Done By :
Rasha AliDiana Bahaa’
Ruba Khalil
Tabarak Majid
Pediatric Emergencies
Supervised by :
Dr. Hasanein Ghali
Pediatric emergency
Objective:1. Anatomical Differences
2. Initial Assessment & ABCDE Approach
3. Vital signs
4. RESPIRATORY EMERGENCIES:
A) ACUTE UPPER AIRWAY OBSTRUCTION.
1. Acute Dyspnea.
2. Epiglottitis.
3. Croup .
4. Acute Foreign Body Aspiration.
B) STATUS ASTHMATICUS.
5. Anaphylaxis
6. NEUROLOGIC EMERGENCIES.
7. POISINING.
Pediatric Emergencies
Emergency care is about providing the right
care and support in a timely manner
Therefore we start with an emphasis on patient
safety— the ABC—the assessment of airway,
breathing, and circulation.
Emergency Care
Anatomical Differences
Smaller airways• Less blood volume
• Bigger heads
• Vulnerable internal organs
Anatomical Differences, cont'd
• Large tongue in relation to a small oropharynx
• Diameter of the trachea is smaller
• Trachea is not rigid and will collapse easily
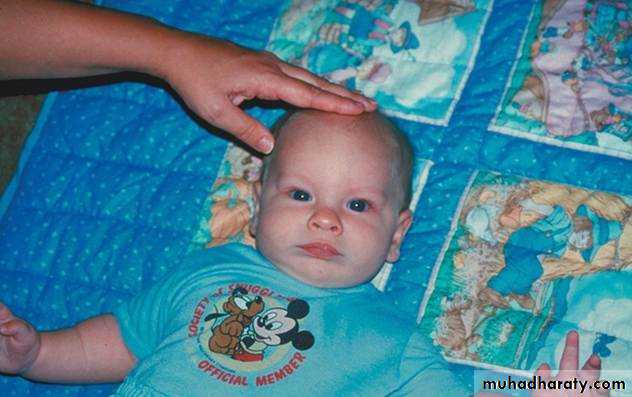
• Back of the head is rounder and requires careful positioning to keep airway open
smaller airway
Anatomical Differences, cont'd
• Relatively smaller blood volume• Approximately 70 cc of blood for every 1kg (2 lbs) of body weight
• A 20 lb child has about 700cc of blood—about the volume of a medium sized soda cup
smaller airway
less blood volume
Anatomical Differences, cont'd
• Head size is proportionally larger• Prominent occiput and a relatively straight cervical spine
• Neck and associated support structures aren’t well developed
• Infants and small children are prone to falling because they are top heavy
less blood volume
bigger heads
smaller airway
Anatomical Differences, cont'd
• Internal organs are not well protected
• Soft bones and cartilage and lack of fat in the rib cage make internal organs susceptible to significant internal injuries• Injury can occur with very little mechanism or obvious signs
bigger heads
internal organs
less blood volume
smaller airway
Initial Assessment
• Begins before you touch the patientform a general impression.
• Determine a chief complaint.
• The Pediatric Assessment Triangle
can help.
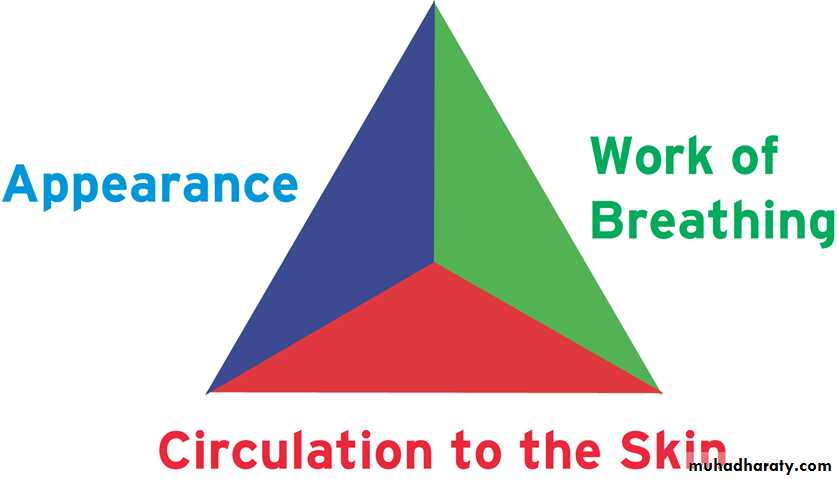
Pediatric Assessment Triangle
• AppearanceAwake
Aware
Upright
• Work of breathing
Retractions
Noises
• Skin circulation
These three clinical indicators reflect the overall status of a child’s cardiovascular, respiratory and neurologic systems.
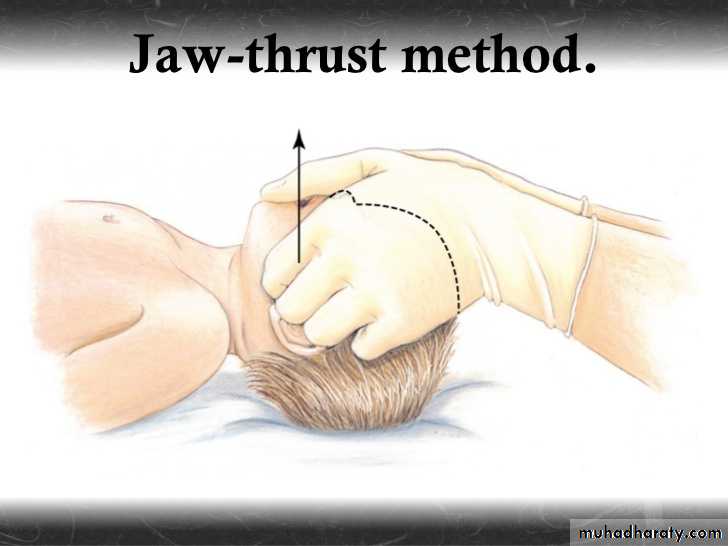
ABCDE Approach to Assessment of the Critically Ill Child
• Airway• Clear
• Maintainable simply
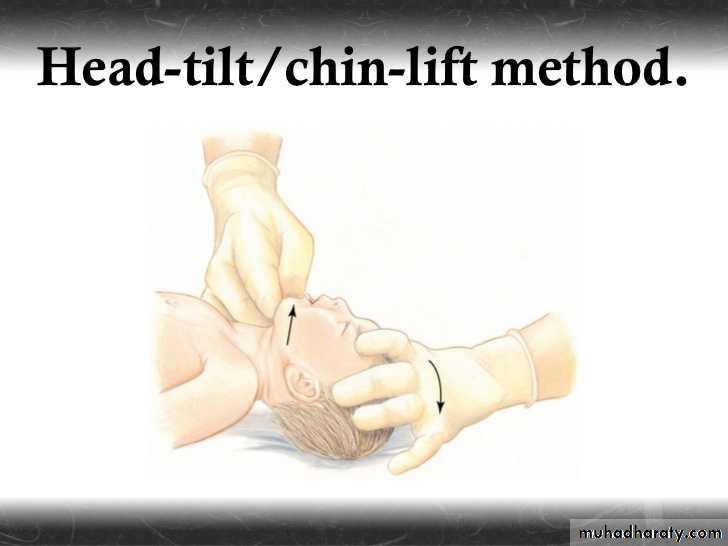
• Head tilt/chin lift (the so-called sniff position)
• Jaw thrust
• Oral and nasal airways
• Unmaintainable
• Removal of a foreign-body obstruction
• Endotracheal intubation
• Percutaneous needle cricothyrotomy
Care of the Pediatric Airway (1 of 2)
Position the airway.Position the airway in a neutral sniffing position.
If spinal injury is suspected, use jaw-thrust maneuver to open the airway.
Care of the Pediatric Airway (2 of 2)
Positioning the airway:Place the patient on a firm surface.
Fold a small towel under the patient’s shoulders and back.
Place tape across patient’s forehead to limit head rolling.
Oropharyngeal Airways
• Determine the appropriately sized airway.• Place the airway next to the face to confirm correct size.
• Position the airway.
• Open the mouth.
• Insert the airway until flange rests against lips.
• Reassess airway.
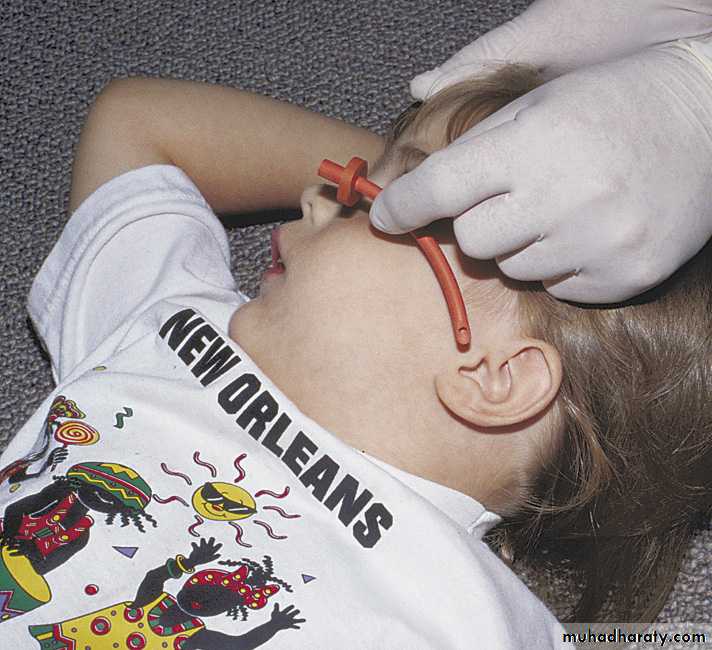
Nasopharyngeal Airways (1 of 2)
• Determine the appropriately sized airway.• Place the airway next to the face to make certain length is correct.
• Position the airway.
• Lubricate the airway.
Nasopharyngeal Airways (2 of 2)
• Insert the tip into the right naris.• Carefully move the tip forward until the flange rests against the outside of the nostril.
• Reassess the airway.
Breathing
• Respiratory rate• Effort
• Retractions
• Use of accessory muscles of respiration
• Nasal flaring
• Grunting
• Air entry/exchange
• Symmetric chest expansion
• Breath sounds
• Paradoxical breathing
• Stridor
• Wheezing
Circulation…
• Color
• Heart rate
• Blood pressure
• Quality/strength of peripheral and central pulses
• Skin perfusion
• Capillary refill time
• Temperature
• Mottling
• End-organ perfusion
• CNS
• Responsiveness (awake, responds to voice, to pain, unresponsive)
• Recognize parents
• Muscle tone
• Pupillary reflexes
• Posturing
• Kidney perfusion
• Urine output >1 mL per kg per hour
A. ASSESSMENT;
Rate, Rhythm.Assess pulses (central and peripheral) and capillary refill (assuming extremity is warm): <2 sec is normal, 2 to 5 sec is delayed, and >5 sec is markedly delayed, suggesting shock .
BP: Measuring blood pressure is one of the least sensitive measures of adequate circulation in children.
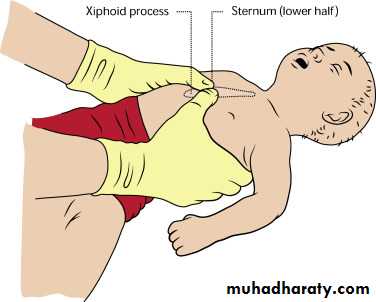
B. MANAGEMENT;
Chest compressions (ensure maximum effectiveness of compressions).
Location[*]
Rate (per min)
Compressions: Ventilation
Infants
1 fingerbreadth below intermammary line
>100
15:2 (2 rescuers)30:2 (1 rescuer)
Pre-pubertal children
2 fingerbreadths below intermammary line
100
15:2 (2 rescuers)30:2 (1 rescuer)
Disability and Exposure
• REALLY D IS FOR DA BRAIN!!!• Cortex
• Brainstem
• Exposure
• Hypothermia
• Significant bleeding
• Petechiae/purpura consistent with septic shock
• Abdominal distension consistent with an acute abdomen
Vital Signs by Age
• Age
• Respirations (breaths/min)
• Pulse (beats/min)
• Systolic Blood Pressure
• (mm Hg)
• Newborn: 0 to 1 mo
• 30 to 60
• 90 to 180
• 50 to 70
• Infant: 1 mo to 1 yr
• 25 to 50
• 100 to 160
• 70 to 95
• Toddler: 1 to 3 yr
• 20 to 30
• 90 to 150
• 80 to 100
• Preschool age: 3 to 6 yr
• 20 to 25
• 80 to 140
• 80 to 100
• School age: 6 to 12 yr
• 15 to 20
• 70 to 120
• 80 to 110
• Adolescent: 12 to 18 yr
• 12 to 16
• 60 to 100
• 90 to 110
• Older than 18 yr
• 12 to 20
• 60 to 100
• 90 to 140
Respirations
Abnormal respirations are a common sign of illness or injury.
Signs of Res. Distress ??
Count respirations for 30 seconds.
In children less than 3 years, count the rise and fall of the abdomen.
Note effort of breathing.
Listen for noises.
Pulse
• In infants, feel over the brachial or femoral area.• In older children, use the carotid artery.
• Count for at least 1 minute.
• Note strength of the pulse.
Blood Pressure
Use a cuff that covers two thirds of the upper arm.If scene conditions make it difficult to measure blood pressure accurately, do not waste time trying.
Skin Signs
Feel for temperature and moisture.Estimate capillary refill.
In infants we can do the capillary refill of the dorsum of the foot
If more than 2 sec it considers abnormal
RESPIRATORY EMERGENCIES
Causes:Acute dyspnea
Nasopharynx : choanal atresia , tonsillar hypertrophy, diphtheria.
Upper airway obstruction : vocal cord dysfunction, croup , epiglottitis.
Lower airway disorder : foreign body bronchitis asthma.
Disordered gas exchange carbon monoxide poisoning, pulmonary oedema, pulmonary hypertension.
Respiratory drive : psychogenic, brain stem tumor.
Neuromuscular : Duchene muscular dystrophy.
Other : pneumothorax.
Management
Clinical assessmentColor: pallor or cyanosis.
Respiratory drive: Pattern and timing of breathing
Upper airway obstruction : produces stridor; lower airway obstruction leads to cough, wheeze, and a prolonged expiratory phase.
Chest and abdominal wall dynamics :may indicate flail-chest, or foreign body inhalation.
Mental state.
Heart rate and perfusion.
Investigations
Non-invasive: pulse oximetry.
Arterial blood gas.Blood tests: FBC, electrolytes, glucose, and cultures.
Chest X-ray.
Treatment
According to ABC RULEThere are specific therapies for each condition In regard to fluid therapy, we generally restrict total volume to 80% maintenance.
Croup
EpiglottitisTime course
Days
Hours
Prodrome
Coryza
None
Cough
Barking
Slightly
Feeding
Can drink
No
Mouth
Closed
Drooling saliva
Toxic
No
Yes
Fever
<38.5°C
>38.5°C
Stridor
Rasping
Soft
Voice
Hoarse
Weak or silent
Epiglottitis
Is a true emergency.
If epiglottitis is suspected, definitive airway placement should precede all diagnostic procedures.Avoid unnecessary
excessive manipulation
visualization of epiglottis
Blood sample
Quick assessment:
(1) unstable (unresponsive, cyanotic, bradycardic), EMERGENCY INTUBATION
(2) stable with high suspicion…DO INTUBATION UNDER GA
(3) stable with moderate or low suspicion..DO XRAY
An “epiglottitis protocol” may include the following:
a. All need intubation + O2 (blow-by).b. Have parent accompany child to allay anxiety.
c. Have physician accompany patient at all times.
d. Call “epiglottitis team” (most senior pediatrician, anesthesiologist, and otolaryngologist in hospital).
e.After airway is secured, obtain cultures of blood and epiglottic surface. Begin antibiotics to cover Haemophilus influenzae type B, Streptococcus pneumoniae, group A streptococci, Staphylococcus aureus.
Epiglottitis may be caused by thermal injury.
Croup (laryngotracheobronchitis)
-Is a viral URTI-Characteristic barking cough
-Children < 3 yrs
MILD
a. Minimal disturbance.b. Antipyretic.
c. Consider oral Dexamethasone 0.15-0.6 mg/kg single dose.
d-Discharge.
Moderate – Severe
-Humidified oxygen.-Neb racemic epinephrine
Can be repeated as often as every 20 min. (Should be used cautiously in tachycardia & CHD).
-Dexamethasone 0.15 – 0.6 mg/kg IM 0r PO once
-Or Neb budesonide 2 mg.
-Observe for 2 -3 hr.
(No stridor at rest. Normal air entery Normal color. Normal level of consciousness)
-Discharge
Progressive stridor.
Sever stridor at rest.Respiratory distress, hypoxia, cyanosis ADMISSION
Depressed mental status.
Need for reliable observation;
Status asthmaticus
It is a medical emergency in which asthma symptoms are refractory to initial bronchodilator therapy in the emergency department.Status Asthmaticus
HistoryPatients have severe dyspnea that has developed over hours to days. Frequently, patients have a prior history of endotracheal intubation and mechanical ventilation, frequent emergency department visits, and previous use of systemic corticosteroids. Patients usually present with audible wheezing.
Physical examination
Patients are usually tachypneic in early stages there is wheezing.
The chest is hyperexpanded, and accessory muscles, are used. Later wheezing may disappear, which may indicate severe airflow obstruction.
Treatment
High concentration of oxygen
humidified if possible.
rehydration
High doses of inhaled bronchodilator
the first choice is short acting beta agonist(salbutamol) given via nebulizer
Inhaled ipratopium bromide via nebulizer
Treatment
Systemic corticosteroids:-intravenous hydrocortisone 10 mg/kg
aminophylline IV 1mg/kg/hour slowly infusion over 20-30 min. with normal saline
Magnesium sulfate
Assisted ventilation
Acute Foreign Body Aspiration
H/O chockingWitnessed event High Index of suspicion
Responsive
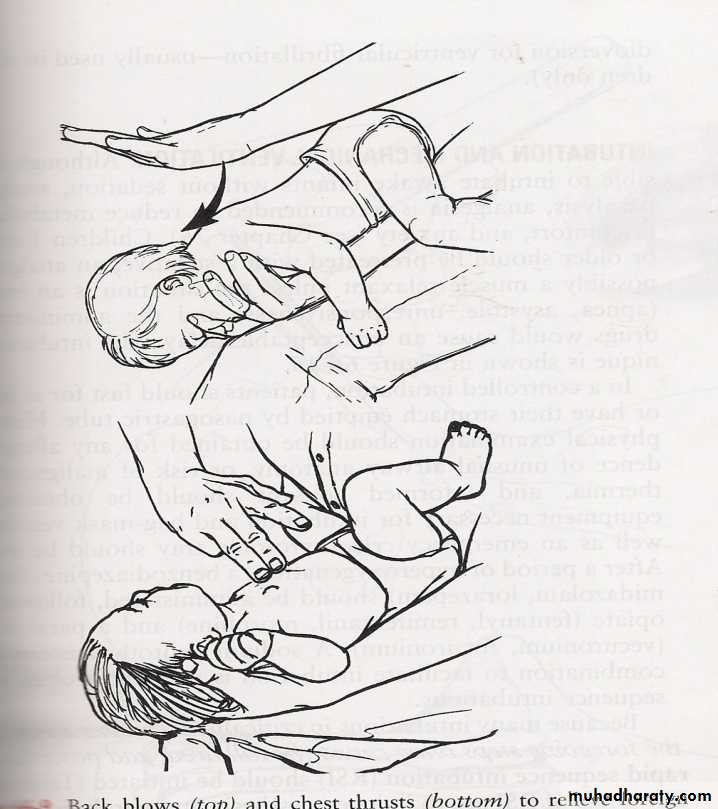
Infant; 1. Hold infant prone. deliver up to 5 back blows forcefully 2. Turn infant supine. Provide up to 5 quick chest thrust. 3. Continue alternating back blows & chest thrust until FB is expelledOR INFANT BECOME UNRESPONSIVE.
Child; Abdominal thrust. Repeat, until: FB is expelled OR unresponsive.
Unresponsive
--- Unable to speak.--- Move air poorly.--- Cyanotic.1. Open mouth by tongue – jaw lift & remove FB if visible only.2. Open the airway by head tilt – chin lift + rescue breath. Breath still not effective:3. Infant ; 5 back blows, 5 chest thrust. Child; Abdominal thrust.4. Repeat step 1 – 3 until the FB expelled & airway is patent OR up to 1 min lasted.
Effective, (Check circulation.CPR as needed. Place child in recovery position).
Ineffective, Ventilate by bag (mask) or ETT.
Remain Ineffective, Consider percutaneous (needle) circothyroidostomy.
Anaphylaxis
Anaphylaxis is a severe, systemic allergic reaction
multisystem involvement, including the skin, airway, vascular system, and GISevere cases may result in complete obstruction of the airway, cardiovascular collapse, and death
Anaphylactoid or pseudoanaphylactic reactions display a similar clinical syndrome, but they are not immune-mediated. Treatment for the two conditions is similar .
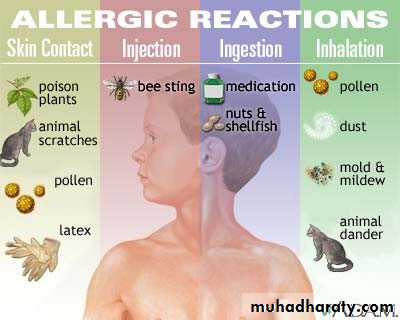
Etiology:
• Pharmacologic agents• Antibiotics especially parenteral penicillins,aspirin , nonsteroidal anti-inflammatory drugs and intravenous (IV) contrast agents.
Latex
Much attention has focused on latex-induced anaphylaxis, but it is actually quite rare.
• Stinging insects
ants, bees, hornets, wasps, and yellow jackets.
Fatal anaphylaxis can develop when a person with IgE antibodies induced by a previous sting is stung
A fatal reaction occurs within 10 to 15 minutes. Cardiovascular collapse is the most common mechanism
Foods
Peanuts, seafood, and wheat are the foods most frequently associated with life-threatening anaphylaxis.
Signs and Symptoms:
Anaphylaxis involves a range of signs and symptoms from hives, wheezing and angioedema to cardiovascular collapse and death.Sneezing.
Coughing.
Itching “pins and needles”sensation on the skin .
Flushing of the skin .
Facial Edema(perioral , oral or priorbital).
Anxiety.
Palpitation.Early respiratory difficulties (eg: wheezing, dyspnea, chest tightness).
Hypotension which may progress to shock and collapse.
Serious upper airway (laryngeal) edema, lower airway edema (asthma), or both may develop, causing stridor and wheezing.
Rhinitis
Cardiovascular collapse is the most common periarrest manifestation
Gastrointestinal signs and symptoms of anaphylaxis include abdominal pain, vomiting, and diarrhea .
Management:
Place the child in a recumbent position (elevating the feet if possible).
Establish and maintain oral airway if necessary.Give oxygen by mask, 10-12 L/min by mask; keep oxygen saturations > 97% to 98%.
Start IV therapy with normal saline to keep vein open, unless severe anaphylaxis and signs of shock are evident.
Administer
Aqueous epinephrine 1:1000,0.01 ml/kg (maximum dose 0.3 ml) SC or IM in the limb opposite that in which the original injection was given.A single SC injection is usually sufficient for mild or early anaphylaxis.
Epinephrine can be repeated twice at 15- 20 minute intervals, if necessary.
In severe reactions it may be necessary to give these repeat doses at shorter intervals (10–15 minutes).
If hypotensive after epinephrine, start IV N/S 20 cc/kg bolus over 20 minutes.
Diphenhydramine 1-2 mg/kg IM or IV, up to 50 mg every 4-6h.Hydrocortisone 5-10 mg/kg up to 500 mg every 4-6h.
Ranitidine 12.5-50 mg IV q6-8h.Monitor Vital signs frequently.
Salbutamol for persistent bronchospasm.
Observe for 6-8 hours minimum with rapid response.
If protracted course monitor for 24 hours.
prevention:
Take a careful patient and family history of allergies.
Be prepared with emergency response.Monitor child for 20 minutes after injection.
Neurological
emrgenciesPediatric seizures
Common causesFever, infections
Hypoxia
Idiopathic epilepsy
Electrolyte disturbances
Head trauma
Hypoglycemia
Toxic ingestion or exposure
Tumors or CNS malformations
A seizure or convulsion is a paroxysmal, time-limited change in motor activity and/or behavior that results from abnormal electrical activity in the brain.
The most important causes in the emergency are:
Status epilipticusFebrile convulsion
meningitis
Febrile Seizures
Result from a sudden increase in body temperatureMost common between 6 months and 6 years.
Commonest age range 9 - 18 months.
Recurrent in up to 50% of children.
Related to rate of increase, not degree of fever
Recent onset of cold or fever often reported
Patients must be transported to hospital
MANAGEMENT:
Routine treatment of a normal infant with simple febrile convulsions includes a careful search for the cause of the fever, active measures to control the fever, including the use of antipyretics, and reassurance of the parents.Undress the child to singlet and underpants to keep cool.
Maintain the airway and prevent injury.
Place patient chest down with head turned to one side.
Oxygen 8 L/min by mask.
Give diazepam by one of two routes:
IV 0.3 mg/kg, undiluted or diluted (10 mg in 20 ml N saline) or rectally 0.5 mg/kg (dilute with saline or in preprepared syringe) up to 10 mg or with suppository or rectal gel.
If continues (status epilepticus protocol).
Status Epilepticus
is a life-threatening condition in which the
brain is in a state of persistent seizure.
Definitions vary, but traditionally it is
defined as one continuous unremitting
seizure lasting longer than 30 minutes,
or recurrent seizures without regaining
consciousness between seizures for greater
than 30 minutes (or shorter with medical
intervention).
Nowadays, even 20 minutes.
Etiology
Three major subtypes:• Prolong febrile condition - younger than
3 years. Rule out CNS infection.
• Symptomatic status - neurological or
metabolic.
• Idiopathic - no underlying cause . Most
common in drug withdrawal plus
aggravating factors. Sleep, inter current
illness
Status as first presentation?
History
• Seizure history including onset, duration,
pattern and associated details.
• Trauma? fever? toxic ingestion?
• If known case of epilepsy then ask
about medication and control?
• DON’T FORGET IMMUNIZATION
• Which vaccine is important??
Pertussis vaccine
Physical ExaminationFocus on:
• Trauma?
• Toxic exposure?
• Infection?
• Vital signs!
• Complete CNS examination including
meningeal signs and look for focal deficit,
eyes signs –papilledema?
Laboratory Evaluation
• Glucose• Electrolytes: Na, Calcium, Phosphate
and Magnesium.
• Blood study for infection screen, WBC?!
so Culture can be considered!
• Drug level and toxicology?
• LP? how is that?
• Neuroimaging: trauma, bleeding, tumor.
Treatment
• Don’t hesitate, always ABC• Positioning: recovery position and
avoid injury
• Reverse potential possible cause,
hypoglycemia for example.
Pharmacological measures?
Can’t get and IV line??
Rectal Diazepam
Can’t get and IV line??Intraosseous infusion needle
Drugs and DosesIf there is no response, repeat the dose after 5-10min
ABC
Establish IV access
Monitor vital signs especially pulse oximetry saturation
Give 100% oxygen via mask
1st line agent anticonvulsants
*IV
Lorazepam 0.1mg/kg
Diazepam 0.2 mg/kg
Midazolam 0.2 mg/kg
*Rectal diazepam 0.5 mg/kg
*IM, intranasal, buccal midazolam
Notes
• 2nd line agents if seizure persists
Load with IV phenytoin (15-20mg/kg, at rate <1mg/kg/min) or
IV phenobarbital (15-20mg/kg, at rate <1mg/kg/min)
• note
>2 years old: phenytoin 15-20 mg/kg IV(or phosphenytoin equivalent)
<2 years old: phenobarbital 10-20
mg/kg IV
Dosing information
DoseTreatment
Seizure etiology
Use 2 ml/kg D25 or 5 ml/kg in neonates
0.5 mg/kg
Glucose
Hypoglycemia
Use 3% NACL over 10-20 min
5-10 ml/kg
Sodium chloride
Hyponatremia
Central IV only, max dose 500 mg, infuse over 10 min
Peripheral or central IV over 10 min, max 1 g
20 mg/kg
60 mg/kg
Calcium chloride
Calcium gluconate
HypocalcemiaInfuse over 10-20 min
25-50 mg/kg
Magnesium sulfate
Hypomagnesemia
Give 5 g IV of 5-10% solution if amount ingested unknown
1 g/g ingested
Pyridoxine
Isoniazid ingestion
Infuse over several min, monitor blood pressure
0.1-0.2 mg/kg
Hydralazine
Hypertension
Give IV to infants with no previous history of seizure
100 mg
Pyridoxine
Pyridoxine dependency
Specific Conditions
Refractory Status
• If previously loaded with phenobarbital,
load with phenytoin
• If previously loaded with phenytoin,
load with phenobarbital
• Endotracheal intubation (avoid use of
prolonged paralytics)
• Other medications: propofol, lidocaine
• Critical care monitoring: midazolam
infusion, general anesthesia, barbiturate
coma
Kerosene ingestion
Hydrocarbons• Description
• Toxic dose varies depending on agent involved and whether it was aspirated, ingested, or inhaled
• Common products:
• Lamp oil
• Gasoline
• Lighter fluid
• Kerosene
• Furniture polish
• Phenol
Definition
Kerosene is a hydrocarbon product of petroleum distillate, made up of paraffin and naphthenes.
In developing countries kerosene is commonly kept in the home, being extensively used for
cooking, heating and lighting. Consequently
accidental kerosene ingestion is often
seen in children in these countries.
Children at Risk
• Developmental characteristics• Peak age 1-4 years, boys more than girls
• Usually it occurs in summer more than winter ??
• Mobile & Curious by nature
• Explore their environment by putting most things in their mouths
• Imitate the behavior of others
• Inability to discriminate a toxic substance from a nontoxic one
• Drawn to attractive packaging and smell of many products found around the home
Children at Risk
• Environmental characteristics
• Toxic substances are often accessible to a child
• Improper storage
• Availability of substances in their immediate environment
• Inattentiveness of caregiver / inadequate supervision
In Our country
• SOCIOECONOMIC STATUSOver 75 % of the patients were from poor families, living in crowded conditions where kerosene is used extensively and where care and supervision of children are suboptimal.
• KEROSENE STORAGE
It is unfortunate that kerosene is usually stored
in unlocked and exposed containers. Containers
are placed on the floor, in the vicinity of
the play areas, within easy reach of infants and
toddlers. As with other studies improper storage
was found to be the main cause
How it affects the body ?
Respiratory system 90% : cough, tachypnea, cyanosisCNS 30% : Varies-restlessness, lightheadedness, rarely seizure and coma etc.
GIT : commonly mild vomiting , diarrhea ,pain.
Fever : persistent for days and it correlates with lung involvement
Assessment of the Child with a Possible Kerosene Ingestion
History:
• How was it taken?• When was it taken?
• Where was the child found?
• How much was taken?
• Amount of liquid
• How much amount available before ingestion?
• How much now in the container?
• Where is the substance stored?
Clinical Features
• Signs/• Symptoms
• Coughing and choking on initial ingestion; gradual increase in work of breathing.
• Odor of kerosene on breath.
• Dry, persistent cough; crackles, wheezes, diminished breath sounds, tachypnea.
• Nausea/vomiting, dizziness, altered mental status, dysrhythmias are possible.
Lab evaluation
• CBC shows leukocytosis ?? Is it infection ??
• Chest X ray is essential But when ??
• What are the findings ??
Chest X-Ray
• Lower lobes more than upper• Right more than left
• Patchy involvement
• Some times bilateral
• Plural effusion and consolidation were reported
• Poor correlation with clinical state.
Treatment
• The whole issue is supportive• Lung is involved or not ??
• ABCs , Oxygen , Bronchodilators, monitor Vitals
• Emesis and Gastric lavage ?
• Activated charcoal ?
• Antibiotics ?
• Steroids ?Follow-up
• Further Inpatient Care
• Patients may be safely discharged home if all of the following conditions are met:
• 1. observed in the emergency department for at least 6 hours
• 2.asymptomatic
• 3.Chest radiograph findings are normal
• They are instructed to return if respiratory symptoms develop
Complications
• Aspiration pneumonitis is the most common complication• Pneumothoraces and barotrauma are potential complications of mechanical ventilation.
• CNS complications include seizures, encephalopathy, and memory loss.
• Myocarditis and cardiomyopathy
With appropriate supportive care, most patients recover without residual complications.
Patient EducationAdvise the parents about the proper storage and labeling of harmful chemicals
Sudden Infant Death SyndromeDefinition - unexplained death of an apparently healthy infant.
Leading cause of death in infants <1 year old
Several known risk factors:
• >Mother younger than 20 years old
• >Mother smoked during pregnancy
• >Low birth weight
• >Putting babies to sleep on stomach
• >Siblings of SIDS babies
SIDS
• >Treat as any patient in cardiac or respiratory arrest
• >Resuscitate unless there is rigor mortis
• >Give emotional support for parents
• >The death of child is very stressful for the family
• >Parents guilt is overwhelming
• >Provide support in whatever ways you can
• >IT IS NOT YOUR PLACE TO JUDGE
• >Allow family time with the infant
Child Abuse and Neglect
Any improper or excessive action that injures or harms a child or infantphysical, sexual, emotional abuse and neglect
More than 2 million cases reported annually
Be aware of signs of child abuse and report it to authorities
Signs of Possible Physical and Sexual Abuse
Slap marks, bruises, abrasions, lacerations, incisionsBroken bones
Head injuries
Abdominal injuries
Bite marks
Burn marks
YOUR ROLE:
Gather information from adults without judgmentTalk with child separately
Plainly and clearly report to medical staff any finding or suspicion regarding physical or sexual abuse
Use terms suspected and possible even when talking to partner, hospital staff, police, and superiors
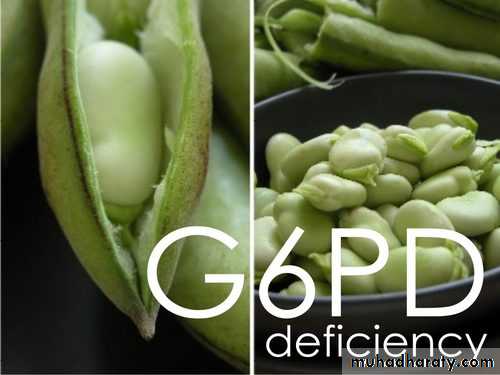
Acute hemolysis
A hemolysis is the premature destruction of erythrocytes.Causes: the most common cause of acute haemolysis is G6PD
Clinical presentation:
-pallor, fatigue, dizziness,
-jaundice
-fever, chills
-dark urine
-headache
-abdominal pain
Signs:
- vital signs: tachycardia, tachypnea & hypotension-ejection systolic murmur
Treatment
>During the attack:
Remove offending drugs and treat any underlying infection
Brisk hydration to ensure adequate urine out put that prevent clogging of renal tubules
Transfusion may be necessary in severe hemolysis (obtain blood sample before transfusion)
>Teaching to avoid oxidant drugs, chemicals and fava beans
>Genetic Consultation, evaluation of family members