1
Medicine Dr.Sabah
ACUTE CORONARY SYNDROME
UNSTABLE ANGINA & MYOCARDIAL INFARCTION
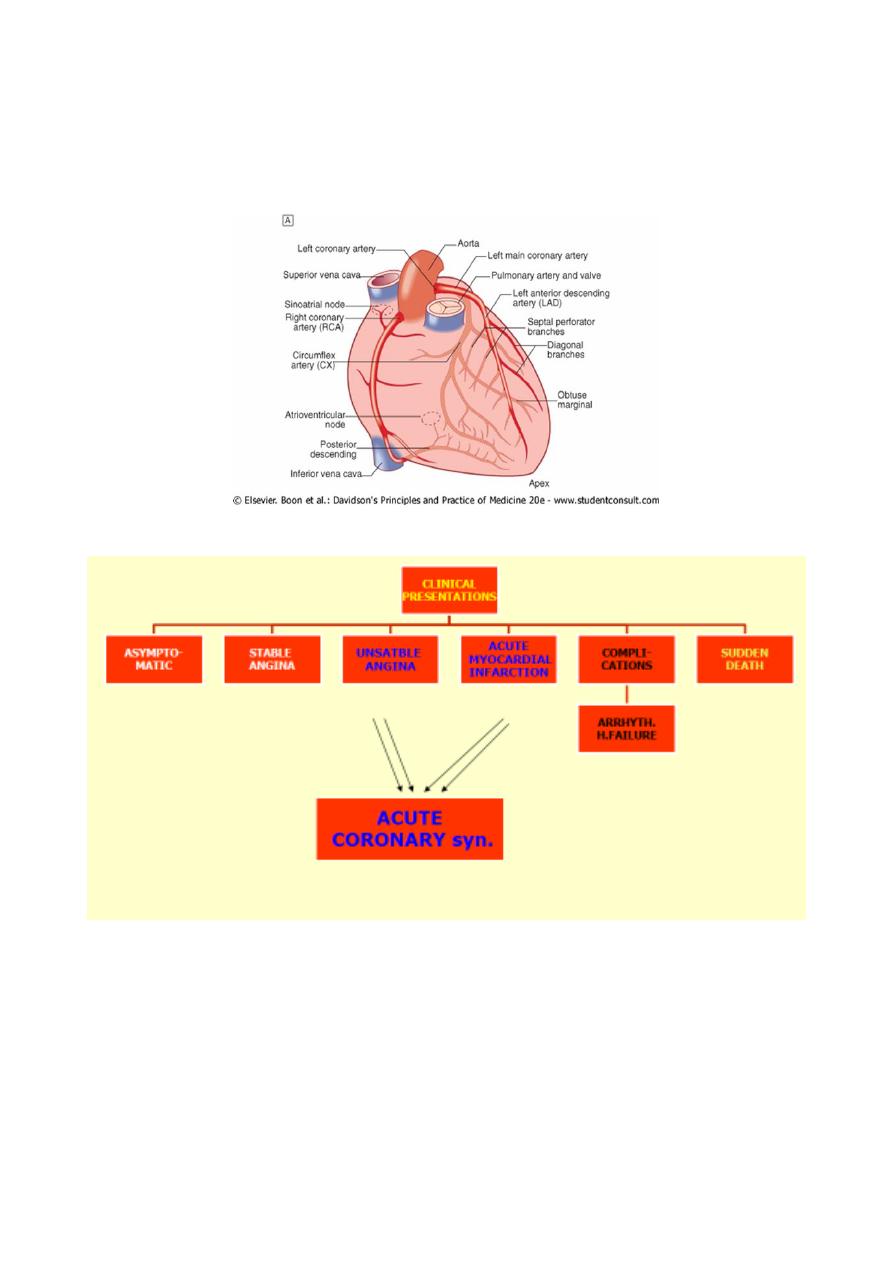
Coronary heart disease:
clinical manifestations and pathology
D Stable angina =Ischaemia = fixed atheromatous stenosis of one or more coronary A
D Unstable angina= Ischaemia = dynamic obstruction of a coronary artery == plaque
rupture or erosion with superimposed thrombosis
2
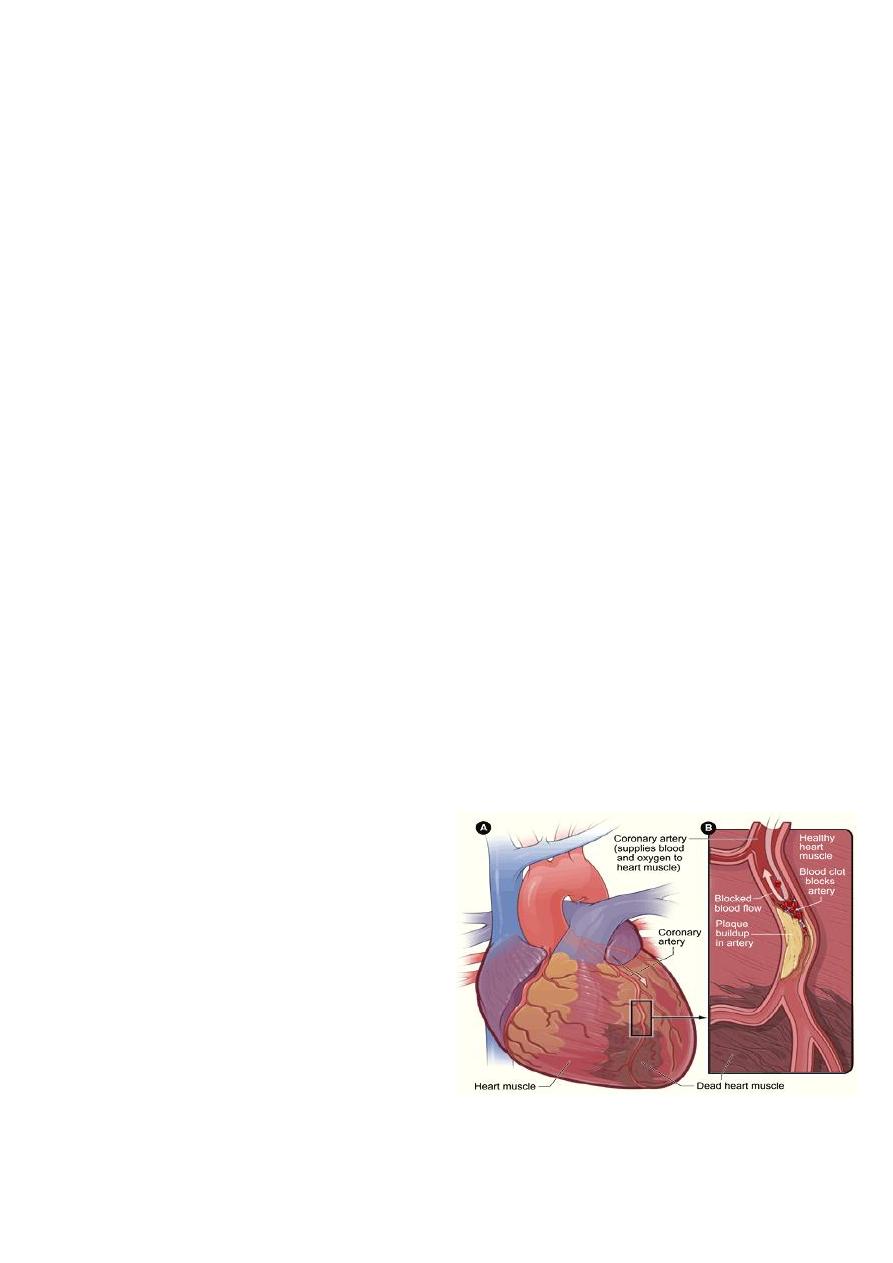
D Myocardial infarction= Myocardial necrosis = acute occlusion of a coronary artery
=plaque rupture or erosion with superimposed thrombosis
D Heart failure=Myocardial dysfunction =infarction or ischaemia
D Arrhythmia Altered conduction = ischaemia or infarction
D Sudden death Ventricular arrhythmia / asystole or /massive MI
ACS:
c Pathology, clinical manifestations,investigations
c Diagnosis and Risk stratification
c Management
- Early in the first 12-hours
- Late in-hospital management
c Complications and risk stratification
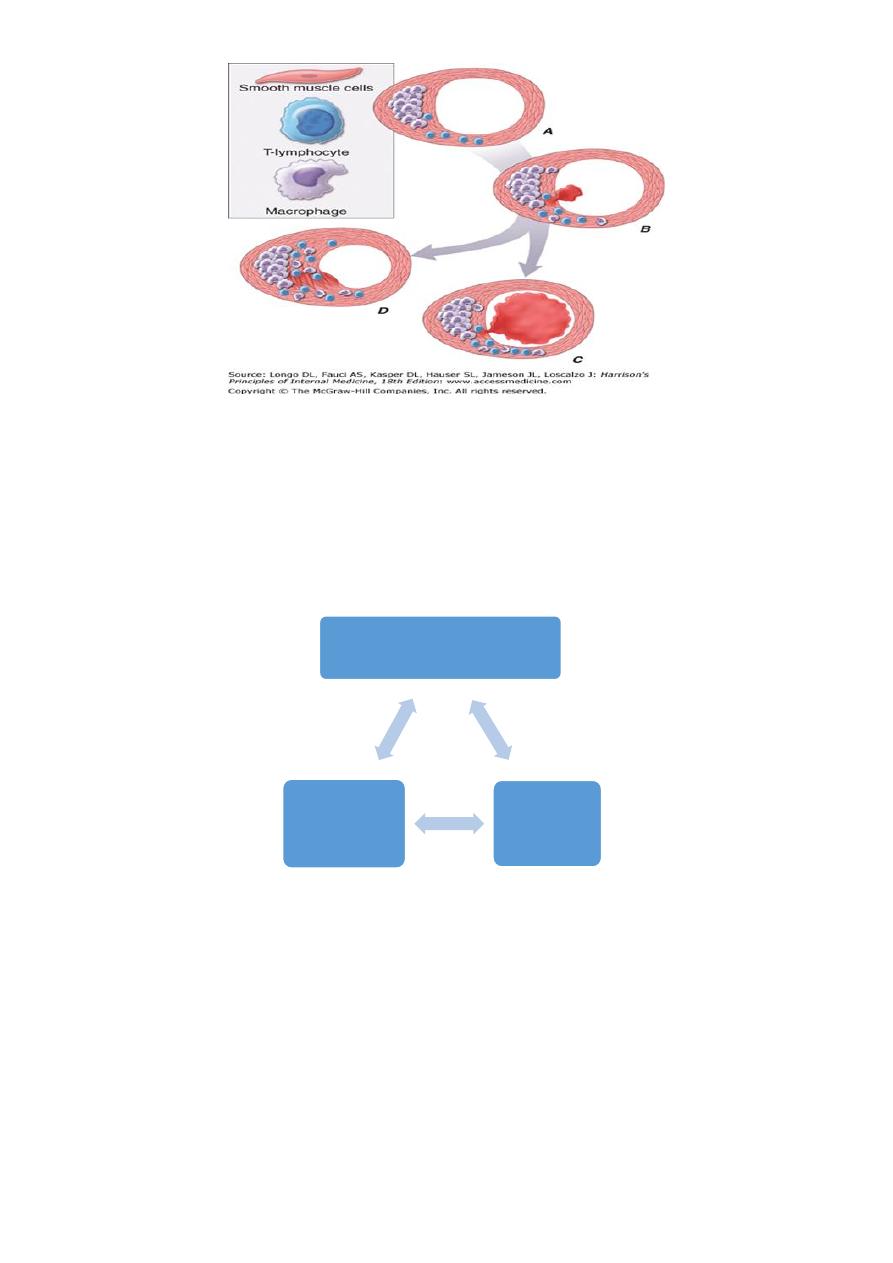
Pathologically
Z Culprit lesion = complex ulcerated or fissured atheromatous plaque + adherent
platelet-rich thrombus + local CA spasm .
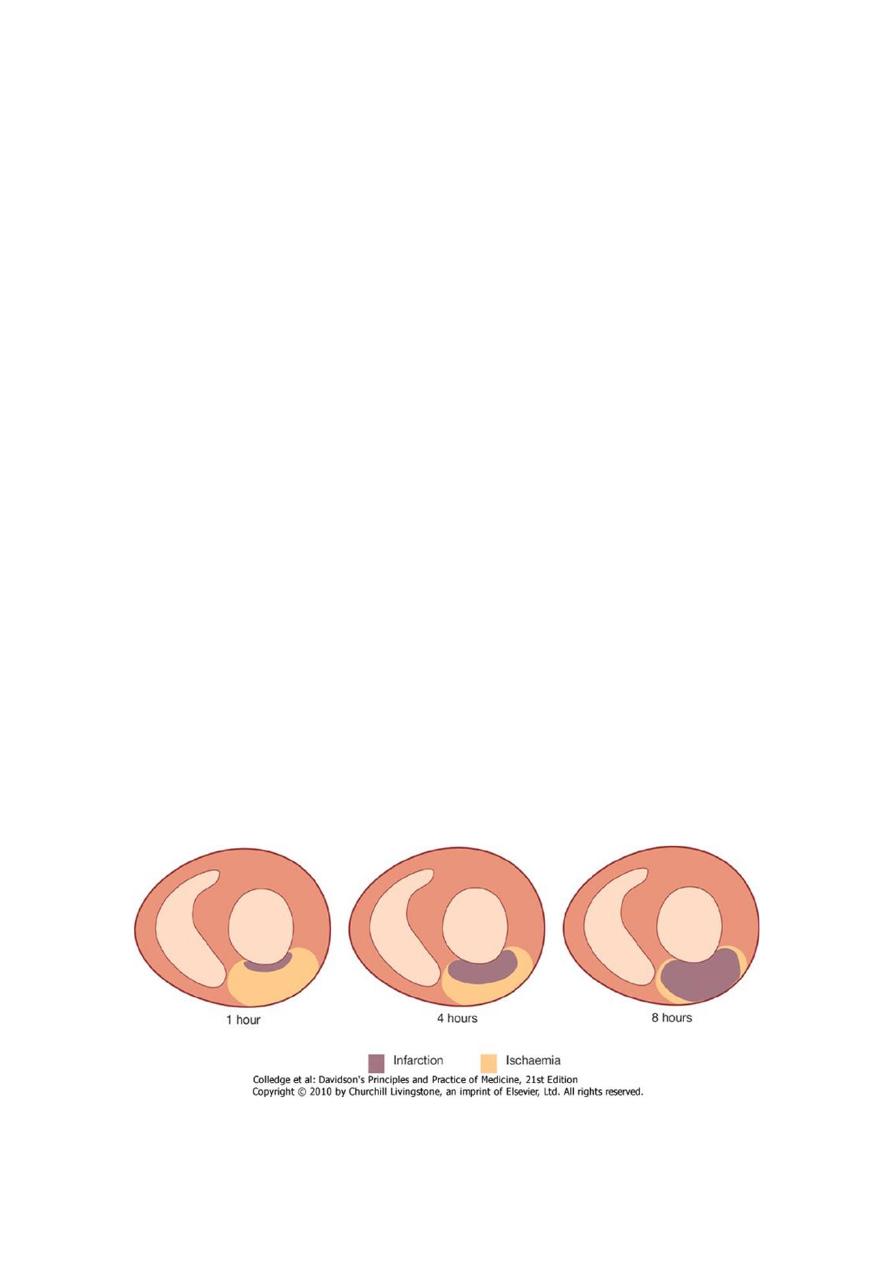
Z Dynamic process =degree of obstruction = increase complete vessel occlusion, or
regress (effects of platelet disaggregation and endogenous fibrinolysis.)
Z Acute MI= occlusive thrombus -at site of rupture or erosion of Ath.plaque
Z thrombus spontaneous lysis over next few days (irreversible myocardial damage
occurred).
Z Without treatment=infarct-related a. permanently occluded in 20-30% process of
infarction progresses over several hours and most p. present -still possible to salvage
myo. and improve outcome
3
Acute coronary syndrome
Both unstable angina and Myocardial infarction
ACS (1) new phenomenon or (2) against background of chronic stable A.
(Stable angina =Angina pectoris =symptom complex = transient myocardial ischaemia
1- Unstable angina =characterised by
1. new-onset or rapidly worsening angina (crescendo angina),
2. angina on minimal exertion or angina at rest . No myocardial damage
2- MI :symptoms occur at rest +evidence of myocardial necrosis (elevation in cardiac
troponin or creatine kinase-MB isoenzyme ) myocardial infarction =evidence of m.
necrosis in a clinical setting consistent with m. ischaemia
ACS
MI
UA
4
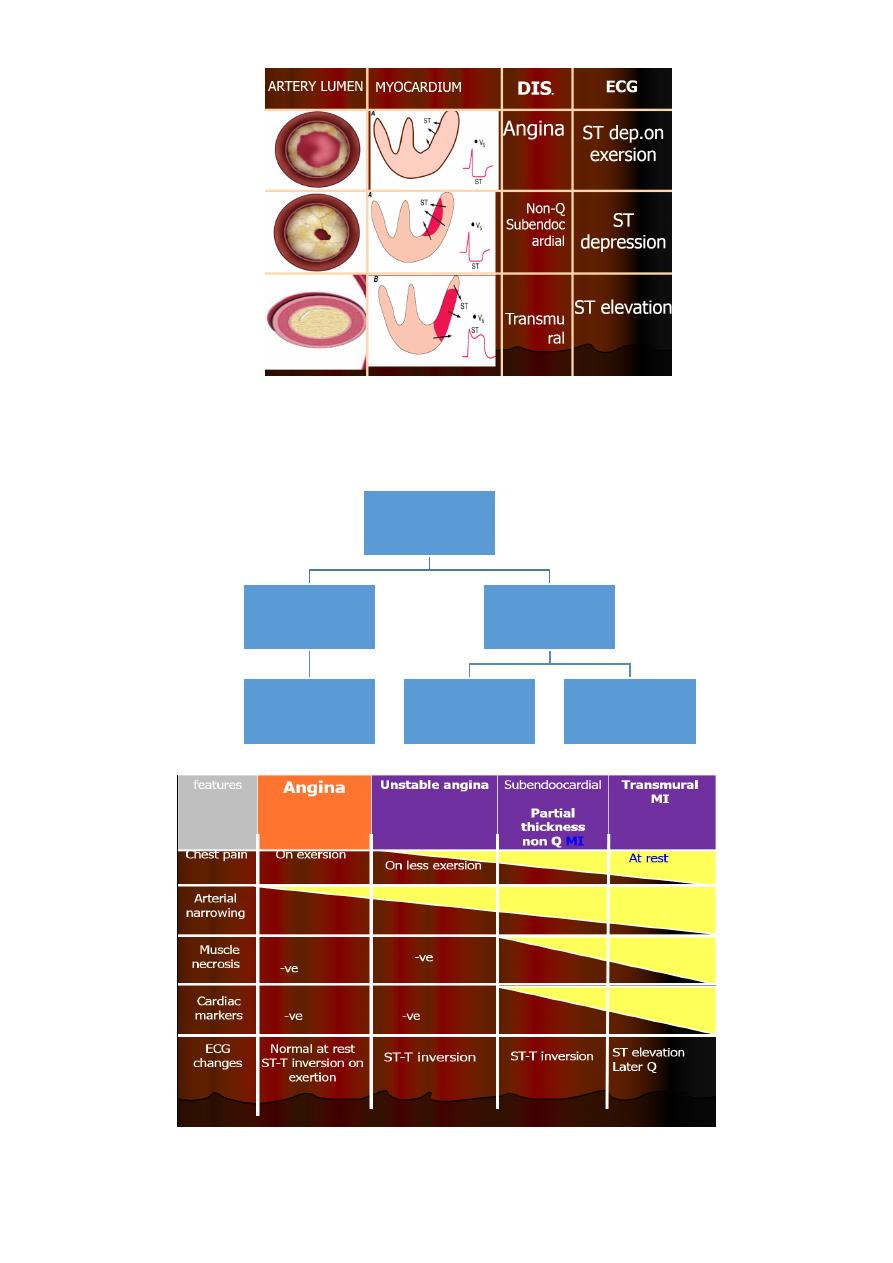
ACS-ECG PRESENTATION
ACUTE
CORONARY
SYNDROME
ST-ELEVATION
MI
TRANMURAL MI
(Q-WAVE MI)
NON-ST
ELEVAT.MI
UNSTABLE
ANGINA
SUB-
ENDOCARD.MI
(NON-Q MI)

5
CLINICAL FEATURES
SYMPTOMS
1. PAIN
2. PAINLESS-SILENT
3. BREATHLESSNESS
4. SYNCOPE
5. SUDDEN DEATH-ARRHYTHMIAS
6. CARDIAC FAILURE
SIGNS
1) GENERAL-SYMPATHETIC AND PARASYMPATHETIC
2) PULSE
3) BP
4) JVP
5) PRECORDIUM
Clinical features
¥ Pain =cardinal symptom, breathlessness, vomiting, and collapse are common features
same sites as angina, more severe , excruciating, and patient's expression and pallor
lasts longer than angina described as a tightness, heaviness or constriction in chest.
- Most patients are breathless (only symptom).
- Painless or 'silent' MI = common in older patients or those with DM.
- MI may pass unrecognised.
¥ syncope =(arrhythmia or profound hypotension).
- Vomiting and sinus bradycardia ( vagal stimulation) -particularly common in
patients with inferior MI.
- Nausea and vomiting(caused or aggravated by opiates given for pain relief).
¥ Sudden death(from VF or asystole) immediately and often within the first hour
- Liability to dangerous arrhythmias remains (If the patient survives this most critical
stage) but diminishes as each hour goes by.
- Development of cardiac failure reflects the extent of myocardial ischaemia major
cause of death in those who survive the first few hours
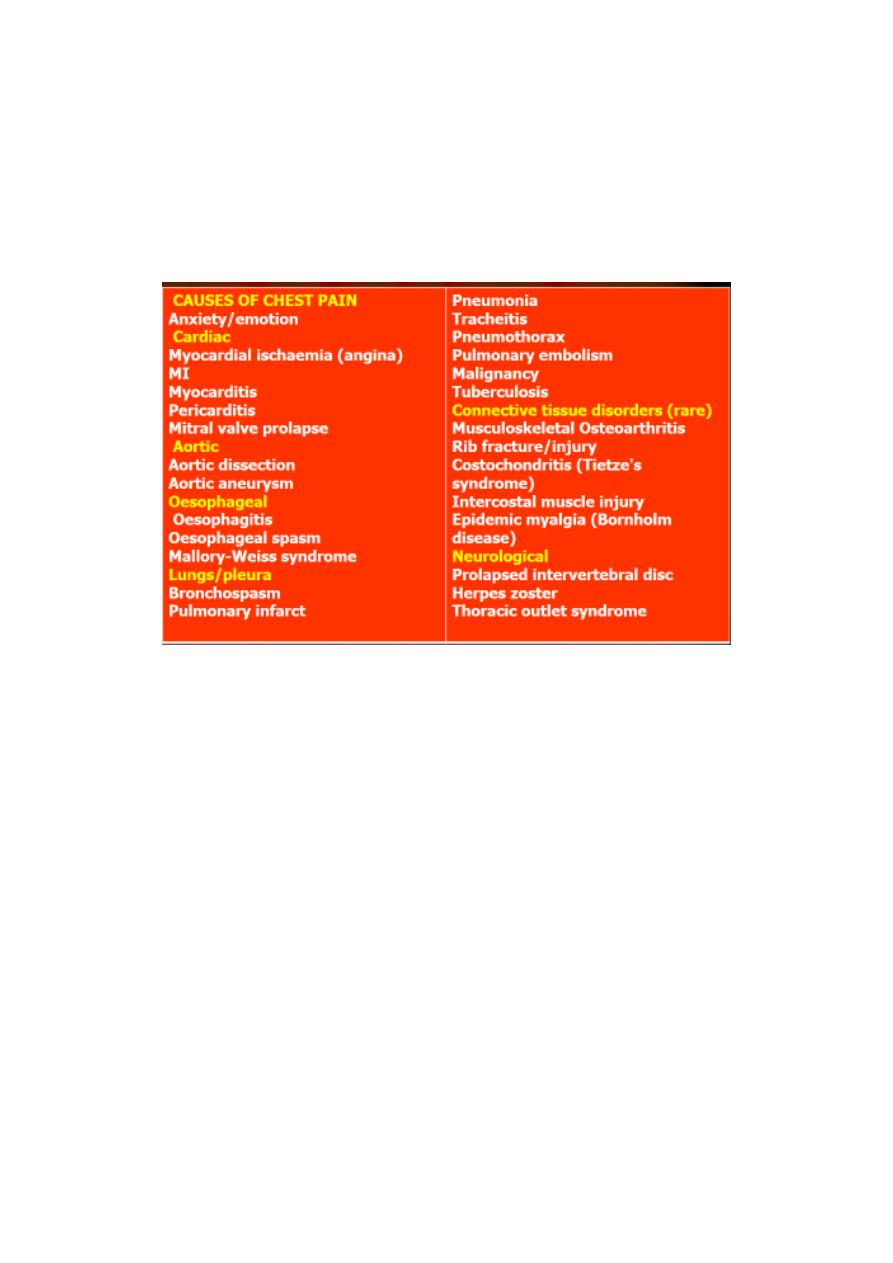
Diagnosis and risk stratification
3 Differential diagnosis includes causes of
1- central chest pain
2- collapse
6
3 Assessment of acute chest pain
3 Risk stratification
3 ECG
3 CARDIAC MARKERS(ENZYMES & PROTEINS)
DIAGNOSIS & DIFFERENTILA DIAGNOSIS
1- central chest pain
2-Shock/collapse:
Causes of circulatory failure or 'shock' -categorised
1) low flow (Low stroke volume )
- Hypovolaemic:
- Cardiogenic:
- Obstructive:
2) low peripheral arteriolar resistance (Vasodilatation )
- Septic/SIRS:
- Anaphylactic:.
- Neurogenic:
3- Syncope and presyncope
Syncope=sudden loss of consciousness =reduced cerebral perfusion.
Presyncope=lightheadedness =.
a. Structural heart disease
b. Neurocardiogenic syncope abnormal autonomic reflexes.
c. Situational syncope identifiable triggers
7
DIAGNOSIS
* CLINICAL
* ECG
* ENZYMES AND PROTIENS(From necrosed muscle)
Universal definition of myocardial infarction
o Detection of rise and/or fall of cardiac biomarkers (preferably troponin), with at least
one value above the 99th percentile of the upper reference limit, together with at
least one of the following:
o Symptoms of ischaemia
o ECG changes indicative of new ischaemia (new ST-T changes or new LBBB)
o Development of pathological Q waves
o Imaging evidence of new loss of viable myocardium or new regional wall motion
abnormality
o Identification of an intracoronary thrombus by angiography of post-mortem
cardiac death, with symptoms suggestive of myocardial ischaemia, and Presumed new
ischemic ECG changes or new left bundle branch block but death occurring before cardiac
biomarkers were obtained ,or before cardiac biomarkers values would be increased
INVESTIGATIONS
1) Electrocardiography (ECG)
2) Plasma cardiac markers
3) Other blood tests
4) Chest X-ray
5) Echocardiography
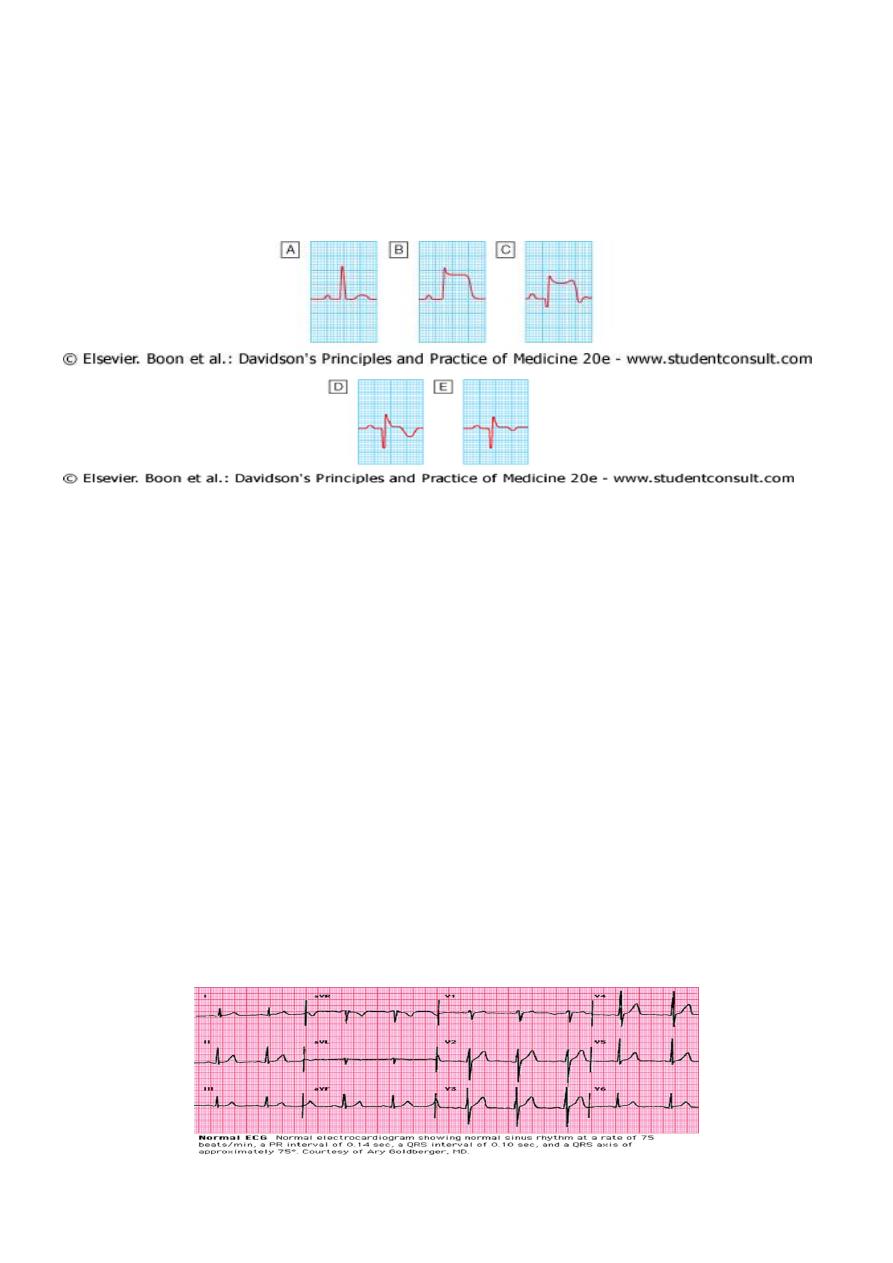
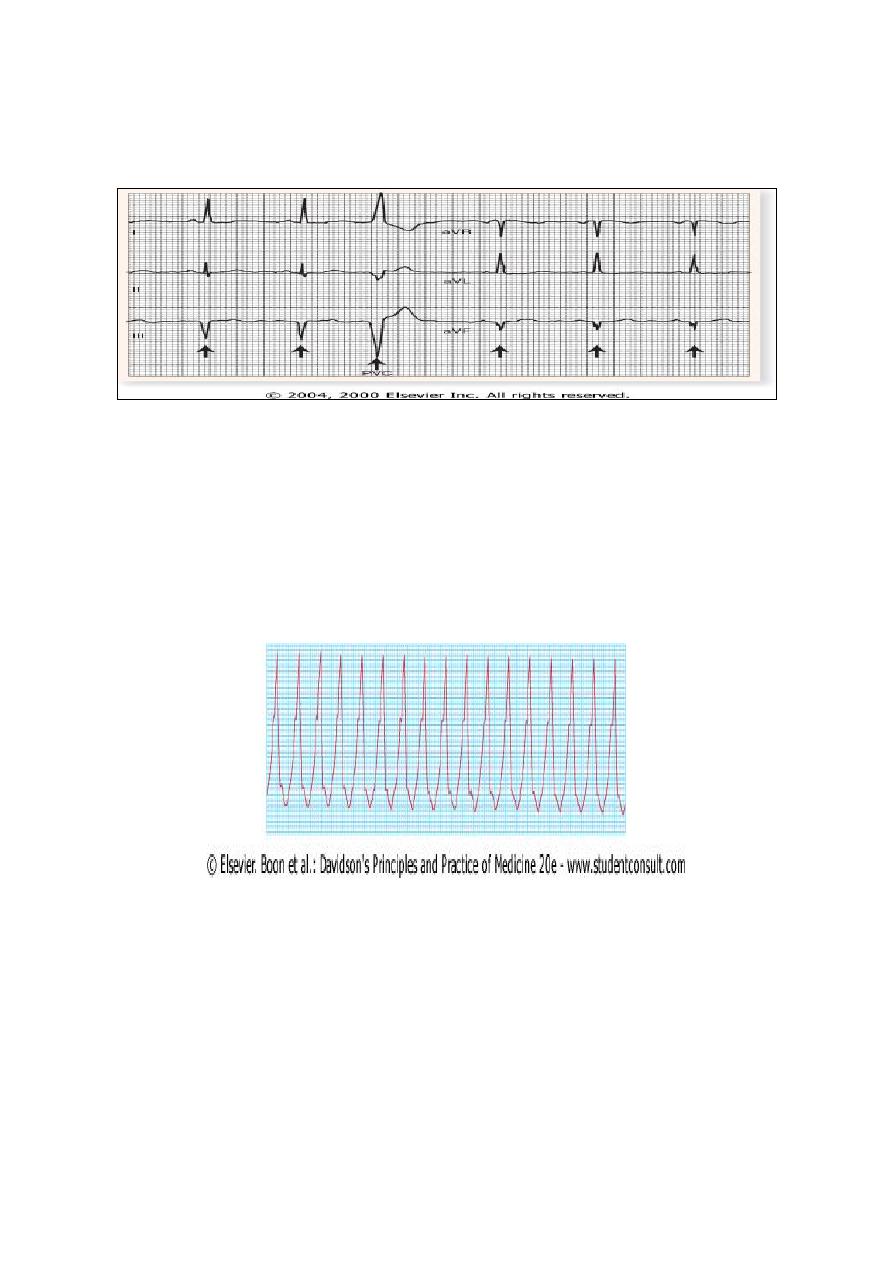
ECG in MI
may be difficult to interpret if there is bundle branch block or previous MI.
Initial ECG may be normal or non-diagnostic in one-third of cases. Repeated ECGs are
important, especially where the diagnosis is uncertain or patient has recurrent or
persistent symptoms
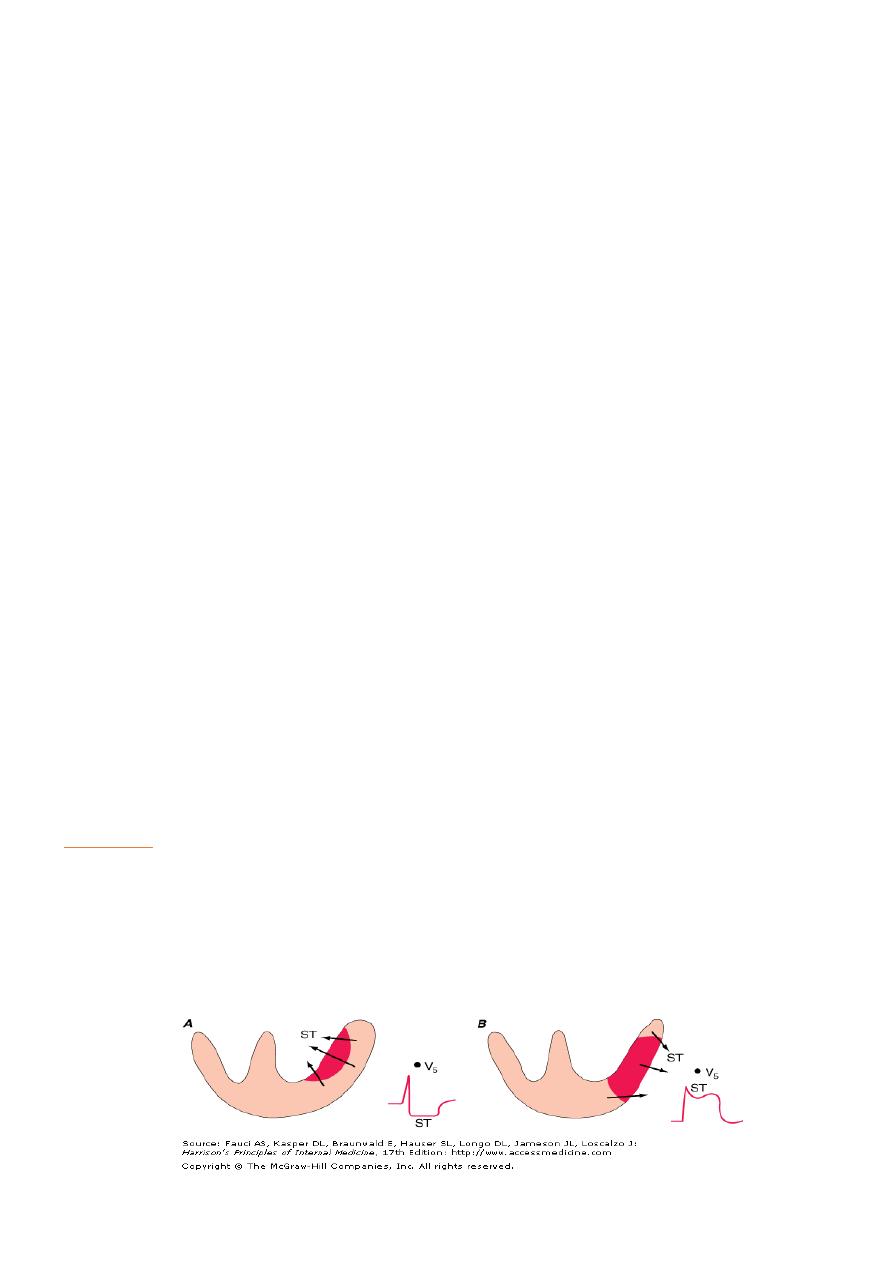
1. ST elevation ACS =proximal occlusion of major coronary a
2. non-ST segment ACS= =partial occlusion of a major vessel or complete occlusion of a
minor vessel
8
1- ST elevation ACS,
` ST-segment elevation (or new bundle branch block) -initially
` later diminution in size of R wave, in transmural (full thickness) infarctionQ wave.
` Subsequently, T wave becomes inverted (change in V. repolarisation) this change
persists after ST segment has returned to normal.
` sequential features sufficiently reliable for approximate age of infarct to
2- non-ST segment ACS unstable angina or partial-thickness (subendocardial) MI.
usually associated with ST-segment depression and T-wave changes.
In the presence of infarction=may be accompanied by some loss of R waves in the
absence of Q waves .
SITE (WALLS)
8 ECG changes best seen in leads that 'face' ischaemic or infarcted area.
8 Anteroseptal infarction=abnormalities in one or more leads from V1 to V4
8 Anterolateral infarction = changes from V4 to V6, in aVL and in lead I.
8 Inferior infarction =leads II, III and aVF, at the same time leads I, aVL and anterior
chest leads may show 'reciprocal' changes of ST depression .
8 Infarction of posterior wall of LV does not cause ST elevation or Q waves in the
standard leads can be diagnosed by the presence of reciprocal changes (ST depression
and a tall R wave in leads V1-V4).
8 Right ventricle=Some infarctions (especially inferior) also involve the RV.
8 identified by recording from additional leads placed over Rt.precordium normal ECG.
9
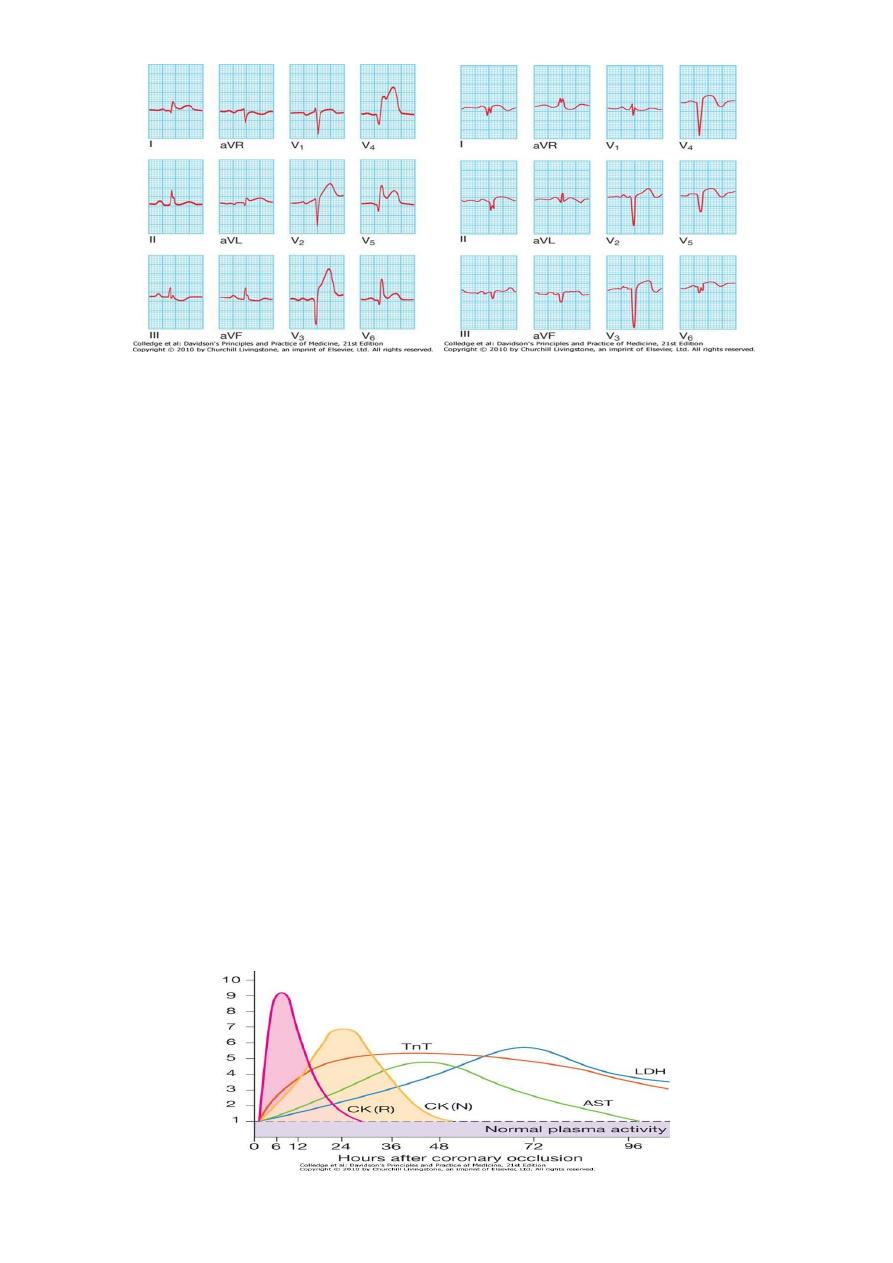
Plasma cardiac markers
E Unstable angina=no detectable rise in cardiac markers or enzymesthe initial diagnosis
is made from the clinical history and ECG only.
E MI = rise in plasma concentration of enzymes and proteins that are normally
concentrated within cardiac cells.
biochemical markers =
1- creatine kinase (CK) more sensitive and cardiospecific isoform of this enzyme (CK-
MB),
2- cardiospecific proteins
- troponins T and I .
- Admission and serial (usually daily) estimations = helpful =change in plasma
concentrations of these markers that confirms the diagnosis of MI .
CK starts to rise at 4-6 hours, peaks at about 12 hours and falls to normal within 48-72
hours. CK is also present in skeletal muscle, and a modest rise in CK (but not CK-MB) may
sometimes be due to an intramuscular injection, vigorous physical exercise or,
particularly in older people, a fall. Defibrillation causes significant release of CK but not
CK-MB or troponins.
Most sensitive markers of myocardial cell damage =cardiac troponins T and I=released
within 4-6 hours and remain elevated for up to 2 weeks
10
Risk stratification
Assessment of acute chest pain depends on
1- analysis of character of the pain and its associated features,
2- evaluation of ECG,
3- serial measurements of biochemical markers of cardiac damage, such as troponin I
and T.
A 12-lead ECG is mandatory and defines initial triage, management and treatment .
1) Patients with ST segment elevation or new bundle branch block require emergency
reperfusion therapy .
2) patients with acute coronary syndrome without ST segment elevation, ECG may show
transient or persistent ST/T wave changes including ST depression and T-wave
inversion.
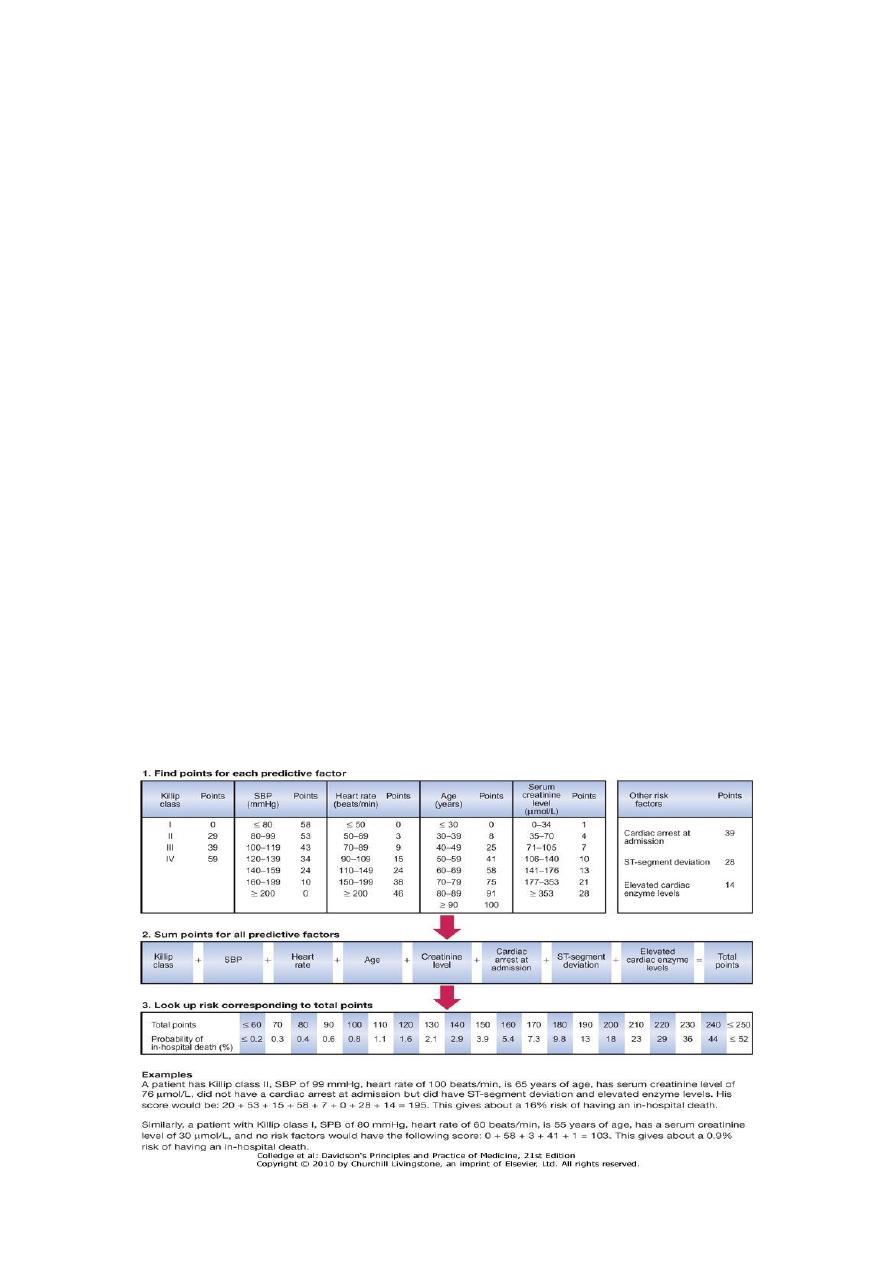
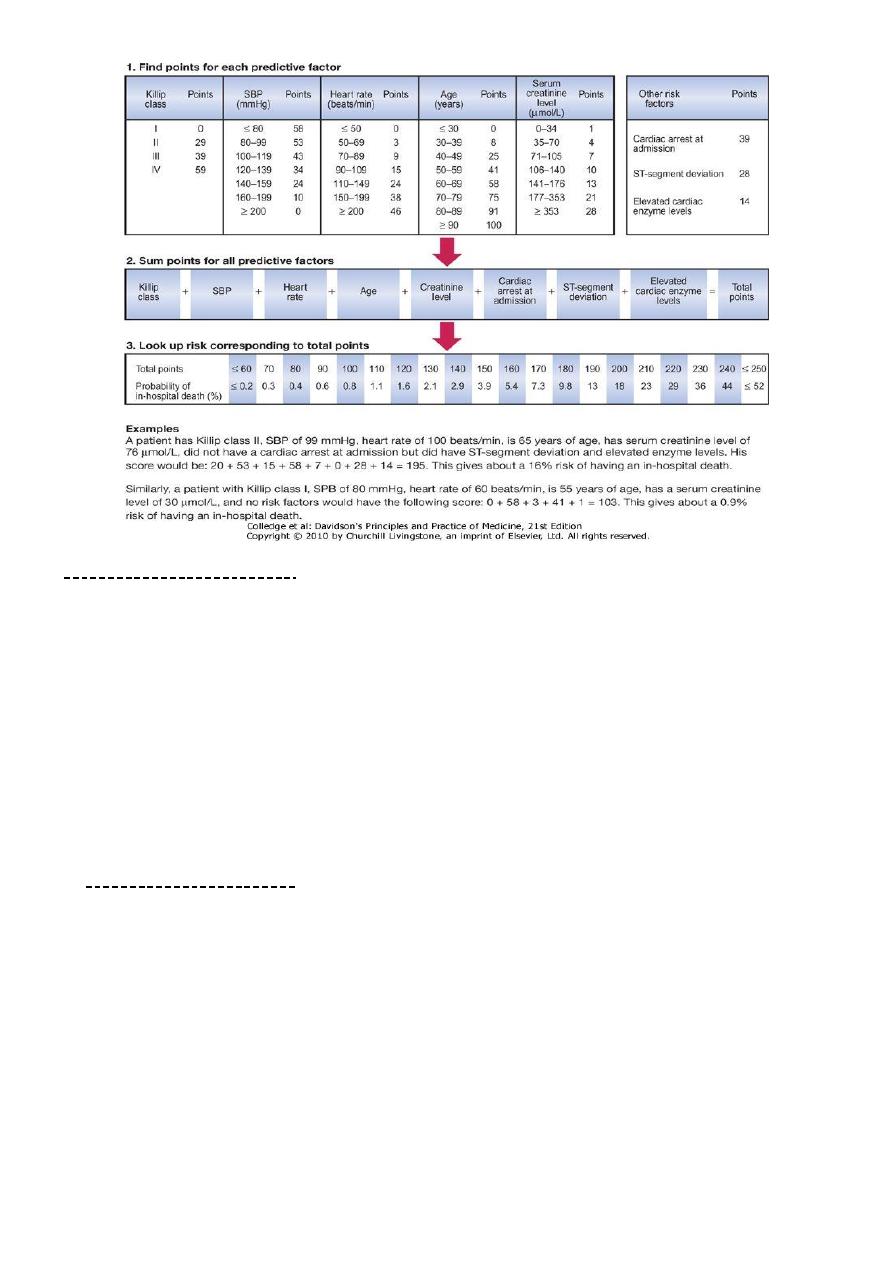
GRACE SCORE
Global Registry of Acute Coronary Events
C Hx of cardiac arrest at admission=39
C Age=0-100(<30->90)
C Dyspnea=killip class(HF)=0-59
C Pulse=0-48(<50->200)
C SBP=0-58(>200-<80)
C ST segment deviation=28
C Enzymes=14
C S.creatinine=1-28(34->353)
11
Risk stratification
Approximately 12% of patients will die within 1 month
fifth within 6 months of the index event.
Risk markers that are indicative of an adverse prognosis
1- recurrent ischaemia,
2- extensive ECG changes at rest or during pain,
3- release of biochemical markers (creatine kinase or troponin),
4- arrhythmias,
5- recurrent ischaemia and
6- haemodynamic complications (e.g. hypotension, mitral regurgitation) during
episodes of ischaemia.
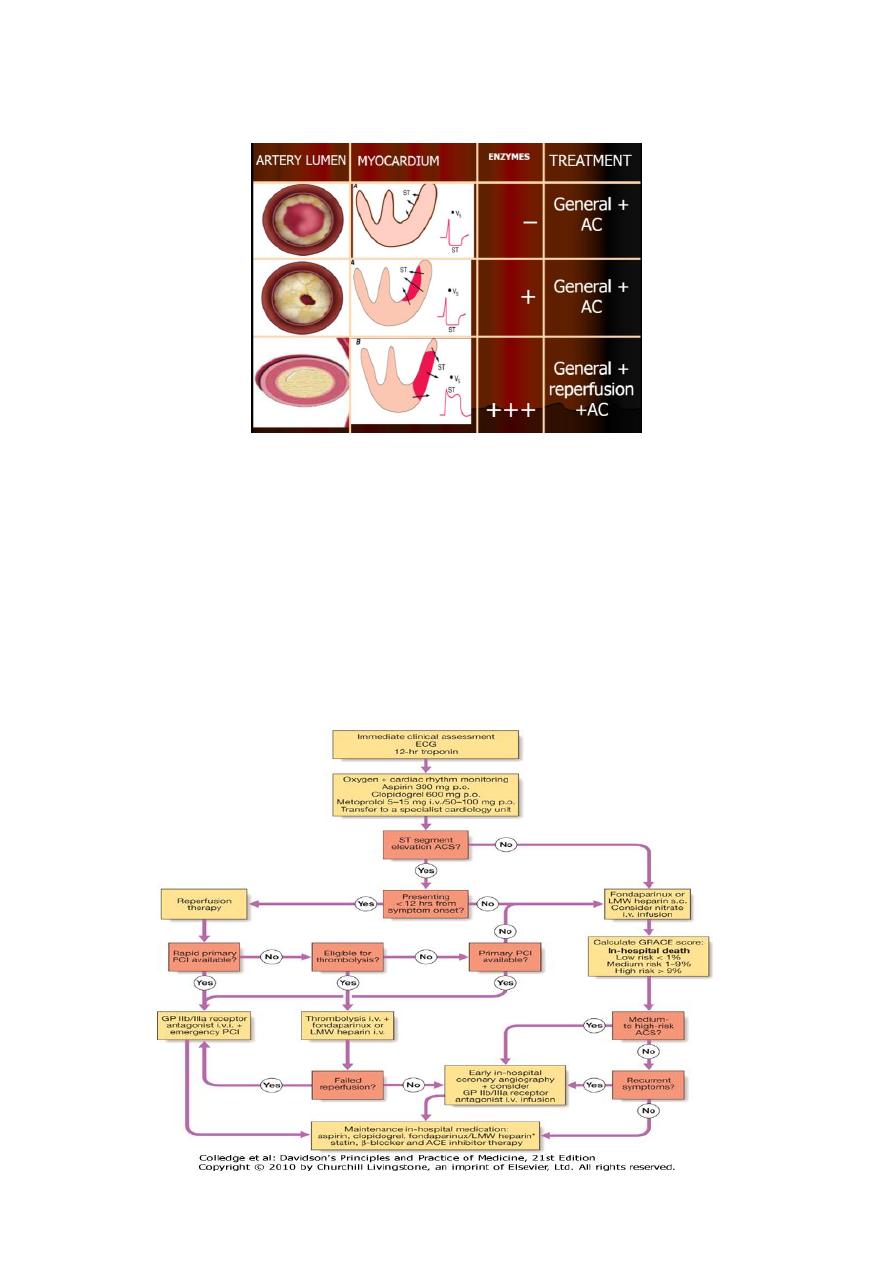
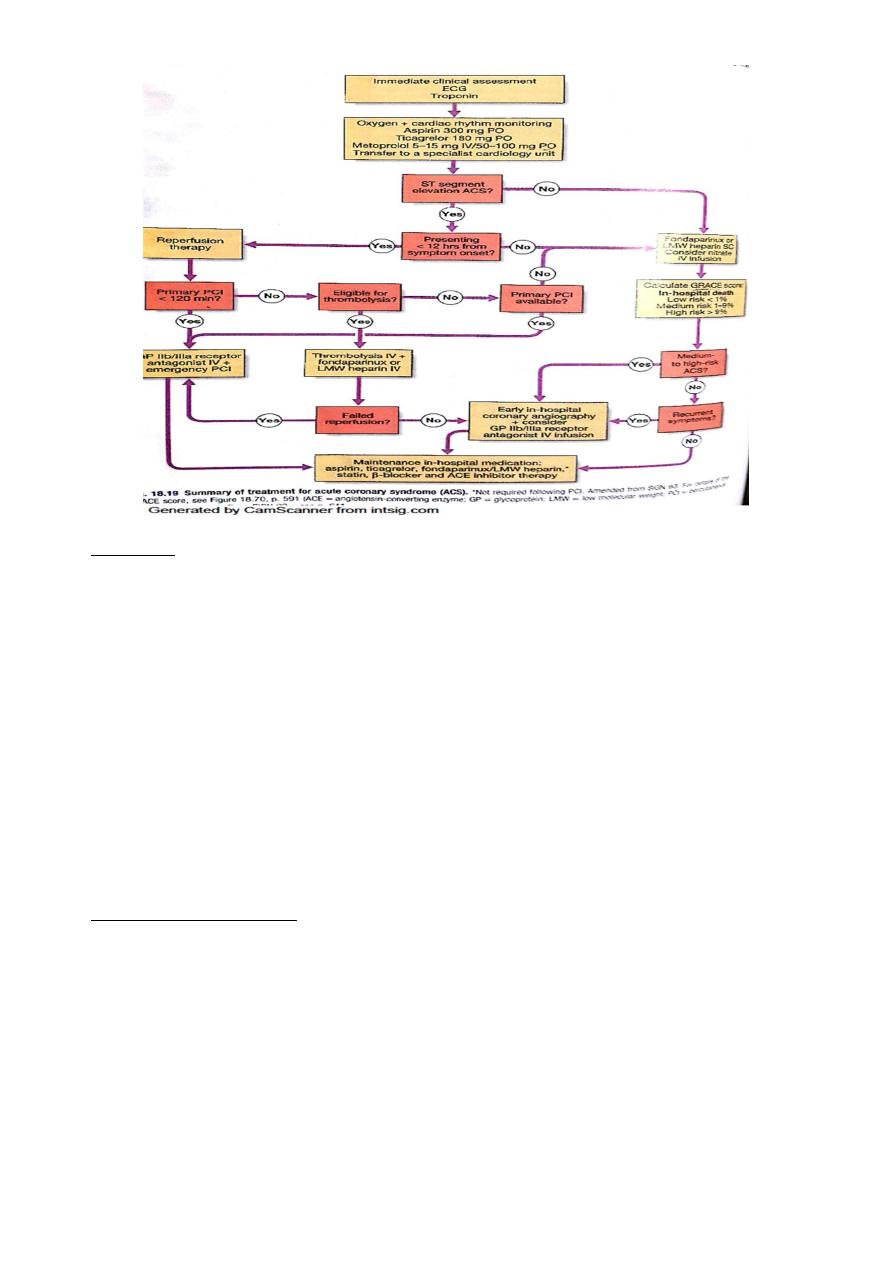
MANAGEMENT OF ACS
IN THE FIRST 12 HR.
O GENERAL ANALGESIA
- ANTI-THROMBOTIC THERAPY
- ANTI-PLATELET
- ANTI-COAGULANT
- ANTI-ANGINAL THERAPY
O SPECIFIC-Reperfusion
TREATMENT OF COMPLICATIONS-
O LATER-AFTER 12 HR :
o risk stratification
o life style change
o mobilization and rehabilitation
o secondary prevention
o device therapy
CAD= CH.STABLE ANGINA
ACUTE CORONARY SYNDROME(ACS)
UA
NON-ST ELEVATION
SUBENDOCARDIAL
NON-ST ELEVATION MI
TRANSMURAL
ST-ELEVATION MI
12
Immediate management:
first 12 hours
Admission urgently to hospital significant risk of death or recurrent myocardial
ischaemia during the early unstable phase,
Appropriate medical therapy can reduce incidence of these by at least 60%.
Patients are usually managed in a dedicated cardiac unit where the necessary
expertise, monitoring and resuscitation facilities can be concentrated.
If no complications --> mobilize from the 2
nd
. Day discharge from hospital after 3-5
days
13
1- Analgesia
Adequate analgesia = essential to
a. relieve distress
b. lower adrenergic drive -->reduc vascular resistance, BP infarct size susceptibility to
ventricular arrhythmias.
IV opiates
o initially morphine sulphate 5-10 mg or diamorphine 2.5-5 mg + antiemetics (initially
metoclopramide 10 mg) = administered and titrated by giving repeated small aliquots
until the patient is comfortable.
o ( IMr injections -avoided clinical effect may be delayed by poor skeletal muscle
perfusion painful haematoma may form following thrombolytic or anti-thrombotic
therapy
2- Antithrombotic therapy
A) Antiplatelet therapy
1. maintain patency of infarct-related artery,
2. reduce tendency to thrombosis and likelihood of mural thrombus formation or
deep venous thrombosis,
1. Aspirin oral -75-300 mg daily (First tablet (300 mg) 25% relative risk reduction
in mortality. continued indefinitely.
2. Clopidogrel 600 mg
150 mg daily for 1 week
75 mg daily with aspirin-
further reduction in ischaemic events .

14
3. ACS with or without ST-segment elevation, ticagrelor (180 mg followed by 90
mg 12-hourly) more effective than clopidogrel in reducing vascular death, MI
or stroke, and all-cause death without affecting overall major bleeding risk
Glycoprotein IIb/IIIa receptor antagonists, (tirofiban and abciximab) block final
common pathway of platelet aggregation potent inhibitors of platelet-rich thrombus
formation. ACS who undergo PCI , recurrent ischaemia those at particularly high
risk,(patients with DM or an elevated troponin ) -
B) Anticoagulants
reduces risk of thromboembolic complications
prevents reinfarction
1. in absence of reperfusion therapy or
2. after successful thrombolysis .
achieved using
unfractionated heparin, fractioned (LMW) heparin or pentasaccharide.
pentasaccharides (s.c fondaparinux 2.5 mg daily) best safety and efficacy low
molecular weight heparin (sc enoxaparin 1 mg/kg 12-hr =alternative.
Anticoagulation -continued for 8 days or until discharge from hospital or coronary
revascularisation.
A period of treatment with warfarin -considered if there is
1- persistent atrial fibrillation or
2- evidence of extensive anterior infarction, or
3- if echocardiography-mobile mural thrombus- (systemic thromboembolism)
3-Anti-anginal therapy
NITRATES: Sublingual glyceryl trinitrate (300-500 μg) -first-aid measure in unstable
angina or threatened infarction, intravenous nitrates (GTN 0.6-1.2 mg/hr or isosorbide
dinitrate 1-2 mg/hr) =treatment of LV failure and relief of recurrent or persistent
ischaemic pain
B-BLOCKERS
Intravenous β-blockers (atenolol 5-10 mg or metoprolol 5-15 mg -over 5 mins) relieve
pain, reduce arrhythmias, improve short-term mortality in patients who present
within 12 hours of the onset of symptoms .
avoided =heart failure (pulmonary oedema) = hypotension (systolic BP < 105 mmHg)
or bradycardia (HR< 65/min).
CALICIUM CHANNEL BLOCKERS
Dihydropyridine calcium channel antagonist (e.g. nifedipine or amlodipine) added to
β-blocker i(persistent chest discomfort )-cause unwanted tachycardia -used alone.

15
Because of their rate-limiting action, verapamil and diltiazem are the calcium channel
antagonists of choice if a β-blocker is contraindicated
4-Reperfusion therapy
ST segment elevation acute coronary syndrome
Immediate reperfusion therapy
- restores coronary artery patency,
- preserves left ventricular function
- improves survival.
Successful therapy is associated with
- pain relief
- resolution of acute ST elevation
- transient arrhythmias (e.g. idioventricular rhythm
Non-ST segment elevation acute coronary syndrome
Immediate emergency reperfusion therapy = no demonstrable benefit in patients with
non-ST segment elevation MI
thrombolytic therapy may be harmful.
Selected medium- to high-risk patients do benefit from in-hospital coronary
angiography and coronary revascularisation but this does not need to take place in
the first 12 hours
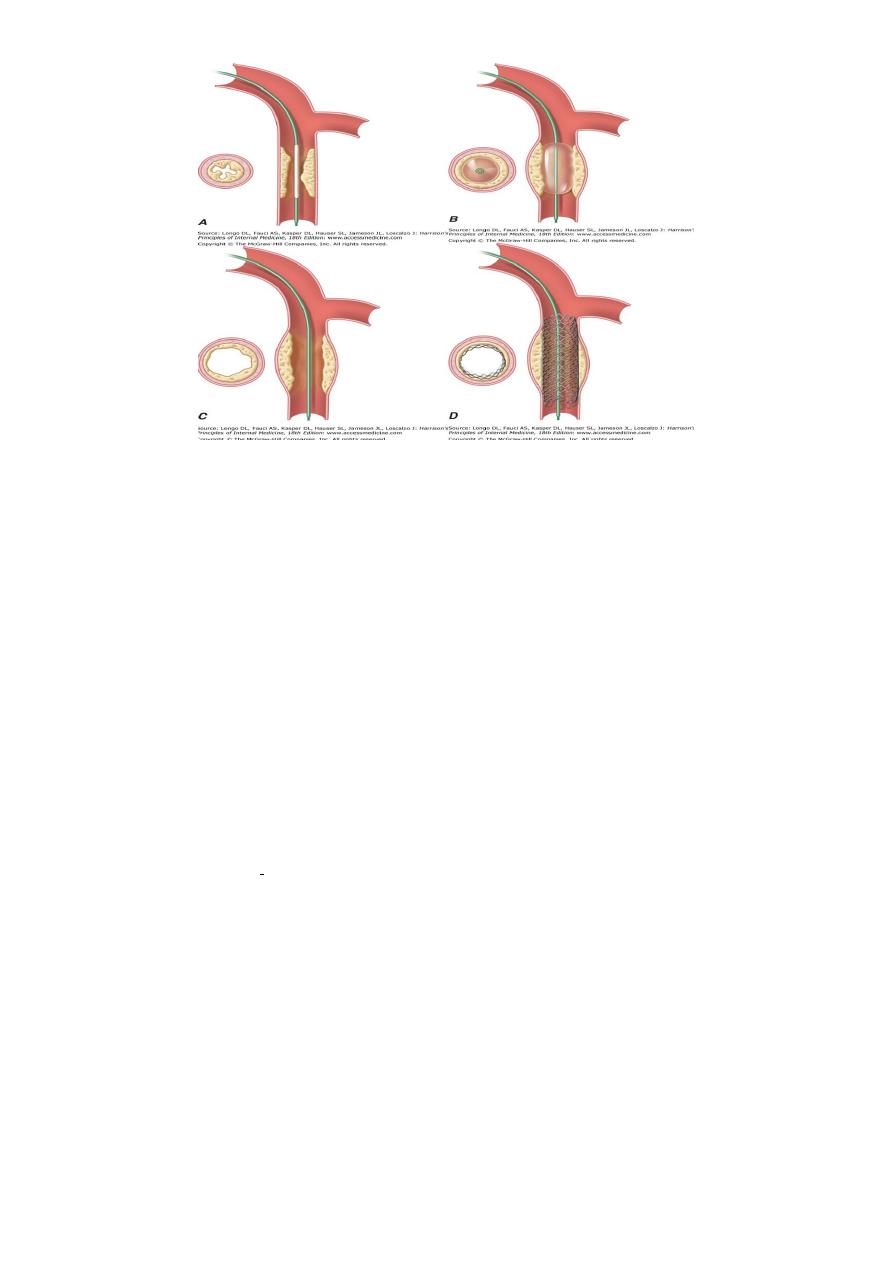
1- Primary percutaneous coronary intervention (PCI)
treatment of choice for ST segment elevation MI . Outcomes are best when it is used
in combination with glycoprotein IIb/IIIa receptor antagonists and intracoronary stent
implantation.
In comparison to thrombolytic therapy, it is associated with a greater reduction in the
risk of death, recurrent MI or stroke
universal use of primary PCI has been limited by availability of the necessary resources
to provide this highly specialised emergency service.
Intravenous thrombolytic therapy =first-line reperfusion treatment in many hospitals,
especially those in rural or remote areas.
When primary PCI cannot be achieved within 2 hours of diagnosis, thrombolytic
therapy should be administered.
16
2-Thrombolysis
Use of thrombolytic therapy = reduce hospital mortality = 25-50% survival
advantage is maintained for at least 10 years .
benefit is greatest in those patients who receive treatment within the first few
hours: 'minutes mean muscle'.
1) Alteplase (human tissue plasminogen activator or tPA) -genetically engineered given
over 90 minutes (bolus dose of 15 mg, -->0.75 mg/kg body wt, but not exceeding 50
mg, over 30 mins and then 0.5 mg/kg body wt, but not exceeding 35 mg, over 60
mins).better survival rates than other thrombolytic agents, such as streptokinase, but
carries a slightly higher risk of intracerebral bleeding (10 per 1000 increased survival,
but 1 per 1000 more non-fatal stroke).
Analogues of tPA, =tenecteplase and reteplase, longer plasma half-life than alteplase
and can be given as IV bolus.
2) Tenecteplase (TNK) is as effective as alteplase major bleeding and transfusion risks
are lower practical advantages of bolus administration may provide opportunities for
prompt treatment in emergency department or in the pre-hospital setting.
3) Reteplase (rPA) is administered as a double bolus and also produces a similar
outcome to that achieved with alteplase, although some of the bleeding risks appear
slightly higher
Thrombolytic therapy
1. reduces short-term mortality in patients with MI if it is given within 12 hours of onset
of symptoms and ECG shows bundle branch block or characteristic ST segment
elevation > 1 mm in the limb leads or 2 mm in the chest leads
17
2. little net benefit and may be harmful in those who present more than 12 hours after
the onset of symptoms in those with a normal ECG or ST depression. benefit greatest
for patients treated within the first 2 hours. major hazard of thrombolytic therapy is
bleeding.
SE
Cerebral haemorrhage causes 4 extra strokes per 1000 patients treated and the
incidence of other major bleeds is between 0.5% and 1%.
treatment withheld if there is a significant risk of serious bleeding .
some patients, thrombolytic therapy is contraindicated or fails to achieve coronary
arterial reperfusion =Early emergency PCI may then be considered, particularly where
there is evidence of cardiogenic shock
RELATIVE CONTRAINDICATIONS TO THROMBOLYTIC THERAPY (POTENTIAL
CANDIDATES FOR PRIMARY ANGIOPLASTY)
Active internal bleeding
Previous subarachnoid or intracerebral haemorrhage
Uncontrolled hypertension
Recent surgery (within 1 month)
Recent trauma (including traumatic resuscitation)
High probability of active peptic ulcer
Pregnancy
COMPLICATIONS OF ACS
Complications of acute coronary syndrome
1. Arrhythmias
2. Ischaemia
3. Heart failure and Acute circulatory
failure
4. Mechanical complications
5. Pericarditis
6. Embolism
7. Impaired ventricular function,
remodelling and V aneurysm
8. Right ventricular infarction
18
Complications of ACS
Functional
1. Left ventricular failure
2. Right ventricular failure
3. Cardiogenic shock
Mechanical
1) Free-wall rupture
2) Ventricular septal defect
3) Papillary muscle rupture with acute mitral regurgitation
Electrical
a) Bradyarrhythmias (first-, second-, and third-degree,atrioventricular blocks)
b) Tachyarrhythmias (supraventricular, ventricular)
c) Conduction abnormalities (bundle branch and fascicular block)
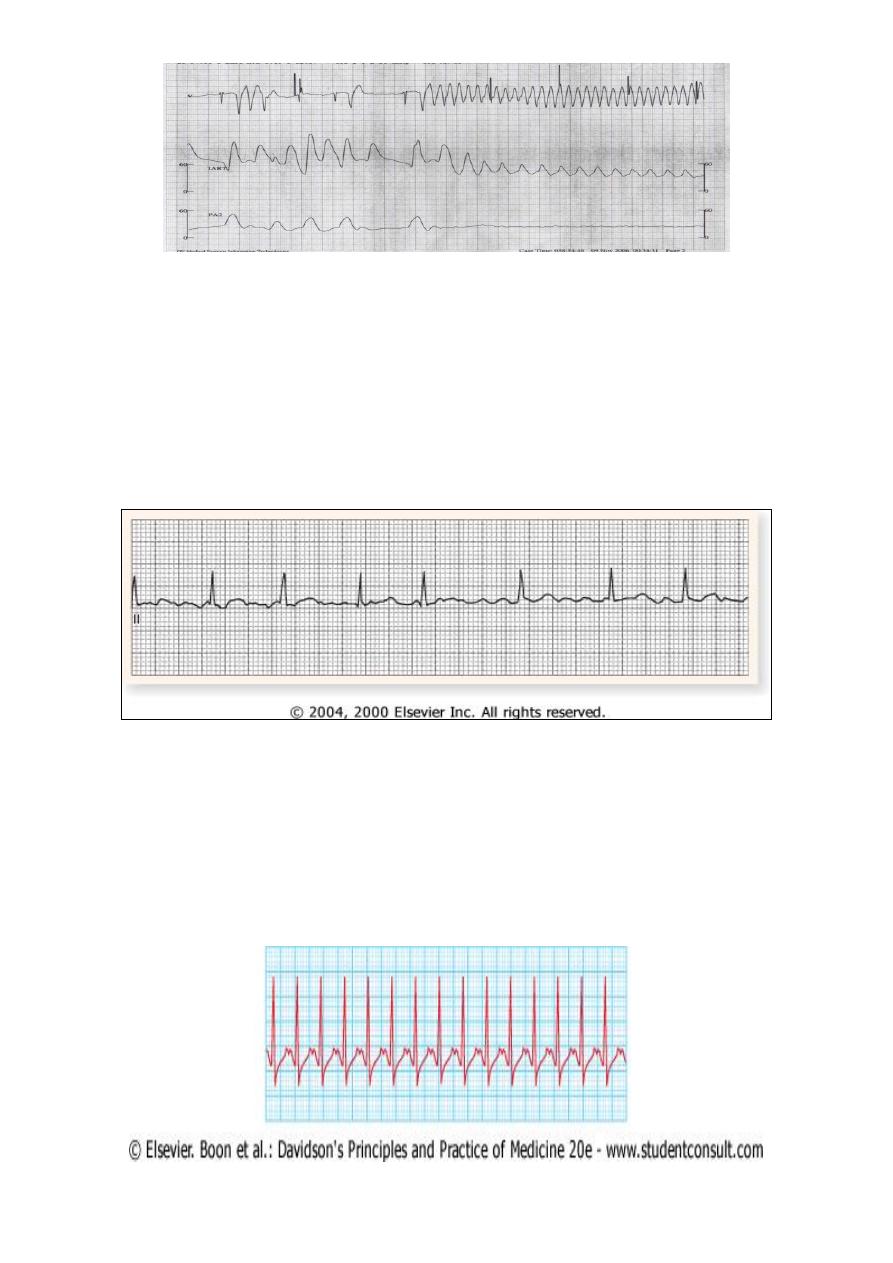
1-Arrhythmias
Common arrythmias complicationg MI
1. Ventricular fibrillation
2. Ventricular tachycardia
3. Accelerated idioventricular rhythm
4. Ventricular ectopics
5. Atrial fibrillation
6. Atrial tachycardia
7. Sinus bradycardia (particularly after inferior MI)
8. Heart block
Nearly all patients with acute MI have some form of arrhythmia; in many cases this is
transient and of no haemodynamic or prognostic significance.
Various degrees of atrioventricular block are also common.
Pain relief, rest and correction of hypokalaemia can all play a major role in prevention of
arrhythmias
Ventricular Premature Beats
Infrequent, sporadic V premature depolarizations -in almost all patients with STEMI
=do not require therapy.
pharmacologic therapy = for patients with sustained V arrhythmias.
Prophylactic antiarrhythmic therapy = contraindicated for VPB may actually increase
the mortality rate.
19
Beta-adrenoceptor blocking agents are effective in abolishing ventricular ectopic
activity in patients with STEMI and in prevention of ventricular fibrillation.
hypokalemia and hypomagnesemia are risk factors for ventricular fibrillation in
patients with STEMI;
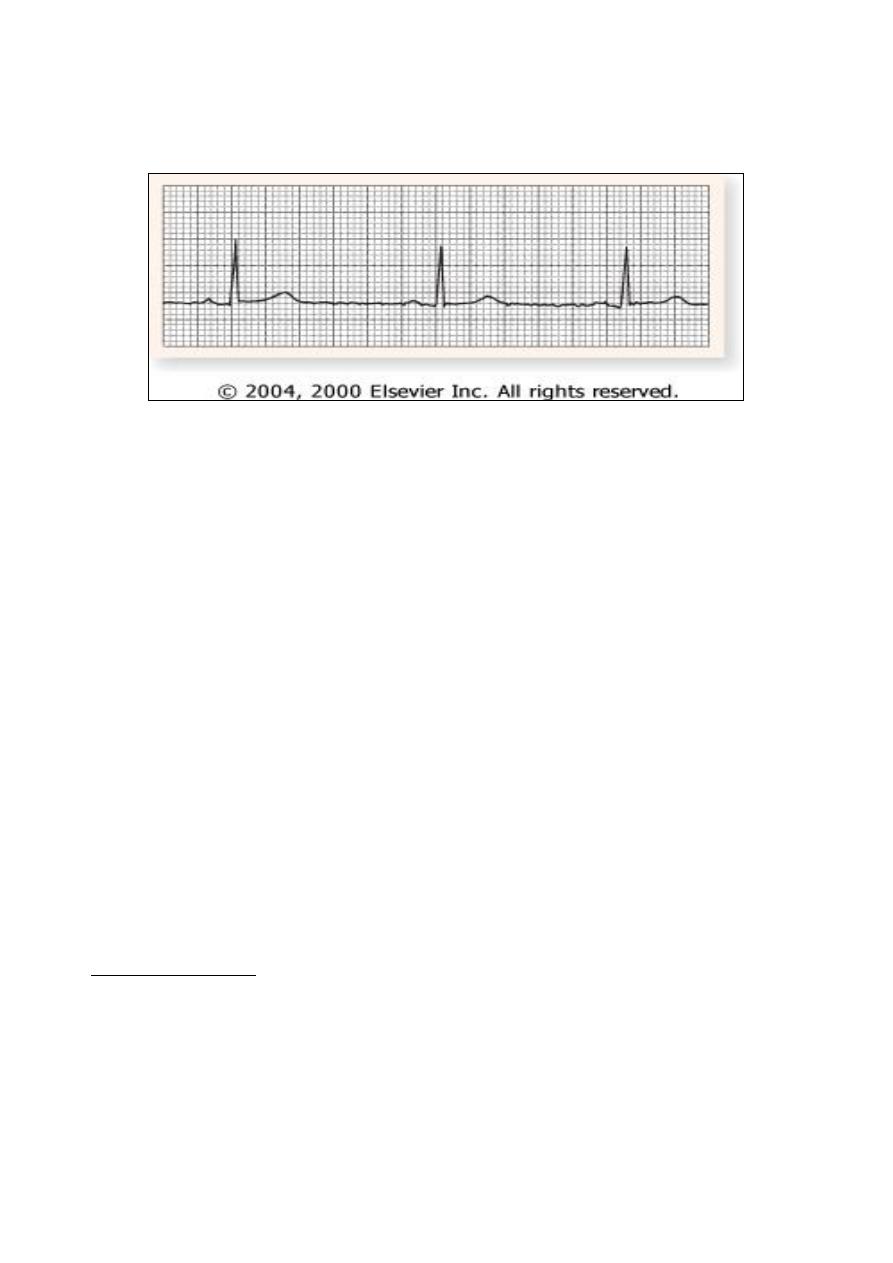
Sustained ventricular tachycardia
A. well tolerated hemodynamically
IV regimen of amiodarone (bolus of 150 mg over
10 min
infusion of 1.0 mg/min for 6 h and then 0.5 mg/min); or Ldocaine may
depress LV function,=hypotension or acute heart failure.
B. if it does not stop or if systolic BP is < 90 mmHg promptly= Synchronised DC
cardioversion (200–300 J VT )hemodynamic deterioration.
Ventricular fibrillation
occurs in about 5-10% of patients who reach hospital, major cause of death in those
who die before receiving medical attention.
Prompt defibrillation usually restore sinus rhythm.
prognosis of patients with early ventricular fibrillation (within the first 48 hours) who
are successfully and promptly resuscitated =identical to the prognosis of patients with
acute MI that is not complicated by VF
Prompt pre-hospital resuscitation and defibrillation have the potential to save many
more lives than thrombolysis
20
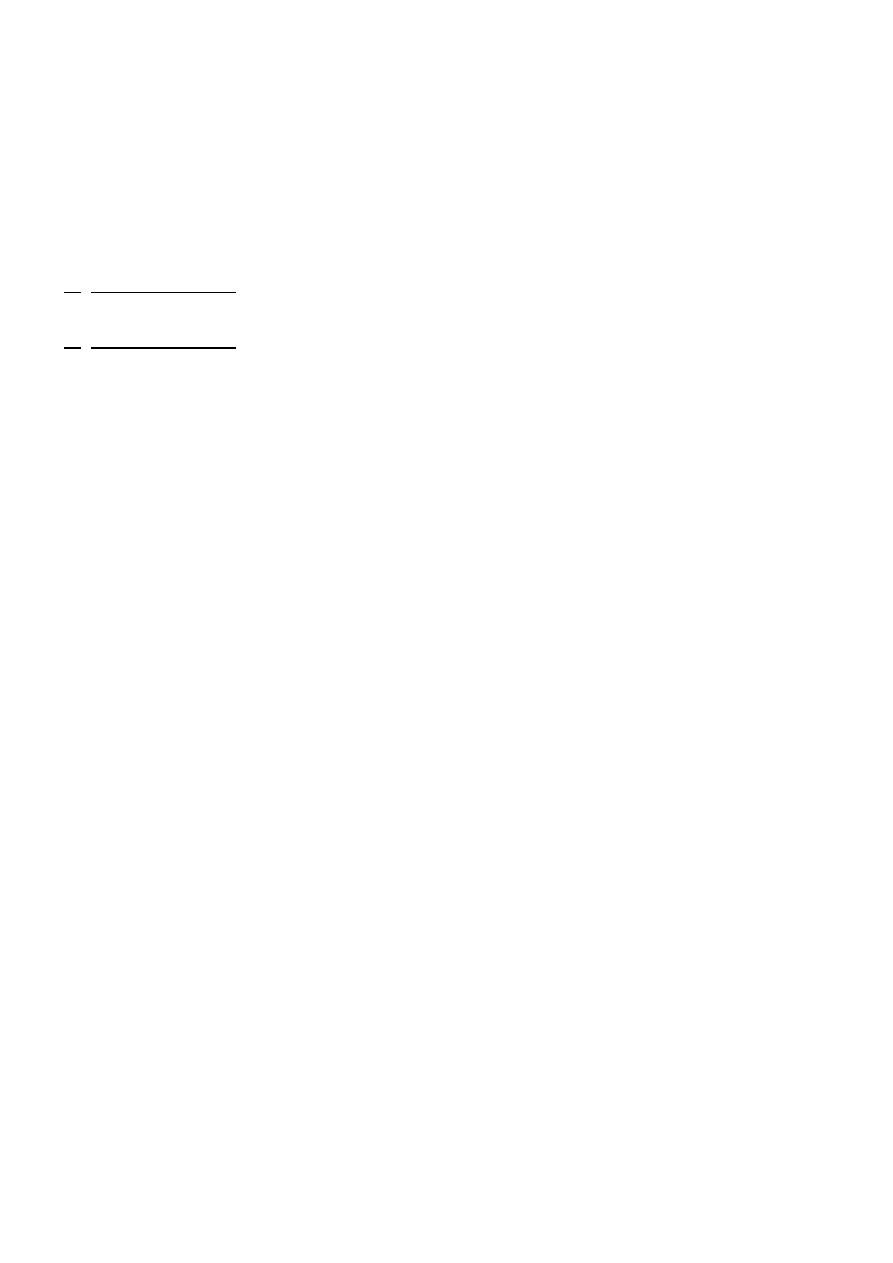
Atrial fibrillation
common, frequently transient =may not require treatment.
if causes a rapid ventricular rate with severe hypotension or circulatory collapse=
cardioversion =immediate synchronised DC other situations, digoxin or β-blockers
usually=treatment of choice.
Atrial fibrillation (due to acute atrial stretch) -feature of impending or overt left
ventricular failure,therapy for heart failure.
Anticoagulation may be required if AF persists
Supraventricular tachycardias
j Digoxin -treatment of choice for supraventricular arrhythmias if heart failure .
j Beta blockers, verapamil, or diltiazem= If heart failure is absent=.
j synchronized electroshock (100–200 J monophasic wave form)=
j If the abnormal rhythm persists for >2 h with ventricular rate >120 bpm, or
j if tachycardia induces heart failure, shock, or ischemia =
21
Bradyarrhythmias
Sinus bradycardia does not usually require treatment hypotension or haemodynamic
deterioration atropine (0.6 mg i.v.).
Atrioventricular block
Atrioventricular block complicating inferior infarction = usually temporary
often resolves following thrombolytic therapymay respond to atropine (0.6 mg i.v.
repeated as necessary).
if clinical deterioration =second-degree or complete atrioventricular block=temporary
pacemaker.
Atrioventricular block complicating anterior infarction = more serious (asystole may
suddenly supervene) == prophylactic temporary pacemaker)
2-Ischaemia
MANAGEMENT
1) recurrent angina at rest or on min exertion following ACS - at high risk
- managed as UA=IV nitrates + IV heparin+Glycoprotein IIb/IIIa RA
- considered for prompt coronary angiography (revascularisation).
2) dynamic ECG changes and ongoing pain = IV glycoprotein IIb/IIIa receptor
antagonists.
3) resistant pain or marked haemodynamic changes
considered for intra-aortic
balloon counterpulsation and emergency coronary revascularisation.
Post-infarct angina occurs in 50% of patients treated with thrombolysis = residual
stenosis in infarct-related vessel ( still viable myocardium downstream). = considered
for early (within the first 6-24 hours) coronary angiography with a view to coronary
revascularisation.
occlusion of a vessel may precipitate angina by disturbing a system of collateral flow
that was compensating for disease in another vessel
22
Early post-MI ischaemia: managed in the same way as patients with high-risk unstable
angina .
1- spontaneous angina=>
2- Patients without spontaneous ischaemia = suitable candidates for revascularisation ==
>exercise tolerance test approximately 4 weeks after the infarct identify individuals
with significant residual myocardial ischaemia
1- exercise test –ve + good effort tolerance,=outlook is good= 1-4% chance of an
adverse event in the next 12 months.
2- exercise test +ve +residual ischaemia = chest pain or ECG changes at low exercise
levels = at high risk
- 15-25% chance of suffering a further ischaemic event in the next 12 months.
- Coronary angiography= angioplasty or bypass grafting
- considered in any patient with spontaneous ischaemia,significant angina on effort,
or a strongly positive exercise tolerance test
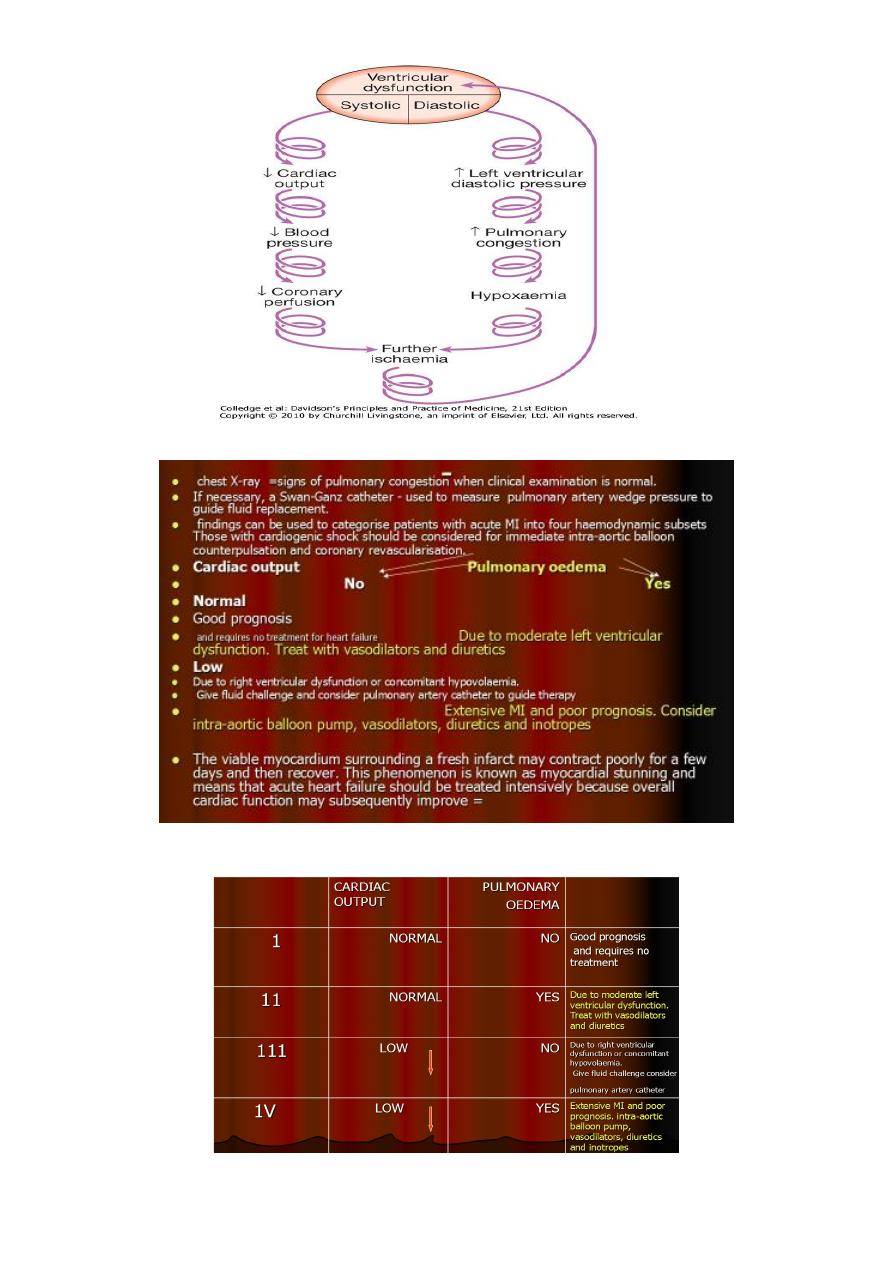
3-Heart failure & Acute circulatory failure
Acute circulatory failure= extensive myocardial damage = bad prognosis.
All other complications of MI = more likely to occur when acute HF is present.
Shock in acute MI
1. left ventricular dysfunction in more than 70% of cases.
2. infarction of the RV
3. a variety of mechanical complications, including tamponade (due to infarction and
rupture of the free wall), an acquired ventricular septal defect (due to infarction and
rupture of the septum) and acute mitral regurgitation (due to infarction or rupture of
the papillary muscles).
Others= pain,arrhythmias,pul.embolism,
Severe myocardial systolic dysfunction = fall in cardiac output, BP and coronary
perfusion pressure.
Diastolic dysfunction = rise in LV end-diastolic pressure, pulmonary congestion and
oedema-->hypoxaemia that worsens myocardial ischaemia=further exacerbated by
peripheral vasoconstriction.
factors combine to create the 'downward spiral' of cardiogenic shock
Hypotension, oliguria, confusion and cold clammy peripheries are the manifestations
of a low cardiac output,breathlessness, hypoxaemia, cyanosis and inspiratory crackles
at the lung bases are typical features of pulmonary oedema.
23
CATEGORIES OF MI+HF

24
Therapy acute MI and resultant LV dysfunction depends on the extent dysfunction.
1. normotensive with symptoms and signs of congestive heart failure (i.e., mild
orthopnea, basilar rales, S3) =Killip class II
- bed rest / salt restriction/ loop diuretic/ low-dose vasodilator ACEI
- digitalis or other inotropic agents invasive hemodynamic monitoring. is not usually
necessary,
2. more severe heart failure (Killip class III or IV)
- hemodynamic assessment.
- Adequate oxygenation.
- urinary catheter,
- IV furosemide = normotensive individual, vasodilator therapy = nitroglycerin and
oral ACE inhibitors
- heart failure and hypotension or an inadequate response to diuretics and
vasodilators = IV inotropic agents (e.g., dopamine or dobutamine)
- mildly hypotensive=dobutamine preferred inotropic agent.
- Dopamine =more severe hypotension
4.Pericarditis
may occur at any stage of the illness particularly common on the second and third
days.
patient recognise that a different pain has developed even though it is at the same
site, and that this pain is positional and tends to be worse or is sometimes only
present on inspiration.
A pericardial rub may be audible.
Non-steroidal and steroidal anti-inflammatory drugs should be avoided in the early
recovery period as they may increase the risk of aneurysm formation and myocardial
rupture.
Opiate-based analgesia should be used.
Post-myocardial infarction syndrome (Dressler's syndrome)
A. characterised by persistent fever, pericarditis and pleurisy, and is probably due to
autoimmunity.
B. symptoms tend to occur a few weeks or even months after the infarct and often
subside after a few days; prolonged or severe symptoms may require treatment with
high-dose aspirin, an NSAID or even corticosteroids.
25
5.Mechanical complications
Part of the necrotic muscle in a fresh infarct may tear or rupture, with devastating
consequences:
1- Papillary muscle damage =acute pulmonary oedema (sudden onset of severe mitral
regurgitation, which presents with a pansystolic murmur and third heart sound).
severe valvular regurgitation=murmur may be quiet or absent. diagnosis =Doppler
echocardiography, and emergency mitral valve replacement may be necessary.
Lesser degrees of mitral regurgitation = papillary muscle dysfunction = common and may
be transient.
2- Rupture of the interventricular septum =left-to-right shunting through a ventricular
septal defect.
sudden haemodynamic deterioration accompanied by a new loud pansystolic murmur
radiating to the right sternal border, may be difficult to distinguish from acute mitral
regurgitation.
acquired ventricular septal defect tend to develop right heart failure rather than
pulmonary oedema.
Doppler echocardiography and right heart catheterisation will confirm the diagnosis.
Without prompt surgery, the condition is usually fatal.
3- Rupture of the ventricle =cardiac tamponade and is usually fatal ,although it may
rarely be possible to support a patient with an incomplete rupture until emergency
surgery is performed
Impaired ventricular function
Remodelling
Acute transmural MI is often followed by thinning and stretching of the infarcted
segment (infarct expansion) ==> increase in wall stress = progressive dilatation and
hypertrophy of the remaining ventricle =ventricular remodelling-.
As the ventricle dilates, it becomes less efficient and HF..
Infarct expansion occurs over a few days and weeks
ventricular remodelling may take years; heart failure =many years after acute MI.
ACE inhibitor = reduces LV remodelling =prevent HF
Left ventricular aneurysm
10%
particularly common -- persistent occlusion of infarct-related vessel.

26
recognised complications
Heart failure, ventricular arrhythmias, mural thrombus and systemic embolism.
But not a cause of wall rupture
Other clinical features paradoxical impulse on the chest wall, persistent ST elevation
on the ECG, sometimes unusual bulge from the cardiac silhouette on chest X-ray.
Echocardiography is usually diagnostic.
Surgical removal of a left ventricular aneurysm carries a high morbidity and mortality
but is sometimes necessary.
Right Ventricular Infarction
one-third of patients with inferior infarction demonstrate at least a minor degree of
RV necrosis.
occasional patient with inferoposterior LV infarction = has extensive RV IN
rare patients present with infarction limited primarily to the RV IN
Clinically significant RV infarction
1. causes signs of severe RV failure [jugular venous distention, Kussmaul's sign,
hepatomegaly with or without hypotension.
2. ECG=ST-segment elevations of right-sided precordial ECG leads, particularly lead V
4
R,
are frequently present in the first 24 h in patients with RV infarction.
3. 2D echocardiography =helpful in determining the degree of RV dysfunction.
4. Catheterization of the right side of the heart often reveals a distinctive hemodynamic
pattern resembling constrictive pericarditis (steep right atrial "y" descent and an early
diastolic dip and plateau in RV waveforms) .
5. Therapy =volume expansion to maintain adequate RV preload
6. efforts to improve LV performance with attendant reduction in pulmonary capillary
wedge and pulmonary arterial pressures.
6.Embolism
Thrombus often forms on endocardial surface of freshly infarcted myocardium==>
systemic embolism
stroke or ischaemic limb.
Venous thrombosis and pulmonary embolism (less common with use of prophylactic
anticoagulants and early mobilisation)
27
LATER IN-HOSPITAL MANAGEMENT
1- Risk stratification and further investigation
2- Lifestyle AND risk factor modification
- Stop smoking
- Regular exercise
- Diet (weight control, lipid-lowering)
3- Mobilisation and Rehabilitation
4- Secondary prevention drug therapy
- Antiplatelet therapy (aspirin and/or clopidogrel)
- β-blocker
- ACE inhibitor
- Statin
Additional therapy for control of diabetes and hypertension
1. Risk stratification and further investigation
Simple clinical tools -used to identify medium- to high-risk patients.
GRACE score =Global Registry of Acute Coronary Events method of calculating
early mortality
help guide which patients should be selected for intensive therapy, and specifically
early inpatient coronary angiograph
----------------------------------------------------------------------------
Hx of C. arrest at admission=39 Age=0-100(<30->90)
Dyspnea=killip class(HF)=0-59 Pulse=0-48(<50->200)
SBP=0-58(>200-<80) ST segment deviation=28
Enzymes=14 S.creatinine=1-28(34->353)
Prognosis of pt .who have survived an acute MI is related to
1- degree of myocardial damage,
2- extent of any residual myocardial ischaemia and
3- presence of significant ventricular arrhythmias.
28
1- Left ventricular function
Degree of LV dysfunction –Crude assessment
1) physical findings (tachycardia, third heart sound crackles at the lung bases elevated
venous pressure etc.),
2) ECG changes
3) chest X-ray=size of heart & presence of pulmonary oedema.
Formal measurements
a. echocardiography or
b. radionuclide imaging
2- early post-MI ischaemia managed as high-risk unstable angina .
A) spontaneous angina=>
B) without spontaneous ischaemia (suitable candidates for revascularisation )
- exercise tolerance test
- approximately 4 weeks after the infarct
- individuals with significant residual m. ischaemia
- further investigation
1. exercise test= -ve + good effort tolerance=outlook good 1-4% chance of an
adverse event in the next 12 months.
29
2. exercise test
+ve= residual ischaemia = chest pain or ECG changes at low exercise
levels are at high risk 15-25% chance of suffering a further ischaemic event in next
12 months.
Coronary angiography+angioplasty or bypass grafting spontaneous ischaemia,
significant angina on effort, or a strongly positive exercise tolerance test
3-Arrhythmias
ventricular arrhythmias during convalescent phase of MI = marker of poor ventricular
function may herald sudden death.
empirical anti-arrhythmic treatment == no value and even hazardous
selected patients may benefit from sophisticated electrophysiological testing and
specific anti-arrhythmic therapy (including implantable cardiac defibrillators,
Recurrent ventricular arrhythmias =
1. manifestations of myocardial ischaemia or
2. impaired LV function may respond to appropriate treatment directed at the
underlying problem
2.
Lifestyle and risk factor modification
1- Smoking
5-year mortality =continue smoke cigarettes double that of those who quit
smoking at the time of their infarct.
Giving up smoking single most effective contribution = own future.
success of smoking cessation increased by supportive advice and nicotine
replacement therapy
2-hyperlipedeimia
O Lipids =measured within 24 hours of presentation (transient fall in blood cholesterol
in 3 months following infarction.)
O Dietary advice =given =often ineffective.
O HMG CoA reductase enzyme inhibitors ('statins') = produce marked reductions in
total (and LDL) cholesterol reduce subsequent risk of death reinfarction stroke need
for revascularisation
O Irrespective of serum cholesterol all patients should receive statin therapy after MI
serum LDL cholesterol concentrations greater than 3.2 mmol/l (∼120 mg/dl) benefit
from more intensive lipid-lowering (e.g. atorvastatin 80 mg daily).
3-Maintaining an ideal body weigh taking regular exercise
4- control of hypertension and diabetes

30
3-Mobilization and rehabilitation
histological evidence =necrotic muscle of acute myocardial infarct takes 4-6 weeks
=replaced with fibrous tissue restrict physical activities during this period.
When there are no complications,sit in a chair on second day,walk to the toilet on
third day, return home in 5 days gradually increase activity =returning to work in 4-6
weeks.
majority of patients may resume driving after 4-6 weeks; (most countries, vocational
driving licence holders (e.g. heavy goods and public service vehicle) require special
assessment.
Emotional problems, = denial, anxiety and depression=common, must be recognised
and dealt with accordingly.
Many patients are severely and even permanently incapacitated as a result of
psychological rather than physical effects of MI, all benefit from thoughtful explanation,
counselling and reassurance at every stage of the illness.
Many patients mistakenly believe that 'stress' was the cause of their heart attack and
may restrict their activity inappropriately.
The patient's spouse or partner will also require emotional support, information and
counselling.
Formal rehabilitation programmes based on graded exercise protocols with individual
and group counselling are often very successful, and in some cases have been shown to
improve the long-term outcome
4-Secondary prevention drug therapy
1. Aspirin and clopidogrel : Low-dose aspirin therapy
reduces the risk of further
infarction and other vascular events by approximately 25% continued indefinitely if
there are no unwanted effects.
Clopidogrel : given in combination with aspirin for at least 3 months If patients are
intolerant of aspirin, clopidogrel is a suitable alternative.
2. Beta-blockers : Continuous treatment =reduce long-term mortality by approximately
25% significant minority of patients do not tolerate β-blockers (bradycardia,
atrioventricular block, hypotension or asthma). heart failure irreversible chronic
obstructive pulmonary disease or peripheral vascular disease derive similar if not
greater secondary preventative benefits from β-blocker therapy if they can tolerate it
3. HMG CoA reductase enzyme inhibitors ('statins') : produce marked reductions in
total (and LDL) cholesterol reduce subsequent risk of death, reinfarction, stroke
need for revascularisation .

31
Irrespective of serum cholesterol concentrations all patients should receive statin
therapy after MI. patients with serum LDL cholesterol concentrations greater than 3.2
mmol/l (∼120 mg/dl) benefit from more intensive lipid-lowering (e.g. atorvastatin
80 mg daily).
ACE inhibitors: long-term treatment with an ACE inhibitor (e.g. enalapril 10 mg 12-hourly
or ramipril 2.5-5 mg 12-hourly) can
1) counteract ventricular remodelling,
2) prevent onset of heart failure,
3) improve survival
4) reduce hospitalisation.
- benefit of treatment greatest in those with overt heart failure (clinical or
radiological) extends to patients with asymptomatic LV dysfunction those with
preserved LV function.
- considered in all patients who have sustained a myocardial infarct.
- Caution must be exercised in hypovolaemic or hypotensive patients because the
introduction of an ACE inhibitor may exacerbate hypotension and impair coronary
perfusion.
- In patients intolerant of ACE inhibitor therapy, angiotensin receptor blockers (e.g.
valsartan 40-160 mg daily or candesartan 4-16 mg daily) are suitable alternatives
and are better tolerated.
Aldosterone receptor antagonist: Patients with acute MI complicated by heart failure
and LV dysfunction benefit from additional aldosterone receptor antagonism (e.g.
eplerenone 25-50 mg daily).
Coronary revascularisation AND Device therapy: Coronary revascularisation
Most low-risk patients stabilise with aspirin, clopidogrel, anticoagulation and anti-
anginal therapy, and can be rapidly mobilised.
In the absence of recurrent symptoms, low-risk patients do not benefit from
routine coronary angiography.
Coronary angiography =considered with a view to revascularisation
1- moderate or high risk, including
2- those who fail to settle on medical therapy,
3- those with extensive ECG changes,
4- those with an elevated plasma troponin
5- those with severe pre-existing stable angina.
In these cases coronary revascularisation is associated with short- and long-term
benefits, including reductions in MI and death.

32
Device therapy
Implantable cardiac defibrillators
of benefit in preventing sudden cardiac death in patients who have
severe left ventricular impairment (ejection fraction ≤ 30%) after MI
PROGNOSIS DEATH in MI
$ 25 % of all cases of MI= Die within a few minutes without medical care.
$ 50% deaths from MI occur= Die within 24 hours of the onset of symptoms
$ 40% of all affected patients Die within the first month.
$ prognosis of those who survive to reach hospital much better 28-day survival of
more than 80%.
$ Early death =an arrhythmia
$ later on=outcome determined by extent of myocardial damage.
Unfavourable features =
1- poor left ventricular function,
2- atrioventricular block
3- persistent ventricular arrhythmias.
4- prognosis is worse for anterior than for inferior infarcts.
5- Bundle branch block and high enzyme levels =extensive myocardial damage.
6- Old age, depression and social isolation are also associated with a higher mortality.
Of those who survive an acute attack, more than 80% live for a further year, about 75%
for 5 years, 50% for 10 years 25% for 20 years
MI IN OLD AGE
Atypical presentation: anorexia, fatigue or weakness rather than chest pain.
Case fatality: rises steeply.
Hospital mortality exceeds 25% in those over 75 years old, =five times greater than that
seen in those aged <55 years.
Survival benefit of treatments: not influenced by age. absolute benefit of evidence-
based treatments greatest in older people.
Hazards of treatments: rise with age (e.g. increased risk of intracerebral bleeding after
thrombolysis) and is due partly to increased comorbidity.
Quality of evidence: older patients, particularly those with significant comorbidity, were
under-represented in many of the RCTs that helped to establish the treatment of
myocardial infarction. balance of risk and benefit for many treatments (e.g.
thrombolysis, primary PTCA) in frail older people is therefore uncertain.
