Dr.Asaad
new 2016
Worldwide a major source of disease in domestic animals and humans.
Major zoonotic disease worldwide particularly Mediterranean, Africa, Middle
East, Latin America.
Other names for human disease:
undulant fever, Malta fever, Mediterranean fever.
Brucellae are slow-growing, small, aerobic, nonmotile, nonencapsulated, non–
spore-forming, gram-negative coccobacilli.
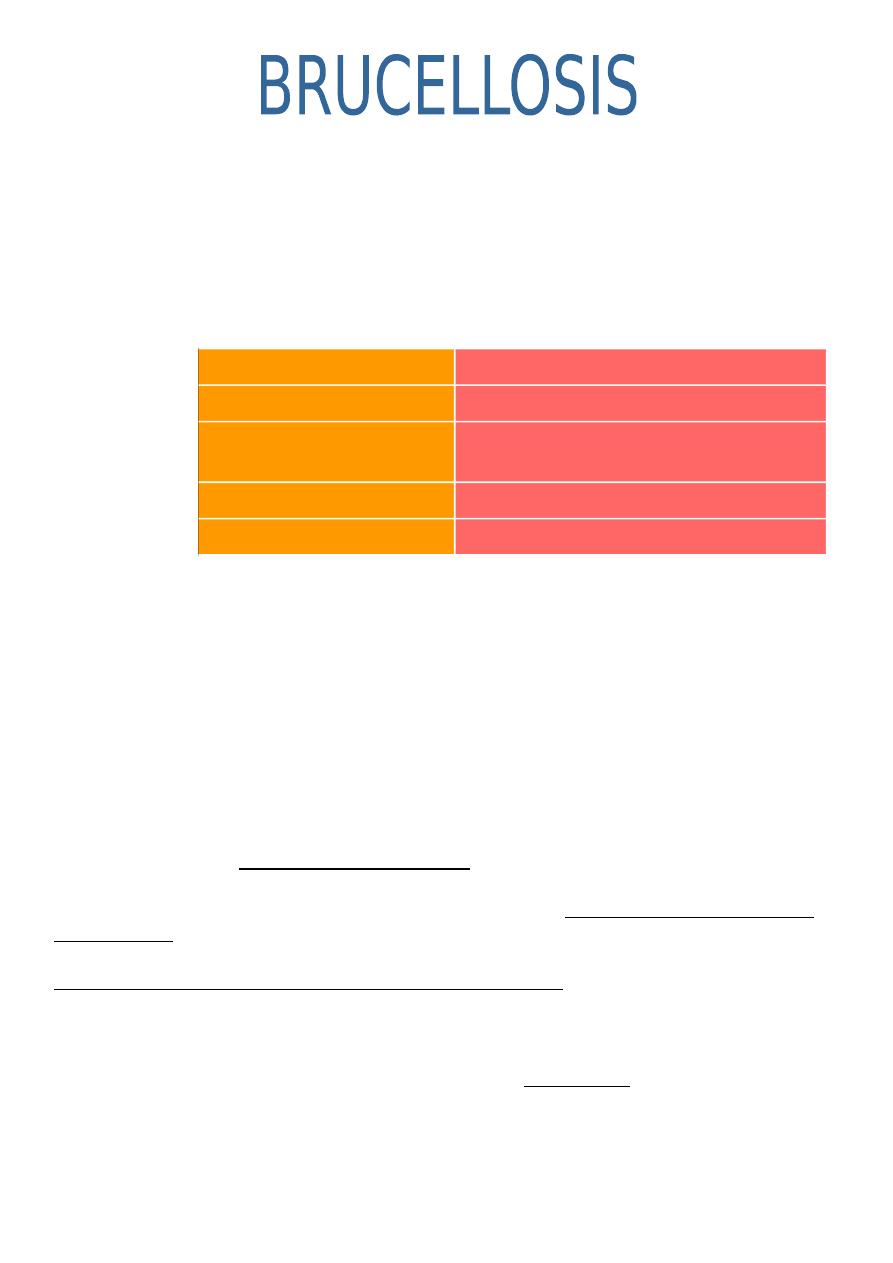
Etiology
Microorganism
Reservoir Host
Brucella abortus
Cattle
B. Melitensis
Sheep, goats, cattle
causes the most severe disease
B. Suis
Swine
B. Canis
Canine
Epidemiology
Routes of transmission to human include:
- Director contact with animals or their secretions, through cuts and skin
abrasions.
- Infected aerosols inhaled or inoculated into eye or conjunctival sac.
- Ingestion of unpasteurized dairy products.
Thus, Brucellosis constitutes occupational risk for: farmers, veterinarians, abattoirs
and Laboratory personnel.
Pathogenesis
After penetrating the epithelial cells of human skin, conjunctiva, pharynx, or lung,
Brucella organisms initially induce an excess polymorphonuclear neutrophil
response in the submucosa. After ingestion of organisms by neutrophils and tissue
macrophages, spread to regional lymph nodes occurs. If host defenses within the
lymph nodes are overwhelmed, bacteremia follows. The usual incubation period
between infection and bacteremia is 1½ to 3 weeks. Bacteremia is accompanied by
phagocytosis of free Brucella organisms by neutrophils and localization of bacteria
primarily to the spleen, liver, and bone marrow, with the formation of granulomas.
Clinical Manifestations
Clinically, human brucellosis may be conveniently, divided into subclinical illness,
acute or subacute disease, localized disease and complications, relapsing infection,
and chronic disease.
Subclinical Illness
1 Formatted by Mohammed Musa

Detected only by serologic testing, asymptomatic or clinically unrecognized human
brucellosis often occurs in high-risk groups, including slaughterhouse workers,
farmers, and veterinarians. More than 50% of abattoir workers and up to 33% of
veterinarians have high antiBrucella antibody titers but no history of recognized
clinical infection. Children in endemic areas frequently have subclinical illness.
Acute or subacute
Incubation period: 30-60 days ( or longer)
Fever 39.4° C (103° F), occurs in 95% of patients. An undulating or intermittent
fever pattern is unusual.
malaise, chills, sweats, fatigue, and weakness.
myalgias, anorexia, and weight loss.
arthralgias, cough, testicular pain, dysuria, ocular pain, or visual blurring.
Splenomegaly is present in 10 to 15%, and lymphadenopathy occurs in up to 14%
hepatomegaly is less frequent.
Localized Disease and Complications
1. Musculoskeletal (Suppurative arthritis; synovitis, bursitis, Osteomyelitis, Spinal
spondylitis or sacro-iliitis, aravertebral or psoas abscess).
2. Neurological (Meningitis, Intracranial or subarachnoid haemorrhage,Stroke,
Myelopathy, Radiculopathy, Cranial nerve palsies).
3. Eye (Uveitis, Retinal thrombophlebitis).
4. Cardiac (Myocarditis, Endocarditis).
5. Respiratory (Pneumonitis or abscesses, Hilar adenopathy).
6.Abdominal (Splenic abscesses or calcification, Hepatitis).
7.Genitourinary: Epididymo-orchitis.
8. Hematological: Pancytopenia.
9-Cutaneous manifestations( in 5-10%) of patients, are transient and nonspecific,
resolve with therapy, include the following
- Erythema nodosum, abscesses, and papulonodular eruptions , Impetigo,
psoriatic, eczematous, and pityriasis rosea –like lesions
- Macular, maculopapular, Vasculitic lesions (eg, petechiae, purpura, and
thrombophlebitis)
Relapsing Infection
Up to 10% of patients with brucellosis experience relapses after antimicrobial
therapy. Relapses occur usually 3 to 6 months after completion of therapy but may
be seen up to 2 years after treatment. Relapses are associated frequently with
antimicrobial resistance as well as the intracellular location of the organisms, which
protects the bacteria from certain antibiotics and host defense mechanisms.
Relapsing infection is difficult to distinguish from reinfection in high-risk groups with
continued exposure.
2 Formatted by Mohammed Musa
Chronic Disease
Disease with a duration of more than 1 year has been called chronic brucellosis. A
majority of patients classified as having chronic brucellosis really have persistent
disease caused by inadequate treatment of the initial episode, or they have focal
disease in bone, liver, or spleen. About 20% of patients diagnosed as having chronic
brucellosis complain of persistent fatigue, malaise, and depression; in many aspects
this condition resembles the chronic fatigue syndrome. These symptoms frequently
are not associated with clinical, microbiologic, or serologic evidence of active
infection and may represent a preexisting psychoneurosis.
Diagnosis
Culture The most conclusive means of establishing the diagnosis In Acute
brucellosis is by positive cultures from normally sterile body fluids or tissues. The
culture of brucella organisms is potentially hazardous to laboratory personnel.
In acute brucellosis, positive blood cultures are obtained in 50-75% of cases, Blood
culture positivity decreases with increasing duration of illness. With localized
brucellosis (e.g., lymph nodes, spleen, liver, or skeletal system), cultures of purulent
material or tissues usually yield brucella organisms. Culture of cerebrospinal fluid is
positive in 45% of patients with meningitis.
Identification of specific antibodies against bacterial lipopolysaccharide and other
antigens can be detected by the standard agglutination test (SAT),, 2-
mercaptoethanol (2-ME), rose Benga lELISA typically uses cytoplasmic proteins as
antigens. It measures IgM, IgG and IgA with better sensitivity and specificity than the
SAT in most recent comparative studies.
SAT in most recent comparative studies.
Standard Tube Agglutination
Most patients mount significant serologic responses to Brucella infections. The most
frequently used test is the standard tube agglutination (STA) test, measuring
antibody to B.abortus antigen.
3 Formatted by Mohammed Musa
No single titer of brucella antibodies always “diagnostic”, but, most cases of active
infection, have titer higher than 1:160.
Rose Bengal test(ELIZA), rapid screening method, but positive sera should always
be confirmed by SAT.
False-negative reactions in SAT, result from
prozone phenomenon, and false-positive results from cross-reaction with
antibodies to yersinia,
cholera, and tularemia.
- False-negative and false-positive reactions, avoidable by routinely diluting
serum beyond 1:320.
Other Tests
The peripheral blood–based polymerase chain reaction (PCR) has enormous
potential to detect bacteremia, to predict relapse, and to exclude "chronic
brucellosis." PCR is probably more sensitive and is certainly quicker than blood
culture, and it does not carry the attendant biohazard risk posed by culture.
The 2-mercaptoethanol test detects immunoglobulin G (IgG), and titers higher than
1:80 define active infection. A high IgG antibody titer or a titer that is higher after
treatment suggests persistent infection or relapse
Although Brucella infection is primarily controlled through cell-mediated immunity
rather than antibody activity, some immunity to reinfection is provided by serum
immunoglobulin (Ig). Initially, IgM levels rise, followed by IgG titers. IgM may remain
in the serum in low levels for several months, whereas IgG eventually declines.
Persistently elevated IgG titers or second rises in IgG usually indicate chronic or
relapsed infection
Treatment
Antimicrobial therapy of brucellosis relieves symptoms, shortens illness duration,
and reduces complication incidence.
Intracellular localization of brucellae, believed to offer some protection against
antimicrobials, thus drugs with good intra-cellular penetration are necessary for
cure.
The "gold standard" for the treatment of brucellosis in adults is IM streptomycin
(0.75–1 g daily for 14–21 days) together with doxycycline (100 mg twice daily for 6
weeks). In both clinical trials and observational studies, relapse follows such
treatment in 5–10% of patients.
The usual alternative regimen (and the current World Health Organization
recommendation) is rifampin (600–900 mg/d) plus doxycycline (100 mg twice daily)
for 6 weeks. Patients who cannot tolerate or receive tetracyclines (children,
pregnant women) can be given high-dose TMP-SMX instead (2 or 3 standard-
strength tablets twice daily for adults, depending on weight).
Evidence is beginning to accumulate that other aminoglycosides can be substituted
for streptomycin—e.g. gentamicin given at a dosage of 5–6 mg/kg per day for at
least 2 weeks. Early experience with fluoroquinolone monotherapy was
disappointing, but high-dose ofloxacin (400 mg twice daily) or ciprofloxacin (500 mg
4 Formatted by Mohammed Musa
twice daily), given together with rifampin for 6 weeks, may become accepted as an
alternative to the other 6-week regimens for adults.
A triple-drug regimen (doxycycline and rifampin combined with an initial course of an
aminoglycoside) was superior to double-drug regimens in a meta-analysis. The
triple-drug regimen should be considered for all patients with complicated disease
and for those for whom treatment adherence is likely to be a problem.
Significant neurologic disease due to Brucella requires prolonged treatment (i.e., for
3–6 months), usually with ceftriaxone supplementation of a standard regimen.
Brucella endocarditis is treated with at least three drugs (an aminoglycoside, a
tetracycline, and rifampin), and many experts add ceftriaxone and/or a
fluoroquinolone to reduce the need for valve replacement. Treatment is usually
given for at least 6 months. Surgery is still required for the majority of cases of
infection of prosthetic heart valves and prosthetic joints.
Prevention
The control of human brucellosis is related directly to prevention programs in
domestic animals and avoiding unpasteurized milk and milk products. In
slaughterhouses, important means of prevention include careful wound dressing,
protective glasses and clothing, prohibition of raw meat ingestion.
Occasional person-to-person transmission has been reported, including
transmission to infants via breastfeeding. There is a little evidence for sexual
transmission of brucellosis.
Laboratory transmission of brucellosis may occur, especially in regions of endemic
disease. It is estimated that 12% of laboratory workers in Spain acquire brucellosis.
Prognosis
Brucellosis appropriately treated within the first month of symptom onset is curable.
Acute brucellosis often produces severe weakness and fatigue, and patients are
frequently unable to work for up to 2 months. Immunity to reinfection follows initial
Brucella infection in the majority of individuals. With early antimicrobial therapy,
cases of chronic brucellosis or localized disease and complications are rare. Of
patients who die of brucellosis, 84% have endocarditis involving a previously
abnormal aortic valve, often associated with severe congestive heart failure.
blocking antibody: an antibody that reacts with an antigen but fails to cross-link
with other antigens and cause agglutination. When such antibodies are present in
high concentration, they interfere with the action of other antibodies by occupying all
the antigenic sites
Quiz:
A-Intravascular Device Infections CLINICAL FEATURE AND MICROORGANIZM
B=IMEPENIME OR MROPENIME
5 Formatted by Mohammed Musa
