1
|
Fatima Ehsan
P a g e
ENURESIS
Enuresis is urinary incontinence at any age when urinary continence is
considered normal.
Most children are continent of urine during waking hours by age 3-4 yr.
TYPES:
Primary
when the child has never been continent of urine for a
prolonged period.
The reason for almost all primary enuresis is a delay in the maturation of
urethral sphincter control. This immaturity may be prolonged by a
psychological overlay related to concerns about the problem on the part
of parents and the child.
Secondary:
when incontinence recurs after a prolonged period of continence (6-12
mo).
Secondary enuresis usually is due to a psychologically stressful event or
condition but also is more likely than primary enuresis to have an organic
cause.
A urinary tract infection is the most common organic etiology.
Uncommon causes include chemical distal urethritis (e.g., from bubble
bath), congenital anomalies (e.g., spina bifida), severe lower urinary tract
obstruction (e.g., from posterior urethral valves, urethral cyst, or urethral
duplication), ectopic ureter, diabetes mellitus or insipidus, and pelvic
masses (e.g., presacral teratoma, fecal impaction hydrocolpos
Nocturnal enuresis
is the most common type. The prevalence of bedwetting is so common
before age 6 yr that it is not called enuresis.
About 20% of bed wetters after age 4 yr have secondary enuresis, which
warrants a more careful evaluation.
Condition more common in males
2
|
Fatima Ehsan
P a g e
Daytime enuresis
has a prevalence rate of only about 1% in 6-12 yr olds, with no gender
prevalence.
An organic etiology is present in fewer than 5% of children with primary
enuresis and in only 1% of children with primary nocturnal enuresis.
clinical manifestations of organic causes include incontinence, dysuria,
frequency, hematuria, straining on urination, dribbling, small caliber
stream, stress incontinence (with coughing, lifting, or running), gait
disturbance, poor bowel control, and continuous dampness.
A careful history and physical examination can rule out unusual causes.
Urinalysis and a urine culture should be performed at the initial visit.
Treatment
is usually, not recommended before age 6 yr because
spontaneous cure rates are high.
Even after age 6 yr, the spontaneous cure rate for primary enuresis is
15%/yr; for secondary enuresis without an organic cause, spontaneous
cure rates are also high.
NON PHARMACOLOGIC TREATMENT
1.
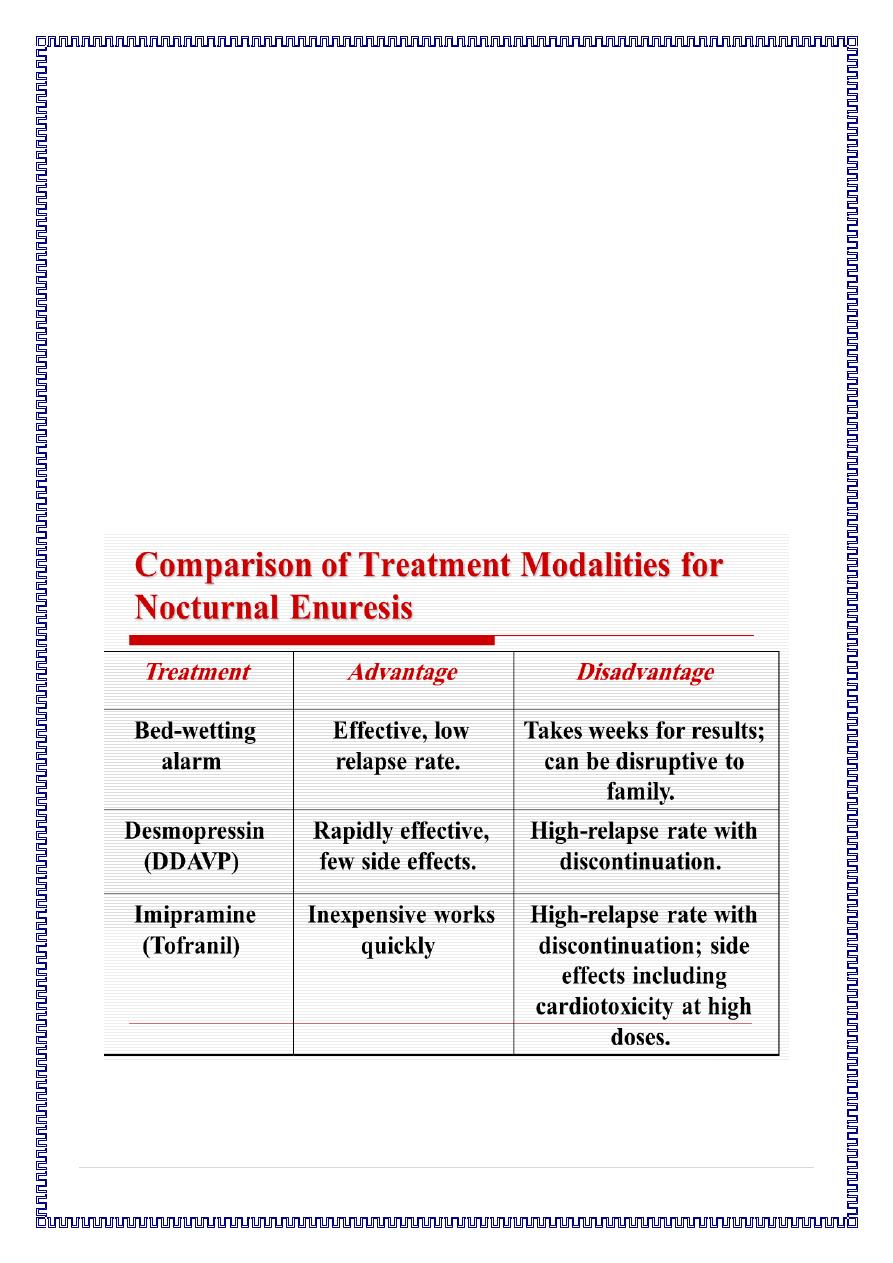
Bed-Wetting Alarm. The concept of using an alarm that emits a
sound when a child wets the bed was first introduced in 1938.
The bedwetting alarm has been shown to be the most effective
treatment for nocturnal enuresis. Compared with other skill-based
or pharmacologic treatments, the bed-wetting alarm has a higher
success rate (75 percent) and a lower relapse rate (41 percent).
3
|
Fatima Ehsan
P a g e
2.
Positive Reinforcement Systems. In one positive reinforcement system,
the child puts stickers on a chart or earns points for every night he or she
remains dry. Once a certain number of stickers or points have been earned,
the child is given a prize.
3.
Responsibility Training. With this technique, the child is given age-
appropriate responsibility, in a non punitive way, for the consequences of
bed-wetting.
PHARMACOLOGIC TREATMENT
Desmopressin (DDAVP) and imipramine (Tofranil) are the primary drugs
used in the treatment of nocturnal enuresis.
Pharmacologic treatment is not recommended for children under six years
of age.
Desmopressin.
A synthetic analog of arginine vasopressin, desmopressin works by
decreasing urine volume at night and by decreasing intravesicular
pressure.
The drug comes in a nasal spray or tablet. Treatment using the nasal
spray is initiated with 10 mcg given at bedtime, one half of the dose in
each nostril. The 0.2-mg tablet is taken at bedtime.
desmopressin is well tolerated. Side effects, which include nasal
irritation, nosebleeds, and headache, are generally mild. emotional
disturbances, including aggressive behavior and nightmares, which
resolved when the medication was discontinued.
Once desmopressin therapy is stopped, relapse rates can range from 80 to
100 percent. If children respond to desmopressin, treatment is continued
for three to six months. To minimize the possibility of relapse, the drug
should be discontinued slowly.
4
|
Fatima Ehsan
P a g e
Imipramine:
has a high rapid initial response rate within the first week, but the relapse
rate after discontinuation of the drug is so high that the long-term cure
rate when the patient is taken off the drug is barely above the
spontaneous cure rate.
The dose of imipramine is 50 mg before bedtime for 8-12 yr olds and 75
mg for children over age 12 yr. After 1 mo without enuresis, the drug
should be tapered over 2-4 wk.
Untoward effects include anticholinergic symptoms, bone marrow
suppression, and life-threatening accidental ingestions.
Blood counts should be taken every 2-4 wk while the patient is on therapy.
