medicine
dr.assad
Shigellosis
Shigellae are Gram-negative nonmotile bacilli, closely related to E. coli, that
invade the colonic mucosa. There are four main groups: Sh. dysenteriae, flexneri,
boydii and sonnei. In the tropics bacillary dysentery is usually caused by Sh.
flexneri, whilst in the UK most cases are caused by Sh. sonnei. The organism only
infects humans. Shigellae survive the low pH of the gastric acid barrier, and as few
as 10– 100 organisms can cause infection.
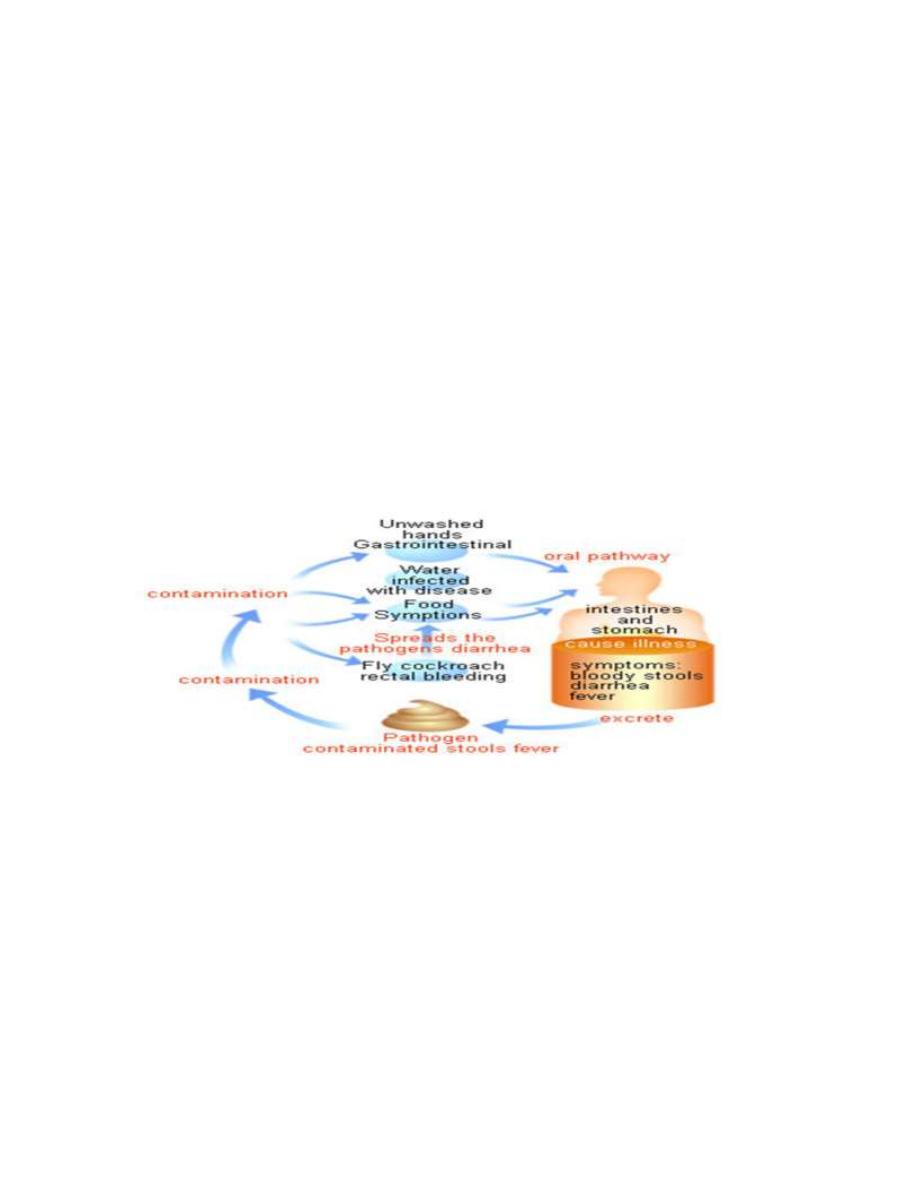
Transmition:
These bacteria are transmitted from person to person via the
fecal-oral route and occasionally via intermediate vectors such as food, water,
flies, and fomites. Shigellosis is associated with a high rate of secondary
household transmission.
Shiga toxin:
is a important factors in disease severity. The toxins target
endothelial cells and play a significant role in the microangiopathic complications
of Shigella such as hemolytic-uremic syndrome (HUS) and thrombotic
thrombocytopenic purpura (TTP). Shigella causes extensive ulceration of the
epithelial surface of the colonic mucosa.
Clinical features
: Pts can remain asymptomatic, develop fever and
diarrhea,or experience a progression to bloody diarrhea and dysentery. Dysentery
is characterized by the passage of 10– 30 stools per day in small volumes

medicine
dr.assad
containing blood, mucus, and pus, with associated severe abdominal cramping
and tenesmus. Fever, dehydration and weakness occur, with tenderness over the
colon. Arthritis or iritis may occasionally complicate bacillary dysentery (Reiter's
syndrome).
Self limiting course ranging 3 days to 1 week . rarely last for 1 month
It cause damage by 2 mech.
1-invasion of colonic epithelium
2- production of enterotoxin which enhance virulence
1 million death and causing 165 million case of diarrhea annually world wide
Complications:
1. Severe cases may progress to toxic dilatation, colonic perforation, and death.
2. HUS is more frequent with E. coli but also occurs with S.dysenteriae type 1. The
syndrome is characterized by oliguria, a marked drop in hematocrit, renal
failure,DIC, and a mortality rate of 5–10%.
3- HYPONATREMIA and inapropriat ADH secretion
4- LEUKOMOID REACTION more in children in 4% .WBC more than 50,000.
5- neurological.seizure in 10% encephalitis( by sonni) more in children in 40% of
children hospitalized for shegillosis
7- Reactive arthritis.(flexinari) occur alone or in combination with congectivitis
and urethritis 1-2 week after dysentery regardless whether the dysentery treated
or not with AB.(Reiter syndrome)70% OF PATIENT is HLAB27.
Reiter syndrom either sexually transmit by chlamydia or uroplasma or GIT by
sheg.salm,yersinia. compylo.Keratoderma blennorragica(pathy scaly skin on palm
and soles or scalp).Sacroilitis , enthesosits.
8-VALVOVAGINITIS

medicine
dr.assad
9-RARLY keratitis ,congectivitis ,myocarditis.
The differential diagnosis:
1-invasive pathogenic bacteria (Salmonella enteritidis, Campylobacter jejuni,
Clostridium difficile, Yersinia enterocolitica)
2-or parasites (Entamoeba histolytica) should be considered. Only bacteriologic
and parasitologic examinations of stool can truly differentiate among these
pathogens.
3-A first flare of inflammatory bowel disease, such as Crohn's disease or ulcerative
colitis, should be considered in patients in industrialized countries.
Laboratory Diagnosis:
Microscopic examination of stool smears shows high PMN counts in each
microscopic field. However, because shigellosis often manifests only as watery
diarrhea, systematic attempts to isolate Shigella are necessary.
The "gold standard" for the diagnosis of Shigella infection remains the isolation
and identification of the pathogen from fecal material. The probability of isolation
is higher if the portion of stools that contains bloody and/or mucopurulent
material is directly sampled.
Blood cultures are positive in <5% of cases and should be done only when a
patient presents with a clinical picture of severe sepsis.
TREATMENT:
1-Rehydration and supportive measures. Oral rehydration therapy or, if diarrhoea
is severe, intravenous replacement of water and electrolyte loss is necessary.
2. Antibiotics:Ciprofloxacin is recommended as first-line treatment. (500 mg 12-
hourly for 3 days) is effective, TMP-SMX (160/800 mg bid for 3– 5 days) can still
be used,as can ampicillin but resistance is the problem. Cephtriaxon is highly
effective. Azithromycin (1 g in a single dose) is effective in adults.

medicine
dr.assad
For public reason AB recommended for any stool +ve culture. It decrease fever
and duration of diarrhea by 2 days. Which reduce the risk of person to person
spread.
Nonspecific, Symptom-Based Therapy
Antimotility agents are suspected of increasing the risk of toxic megacolon and
are thought to have been responsible for HUS in children infected by Shigella For
safety reasons, it is better to avoid antimotility agents in bloody diarrhea.
Prevention:
Hand washing after defecation or handling of children's feces and before handling
of food is recommended. However, this protocol entails an average of 32 hand
washes per day, with consumption of 20 L of water. If soap is too costly, ash or
mud can be used, but access to water remains essential. Stool precautions,
together with a cleaning protocol for medical staff as well as for patients, have
proven useful in limiting the spread of infection during Shigella outbreaks.
Food handler should not involve in food preparation until stool culture is –ve
Post infection carriage less than 4 week
Ideally, patients should have a negative stool culture before their infection is
considered cured. Recurrences are rare if treatment and prevention are correctly
implemented.
Although several live attenuated oral and subunit parenteral vaccine candidates
have been produced and are undergoing clinical trials, no vaccine against
shigellosis is currently available.
BY:TWANA NAWZAD
