidence of multiple organ failure.
Decompensation
Further loss of circulating volume overloads the body’s compen-
satory mechanisms and there is progressive renal, respiratory
and cardiovascular decompensation. In general, loss of around
15% of the circulating blood volume is within normal compen-
satory mechanisms. Blood pressure is usually well maintained
and only falls after 30–40% of the circulating volume has been
lost.
Mild shock
Initially there is tachycardia, tachypnoea and a mild reduction in
urine output and the patient may exhibit mild anxiety. Blood
pressure is maintained although there is a decrease in pulse pres-
sure. The peripheries are cool and sweaty with prolonged capil-
lary refill times (except in septic distributive shock).
Moderate shock
As shock progresses, renal compensatory mechanisms fail, renal
perfusion falls and urine output dips below 0.5mlkg
–1
h
–1
.
There is further tachycardia and now the blood pressure starts to fall.
Patients become drowsy and mildly confused.
Severe shock
In severe shock there is profound tachycardia and hypotension.
Urine output falls to zero and patients are unconscious with
laboured respiration.
New surgical booklet Anwar Qais Saadoon Basrah medical college 56
pitfalls
The classic cardiovascular responses described are not
seen in every patient. It is important to recognise the limitations
of the clinical examination and to recognise patients who are in
shock despite the absence of classic signs.
Capillary refill
Most patients in hypovolaemic shock will have cool, pale peripheries with
prolonged capillary refill times; however, the actual capillary refill time
varies so much in adults that it is not a specific marker of whether a patient is
shocked, and patients with short capillary refill times may be in the early
stages of shock.
In distributive (septic) shock the peripheries will be warm and
capillary refill will be brisk despite profound shock.
Tachycardia
Tachycardia may not always accompany shock. Patients who are
on β-blockers or who have implanted pacemakers are unable to
mount a tachycardia. A pulse rate of 80 in a fit young adult who
normally has a pulse rate of 50 is very abnormal. Furthermore, in
some young patients with penetrating trauma, when there is
haemorrhage but little tissue damage, there may be a paradoxical
bradycardia rather than tachycardia accompanying the shocked
state.
Blood pressure
It is important to recognise that hypotension is one of the last signs
of shock. Children and fit young adults are able to maintain blood
pressure until the final stages of shock by dramatic increases in
stroke volume and peripheral vasoconstriction. These patients can
be in profound shock with a normal blood pressure.
Elderly patients who are normally hypertensive may present
with a ‘normal’ blood pressure for the general population but be
hypovolaemic and hypotensive relative to their usual blood pres-
sure. β-Blockers or other medications may prevent a tachycardic
response. The diagnosis of shock may be difficult unless one is
alert to these pitfalls.
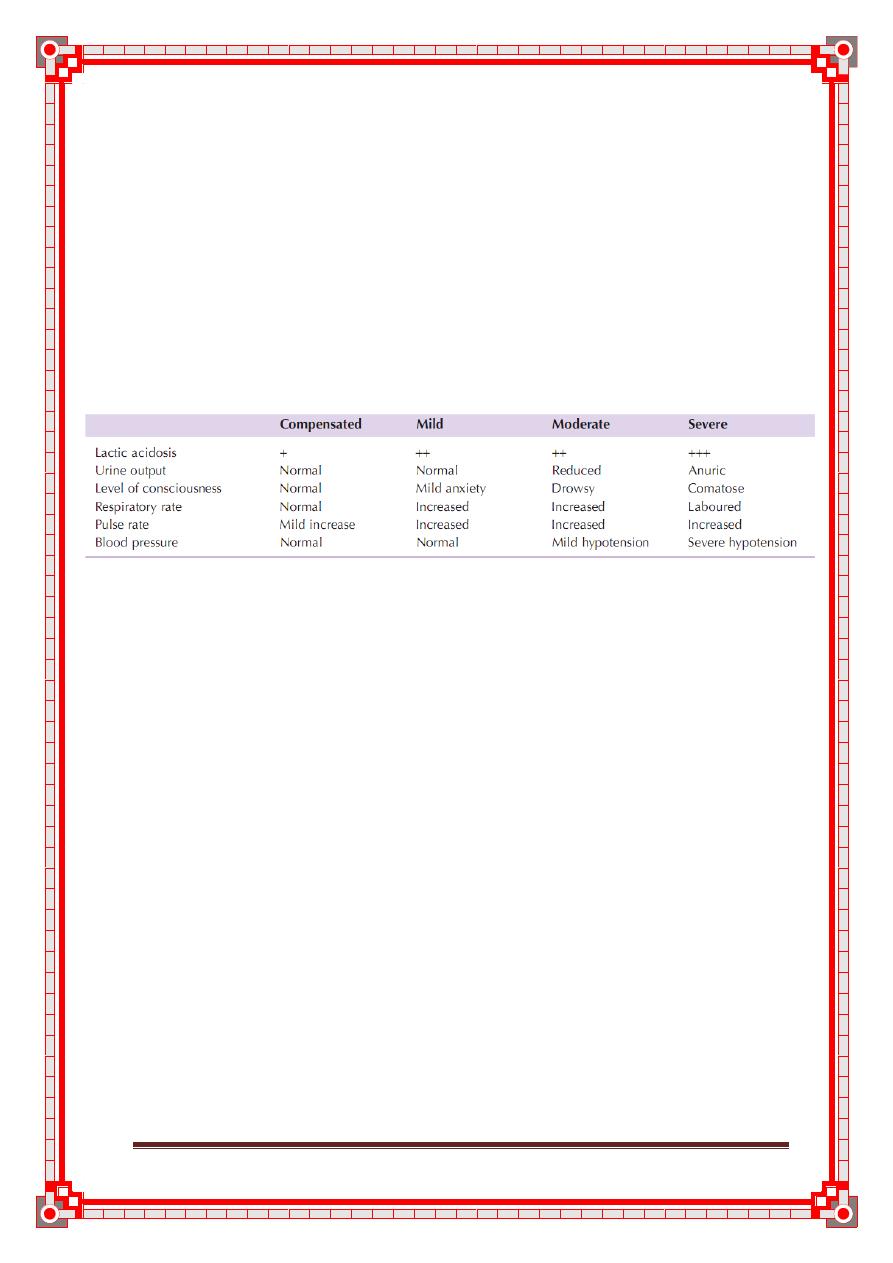
New surgical booklet Anwar Qais Saadoon Basrah medical college 57
Consequences
Unresuscitatable shock
Patients who are in profound shock for a prolonged period of time
become ‘unresuscitatable’. Cell death follows from cellular
ischaemia, and the ability of the body to compensate is lost.
There is myocardial depression and loss of responsiveness to fluid
or inotropic therapy. Peripherally there is loss of the ability to
maintain systemic vascular resistance and further hypotension
ensues. The peripheries no longer respond appropriately to vaso-
pressor agents. Death is the inevitable result.
Table 7: Clinical feature of shock
This stage of shock is the combined result of the severity of the
insult and delayed, inadequate or inappropriate resuscitation in
the earlier stages of shock. When patients present in this late
stage and have minimal responses to maximal therapy it is impor-
tant that the futility of treatment is recognised and that valuable
resources are not wasted.
Multiple organ failure
As techniques of resuscitation have improved, more and more
patients are surviving shock. When intervention is timely and the
period of shock is limited, patients may make a rapid, uncompli-
cated recovery; however, the result of prolonged systemic
ischaemia and reperfusion injury is end-organ damage and
multiple organ failure.
Multiple organ failure is defined as two or more failed organ
systems . There is no specific treatment for multiple
organ failure. Management is by supporting organ systems with
ventilation, cardiovascular support and haemofiltration/dialysis
until there is recovery of organ function. Multiple organ failure
currently carries a mortality rate of 60%. Thus, prevention is vital
by early aggressive identification and reversal of shock.
New surgical booklet Anwar Qais Saadoon Basrah medical college 58
RESUSCITATION
Immediate resuscitation manoeuvres for patients presenting in
shock are to ensure a patent airway and adequate oxygenation
and ventilation. Once ‘airway’ and ‘breathing’ are assessed and
controlled, attention is directed to cardiovascular resuscitation.
Conduct of resuscitation
Resuscitation should not be delayed in order to definitively diag-
nose the source of the shocked state; however, the timing and
nature of resuscitation will depend on the type of shock and the
timing and severity of the insult. Rapid clinical examination will
provide adequate clues to make an appropriate first determina-
tion, even if a source of bleeding or sepsis is not immediately iden-
tifiable. If there is initial doubt about the cause of shock it is safer
to assume the cause is hypovolaemia and begin with fluid resusci-
tation, followed by an assessment of the response.
In patients who are actively bleeding (major trauma, aortic
aneurysm rupture, gastrointestinal haemorrhage) it is counter-
productive to institute high-volume fluid therapy without con-
trolling the site of haemorrhage. Increasing blood pressure merely
increases bleeding from the site, and fluid therapy cools the
patient and dilutes available coagulation factors. Thus, operative
haemorrhage control should not be delayed and resuscitation
should proceed in parallel with surgery.
Conversely, a patient with bowel obstruction and hypovolaemic
shock must be adequately resuscitated before undergoing surgery
otherwise the additional surgical injury and hypovolaemia induced
during the procedure will exacerbate the inflammatory activation
and increase the incidence and severity of end-organ insult.
Fluid therapy
In all cases of shock, regardless of classification, hypovolaemia and
inadequate preload must be addressed before other therapy is insti-
tuted. Administration of inotropic or chronotropic agents to an
empty heart will rapidly and permanently deplete the myocardium
of oxygen stores and dramatically reduce diastolic filling and there-
fore coronary perfusion. Patients will enter the unresuscitatable
stage of shock as the myocardium becomes progressively more
ischaemic and unresponsive to resuscitative attempts.
First-line therapy, therefore, is intravenous access and admin-
istration of intravenous fluids. Access should be through short,
wide-bore catheters that allow rapid infusion of fluids as neces-
sary. Long, narrow lines such as central venous catheters have too
New surgical booklet Anwar Qais Saadoon Basrah medical college 59
high a resistance to allow rapid infusion and are more appropriate
for monitoring than fluid replacement therapy.
Type of fluids
There is continuing debate over which resuscitation fluid is best
for the management of shock. There is no ideal resuscitation fluid
and it is more important to understand how and when to admin-
ister them. In most studies of shock resuscitation there is no overt
difference in response or outcome between crystalloid solutions
(normal saline, Hartmann’s solution, Ringer’s lactate) and col-
loids (albumin or commercially available products). Further, there
is less volume benefit to the administration of colloids than had
previously been thought, with only 1.3 times more crystalloid
than colloid administered in blinded trials. On balance there is
little evidence to support the administration of colloids, which
are more expensive and have worse side-effect profiles.
Most importantly, the oxygen-carrying capacity of crystalloids
and colloids is zero. If blood is being lost, the ideal replacement
fluid is blood, although crystalloid therapy may be required while
awaiting blood products.
Hypotonic solutions (e.g. dextrose) are poor volume
expanders and should not be used in the treatment of shock
unless the deficit is free water loss (e.g. diabetes insipidus) or
patients are sodium overloaded (e.g. cirrhosis).
Dynamic fluid response
The shock status can be determined dynamically by the cardio-
vascular response to the rapid administration of a fluid bolus. In
total, 250–500ml of fluid is rapidly given (over 5–10min) and
the cardiovascular responses in terms of heart rate, blood pressure
and central venous pressure (CVP) are observed. Patients can
bedivided into ‘responders’, ‘transient responders’ and ‘non-
responders’.Responders show an improvement in their cardiovascular
status, which is sustained. These patients are not actively losing
fluid but require filling to a normal volume status.
Transient responders show an improvement but then revert to
their previous state over the next 10–20min. These patients
either have moderate on-going fluid losses (either overt haemor-
rhage or further fluid shifts reducing intravascular volume).
Non-responders are severely volume depleted and are likely to
have major on-going loss of intravascular volume, usually
through persistent uncontrolled haemorrhage.
New surgical booklet Anwar Qais Saadoon Basrah medical college 60
Vasopressor and inotropic support
Vasopressor or inotropic therapy is not indicated as first-line therapy
in hypovolaemia. As discussed above, administration of these agents
in the absence of an adequate preload rapidly leads to decreased coro-
nary perfusion and depletion of myocardial oxygen reserves.
Vasopressor agents (phenylephrine, noradrenaline) are indi-
cated in distributive shock states (sepsis, neurogenic shock), in
which there is peripheral vasodilatation and a low systemic vas-
cular resistance, leading to hypotension despite a high cardiac
output. When the vasodilatation is resistant to catecholamines
(e.g. absolute or relative steroid deficiency), vasopressin may be
used as an alternative vasopressor.
In cardiogenic shock or when myocardial depression compli-
cates a shock state (e.g. severe septic shock with low cardiac out-
put), inotropic therapy may be required to increase cardiac
output and, therefore, oxygen delivery. The inodilator dobuta-
mine is the agent of choice.
Monitoring
The minimum standard for monitoring of the patient in shock is
continuous heart rate and oxygen saturation monitoring, fre-
quent non-invasive blood pressure monitoring and hourly urine
output measurements. Most patients will need more aggressive
invasive monitoring including CVP and invasive blood pressure
monitoring (Summary box 1).
Summary box 1
Monitoring for patients in shock
Minimum
■ Electrocardiogram
■ Pulse oximetry
■ Blood pressure
■ Urine output
Additional modalities
■ Central venous pressure
■ Invasive blood pressure
■ Cardiac output
■ Base deficit and serum lactate
New surgical booklet Anwar Qais Saadoon Basrah medical college 61
Cardiovascular
As a minimum, cardiovascular monitoring should include contin-
uous heart rate [electrocardiogram (ECG)], oxygen saturation
and pulse waveform and non-invasive blood pressure. Patients
whose state of shock is not rapidly corrected with a small amount
of fluid should have CVP monitoring and continuous blood pres-
sure monitoring through an arterial line.
Central venous pressure
There is no ‘normal’ CVP for a shocked patient, and reliance
cannot be placed on an individual pressure measurement to
assess volume status. Some patients may require a CVP of
5cmH2O, whereas others may require a CVP of 15cm H2O or
higher. Further, ventricular compliance can change from minute
to minute in the shocked state, and CVP is a poor reflection of
end-diastolic volume (preload).
CVP measurements should be assessed dynamically as the
response to a fluid challenge (see above). A fluid bolus
(250–500ml) is infused rapidly over 5–10min. The normal CVP
response is a rise of 2–5cmH2O, which gradually drifts back to
the original level over 10–20min.
Patients with no change in their CVP are empty and require further fluid
resuscitation. Patients with a large, sustained rise in CVP have high preload
and an element of cardiac insufficiency or volume overload.
Cardiac output
Cardiac output monitoring allows an assessment of not only the
cardiac output but also the systemic vascular resistance and,
depending on the technique used, end-diastolic volume (preload)
and blood volume. Invasive cardiac monitoring using pulmonary
artery catheters is becoming less frequent as new non-invasive
monitoring techniques such as Doppler ultrasound, pulse waveform
analysis and indicator dilution methods provide similar information
without many of the drawbacks of more invasive techniques.
Measurement of cardiac output, systemic vascular resistance
and preload can help distinguish the types of shock that are
present (hypovolaemia, distributive, cardiogenic), especially
when they coexist. The information provided guides fluid and
New surgical booklet Anwar Qais Saadoon Basrah medical college 62
vasopressor therapy by providing real-time monitoring of the
cardiovascular response.
Measurement of cardiac output is desirable in patients who do
not respond as expected to first-line therapy or who have evidence
of cardiogenic shock or myocardial dysfunction. Early considera-
tion should be given to instituting cardiac output monitoring in
patients who require vasopressor or inotropic support.
Systemic and organ perfusion
Ultimately, the goal of treatment is to restore cellular and organ
perfusion. Ideally, therefore, monitoring of organ perfusion should
guide the management of shock . The best measures of organ perfusion and
the best monitor of the adequacy of shock therapy remain the urine output;
however, this is an hourly measure and does not give a minute-to-minute
view of the shocked state.
The level of consciousness is an important marker of cerebral perfusion, but
brain perfusion is maintained until the very
late stages of shock and, hence, is a poor marker of adequacy of
resuscitation.Currently, the only clinical indicators of perfusion of the
gastrointestinal tract and muscular beds are the global measures
of lactic acidosis (lactate and base deficit) and the mixed venous
oxygen saturation.
New surgical booklet Anwar Qais Saadoon Basrah medical college 63
Chapter VII
Wounds, tissue repair
Topics
Introduction
Types of wound
Managing the acute wound
Some specific wound
Bite
Puncture wounds
Haematomata
Degloving
Compartment syndrome
64
64
65
66
66
67
67
67
68
New surgical booklet Anwar Qais Saadoon Basrah medical college 64
INTRODUCTION
Wound healing is a mechanism whereby the body attempts to
restore the integrity of the injured part. However, this falls far
short of the regeneration of tissue by pluripotent cells, seen in
some amphibians, and is often detrimental, as seen in the prob-
lems created by scarring such as adhesions, keloids, contractures
and cirrhosis of the liver, to name but a few. Several factors may
influence healing (Summary box 2).
Summary box 2
Factors influencing healing of a wound
■ Site of the wound
■ Structures involved
■ Mechanism of wounding
Incision
Crush
Crush avulsion
■ Contamination (foreign bodies/bacteria)
■ Loss of tissue
■ Other local factors
Vascular insufficiency (arterial or venous)
Previous radiation
Pressure
■ Systemic factors
Malnutrition or vitamin and mineral deficiencies
Disease (e.g.diabetes mellitus)
Medications (e.g.steroids)
Immune deficiencies [e.g.chemotherapy,acquired
immunodeficiency syndrome (AIDS)]
Smoking
a.In explosions,the contamination may consist of tissue such as bone from
another individual.
However, a clean incised wound in a healthy person where there
is no skin loss will follow a set pattern, as outlined below.
TYPES OF WOUNDS – TIDY VS. UNTIDY
The site injured, the structures involved in the injury and the
mechanism of injury (e.g. incision or explosion) all influence
healing and recovery of function. This has led to the management
of wounds based upon their classification into tidyand untidy
New surgical booklet Anwar Qais Saadoon Basrah medical college 65
(Summary box 3). The surgeon’s aim is to con-
vert untidy to tidy by removing all contaminated and devitalised
tissue.
Primary repair of all structures (e.g. bone, tendon, vessel and
nerve) may be possible in a tidy wound, but a contaminated
wound with dead tissue requires debridement on one or several
occasions before definitive repair can be carried out (the concept
of ‘second look’ surgery). This is especially true in injuries caused
by explosions, bullets or other missiles, where the external wound
Summary box 3
Tidy vs. untidy wounds
Tidy Untidy
Incised Crushed or avulsed
Clean Contaminated
Healthy tissues Devitalised tissues
Seldom tissue loss Often tissue loss
MANAGING THE ACUTE WOUND
The surgeon must remember to examine the whole patient
according to acute trauma life support (ATLS) principles. A stab
wound in the back can be missed just as easily in the reality of the
accident and emergency room as in a fictitious detective novel.
The wound itself should be examined, taking into consideration
the site and the possible structures damaged (Fig. 3.3). It is essen-
tial to assess movement and sensation while watching for pain
and listening to the patient.
A bleeding wound should be elevated and a pressure pad
applied. Clamps should not be put on vessels blindly as nerve
damage is likely and vascular anastomosis is rendered impossible.
In order to facilitate examination, adequate analgesia and/or
anaesthesia (local, regional or general) are required. General
anaesthesia is often needed in children. In limb injuries, particu-
larly those of the hand, a tourniquet should be used.
After assessment, a thorough debridement is essential.
Abrasions, ‘road rash’ (following a fall from a motorbike) and
explosions all cause dirt tattooing and require the use of a scrub-
bing brush or even excision under magnification. A wound
should be explored and debrided to the limit of blood staining.
Devitalised tissue must be excised until bleeding occurs with the
obvious exception of nerves, vessels and tendons. These may sur-
New surgical booklet Anwar Qais Saadoon Basrah medical college 66
vive with adequate revascularisation subsequently or by being
covered with viable tissue such as that brought in by skin or mus-
cle flaps.
The use of copious saline irrigation or pulsed jet lavage (where
the instrumentation is available) can be less destructive than
knife or scissors when debriding. Muscle viability is judged by the
colour, bleeding pattern and contractility.
In a tidy wound, repair of all damaged structures may be
attempted. A fascicular repair of nerves under magnification
(loupes or microscope) using 8/0 or 10/0 monofilament nylon is
usual. Vessels such as the radial or ulnar artery may be repaired
using similar techniques. Tendon repairs, particularly those in the
hand, benefit from early active mobilisation as this minimises
adhesions between the tendon and the tendon sheath (see above
for extrinsic tendon healing mechanism).
Skin cover by flap or graft may be required as skin closure should
always be without tension and should allow for the oedema typically
associated with injury and the inflammatory phase of healing. A flap
brings in a new blood supply and can be used to cover tendon, nerve,
bone and other structures that would not provide a suitable vascu-
lar base for a skin graft. A skin graft has no inherent blood supply
and is dependent on the recipient site for nutrition.
SOME SPECIFIC WOUNDS
Bites
Most bites involve either puncture wounds or avulsions. Small
animal bites are common in children (Fig. 3.4) and require
cleansing and treatment according to the principles outlined in
Summary box 4, usually under general anaesthetic.
Summary box 4
Managing the acute wound
■ Cleansing
■ Exploration and diagnosis
■ Debridement
■ Repair of structures
■ Replacement of lost tissues where indicated
■ Skin cover if required
■ Skin closure without tension
■ All of the above with careful tissue handling and
meticulous technique
New surgical booklet Anwar Qais Saadoon Basrah medical college 67
Ear, tip of nose and lower lip injuries are most usually seen in victims
of human bites. A boxing-type injury of the metacarpo-phalangeal
joint may result from a perforating contact with the teeth of a vic-
tim. Anaerobic and aerobic organism prophylaxis is required as bite
wounds typically have high virulent bacterial counts.
Puncture wounds
Wounds caused by sharp objects should be explored to the limit
of tissue blood staining. Needle-stick injuries should be treated
according to the well-published protocols because of hepatitis
and human immunodeficiency virus (HIV) risks. X-ray examina-
tion should be carried out in order to rule out retained foreign
bodies in the depth of the wound.
Haematomata
If large, painful or causing neural deficit, a haematoma may
require release by incision or aspiration. In the gluteal or thigh
region, there may be an associated disruption of fat in the form of
a fat fracture, which results in an unsightly groove but intact skin.
An untreated haematoma may also calcify and therefore require
surgical exploration if symptomatic.
Degloving
Degloving occurs when the skin and subcutaneous fat are
stripped by avulsion from its underlying fascia, leaving neuro-
vascular structures, tendon or bone exposed. A degloving injury
may be open or closed. An obvious example of an open degloving
is a ring avulsion injury with loss of finger skin (Fig. 3.5). A closed
degloving may be a rollover injury, typically caused by a motor
vehicle over a limb. Such an injury will extend far further than
expected, and much of the limb skin may be non-viable .
Examination under anaesthetic is required with a radical excision
of all non-bleeding skin, as judged by bleeding dermis.
Fluoroscein can be administered intravenously while the patient
is anaesthetised. Under ultraviolet light, viable (perfused) skin
will show up as a fluorescent yellowish green colour, and the non-
viable skin for excision is clearly mapped out. However, the main
objection to this method is that of possible anaphylactic shock
due to fluoroscein sensitivity. Most surgeons therefore rely upon
serial excision until punctate dermal bleeding is obvious. Split-
skin grafts can be harvested from the degloved non-viable skin
and meshed to cover the raw areas resulting from
debridement.
New surgical booklet Anwar Qais Saadoon Basrah medical college 68
Compartment syndromes
Compartment syndromes typically occur in closed lower limb
injuries. They are characterised by severe pain, pain on passive
movement of the affected compartment muscles, distal sensory
disturbance and, finally, by the absence of pulses distally (a late
sign). They can occur in an open injury if the wound does not
extend into the affected compartment.
Compartment pressures can be measured using a pressure
monitor and a catheter placed in the muscle compartment. If
pressures are constantly greater than 30mmHg or if the above
clinical signs are present, then fasciotomy should be performed.
Fasciotomyinvolves incising the deep muscle fascia and is best
carried out via longitudinal incisions of skin, fat and fascia .
The muscle will be then seen bulging out through the
fasciotomy opening. The lower limb can be decompressed via two
incisions, each being lateral to the subcutaneous border of the
tibia. This gives access to the two posterior compartments and to
the peroneal and anterior compartments of the leg. In crush
injuries that present several days after the event, a late fasciotomy
can be dangerous as dead muscle produces myoglobin which, if
suddenly released into the bloodstream, causes myoglobinuria
with glomerular blockage and renal failure. In the late treatment
of lower limb injuries, therefore, it may be safer to amputate the
limb.
New surgical booklet Anwar Qais Saadoon Basrah medical college 69
Chapter VIII
Nutrition in surgery
Topics
Nutritional support
Techniques of nutritional support
Enteral feeding
Indication of enteral feeding
Contraindication of enteral feeding
Complication of enteral feeding
Total parenteral nutrition
Indication of total parenteral nutrition (T.P.N)
Route of delivery of parenteral nutrition
Complication of T.P.N
70
70
70
71
71
71
72
72
72
74
New surgical booklet Anwar Qais Saadoon Basrah medical college 70
Nutritional support
how could you provide your patient with
his/ her nutritional needs??
Nutritional support should be considered in any
patient who is unable to take or resume an
adequate dietary intake for more than 5 days.
patients who are already malnourished or who are
subjected to significant metabolic stress.
Techniques of nutritional support:
1. Enteral (using the patient's own GIT).
2. Parenteral feeding.
1.Enteral feeding (using the patient's own GIT):
and can be safely accessed.
to:
1. Safer.
2. Less expensive.
3. More physiological.
4. Maintain gut barrier and decrease post-operative
infectious complications. So even when parenteral
nutrition is used, if possible, 10-20% of nutritional
needs should be met by enteral rout.
Techniques used to provide enteral feeding
1. Oral supplements.
2. Naso gastric or Naso enteric tube feeding.
3. Tube enterostomy.
Techniques used to provide enteral feeding
1.Oral supplements:
Used in those who can drink but have impaired appetite.
2.Naso gastric or Naso enteric tube feeding:
-gastric tube feeding can safely be used:
#When enteral feeding is likely to be required for < 6 weeks.
#When the patient has normal gag reflex and normal gastric emptying.
-enteric tube should be used, that can
New surgical booklet Anwar Qais Saadoon Basrah medical college 71
passes through the pylorus be gravity and gastric peristalsis
or can be placed endoscopically or fluoroscopically
3.Tube enterostomy:
-term feeding (> 6 weeks).
Open technique:
used in patient who needs laparotomy.
Per cutaneous endoscopic gastrostomy:
used when laparotomy is not indicated.
Indications of enteral feeding:
1. Protein-energy malnutrition with inadequate oral
intake.
2. Dysphagia, except for fluids.
3. Major trauma, including surgery.
4. Inflammatory bowel disease.
5. Distal, low output (<200 ml) entero-cutaneous
fistula.
6. To enhance adaptation after massive enterectomy.
Contraindications of enteral feeding:
1. Small bowel obstruction or ileus.
2. Severe diarrhea.
3. Proximal small intestinal fistulas.
4. Severe pancreatitis.
Complications of enteral feeding:
1. Complications related to feeding tube.
2. Complications related to feeding regimen.
1. Perforation of intestine.
2. Mal position e.g. trachio-bronchial tree.
3. Dislodgement/ migration.
4. Aspiration pneumonia.
5. Peritonitis.
6. Fistula formation.
7. Intestinal obstruction in case of tube
enterostomy.
8. Tube fracture/ blockage.
New surgical booklet Anwar Qais Saadoon Basrah medical college 72
1. Feeding intolerance (diarrhea and vomiting), its
common complication of enteral feeding.
2. Hyperglycemia.
3. Enteric infection, which might be a nosocomial
infection, if persist, the patient should be
investigated for Cl. difficile.2.Parenteral feeding
ame available since 1960s.
and pharmaceutical formulation of feeding solutions.
Intestinal Failure:
Is defined as intestinal disease, dysfunction or resection that
results in an inability to meet nutritional requirements by
enteral feeding.
Total Parenteral Nutrition (T.P.N.)
Is defined as the intravenous provision of all nutritional requirements,
without the use of the gastrointestinal tract.
Indications of parenteral nutrition
1. Proximal intestinal fistula.
2. Inflammatory bowel diseases (especially in the
preoperative period).
3. Massive intestinal resection (particularly if < 100 cm of
small bowel remains).
4. Ileus.
5. Severe pancreatitis.
So, parenteral nutrition is indicated when
nutritional support is appropriate but effective enteral nutrition is not
possible.
Route of delivery of parenteral nutrition
Peripheral venous line:
needed (less than 2 weeks).
ed into a peripheral vein and
maneuvered into the central venous system; this is called
"Peripherally Inserted Central venous Catheter-PICC".
New surgical booklet Anwar Qais Saadoon Basrah medical college 73
1.Thromophlebitis: infection of the vein.
2.Phlebothrombosis: venous thrombosis.
feeding solution, and both of the above can be reduced by:
1. Careful aseptic techniques during insertion &
handling.
2. Using of as small caliper catheter as possible to allow
blood linear flow.
3. Rate of TPN administration should be kept low (< 3
liters per day).
4. Lipid-based solution should be employed (which have
lower osmolarity than glucose-based solution).
Central veins are:
● Subclavian vein.
● Internal jugular vein.
● External jugular vein.
minimize the risk of infection.
at all possible because it's associated with a high incidence of
infection and thrombosis.
cava under radiological guidance.
controlled volumetric infusion pump.
2.Central venous line:Composition of parenteral nutrition formulas:
parenteral feeding regimens varying in:
-5 liters).
-3200 kcal).
-nitrogen ratio.
source (carbohydrate or lipid):
1. Glucose-based regimens (20% Glucose) – not
used in patients with active infection or severe
injury as they will develop glucose intolerance.
2. Lipid-based regimens.
nt's
fluid requirement and TPN is usually infused over 10-
18 hours, although critically ill patients may be feed continuously.
New surgical booklet Anwar Qais Saadoon Basrah medical college 74
resection) may require long term TPN, in such cases; patients are trained to
administer TPN to themselves at home.
Complications of parenteral feeding:
1. Complications related to feeding catheter.
2. Complications related to feeding regimen.
Complications related to the feeding catheter:
1. Complications those happen at time of catheter insertion
e.g. Arterial, venous, thoracic duct, stellate ganglion and brachial
plexus injuries, also pneumothorax and cardiac perforation.
2. Air embolism.
3. Catheter related infection: this is the most common potential
fatal complication of parenteral nutrition, occurs in about 6%, and > 90
% of cases is caused by Staphylococci. Usually presents with signs of
sepsis and should be treated by parenteral antibiotics and removal of
the catheter.
4. Infective endocarditis, usually suspected if signs of sepsis did not
respond to the usual treatment (see above).
5. Central venous/cardiac thrombosis.
6. Thrombotic catheter occlusion.
7. Catheter migration/embolus.
Complications related to feeding regimen
(Metabolic complications):
1. Hyperglycemia:
2. Hypoglycemia:
n liver failure.
3. Hypertriglyceridemia.
4. Hyperchloremic acidosis.
5. Electrolyte abnormalities.
6. Trace elements (zinc, chromium, and copper) &vitamins
deficiency states.
New surgical booklet Anwar Qais Saadoon Basrah medical college 75
Chapter IX
STOMAS
Topics
Colostomy
Temporary colostomy
Double barrelled colostomy
Permanent colostomy
Complication of colostomies
Loop ileostomies
caecostomy
76
76
77
77
78
78
79
New surgical booklet Anwar Qais Saadoon Basrah medical college 76
Colostomy
A colostomy is an artificial opening made in the large bowel to
divert faeces and flatus to the exterior, where it can be collected
in an external appliance. Depending on the purpose for which the
diversion has been necessary, a colostomy may be temporary or
permanent (Summary box 5).
Temporary colostomy
A transverse loop colostomy has in the past been most commonly
used to defunction an anastomosis after an anterior resection. It
is now less commonly employed as it is fraught with complications
and is difficult to manage; a loop ileostomy is preferred.
A loop left iliac fossa colostomy is still sometimes used to prevent faecal
peritonitis developing following traumatic injury to the rectum, to facilitate
the operative treatment of a high fistula-in-ano and incontinence.
A temporary loop colostomy is made, bringing a loop of colon
to the surface, where it is held in place by a plastic bridge passed
through the mesentery. Once the abdomen has been closed, the
colostomy is opened, and the edges of the colonic incision are
sutured to the adjacent skin margin . When firm
adhesion of the colostomy to the abdominal wall has taken place,
the bridge can be removed after 7 days.
Summary box 5
Stomas
■ May be colostomy or ileostomy
■ May be temporary or permanent
■ Temporary or defunctioning stomas are usually fashioned
as loop stomas
■ An ileostomy is spouted;a colostomy is flush
■ Ileostomy effluent is usually liquid whereas colostomy
effluent is usually solid
■ Ileostomy patients are more likely to develop fluid and
electrolyte problems
■ An ileostomy is usually sited in the right iliac fossa
■ A temporary colostomy may be transverse and sited in the
right upper quadrant
■ End-colostomy is usually sited in the left iliac fossa
■ All patients should be counselled by a stoma care nurse
before operation
■ Complications include skin irritation,prolapse,retraction,
necrosis,stenosis,parastomal hernia,bleeding and fistulation
New surgical booklet Anwar Qais Saadoon Basrah medical college 77
Figure 2: Usual temporary
(loop) colostomy opened over
a rod,and immediate suture of
the colon wall to surrounding skin
(many new rods are designed to lie
beneath the skin’s surface;
alternatively, a skin bridge is used).
Following the surgical cure or healing of the distal lesion for
which the temporary stoma was constructed, the colostomy can
be closed. It is usual to perform a contrast examination (distal
loopogram) to check that there is no distal obstruction or contin-
uing problem at the site of previous surgery. Colostomy closure is
most easily and safely accomplished if the stoma is mature, i.e.
after the colostomy has been established for 2 months. Closure is
usually performed by an intraperitoneal technique, which is asso-
ciated with fewer closure breakdowns with faecal fistulae.
Double-barrelled colostomy
This colostomy was designed so that it could be closed by crush-
ing the intervening ‘spur’ using an enterotome or a stapling
device. It is rarely used now, but occasionally the colon is divided
so that both ends can be brought to the surface separately, ensur-
ing that the distal segment is completely defunctioned.
Permanent colostomy
This is usually formed after excision of the rectum for a car-
cinoma by the abdominoperineal technique.
It is formed by bringing the distal end (end-colostomy) of the divided colon
to the surface in the left iliac fossa, where it is sutured in place, joining the
colonic margin to the surrounding skin
The point at which the colon is brought to the surface must be
carefully selected to allow a colostomy bag to be applied without
impinging on the bony prominence of the anterosuperior iliac
spine. The best site is usually through the lateral edge of the rec-
tus sheath, 6cm above and medial to the bony prominence .
New surgical booklet Anwar Qais Saadoon Basrah medical college 78
Closure of the lateral space between the intraperitoneal segment of the
sigmoid colon and the peritoneum of the pelvic wall,
to prevent internal herniation or strangulation of loops of small
bowel through the deficiency, has been practised, but there is no
good evidence that it is effective.
Many now incorporate a stomahesive backing, which can be left
in place for several days. In most hospitals, a stoma care service is
available to offer advice to patients, to acquaint them with the
latest appliances and to provide the appropriate psychological
and practical help.
Complications of colostomies
The following complications can occur to any colostomy but are
more common after poor technique or siting of the stoma:
• prolapse;
• retraction;
• necrosis of the distal end;
• fistula formation;
• stenosis of the orifice;
• colostomy hernia;
• bleeding (usually from granulomas around the margin of the
colostomy);
• colostomy ‘diarrhoea’: this is usually an infective enteritis and
will respond to oral metronidazole 200 mg three times daily.
Many of these complications require revision of the colostomy.
Sometimes, this can be achieved with an incision immediately
around the stoma but, on occasion, reopening the abdomen and
freeing up the colostomy may be necessary. Occasionally, transfer
to the opposite side of the abdomen may be necessary.
Loop ileostomy
An ileostomy is now often used as an alternative to colostomy,
particularly for defunctioning a low rectal anastomosis. The cre-
ation of a loop ileostomy from a knuckle of terminal ileum has
already been described. The advantages of a loop ileostomy over
a loop colostomy are the ease with which the bowel can be
brought to the surface and the absence of odour. Care is needed,
when the ileostomy is closed, that suture line obstruction does
not occur.
New surgical booklet Anwar Qais Saadoon Basrah medical college 79
Caecostomy
This is rarely used now. In desperately ill patients with advanced
obstruction, a caecostomy may be useful. In late cases of obstruc-
tion, the caecum may become so distended and ischaemic that
rupture of the caecal wall may be anticipated. This can occur
spontaneously, giving rise to faecal peritonitis, or at operation,
when an incision in the abdominal wall reduces its supportive
role and allows the caecum to expand. In such a situation, it
should be decompressed by suction as soon as the abdomen is
opened. In thin patients, it may then be possible to carry out
direct suture of the incised or perforated caecal wall to the
abdominal skin of the right iliac fossa, although a resection of this
area is really the best treatment. Following on-table lavage, via
the appendix stump, the irrigating catheter can be left in place as
a tube caecostomy. Caecostomy is only a short-term measure to
allow a few days for the condition of the patient to improve.
Reoperation should normally follow soon thereafter and a definitive
procedure should be carried out.
New surgical booklet Anwar Qais Saadoon Basrah medical college 80
Chapter X
History of common surgical cases
Topics
Urine retention
Haematuria
Melaena
Haematochesia
Haematemesis
Nipple discharge
Breast lump
Jaundice
Dysphagia
Neck swelling
Scrotal swelling and hernias
Appendicitis
81
82
83
84
85
86
87
88
89
90
91
92
New surgical booklet Anwar Qais Saadoon Basrah medical college 81
1- Urine retention
1-
Duration & Onset
2-
Pain
3-
distention
4-
Preceded symptoms:
1. Dysuria
2. Frequency
3. Nacturia
4. Urgency
5. Urge incontinence
6. Polyuria
7. Hesitancy
8. Intermittency
9. Poor stream
10. Post micturition dribbling
11. Terminal dribbling
5-
Having :
1. Haematuria
2. History of urethral discharge
3. History of Trauma
4.History of passing stone
5.HISTORY of instrumentation
6. History of operation
6- Gynecological problem if female & sexual activity in male
7- Constitutional symptoms
1) Wt. loss
2) Appetite
3) Fever & rigor & night sweat
4) Muscle Weakness
5) Malaise
6) constipation
8- past History :
1) previous CVA
2) neurological dz
3) DM
9-
drug History
10.patient reaction
1) after putting foly catheter
amount and color of urine
2)any investigation
10.Pt. condition now
New surgical booklet Anwar Qais Saadoon Basrah medical college 82
2- Haematuria
1- duration
2- onset
3- Timing(terminal, whole stream, only beginning of micturition)
4- pattern ( intermittent , continuous)
5- Painful or painless
6- severity
1) Associated with clot
2) Amount
3) palpitation , Dyspnea, headache, decrease urine output,
fainting attack
7- Bleeding between voiding
8- Bleeding from other site
9- Having :
1) History of passing stone
2) History of trauma or Exercise
3) History of foley catheter insertion
4) History of URTI
5) Hearing condition
10- Abdominal mass
11-
Review of GUT
1) Dysurea
2) Frequency
3) Nacturia
4) Urgency
5) Urge incontinence
6) Polyuria
7) Hesitancy
8) Intermittency
9) Loin pain
10) Poor stream
11) Post micturition dribbling & Terminal dribbling
12-
Constitutional symptoms
1) Wt. loss
2) Appetite
3) fever
4) Malaise
13-
Menstrual History
14-
History of drug ingestion
15-
Food ingestion (beet root
)
New surgical booklet Anwar Qais Saadoon Basrah medical college 83
3- Melaena
1- Duration
2- Onset
3- Persistence
4- Criteria: black, tarry ,shiny sticky, offensive
5- Associated with:
Abdominal Pain
Haematemesis
Jaundice
6- Bleeding from anywhere in the body
7-Severity : palpitation , dyspnea, palpitation , dyspnea, fainting
attack, headache
Decrease urine output, clot
8- Review of GI
9- Constitutional symptoms
1) Wt. loss
2) Appetite
3) fever
4) Malaise
10- Past history
Same attack
Jaundice
Peptic ulcer
11- Social History
Alcohol
smoking
12- Family history :
Same symptoms
Chronic liver dz.
13- Drug History
Iron
Bismuth
Meat , beet root
NSAID's
Aspirin
Warfarin
Heparin
Any addition
Thank you
New surgical booklet Anwar Qais Saadoon Basrah medical college 84
4- Haematochesia
1- Duration
2- Onset
3- No. of defecations
4- Progression
5- Persistence
6- Painful or painless
7- When the pain begin( at time of defecation after or before
defecation)
8- Contain
1) Pus
2) Mucus
9- The blood mix with the stool before or after the stool
10- Associated with:
Abdominal Pain
Haematemesis
Tenesmus
Protrusion of lump from the anus
11- Bleeding from anywhere in the body
12- Severity : palpitation, dyspnea , clot , amount, fainting attack,
headache, Decrease urine output,
13- Drug History
NSAID's
Aspirin
Warfarin
Heparin
Iron
Bismuth
Meat , beat root
14- Social History
Alcohol
15- Review of GI
16- Constitutional symptoms
Fever
Wt. loss
New surgical booklet Anwar Qais Saadoon Basrah medical college 85
5- Haematemesis
ID: name, age, next of kin
1- Duration
2- Onset
3- frequency
4- timing
5- Preceded by nausea or attacks of vomiting
6- Projectile or effortless
7- Vomitus characters
1) amount
2) color
3) odor
4) content
8- Associated with:
Abdominal Pain
Melaena or Hematochezia
jaundice
9- Bleeding from anywhere in the body
10- Severity : palpitation , dyspnea, fainting attack, headache,
Decrease urine output, clot
11- Drug History
NSAID's
Aspirin
Warfarin
Heparin
12- Social HISTORY
Alcohol
13- Review of GI
14- Constitutional symptoms
Fever
Wt. loss
New surgical booklet Anwar Qais Saadoon Basrah medical college 86
6- Nipple discharge
ID:
1)age
2)marital status
HPI
1- Duration
2- Onset
3- Amount
4- Color Contain blood
5- Unilateral or bilateral
6- Occur spontaneously or on squeezing
7- Persistent
8- progression
11-assuciated with:
1) Lump (in the breast or axilla)
2) Pain
3) Breast skin changes
4) Breast size or nipple position changes retraction
12- Aggregating and relieving factors
13- Relation to menstruation
14- Lactation
15- pregnant
16- History of OCP ingestion
17-History of trauma
18-Constitutional symptoms
1)
Wt. loss
2)
Appetite
3)
fever
4)
Malaise
19- Bone pain, jaundice, cough
New surgical booklet Anwar Qais Saadoon Basrah medical college 87
7- Breast lump
ID:
1)age
2)marital status
HPI
1)History of lump
1- Duration
2-
size ,site , mobile or not
3- First symptom
4- Associated symptoms
a-pain
b-disfiguring
c- redness itching
c-nipple discharge or retraction
5- Progression
when did they notice the change
bigger or smaller
fluctuated in size
more tender
6- Persistence
7- Other lumps
8- Cause of the lump
9)History of trauma
2)relation to the cycle
3)Lactation
4) pregnancy
5)OCP
6) risk factors for breast Ca:
1.
Early menarche late menopause
2.
OCP=> nullipara => delay first pregnancy=> non lactated women
3.
High socioeconomic state => fatty food=> Alcohol
4.
Family History of breast ca => genetic mutation and antigen
5.
Previous Ca in other breast => radiation exposure
7)Constitutional symptoms
1)Wt. loss
2)Appetite
3)fever
4)Malaise
8)Symptoms of metastasis: lumbar pain ,cough , jaundice
New surgical booklet Anwar Qais Saadoon Basrah medical college 88
8- Jaundice:
ID
1)age
2) occupation
3) marital status
HPI
1- Duration
2- Onset
3- Noticed by the family or the pt.
4- Progressive or fluctuant
5- Associated with:
1) Pain
2) Itching
6- Color of urine
7- Color of the stool
8- Bleeding from any where
9- Review of GIT
1-
Anorexia
2- Nausea & vomiting
3- Dysphgia
4- Flatulence & dyspepsia
5- Altered bowel motion (diarrhea or constipation)
6- Weight loss
7- Haematemesis
8- Melaena
9- Bleeding per rectum
10- Constitutional symptoms
Fever & rigor
Malaise
1-
Past History
Blood transfusion
Previous jaundice
Haematemesis and malena
Previous biliary surgery
2- Social History
Contact with jaundice pt.
Alcohol drinking
Tattoos
History of being abroad
3- Family History:
Hemolytic dz
Liver dz
Other member of family Affected
4- Drug History
1) Icterogenic drugs: paracitamol, OCP, mythyle dopa , oral
antihyperglycemic drugs
2) Drug abuse
New surgical booklet Anwar Qais Saadoon Basrah medical college 89
9- Dysphagia
ID
Age
HPI
1- Duration
2- Onset
3- To solid or to liquid
4- At which level
5- Persistence
6- Progression
7- History of foreign body ingestion
8- Corrosive material ingestion
9- Aggravating and reliving factor
10- Associated With:
1) Pain
2) Hurt burn
3) regurgitation
4) vomiting
5) Fever
6) Wt. loss
7) Malaise
8) neck swelling
8) Symptom of anemia: palpitation Dyspnea,
11-Any neurological problem
12- Muscle weakness
13- Social problem
14- History of trauma to the neck
15- Review GIT
16- Drug history
New surgical booklet Anwar Qais Saadoon Basrah medical college 90
10- Neck swelling
Id:
age
Address
Occupation
HPI:
1.
Duration
2.
First symptom
3.
Associated symptoms
a-pain
b-Dyspnea
c- Dysphagia
d-hoarseness of voice
4.
Progression
when did they notice the change
bigger or smaller
fluctuated in size
more tender
5.
Persistence
6.
Other lumps
7.
Cause of the lump
8.
Thyroid status
1) Appetite
2) Weight
3) Bowel habit
4) Palpitation
5) Menorrhagia or amenorrhea or oligomenorrhea
6) Hot or cold preference
7) Anxiety
8) Sleeping pattern
9) Eye problems
9.
General questions: fever, night sweating, hyperactivity
malaise , weakness
10.
Pregnancy
11.
Drug History: OCP , Iodine intake
12.
Family History of goitre
New surgical booklet Anwar Qais Saadoon Basrah medical college 91
11- Scrotal swelling & hernia
1.
Duration
2.
Onset
3.
Unilateral or bilateral
4.
First symptom
5.
Associated symptoms
a-vomiting
b- abdominal distention
c- abd. Pain
d- constipation
strangulation
1)fever
2) pain
3) tense
4) red
6.
Progression
when did they notice the change
bigger or smaller
fluctuated in size
more tender
7.
Persistence
8.
Precipitating factor for hernia :
Chronic Straining
Chronic Cough
Lifting heavy thing
Previous surgery
9.
Other lumps in any site
10.
Cause of the lump
11.
History of trauma
12.
Review of GIT and genitourinary
New surgical booklet Anwar Qais Saadoon Basrah medical college 92
12- Appendicitis
1- Analysis of pain
1) Duration of pain
2) Onset
3) Site: when it start and now it where
4) Severity: interfere with physical activity
5) Character
6) Radiation
7) Aggregating and reliving factors
8) Associated symptoms
2- vomiting
3- anorexia
4- diarrhea
5-cough
6-jaundice
7-dysurea or frequency
8-review other GIT & GUT symptoms
9-constitutional symptoms:
Fever, rigor, Malaise, Sweating
10-past history
Peptic ulcer
Operation
Passing stone
Jaundice
DM
SCA
11-social history
Alcohol
smoking
13-family history
DM
SCA
14-Gynecological history
15-Drug history
متت حبمد اهلل
