1
Medicine Dr. Sabah
CORONARY ARTERY DISEASES
PRESENTING PROBLEMS IN CARDIOVASCULAR DISEASE
1. Palpitation ---
Arrhythmias
2. Breathlessness (dyspnoea) -----
HF
3. Chest pain ---
CAD
4. Syncope and presyncope--
p Hypertension
p Cardiac arrest and sudden cardiac death
p Abnormal heart sounds and murmurs
CAD
1) (Chronic) Stable angina.
2) Acute coronary syndromes
a. unstable angina
b. acute MI
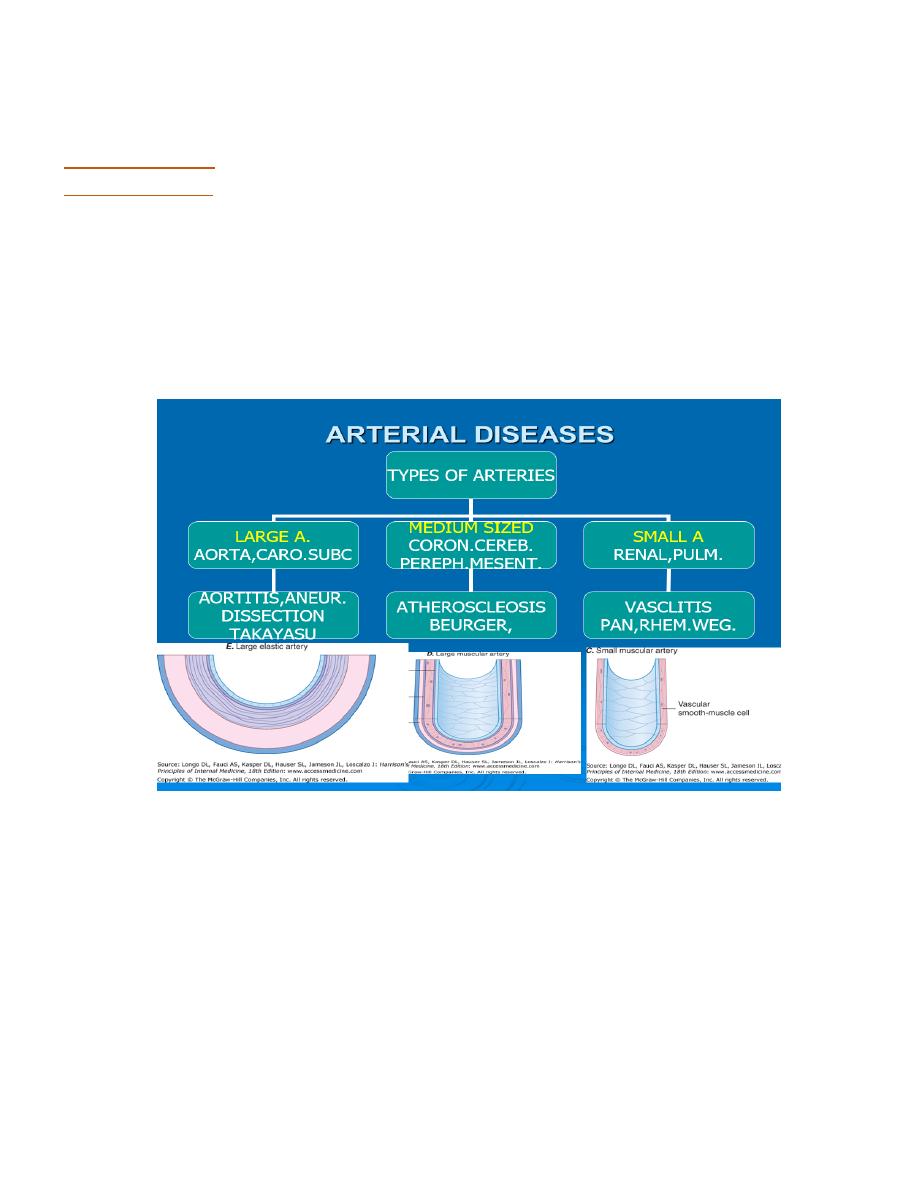
CORNARY ARETRY DIS. (ISCHAEMIC HEART DIS.)
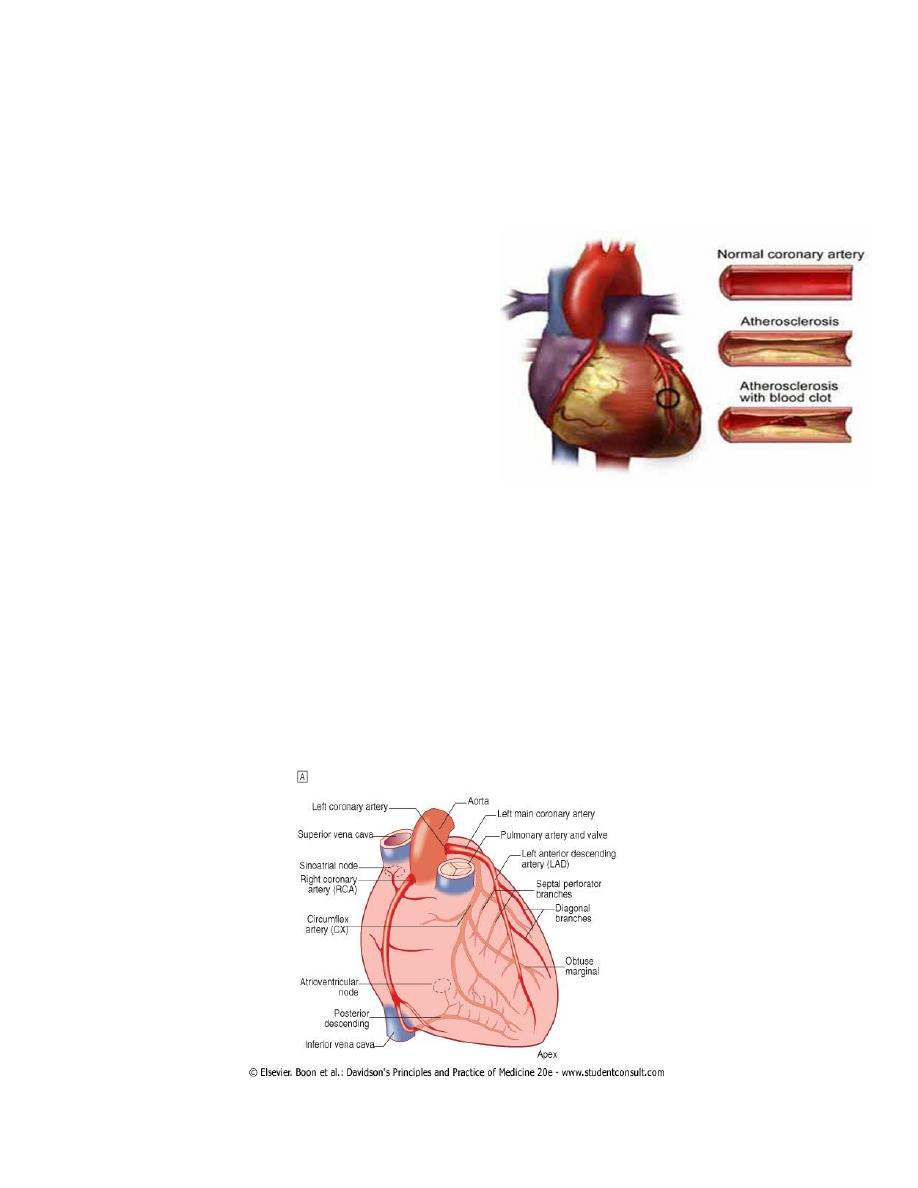
1. ATHEROSCLEROSIS
2. ANGINA PECTORIS
3. MYOCARDIAL INFARCTION
2
ATHEROSCLEROSIS
TERMINOLOGIES
Arteriosclerosis =
generic term for thickened and stiffened arteries of all sizes.
Atherosclerosis =
descriptive term for thickened and hardened lesions of medium and large
muscular and elastic arteries.
lesions
1. lipid rich
2. occur within intima(although media and adventitia may also be involved.)
3. generally eccentric
4. become complicated by mural or occlusive thrombosis, = atherothrombosis
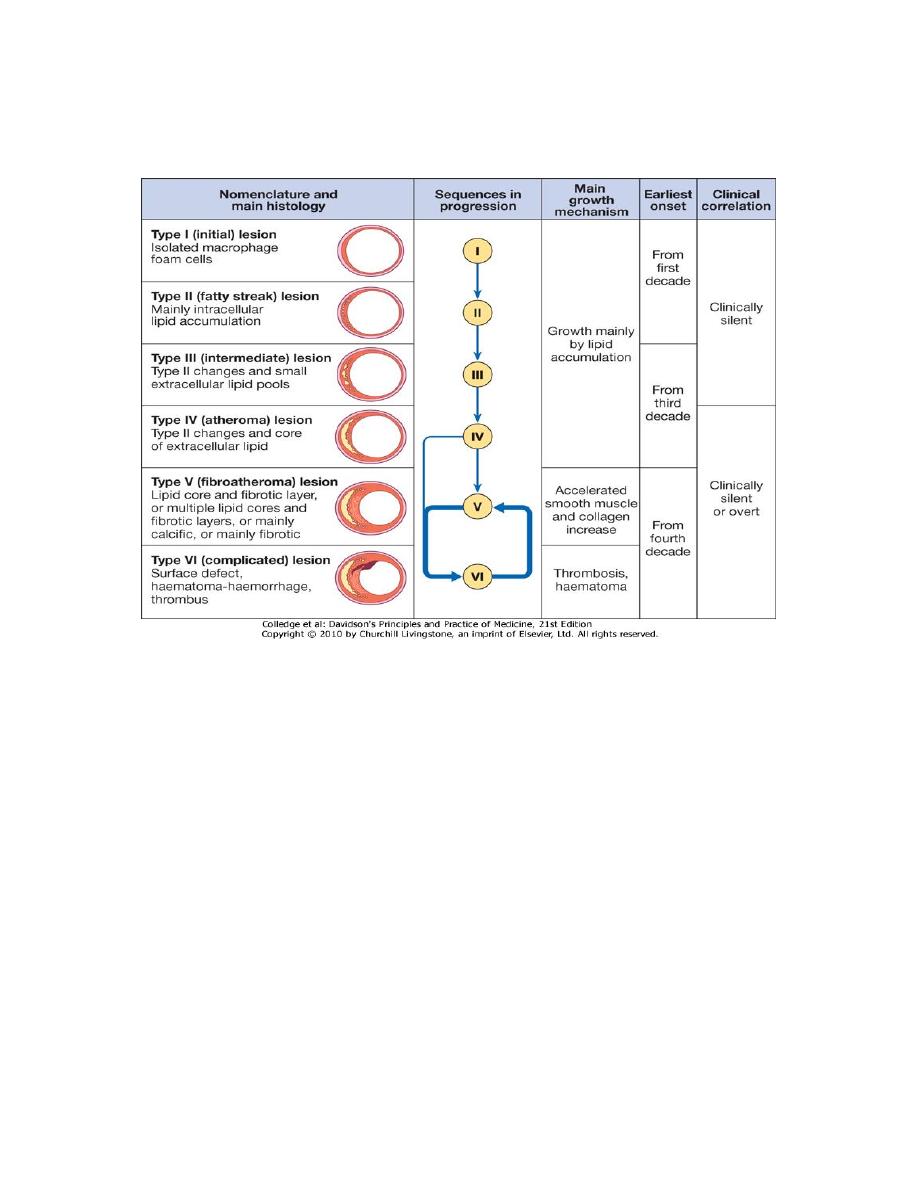
HISTOLOGY
normal artery = tube with
1)
intima or internal lining covered by a continuous layer of endothelial cells maintains
circulating blood flow (antithrombotic),acts as a barrier to keep circulating monocyte-
macrophages from entering into vessel wall (antiadhesion or migration), regulates smooth
muscle cell function (relaxation or antigrowth);
2)
media, = smooth muscle cells = contract and maintain tone of artery wall +extracellular
matrix or fibrils (elastin, collagen, proteoglycans) =supportive structure
3)
adventitia =loose connective tissue (fibroblasts, EC matrix, vasa vaso.).
3
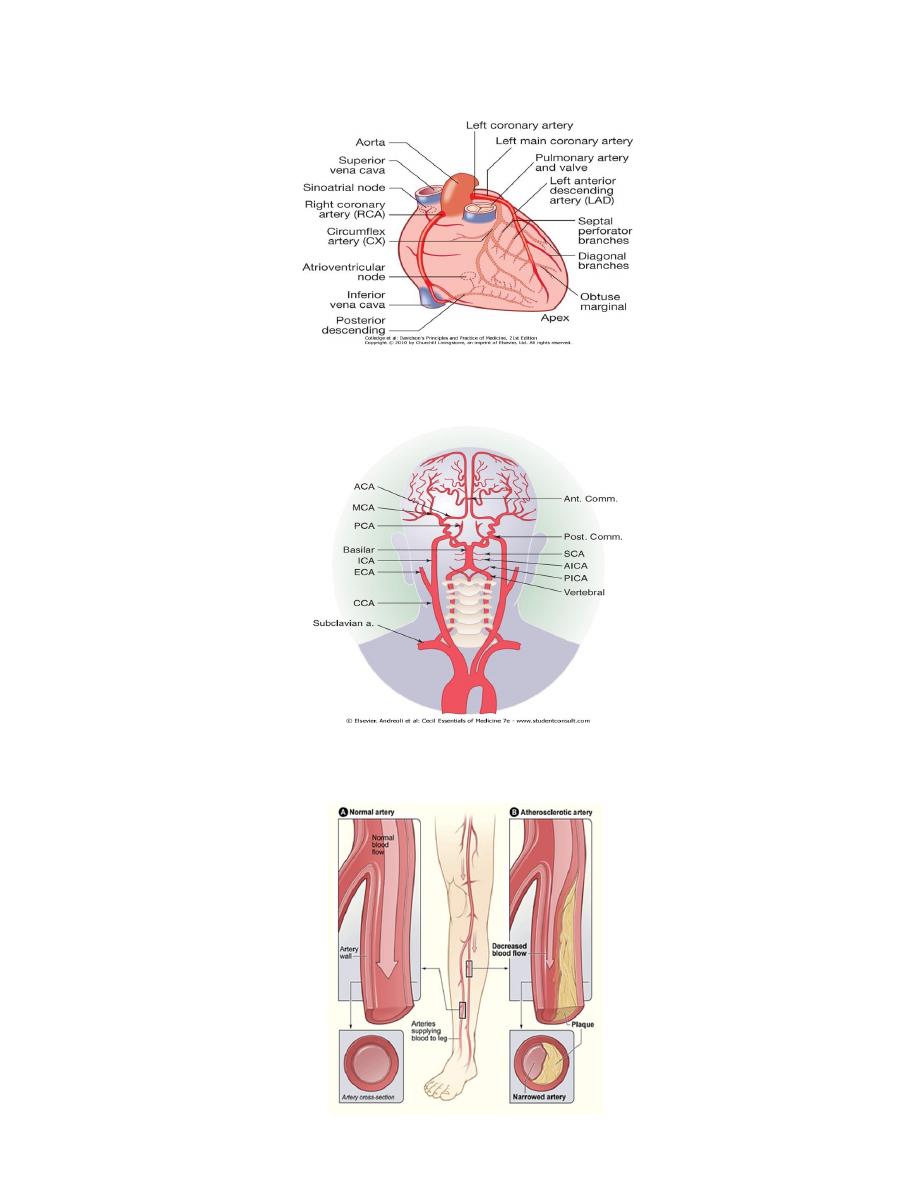
coronary heart disease
angina, myocardial infarction, sudden death
cerebrovascular disease
stroke and transient ischaemic attack
peripheral vascular disease
claudication and critical limb ischaemia
4
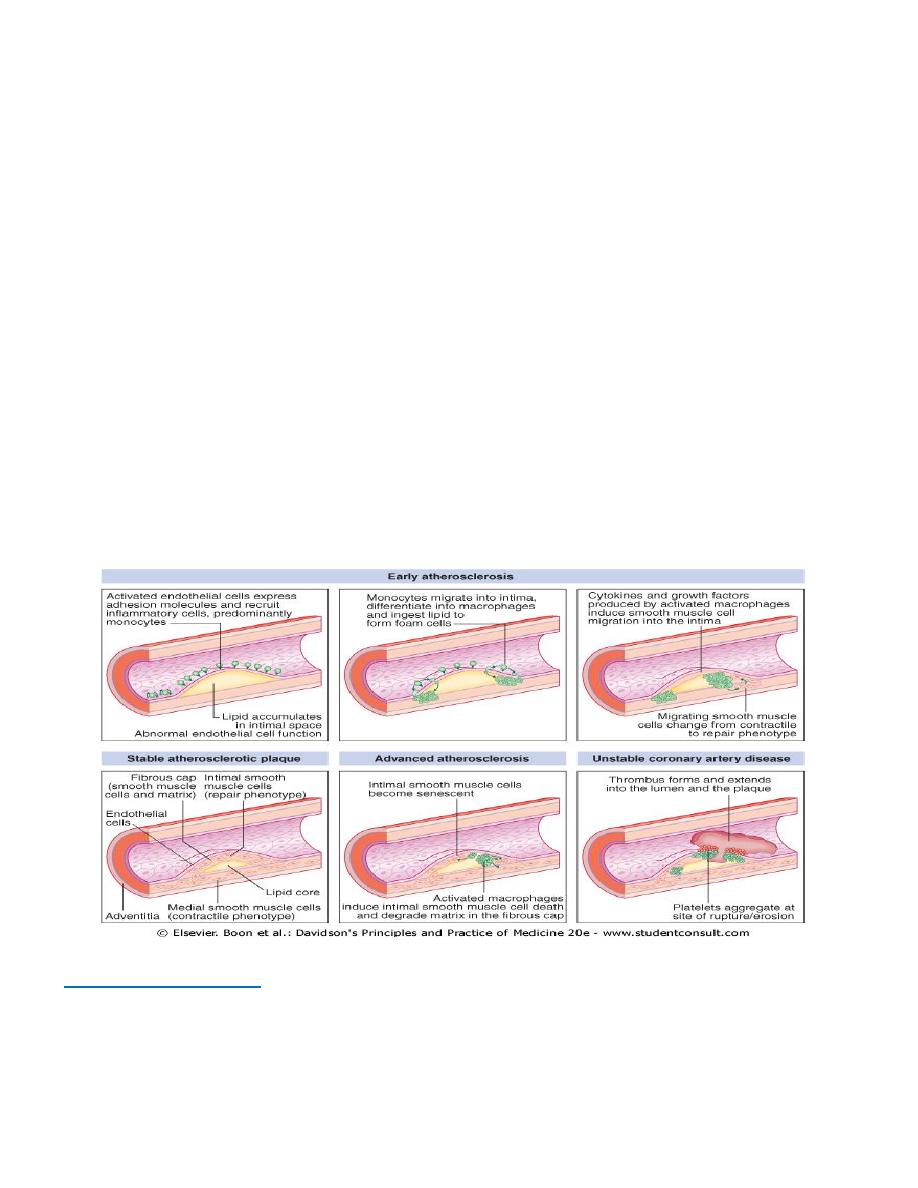
Pathophysiology
Key wards
progressive inflammatory disorder
Early atherosclerosis X Advanced atherosclerosis
active or unstable plaque X stable plaque
Process:
lipid from plasma to intimaPlaque
Elements
e Plasma lipid
e Monocyte-macrophage
e Endothelial cells
e Smooth muscle
e Cytokines
e Platelets
e Blood pressure
Site of lesion :
intimaplaque
mediaremodelling
1-Early atherosclerosis
b Fatty streaks
b small lipoprotein particles penetrate vascular endotheliumoxidized coalesce into
aggregates in intimal layer –
b ? expression of adhesion molecules

5
Monocytes
1. bind to endothelial cells,
2. migrate into intima,
3. take up oxidised LDL) particles =>
4. lipid-laden macrophages or foam cells.
Foam cells:
die and release contents = extracellular lipid pools in intimal space
Activated macrophages
cytokines and growth factors---
1-growth factorsSmooth muscle cells
1- migrate from media of arterial wall into intima
2- change from contractile to repair phenotype stabilise atherosclerotic lesion.
Successful== lipid core will be covered by smooth muscle cells and matrix, stable
atherosclerotic plaque remain asymptomatic = large enough obstruct arterial flow.
2-Advanced atherosclerosis
Established atherosclerotic plaque
macrophages mediate inflammation
smooth muscle cells promote repair.
Inflammation predominates
plaque active or unstable +/-
complicated by ulceration and thrombosis.
Activated macrophages Cytokines
1. intimal smooth muscle cells overlying plaque = senescent
2. collagen cross-struts within the plaque = degrade.
thinning of protective fibrous cap= lesion vulnerable to mechanical stress Breach(
erosion, fissuring or rupture) of plaque surface
6
Breach in integrity of plaque expose its contents to blood, trigger platelet aggregation
and thrombosis that extend into atheromatous plaque and arterial lumen
A. partial or complete obstruction at the site of the lesion or
B. distalembolisation resulting in infarction or ischaemia of affected organ.
number and complexity of plaques increase with age + systemic risk factors rate of
progression of individual plaques is variable.
Types of plaque
1-Vulnerable plaques‘=
% lipid-rich core
% thin fibrocellular cap
% increase in inflammatory cells
% release of specific enzymes =degrade matrix proteins.
2-stable plaques =
d small lipid pool
d thick fibrous cap
d calcification and plentiful collagenous cross-struts.
d Lipid-lowering therapy stabilise vulnerable plaques.

7
Fissuring or rupture = occur at sites of maximal mechanical stress, particularly the margins of
an eccentric plaque, ( may be triggered by a surge in blood pressure (e.g. during exercise or
emotional upset).
plaque events are often subclinical and may heal spontaneously= may allow thrombus to be
incorporated into the lesion plaque growth and further obstruction to flow in the arterial
lumen.
Remodelling
Atherosclerosis = induce complex changes in the media = arterial remodelling;
1. some arterial segments may slowly constrict (negative remodelling) whilst
2. others may gradually enlarge (positive remodelling).
poorly understood / important = amplify or minimise the degree to which atheroma
encroaches into the arterial lumen.
RISK FACTORS
7 Some key factors emerged but do not explain all the risk
7 unknown or yet unconfirmed factors account for up to 40% of variation in risk of
atheromatous VD from one person to the next.
7 Impact of genetic risk = twin studies; monozygotic twin of an affected individual has an
eightfold increased risk, dizygotic twin a fourfold increased risk of dying from coronary
heart disease compared to the general population.
7 Effect of risk factors is multiplicative rather than additive.
7 People with a combination of risk factors (e.g. smoking, hypertension and diabetes) are at
greatest risk and assessment should therefore be based on a holistic approach that takes
account of all identifiable risk factors.
Types:
1)
relative risk (the proportional increase in risk)
2)
absolute risk (the actual chance of an event).
E.x. man of 35 with a plasma cholesterol of 7 mmol/l (∼170 mg/dl) who smokes 40 cigarettes
a day is relatively much more likely to die from coronary disease within the next decade than a
non-smoking woman of the same age with a normal cholesterol, but the absolute likelihood of
his dying during this time is still small (high relative risk, low absolute
8
RISK FACTORS
1. Age and sex.
2. Family history.
3. Smoking.
4. Hypertension
5. Hypercholesterolaemia .
6. Diabetes mellitus
7. Haemostatic factors
8. Physical activity
9. Obesity
10. Alcohol. dietary factors/ Personality.
1-Age and sex.-
Age=most powerful independent risk factor for athero.
Sex=Pre-menopausal women have much lower rates of disease than age- and risk-matched
males difference disappears rapidly after menopause.
Hormone replacement therapy = no role in primary or secondary prevention of coronary
heart disease. ( isolatedoestrogen therapy increased cardiovascular event rate.)
2-Family history.
Atherosclerotic vascular disease often runs in families.
combination of shared genetic, environmental and lifestyle (e.g. smoking, exercise and
diet) factors.
Most common inherited risk characteristics (hypertension, hyperlipidaemia, diabetes) are
polygenic.
A 'positive' family history is present when clinical problems occur in
1. first-degree relatives
2. at relatively young age(< 50 years for men and < 55 years for women)
3-Smoking
most important avoidable cause
strong, consistent and dose-linked relationship
between cigarette smoking and ischaemic heart disease
4-Hypertension incidence
of atherosclerosis increases as BP rises
excess risk is related to both
systolic and diastolic blood pressure + pulse pressure.
AHT = reduce coronary mortality, stroke and heart failure.
5-Hypercholesterolaemia
atherosclerotic vascular disease rises with plasma cholesterol concentration esp. ratio of total
cholesterol to high-density lipoprotein (HDL) cholesterol.
9
weaker correlation = plasma triglyceride concentration. lowering total LDL and cholesterol
concentrations reduces the risk of cardiovascular events including death, myocardial
infarction and stroke, reduces the need for revascularisation
6-Diabetes mellitus.
potent risk factor for all forms of atherosclerosis often associated with
diffuse disease difficult to treat.
Insulin resistance (normal glucose homeostasis +high levels
of insulin) = associated with obesity and physical inactivity= potent risk factor for CAD
Glucose intolerance accounts for a major part of the high incidence of IHD in certain ethnic
groups, e.g. South Asians
7-Haemostatic factors.
Platelet activation +high levels of fibrinogen associated with
increased risk of coronary thrombosis.
Anti-phospholipid antibodies = recurrent
arterielthomboses.
8-Physical activity.
Physical inactivity roughly doubles risk of coronary heart disease and is a major risk factor
for stroke.
Regular exercise (brisk walking, cycling or swimming for 20 min. two or three times a week)
appears to have a protective effect (may be related to increased HDL cholesterol, lower blood
pressure, reduced blood clotting, and collateral vessel development)
9-Obesity .
particularly if central or truncal= independent risk factor
( although often
associated with other adverse factors e.g.hypertension, diabetes and physical inactivity.)
10 -Alcohol.
A moderate intake of alcohol (2-4 units a day) appears to offer some protection
from coronary disease; heavy drinking is associated with hypertension and excess cardiac
events.
Other dietary factors.
A. Diets deficient in fresh fruit, vegetables and polyunsaturated fatty acids = associated with
increased risk of vascular dis..
B. Low levels of vitamin C, vitamin E and other antioxidants may enhance the production of
oxidised LDL.
C. Hyperhomocysteinaemia = accelerated atherosclerosis including stroke and peripheral
vascular disease.
D. Low dietary folate, vitamin B12 and vitamin B6 can elevate homocysteine concentrations.
Personality.
% Certain personality traits are associated with an increased risk of coronary disease.
% little or no evidence to support the popular belief that stress is a major cause of coronary
artery disease
10
POPULATION ADVICE TO PREVENT CORONARY DISEASE
Do not smoke
Take regular exercise (minimum of 20 mins, three times a week)
Maintain 'ideal' body weight
Eat a mixed diet rich in fresh fruit and vegetables
Aim to get no more than 10% of energy intake from saturated fat
PRIMARY PREVENTION
Two complementary strategies
1-population strategy
modify risk factors of whole populationdiet and lifestyle advice
even a small reduction in smoking or average cholesterol, or modification of exercise and
diet will produce worthwhile benefits (Some risk factors for atheroma, such as obesity and
smoking, are also associated with a high risk of other diseases and should be actively
discouraged through public health measures.
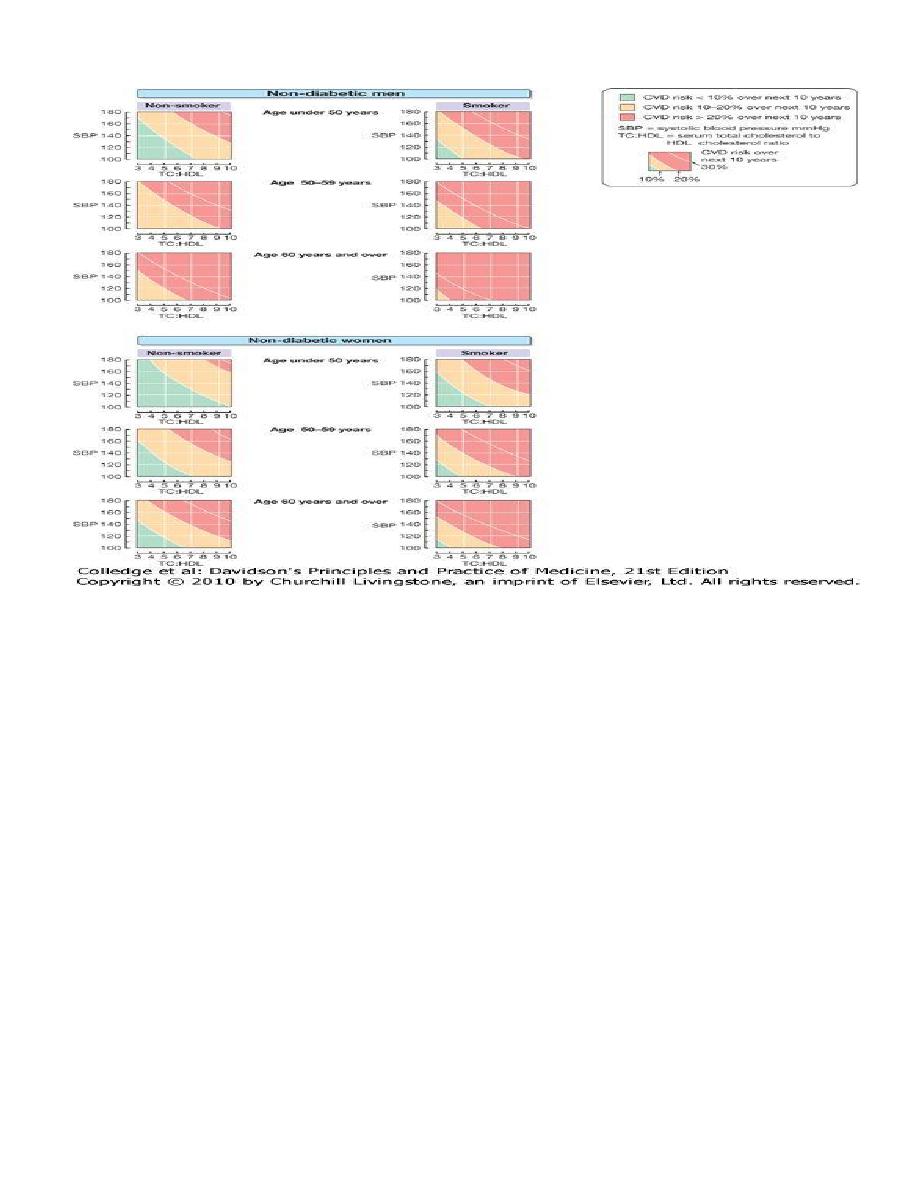
2-targeted strategy
identify and treat high-risk individuals
usually have a combination of risk factors
can be identified by using composite scoring systems
consider the absolute risk of atheromatous cardiovascular disease that any one individual
is facing before contemplating specific antihypertensive or lipid-lowering therapy =
help to determine whether the possible benefits of intervention are likely to outweigh the
expense, inconvenience and possible side-effects of treatment.
55-year-old woman
65-year-old man
exactly the same BP150/90
average BP150/90
Not smoker
Smoker
Not diabetic
diabetic
total:HDL cholesterol of 6
total:HDL cholesterol of 8
Normal ECG
ECG changes of LVH
predicted 10-year CHD risk < 14%;
10-year CHD risk = 68%
AHT prevent fewer than 3 events per
1000 patient years of treatment
AHT(assuming 20% relative risk reduction)
prevent 14 coronary events for every
1000 patient years of treatment
Questionable
Advisable
11
SECONDARY PREVENTION
l Patients already have evidence of atheromatous vascular D (e.g. peripheral vascular
disease or myocardial infarction)
l at high risk of another vascular event
l can be offered a variety of treatments and measures
l improve their outlook (secondary prevention).
energetic correction of risk factors,
particularly smoking, hypertension and
hypercholesterolaemia, = absolute risk of further vascular events is very high. all patients with
coronary heart disease should be given
statin
therapy irrespective of their serum cholesterol
concentration. Blood pressure should be treated to a target of ≤ 130/80 .
Aspirin and ACE inhibitors
are of benefit in all patients with evidence of vascular disease
Beta-blockers
= benefit patients with a history of myocardial infarction or heart failure.
clinical events offer = opportunity to introduce effective secondary preventive measures. E.g.,
patients who have just survived MI or undergone bypass surgery are usually keen to help
themselves and may be particularly receptive to appropriate lifestyle advice, such as weight
reduction, stopping smoking etc.
