PEDIATRIC DR.NAWAL
1
|
P a g e
DONE BY :- #MOHDZ
Respiratory Distress Syndrome (RDS)
Hyaline Membrane Disease
INCIDENCE
Premature infants, incidence is inversely related to
GA& BWT, 60–80% of infants less than 28 wk. of
Gestational age, 15–30% of those 32 -36 wk.
The risk of developing RDS increases:-
1.
Maternal diabetes.
2.
Multiple births.
3.
Cesarean section, precipitous delivery.
4.
Asphyxia, cold stress.
5.
History of previously affected infants.
6.
Preterm male or white infants.
The risk of RDS is reduced in
1. Hypertension.
2. Maternal heroin use.
3. Prolonged rupture of membranes.
4. Antenatal corticosteroid prophylaxis.
PEDIATRIC DR.NAWAL
2
|
P a g e
DONE BY :- #MOHDZ
ETIOLOGY AND PATHOPHYSIOLOGY
Surfactant deficiency ( production and secretion)
Surfactant are (lecithin, phosphatidylglycerol, apoproteins, and
cholesterol.)
With advancing gestational age, increasing amounts of
phospholipids are synthesized and stored in type II alveolar cells.
Released into the alveoli→ reduce surface tension →preventing the
collapse of small air spaces at end-expiration→ maintain alveolar
stability.
Synthesis of surfactant depends in part on normal pH, temperature,
and perfusion.
Alveolar atelectasis, hyaline membrane formation, and
interstitial edema make the lungs less compliant, + compliant
chest wall → atelectasis → hypoxia.
Insufficient alveolar ventilation → hypercapnia, acidosis.
The combination of ;-
Hypercapnia + hypoxia + acidosis → pulmonary arterial
vasoconstriction →increased right-to-left shunting through the
foramen ovale and ductus arteriosus, pulmonary blood flow is
reduced, and ischemic injury to the cells producing surfactant.
PEDIATRIC DR.NAWAL
3
|
P a g e
DONE BY :- #MOHDZ
CLINICAL MANIFESTATIONS
appear within minutes of birth as:
intrapartum asphyxia
initial severe respiratory distress
Characteristically, tachypnea≥ 60/min, grunting, intercostal
subcostal retractions, nasal flaring, Cyanosis.
Breath sounds: normal or diminished, fine rales, especially
Over the lung bases.
The natural course of untreated RDS is characterized by:
o Progressive worsening of cyanosis and dyspnea, hypotension,
fatigue, cyanosis, and pallor, grunting decrease or disappears.
Apnea and irregular respirations are ominous signs requiring
immediate intervention.
o mixed respiratory-metabolic acidosis,
o Edema, ileus, and oliguria.
Respiratory failure.
reach a peak within 3 days, after which improvement is
gradual, often heralded by spontaneous diuresis and the ability
to
Oxygenate the infant at lower inspired oxygen levels or lower
ventilator pressures.
Death 2nd- 7th day,
-alveolar air leaks (interstitial emphysema, pneumothorax),
-pulmonary hemorrhage, or IVH.
PEDIATRIC DR.NAWAL
4
|
P a g e
DONE BY :- #MOHDZ
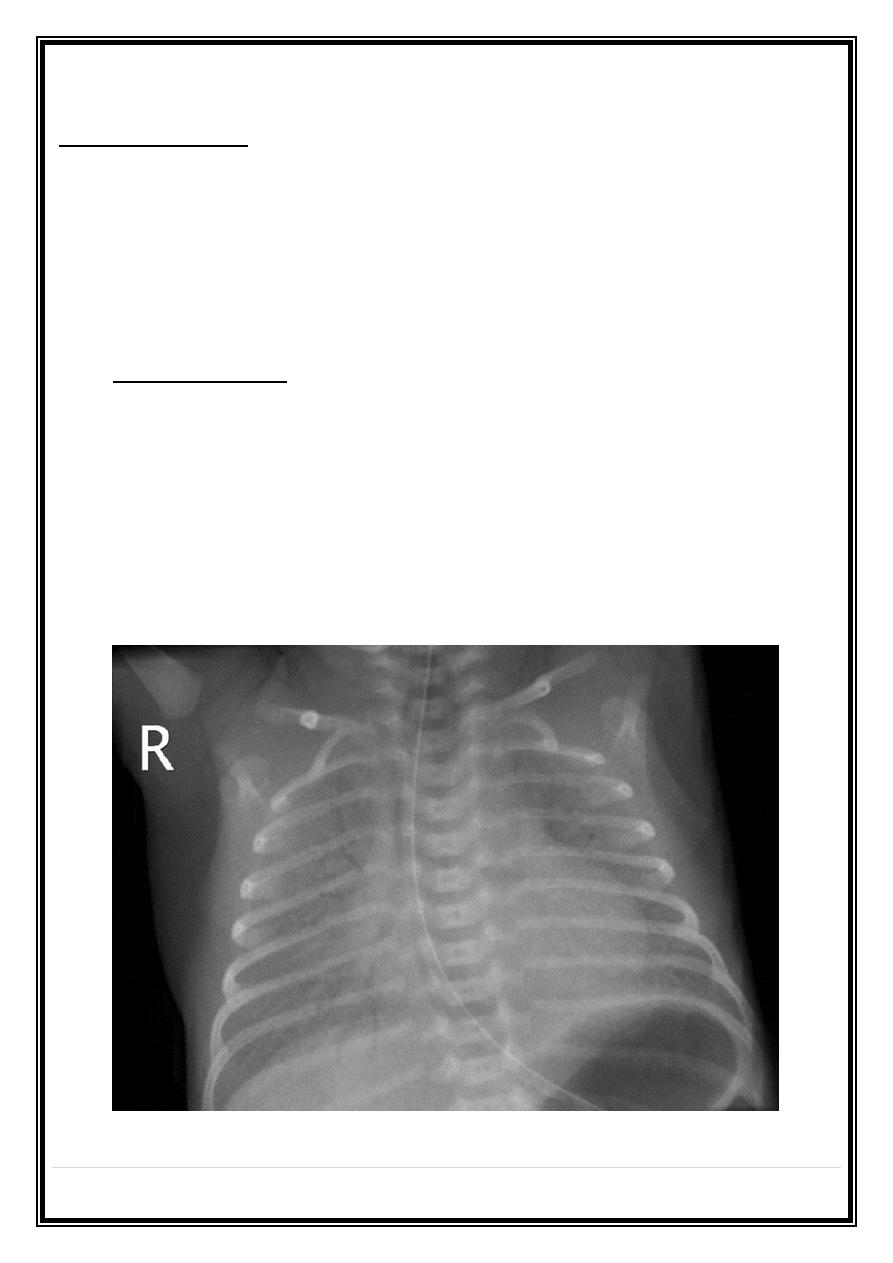
DIAGNOSIS.
1. -CXR:- the lungs may have a characteristic, but not
pathognomonic appearance that includes a fine reticular
granularity of the parenchyma and air bronchograms, which
are often more prominent early in the left lower lobe .The
initial CXR occasionally normal, with the typical pattern
developing at 6–12 hr.
2. -Laboratory findings are initially characterized by hypoxemia
and later by, Hypoxemia, hypercapnia, and metabolic acidosis.
Differential diagnosis
1-early-onset sepsis, in pneumonia. Maternal group B streptococcal
colonization, organisms on Gram stain of gastric or tracheal
aspirates and/or
Marked neutropenia may suggest the diagnosis.
2-Cyanotic heart disease (Echocardiography.
3-Persistent pulmonary hypertension.
4-aspiration (meconium, amniotic fluid) syndromes.
5-spontaneous pneumothorax.
6-pleural effusions.
7-diaphragmatic hernia.
8-lobar emphysema.
9-Transient tachypnea.
PEDIATRIC DR.NAWAL
5
|
P a g e
DONE BY :- #MOHDZ
PREVENTION:-
o -Avoidance of unnecessary or poorly timed CS.
o -appropriate management of high-risk pregnancy& labor.
o -Administration of betamethasone to women 48 hr before the
delivery of fetuses between 24 and 34 wk of gestation reduces
the incidence, mortality of RDS.
o Prenatal glucocorticoids may act synergistically with postnatal
exogenous surfactant therapy.
o Administration of a 1st dose of surfactant into the trachea of
symptomatic premature infants immediately after birth
(prophylactic) or during the 1st few hours of life (early rescue)
reduces air leak and mortality from RDS
TREATMENT:-
1- General supportive care
- placed in an isolette or radiant warmer (core temperature
maintained between 36.5 and 37°C).
- touch times. To avoid hypothermia and minimize oxygen
consumption.
- Calories and fluids: IV. For the 1st 24 hr, 10% GW d through a
peripheral vein at a rate of 65–75 mL/kg/24 hr.
- O2
Warm humidified oxygen should be provided at a concentration
initially sufficient to keep PaO2 between 50 and 70 mm Hg (85–95%
saturation).
PEDIATRIC DR.NAWAL
6
|
P a g e
DONE BY :- #MOHDZ
- CPAP at a pressure of 5–10 cm H2O by nasal prongs, If the Pao2
cannot be maintained above 50 mm Hg at inspired oxygen≥ 60% .
-Assisted ventilation:-If an infant managed by CPAP cannot maintain
an arterial oxygen tension above 50 mm Hg while breathing 70–100%
oxygen.
2- Surfactant
Rescue treatment is initiated in the 1st 24 hr of life. Repeated dosing,
via the endotracheal tube every 6–12 hr for a total of 2 to 4 doses,
Should be given by a physician who is qualified in neonatal
resuscitation and respiratory management and able to care for the
infant.
Complications of surfactant therapy include transient hypoxia,
bradycardia and hypotension, blockage of the endotracheal tube, and
pulmonary hemorrhage
3-Inhaled nitric oxide (iNO)
4-Metabolic acidosis. Sodium bicarbonate, 1–2 mEq/kg, may be
administered over a 15–20 min.
Alkali therapy may result in
-skin slough from infiltration,
-increased serum osmolality, hypernatremia, hypocalcemia,
hypokalemia, and liver injury exacerbate a severe respiratory
acidosis, especially if ventilation is ineffective
5-Periodic monitoring of Pao2, Paco2, and pH.
6- Antibiotic therapy:-is indicated because of the difficulty of
distinguishing group B streptococcal, until the results of blood
cultures are available. Penicillin or ampicillin with an aminoglycoside.
PEDIATRIC DR.NAWAL
7
|
P a g e
DONE BY :- #MOHDZ
COMPLICATIONS OF RDS
Tracheal intubation asphyxia from obstruction of the tube, cardiac
arrest during intubation or suctioning, subglottic stenosis .bleeding
during intubation, erosion of the palate, avulsion of a vocal cord,
laryngeal ulcer, papilloma of a vocal cord, persistent hoarseness,
stridor, or edema of the larynx.
Umbilical arterial catheterization
Vascular embolization, thrombosis, spasm, perforation.
Ischemic or chemical necrosis of abdominal viscera;
Infection; accidental hemorrhage.
Umbilical vein catheterization
Cardiac perforation and pericardial tamponade
Portal hypertension (portal vein thrombosis).
Reno vascular hypertension
.
Patent ductus arteriosus (PDA) , Bronchopulmonary
dysplasia (BPD)
is a result of lung injury in infants requiring
mechanical ventilation and supplemental oxygen.
On the 3rd–4th day, Respiratory distress persists or worsens and is
characterized by hypoxia, hypercapnia, oxygen dependence, in severe
cases, right-sided heart failure.
PEDIATRIC DR.NAWAL
8
|
P a g e
DONE BY :- #MOHDZ
Transient Tachypnea of the Newborn
-usually follows uneventful normal preterm or term
Vaginal or cesarean delivery.
-tachypnea, sometimes with retractions, or grunting occasionally,
cyanosis.
-The lungs clear
-recover rapidly within 3 days.
CXR prominent pulmonary vascular markings, fluid in the intrapolar
fissures, over aeration, flat diaphragms, rarely pleural effusions.
Hypercapnia and acidosis are uncommon.
The syndrome is believed to be secondary to slow absorption of fetal
lung fluid → decreased pulmonary compliance.
- Treatment is supportive.
Meconium Aspiration
o -Meconium-stained amniotic fluid occurs in term or post-term
infants.
o -Meconium aspiration pneumonia develops in 5%.
o -fetal distress and hypoxia.
o Passage of meconium into amniotic fluid.
o -infants are meconium stained and may be depressed and require
resuscitation at birth.
o The Meconium inactivates surfactant.
o -in utero or more often with the 1st breath, thick, particle is
aspirated into the lungs.
o -small airway obstruction may produce respiratory distress
PEDIATRIC DR.NAWAL
9
|
P a g e
DONE BY :- #MOHDZ
o -Partial obstruction of some airways may lead to pneumothorax,
pneumomediastinum, or both.
CLINICAL MANIFESTATIONS
Tachypnea, retractions, grunting, cyanosis (severe)
-only tachypnea without retractions.
-Over distention of the chest.
-usually improves within 72 hr,
-severe (assisted ventilation) high risk for mortality.
Tachypnea may persist for days or weeks.
-CXR characterized by patchy infiltrates, coarse streaking of both lung
fields, increased anteroposterior diameter, and flattening of the
diaphragm.
-Arterial Po2 may be low, if hypoxia has occurred, metabolic acidosis
is usually present.
PREVENTION
-rapid identification of fetal distress and initiating prompt delivery.
- Routine intrapartum nasopharyngeal suctioning does not reduce the
risk for MAS & rarely may cause nasopharyngeal trauma or cardiac
arrhythmia.
TREATMENT
-Routine intubation not recommended only in depressed infants &
suction to the endotracheal Tube (The risk associated with
laryngoscopy and endotracheal intubation is less than the risk of MAS
In these high-risk).
PEDIATRIC DR.NAWAL
10
|
P a g e
DONE BY :- #MOHDZ
Pneumonia TTT
1. -supportive care and standard management for Respiratory
distress. Mean airway pressure.
2. -exogenous surfactant to infants with MAS requiring
3. -Mechanical ventilation; - Severe meconium aspiration may be
complicated by persistent pulmonary hypertension.
PROGNOSIS.
o The mortality rate of meconium-stained infants is higher.
o Residual lung problems are rare:
Symptomatic cough, wheezing, and persistent hyperinflation.
o The extent of CNS injury & associated problems such as
pulmonary hypertension
