Neonatal Examination
Done By :Jaafar Sedqi
Aya Nazar
Dima Amir
Raheeq Abdul Hadi
Supervision
Dr.Numan
The Newborn Examination
Learning ObjectivesClassification of newborn
Estimate the gestational age
Understand Apgar score
Assess vital signs
General Examination
Physical examination
Neurological examination
Classification of newborn
Classification By Birth Weight
Low Birth Weight < 2500 g
Very Low birth weight < 1500 g
Extreme low birth weight < 1000 g
• Classification by Gestational Age
• Preterm <37 wksFull term 37-42
Postterm >42 Wks
Classification
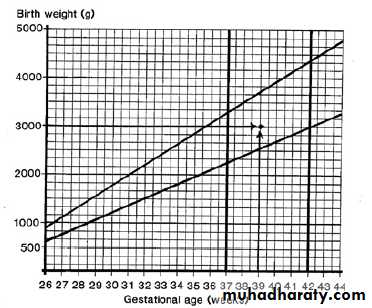
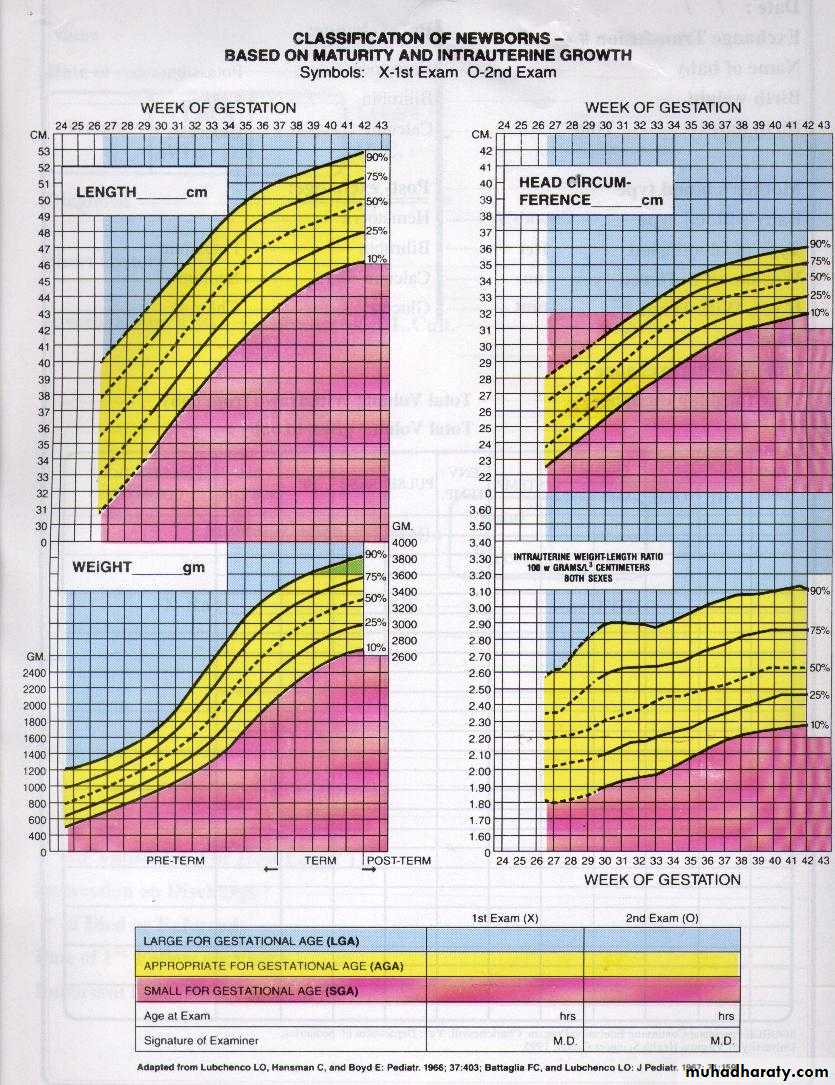
Classification By Weight Percentiles• AGA 10th-90th percentile for GA
• SGA < 10th percentile for GA
• LGA >90th percentile for GA
Weight for Gestational Age Chart
Acta Paediatr Scand Suppl 1985; 31: 180.
Estimation of
gestational ageGestational Age Assessment
Obstetricians- LMP
- Ultrasound
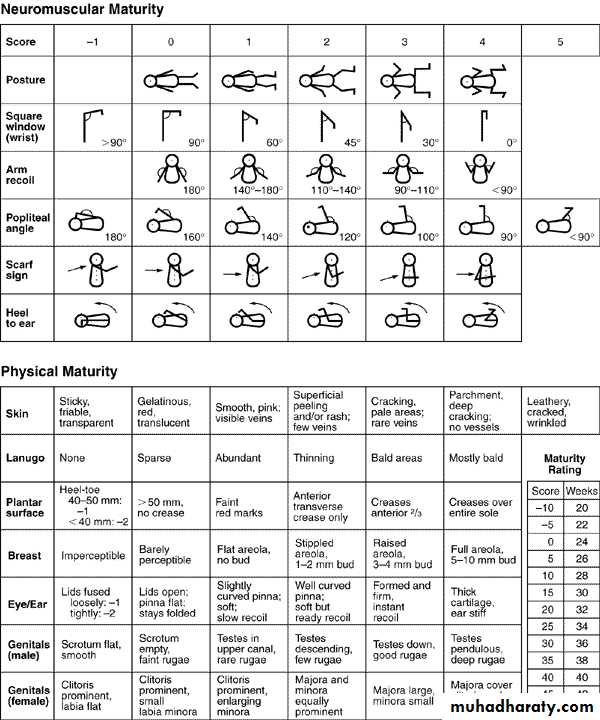
New Ballard score
Gestational Age Assessment
New Ballard Score- Performed within 12-24 hours
- Neuromuscular maturity (6)- Physical maturity (6)
Ballard JL, et al. J Pediatrics; 1991: 119 (3)
Ballard Score
External CharacteristicsEdema
Skin texture, color, and opacity
Lanugo
Plantar creases
Nipples and breasts
Ear form and firmness
Genitals
Neuromuscular Score
Posture
Square Window
Arm recoil
Popliteal angle
Scarf sign
Heel to ear
Ballard JL, et al. J Pediatrics; 1991: 119 (3)
New Ballard Score
Small for Gestational Age
SymmetricHC, length, weight all <10 percentile
33% of SGA infants
Cause: Infection, chromosomal abnormalities, inborn errors of metabolism, smoking, drugs
Asymmetric
Weight <10 percentile, HC and length normal
55% of SGA infants
Cause: Uteroplacental insufficiency, Chronic hypertension or disease, Preeclampsia, Hemoglobinopathies, altitude, Placental infarcts or chronic abruption
Combined
Symmetric or asymmetric
12% of SGA infants
Cause: Smoking, drugs, Placental infarcts or chronic abruption, velamentous insertion, circumvallate placenta, multiple gestation
0
Large for Gestational Age
EtiologiesInfants of diabetic mothers
Beckwith-Wiedemann Syndrome
characterized by macroglossia, visceromegaly, macrosomia, umbilical hernia or omphalocele, and neonatal hypoglycemia
Hydrops fetalis
Large mother
0
APGAR Score
• Score
• 0
• 1
• 2
• Heart Rate
• Absent
• <100bpm
• >100bpm
• Respiratory effort
• Absent, irregular
• Slow, crying
• Good
• Muscle tone
• Limp
• Some flexion of extremities
• Active motion
• Reflex irritability (nose suction)
• No response
• Grimace
• Cough or sneeze
• Color
• Blue, pale
• Acrocyanosis
• Completely pink
0
Apgar Score
Assess the physical condition of newborns after delivery at 1,5 m and every 5 m.until its value is > 7A value > 7 indicate the baby’s condition is good to excellent
A value less than 4 necessitate continued resuscitation
Apgar score is a good predictor of survival but using it to predict long-term outcome is inappropriate
Temperature
Heart rateRespiratory rate
Blood pressure
Capillary refill time
Vital signs
1.Temperature
Temperature should be taken axillaryThe normal temperature for infant is 36.5- 37-50C.
Axillary temp.is 0.5-1 0c lower than rectal
2- Heart rate
It should be obtained by auscultation and counted for a full minute
Normal heart rate is 120-160 beat /m.
If the infant is tachycardic (heart rate >170 BPM), make sure the infant is not crying or moving vigorously3. Respiratory rate
Normal respiratory rate is 40 –60/minuteRespiratory rate should be obtained by observation for one full minute
Newborns have periodic rather than regular breathing4. Blood pressure
It is not measured routinelyNormal blood pressure varies with gestational and postnatal ages
5. Capillary refill time
Normally < 3 seconds over the trunkMay be as long as 4 seconds on extremities
Delayed capillary refill time indicates poor perfusion
GENERAL EXAMINATION
SkinGeneral description:
At birth;
Color: bright red,
Texture: soft and has good elasticity.
Edema is seen around eye, face, and scrotum or labia.Cyanosis of hands & feet (acrocyanosis)
General description of the skin
Acrocyanosis
1.Vernix Caseosa
Soft yellowish cream layer that may thickly cover the skin of the newborn, or it may be found only in the body creases and between the labia.The debate of wash it off or to keep it.Vernix Caseosa
2. Lanugo hair
Distribution- The more premature baby is, the heavier the presence of lanugo is.- It disappears during the first weeks of lifeLanugo hair
3. Mongolian spots
Black coloration on the lower back, buttocks, anterior trunk, & around the wrist or ankle.They are not bruise marks or a sign of mental retardation, they usually disappear during preschool years without any treatment.Mongolian spots
4. Desquamation
Peeling of the skin over the areas of bony prominence that occurs within 2-4 weeks of life because of pressure and erosion of sheets.Desquamation
5. Physiological Jaundice
6. Milia
Small white or yellow pinpoint spots. Common on the nose, forehead, & chin of the newborn infants due to accumulations of secretions from the sweat & sebaceous glands that have not yet drain normally.They will disappear within 1-2 weeks, they should not expressed.Milia
7. Head
The Anterior fontanel: is diamond in shape, located at the junction of 2 parietal & frontal bones. It is 2-3 cm in width & 3-4 cm in length. It closes between 12-18 months of age.The posterior fontanel: is triangular in shape, located between the parietal &occipital bones. It closes by the 2nd month of age
Fontanels should be flat, soft, & firm. It bulge when the baby cries or if there is increased in ICP. Two conditions may appear in the head:Caput succedaneum & CephlhemtomaCaput succedaneum
An edematous swelling on the presenting portion of the scalp of an infant during birth, caused by the pressure of the presenting part against the dilating cervix. The effusion overlies the periosteum with poorly defined margins.Caput succedaneum
Caput succedaneum extends across the midline and over suture lines. Caput succedaneum does not usually cause complications and usually resolves over the first few days. Management consists of observation only.Caput succedaneum
Caput succedaneum
Cephalhematoma
Cephalhematoma is a subperiosteal collection of blood secondary to rupture of blood vessels between the skull and the periosteum, in which bleeding is limited by suture lines (never cross the suture lines).
Cephalhematoma
Cephalhematoma
Anterior and posterior fontanelle
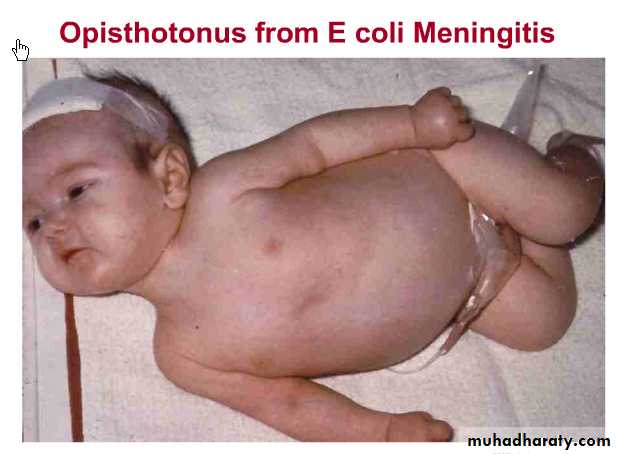
Large anterior fontanelle is seen inhypothyroidism,osteogenesisimperfecta,hydrocephalus
Small ant.fontanelle in microcephaly and craniostenosisBulging ant. fontanelle in menigitis and hydrocephalus Intracranial hemorrhage
Depressed ant.fontanelle in dehydrationLarge post.fontanelle :suspicious of hypothyroidism
8. Eyes
Usually edematous eye lids- Gray in color. True color is not determined until the age of 3-6 months.- Pupil: React to light- Absence of tears- Blinking reflex is present in response to touch- Can not follow an object (Rudimentary fixation on objects).Normal Eye
Eyelid Edema
Dysconjugate Eye Movements
Subconjunctival Hemorrhage
Congenital Glaucoma
Congenital Cataracts
9. Ears
• Position: In the normal newborn the top of the ear should be parallel to the outer and inner canthus• of the eye Startle Reflex:Pinna flexible, cartilage present.
Normal Ears
Ear Tag
10. Nose
Nasal Patency (stethoscope).Nasal discharge – thin white mucousNormal Nose
Dislocated Nasal Septum11. Mouth & Throat
- Intact, high arched palate.- Sucking reflex – strong and coordinated- Rooting reflex- Gag reflex- Minimal salivation12. Neck
Short, thick, usually surrounded by skin folds.Cysts: Thyroglossal cyst
Cystic hygromaMasses: Sternomastoid tumor
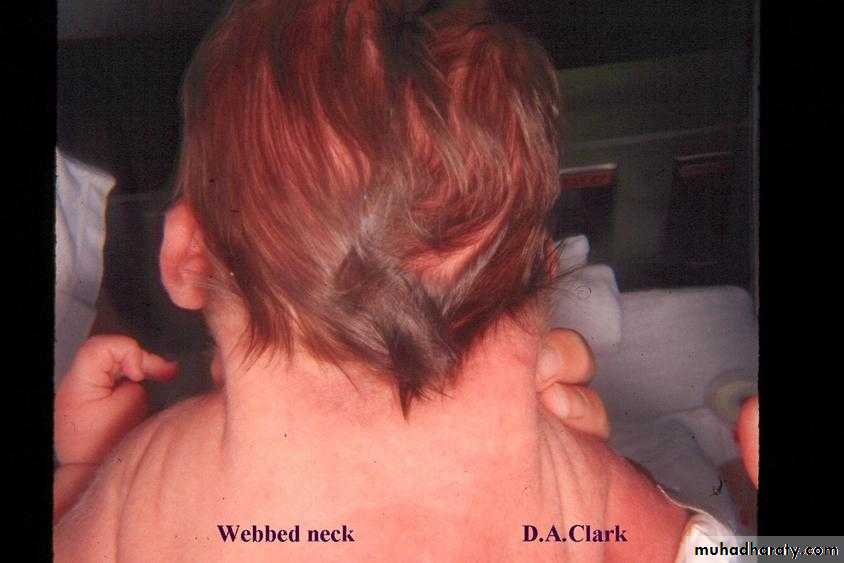
ThyroidWebbing
Webbed NeckSystem assessment of the neonates:
1. Gastrointestinal System:Mouth should be examined for abnormalities such as cleft lip and/or cleft palate.Epstein pearls are brittle, white, shine spots near the center of the hard palate. They mark the fusion of the 2 hollows of the palate. If any; it will disappear in time.Cleft Palate
Cleft Lip
Cheeks Have a chubby appearance due to development of fatty sucking pads that help to create negative pressure inside the mouth which facilitates sucking.
Normal Tongue Ankyloglossia
Ankyloglossia
Gum: May appear with a quite irregular edge.Sometimes the back of gums contain whitish deciduous teeth that are semi-formed, but not erupted
Irregular edges with Natal Teeth
Natal Tooth
13. Abdomen
Cylindrical in ShapeNormal Umbilical Cord
Bluish white at birth with 2 arteries & one vein.Meconium Stained Umbilical Cord
14. Circulatory system
Heart:Apex- lies between 4th & 5th intercostal space, lateral to left sternal border.
15. Respiratory system
Slight substernal retraction evident during inspiration15. Respiratory system Cont.
Respiratory is chiefly abdominalCough reflex is absent at birth, present by 1-2 days postnatal.Possible signs of RDS are:- Cyanosis other than hands & feet.- Flaring of nostrils.- Expiratory grunt-heard with or without stethoscope.Respiratory system Cont.
Xiphesternal process evidentMuskloskletal
FracturesDislocations
Polydactyly
Syndactyly
Deformities
Extremities
Nail beds pink
Extremities
Creases on anterior two thirds of sole.Common feet abnormalities
Club FeetPhysical exam
Physical examination1st examination in delivery room or as soon as possible after delivery
2nd and more detailed examination after 24 h of life
Discharge examination with 24 h of discharge from hospital
1- Measurements• There are three components for growth measurements in neonates
• Weight
• Length
• Head circumference
• All should be plotted on standardized growth curves for the infant’s gestational age
1- Weight
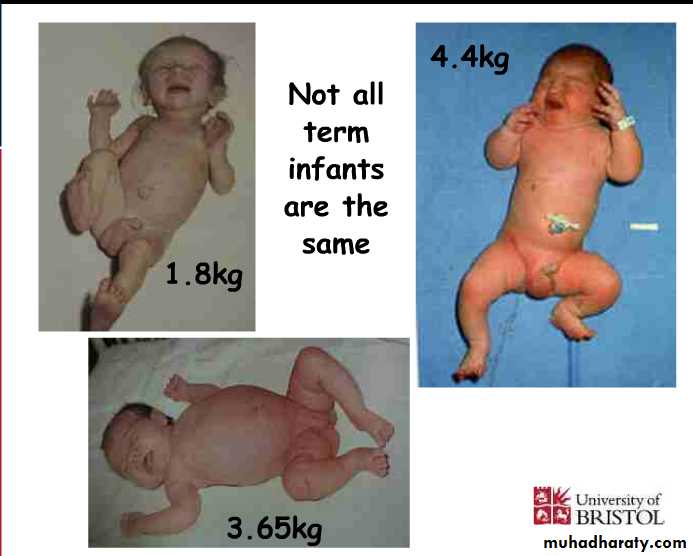
Weight of F.T infants at birth is 2.6– 3.8kg.Babies less than 2.5 kg are considered low birth weight.
Babies loose 5 – 10% of their birth weight in the first few days after birth and regain their birth weight by 7 – 10 days.
Weight gain varies between 15-20 gm/day.
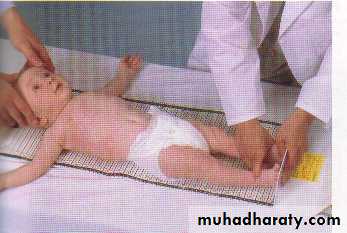
2. Length
Crown to heel length should be obtained on admission and weekly
Acceptable newborn length ranges from 48-52 cm at birth
2. Length
3. Head Circumference
Head circumference should be measured on admission and weeklyUsing the measuring paper tape around the most prominent part of the occipital bone and the frontal bone
Acceptable head circumference at birth in term newborn is 33-38 cm
3. Head CircumferenceNeurological exam
Muscle tone
Connvulsions
Neonatal reflexes
Moro
Grasp
Tonic Neck
Stepping and Placing
Rooting &Suckling
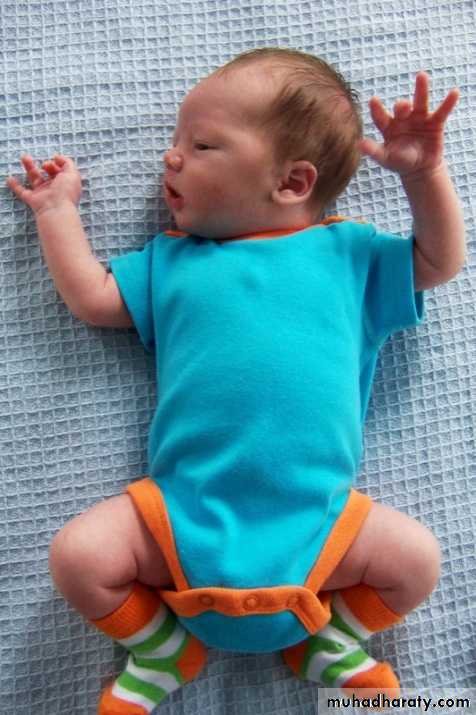
Posture
Term infants normal posture is hips abducted and partially flexed, with knees flexed.Arms are abducted and flexed at the elbow.
Fists are often clenched, with the fingers covering the thumb
Tone
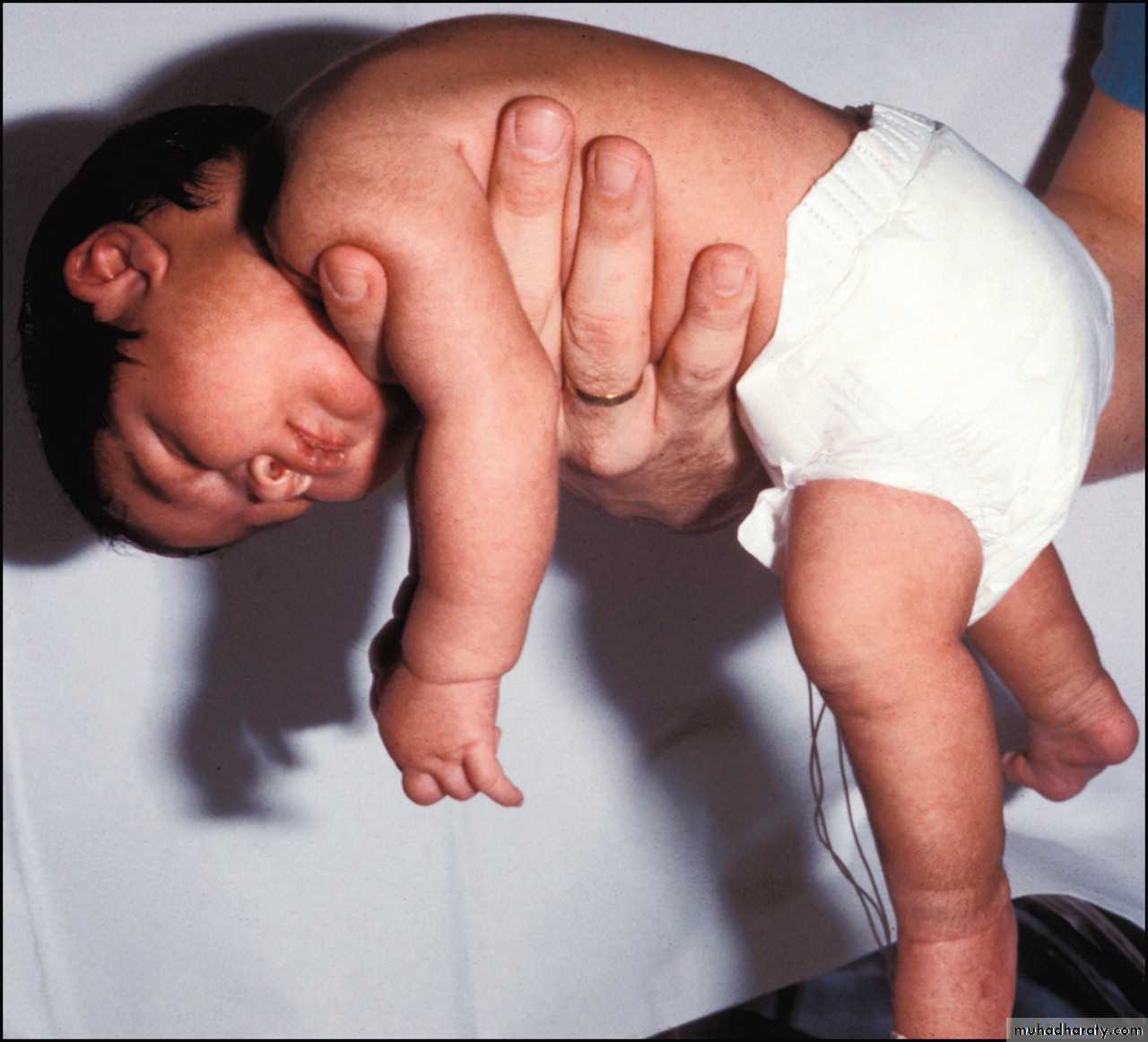
To test, support the infant with one hand under the chest. Neck extensors should be able to hold head in line for 3 secondsThere should be no more than 10% head lag when moving from supine to sitting positions.
Hypotonia
Neonatal reflexes
Also known as developmental, primary,or primitive reflexes.They consist of autonomic behaviors that do not require higher level brain functioning
They can provide information about integrity ofC.N.S. Their absence indicate C.N.S depression
They are often protective and disappear as higher level motor functions emerge.
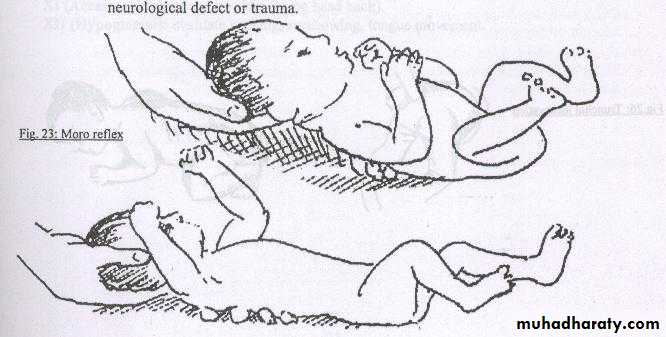
Moro Reflex
Onset: 28-32 weeks GADisappearance:4- 6 months
It is the most important reflex in neonatal period
Moro reflex
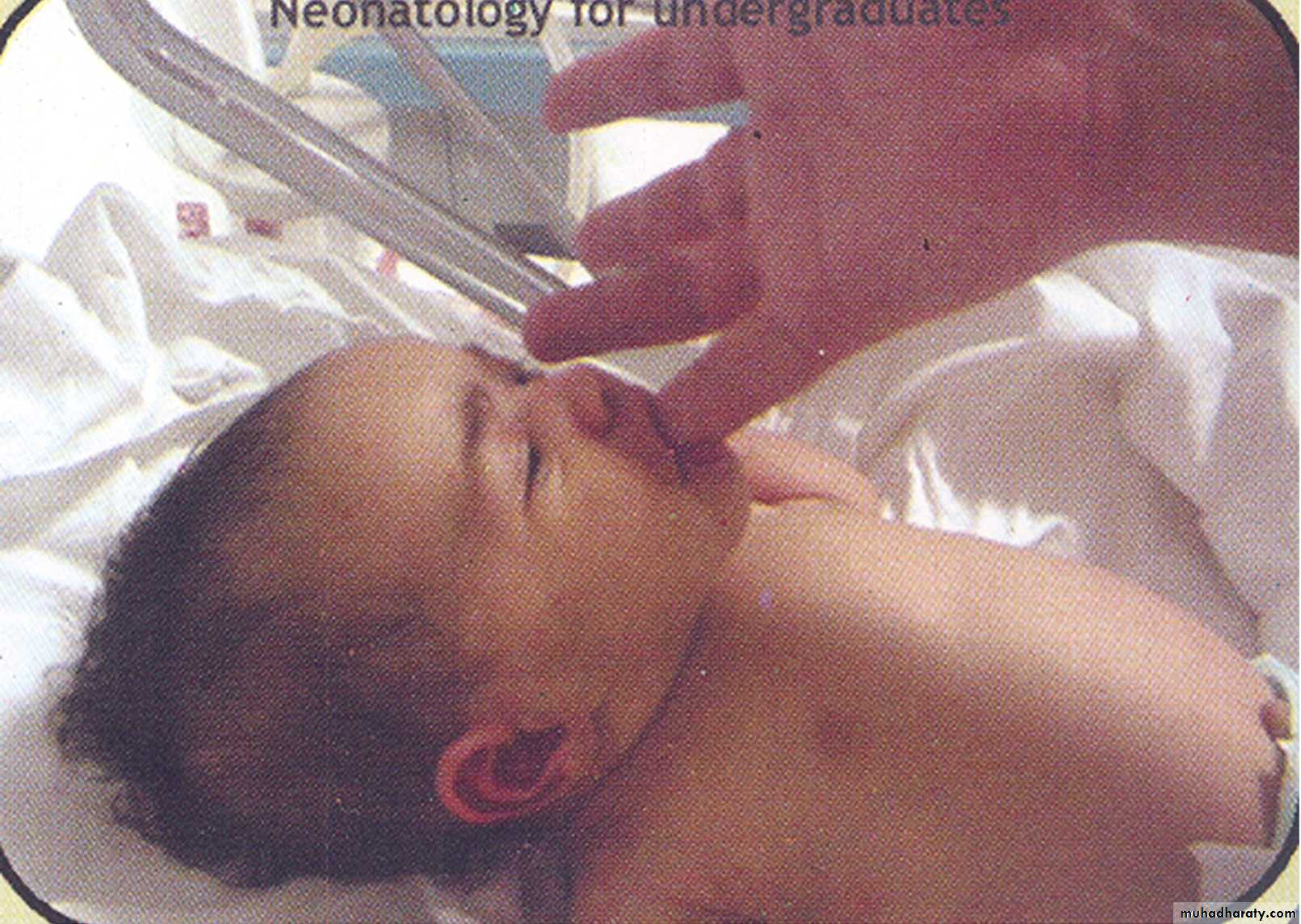
Stimulus : when baby in supine position elevate his head by your hand then allow head to drop suddenly:Response
Extension of the back
Extension and abduction of the UL
Flexion and adduction of the UL with open fingers
Crying
Significance of Moro
Bilateral absence:CNS depression by narcotics or anesthesia
Brain anoxia and kernicterus
Very Premature baby
Asymmetric response:
Erbs palsy , fracture clavicle or humerus
Persistence beyond 6th month:
CNS damage
Suckling Reflex
When a finger or nipple is placed in the mouth, the normal infant will start to suck vigorouslyAppears at 32 w & disappears by 3 – 4 m
Suckling Reflex
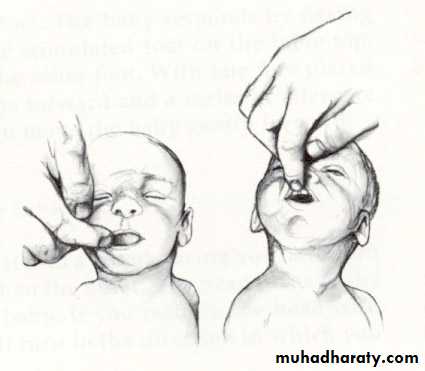
Rooting ReflexWell-established: 32-34 weeks GA
Disappears: 3-4 months
Elicited by the examiner stroking the upper lip or corner of the infant’s mouth
The infant’s head turns toward the stimulus and opens its mouth
Rooting ReflexRooting reflex
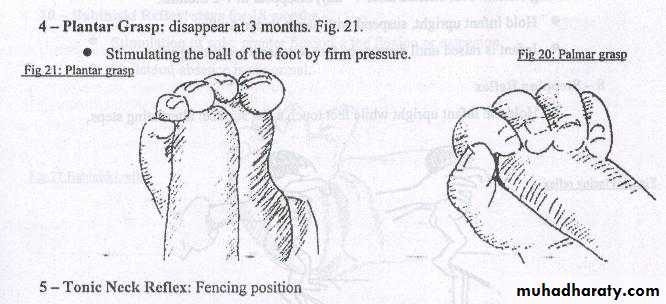
Palmar grasp
Well-established: 36 weeks GADisappears: 4 months
Elicited by the examiner placing her finger on the palmar surface of the infant’s hand and the infant’s hand grasps the fingerAttempts to remove the finger result in the infant tightening the grasp
Grasp reflex
Technique: put the examiner finger in the baby palm with slight rubbing .
Response: the infant grasp the finger firmly
Significance:
Absent CNS depression
Persist CNS damage
•
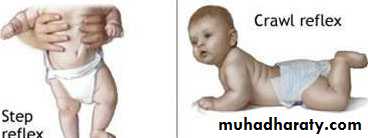
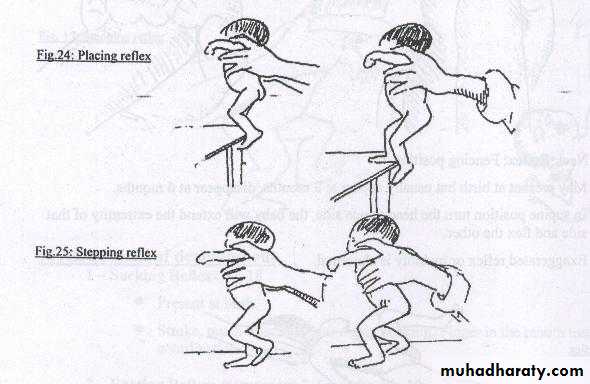
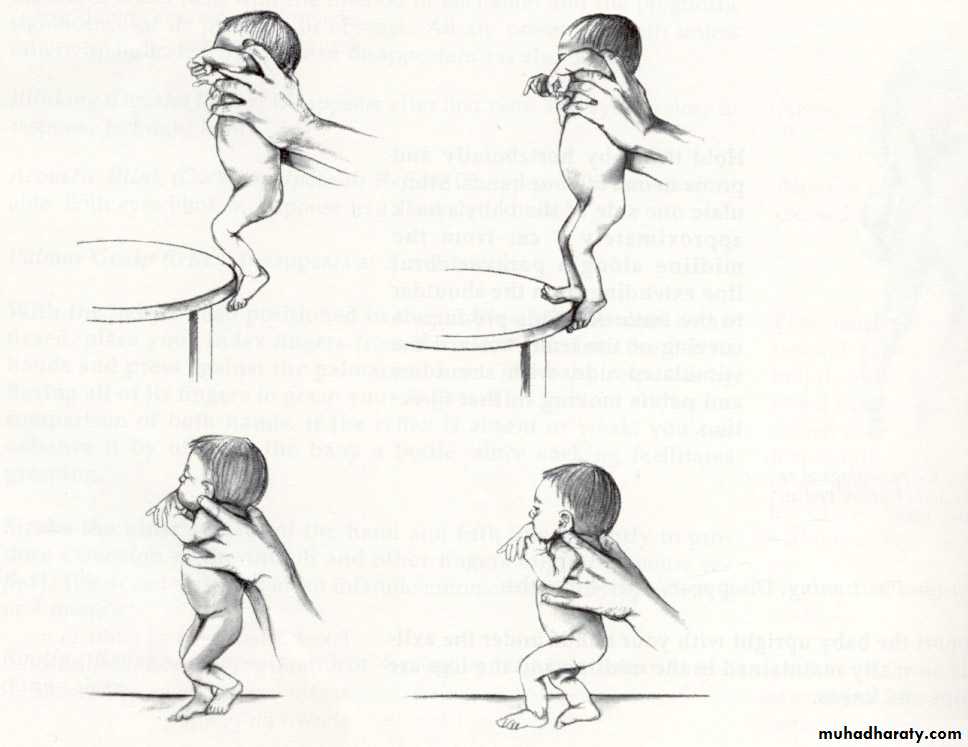
Stepping Reflex
Onset: 35-36 weeks GADisappearance: 6 weeks
Elicited by touching the top of the infant’s foot to the edge of a table while the infant is held upright.The infant makes movements that resemble stepping
Stepping :
Hold baby in upright position then lower him till his sole touch table → stepping movement start.
Placing :
When dorsum of the baby foot touches the under surface of the table → flexion then extension to place or put his foot on the tablePlacing Reflex
Placing reflex
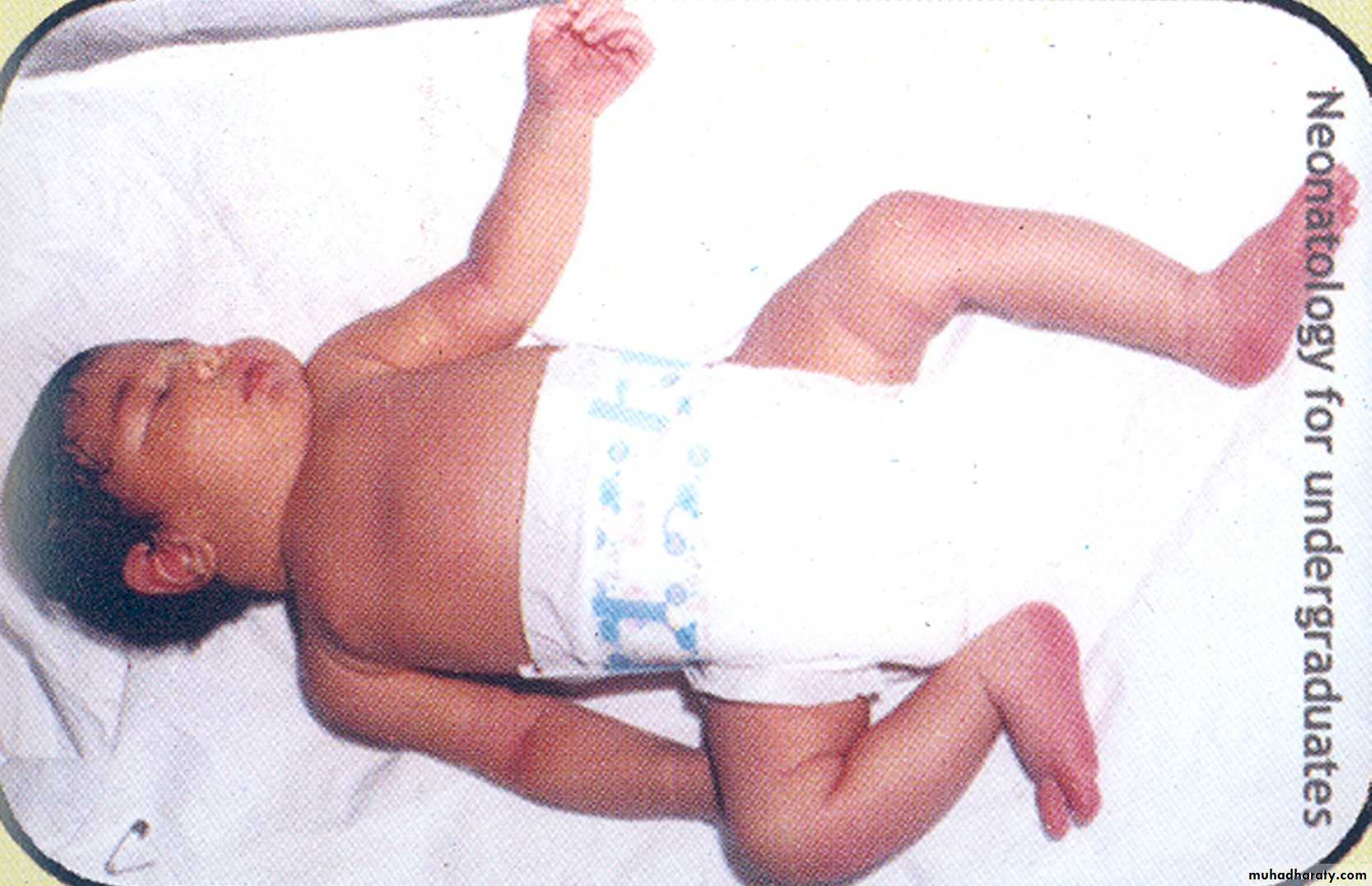
Tonic neck (Fencing posture)
Evident at 4 weeks PGADisappearance: 7 months
Elicited by rotating the infant’s head from midline to one sideThe infant should respond by extending the arm on the side to which the head is turned and flexing the opposite arm