Pediatrics Lec 6 Dr. Ziyad
1
PREMATURITY & INTRAUTERINE
GROWTH RETARDATION
DEFINITIONS
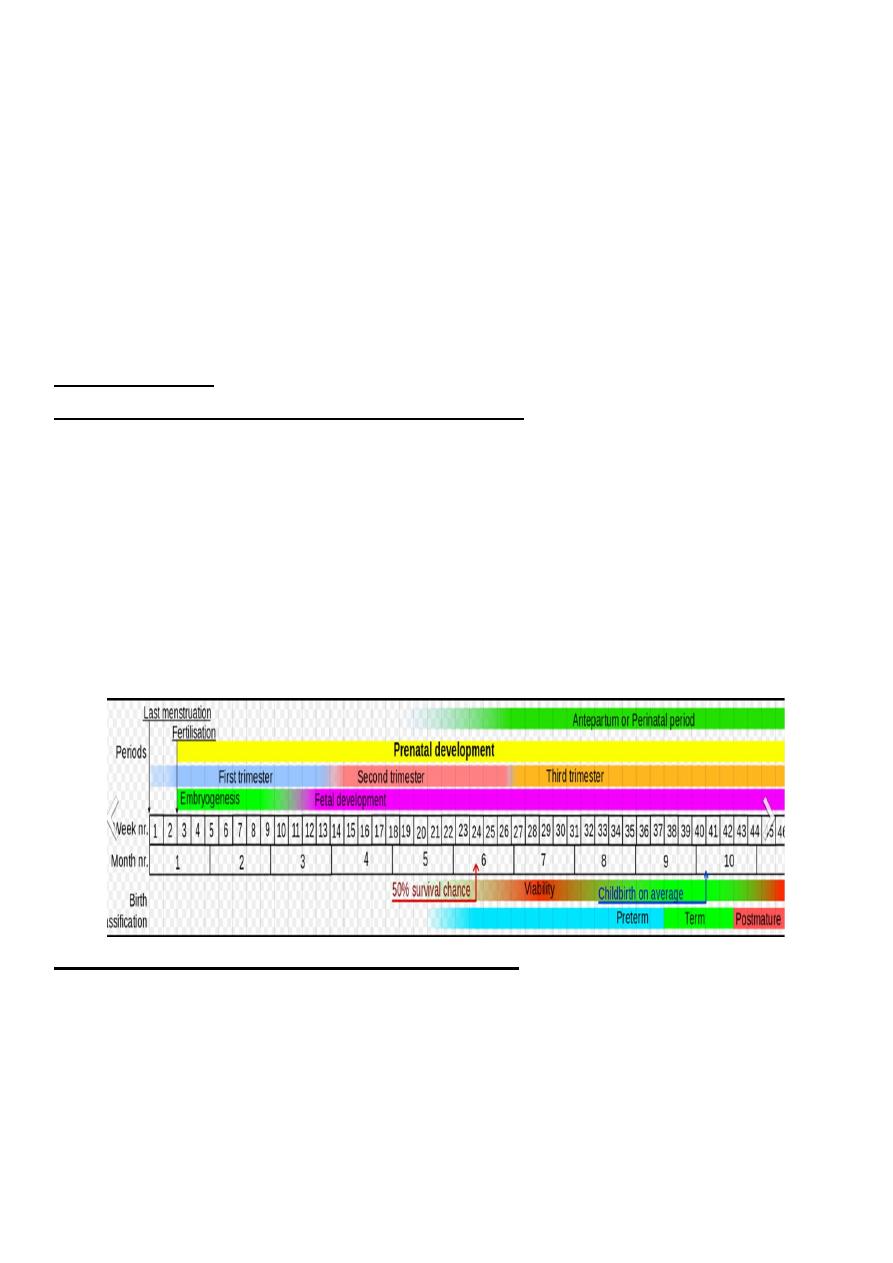
GESTATION (INDEPENDENT OF BIRTH WEIGHT)
Preterm: less than 37 completed weeks of gestation (259 days)
Full term:
between 38 weeks and 41 completed weeks of gestation (259 –293 days)
Post-term or postmature: more than 42 weeks.
Dates are taken from the first day of the last menstrual period.
Conception is presumed to be approximately 2 weeks after this date.
Ultrasound dates are based on conception and have to be altered to fit with the
dates estimated from the last menstrual period.
BIRTH WEIGHT (INDEPENDENT OF GESTATION)
Low birth weight (LBW): less than 2500 g.
Very low birth weight (VLBW): less than 1500 g.
Extremely low birth weight (ELBW): less than 1000 g.
Pediatrics Lec 6 Dr. Ziyad
2
SIZE FOR GESTATION
Small for gestation (SGA): less than 10th centile in weight expected for
gestation (small for dates).
Appropriate for gestation (AGA): between 10th and 90th Gentiles of weight
expected for gestation.
Large for gestation (LGA): more than 90th centile in weight expected for
gestation.
AGE IN UTERO
Less than 1 week: fertilized egg to the formation of the blastocyst.
1-12 weeks: embryo.
12 weeks – delivery: fetus.
24 weeks or more: current period of 'legal' viability.
Premature: Live born infants delivered before 37 wk from the 1st day of the last
menstrual period are termed premature by the World Health Organization.
(Low birth weight may be due to prematurity or poor intrauterine growth (IUGR,
also referred to as SGA).
Prematurity and IUGR are associated with increased neonatal morbidity and
mortality. VLBW infants account for over 50% of neonatal deaths and 50% of
handicapped infants. Their survival is directly related to birth weight.
FACTORS RELATED TO PREMATURE BIRTH:
The etiology of preterm birth is multifactorial and involves a complex
interaction between fetal, placental, uterine, and maternal factors.
A strong positive correlation exists between both preterm birth and IUGR and
low socioeconomic status.
Families of low socioeconomic status have higher rates of maternal under-
nutrition, anemia, and illness; inadequate prenatal care; drug misuse; obstetric
complications; and maternal histories of reproductive inefficiency (abortions,
stillbirths, premature or LBW infants).
Pediatrics Lec 6 Dr. Ziyad
3
IDENTIFIABLE CAUSES OF PRETERM BIRTH:
Fetal
Fetal distress.
Erythroblastosis
Multiple gestation.
Nonimmune hydrops
Placental
Placenta previa.
Abruptio placentae
Uterine
Bicornate uterus.
Incompetent cervix.
(premature dilation)
other
Maternal
Pre–eclampsia Chronic medical illness (e.g.,
cyanotic heart disease, renal disease)
Drug abuse(cocaine),Infection (e.g., Listeria
monocytogenes, group B streptococcus, urinary
tract infection)
Iatrogenic.
Premature rupture
membranes.
Polyhydramnios.
FACTORS ASSOCIATED WITH INTRAUTERINE GROWTH RETARDATION
IUGR is associated with medical conditions that interfere with the circulation
and efficiency of the placenta, with the development or growth of the fetus, or
with the general health and nutrition of the mother.
Intrauterine growth retardation often classified as reduced growth that is
symmetric (head circumference, length, and weight equally affected) or
asymmetric IUGR (with relative sparing of head growth).
Symmetric IUGR often has an earlier onset and is associated with diseases that
seriously affect fetal cell number, such as conditions with chromosomal,
genetic, malformation, teratogenic, infectious, or sever maternal hypertension.
Asymmetric IUGR is often of late onset and associated with poor maternal
nutrition or with late onset or exacerbation of maternal vascular disease
(preeclampsia, chronic hypertension).
Pediatrics Lec 6 Dr. Ziyad
4
IDENTIFIABLE CAUSES OF INTRAUTERINE GROWTH RETARDATION:
1.Fetal
Chromosomal disorders (e.g., autosomal trisomies).
Chronic fetal infections (e.g., cytomegalic inclusion disease, congenital
rubella, syphilis).
Congenital anomalies - syndrome complexes
Radiation injury.
Multiple
gestations.
Pancreatic aplasia.
2. Placental
Decreased placental weight or cellularity or both.
Decrease in surface area.
Vinous placentitis (bacterial, viral, parasitic Infarction).
Tumor (chorioangioma, hydatidiform mole).
Placental separation.
Twin transfusion syndrome (parabiotic syndrome).
3. Maternal
Toxemia.
Hypertensive or renal disease or both.
Hypoxemia (high altitude, cyanotic cardiac or pulmonary disease).
Malnutrition or chronic illness.
Sickle cell anemia.
Drugs (narcotics, alcohol, cigarettes, cocaine, antimetabolites).
DISEASE IN LOW-BIRTH WEIGHT INFANTS:
Immaturity increases the severity but reduces the distinctiveness of the clinical
manifestations of most neonatal diseases.
Among VLBW infants, morbidity is inversely related to birthweight. Respiratory
distress syndrome, Severe intraventricular hemorrhage (IVH, late sepsis,
bronchopulmonary dysplasia, necrotizing enterocolitis, and prolonged
hospitalization (45-125 days) is high in VLBW infants.
Pediatrics Lec 6 Dr. Ziyad
5
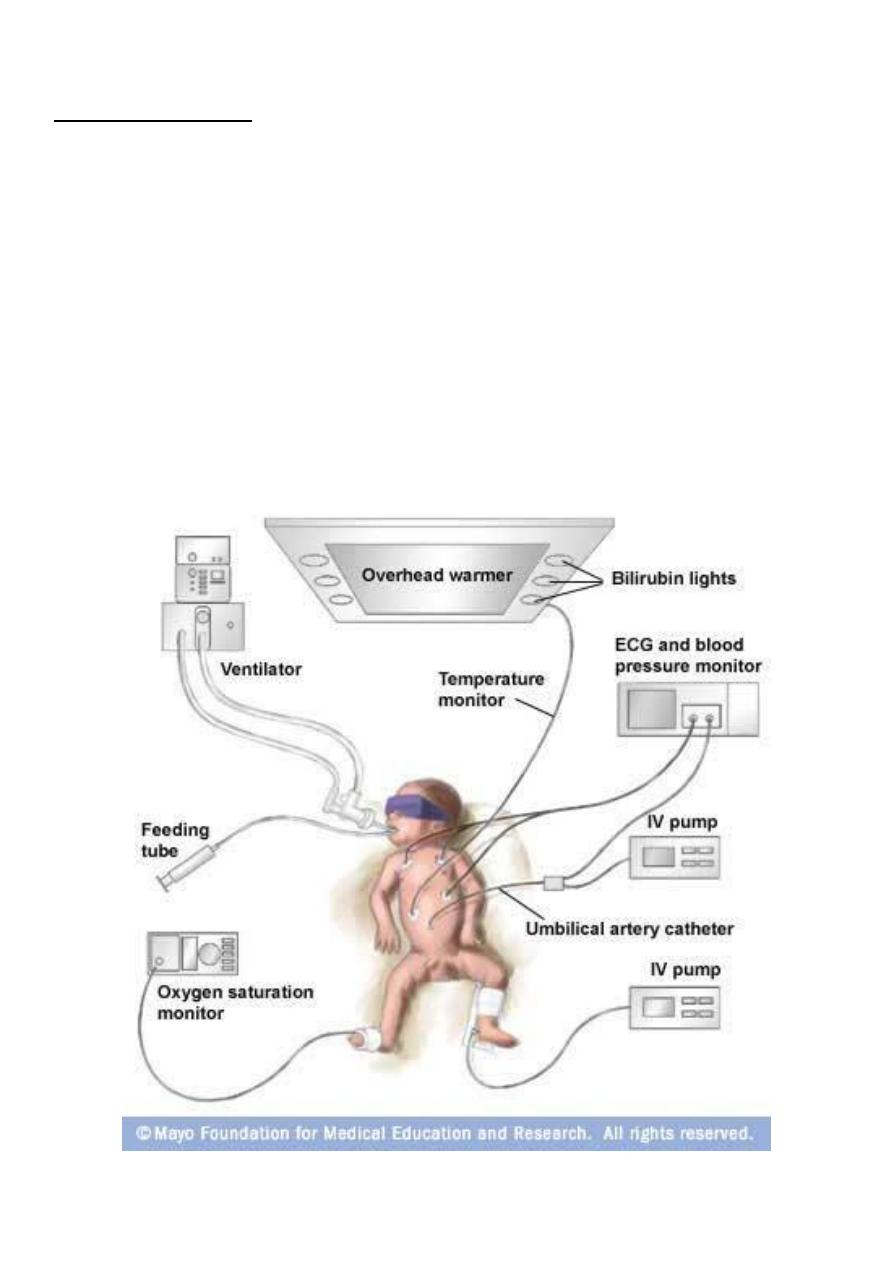
NURSERY CARE:
At birth, the measures needed to clear the airway, initiate breathing, care for
the umbilical cord, and eyes, and administer vitamin K are the same for
immature infants as for those of normal weight and maturity.
Special care is required to maintain a patent airway and avoid potential
aspiration of gastric contents. Additional considers are the needed for:
1. Thermal control and monitoring of the heart rate and respiration.
2. Oxygen therapy.
3. Special attention to the details of feeding.
Routine procedures that disturb these infants may result in hypoxia.

Pediatrics Lec 6 Dr. Ziyad
6
Thermal Control:
The survival rate of LBW and sick infant is higher when they are cared for at or near their
natural thermal environment.
This environment is a set of thermal conditions including air and radiating surface
temperatures, relative humidity, and airflow, at which heat production is minimal and the
infant's core temperature is within the normal range. This depends on size and postnatal
age of an infant; larger, older infant require lower environmental temperatures than
smaller younger infant.
(Incubators) or radiant warmers can be used to maintain body temperature. Body heat is
conserved through provision of a warm environment and standard conditions of humidity.
The optimal environmental temperature for minimal heat loss and oxygen consumption for
an unclothed infant is one that maintains the infant's core temperature at 36.5-37 °C.
It depends on infant size and maturity; the smaller and more immature infant, the higher
the environmental temperature required.
Continuous monitoring of the infant's temperature is required so that the environmental
temperature can be adjusted to maintain optimal body temperature
Kangaroo mother care with direct skin to skin contact and hat and blanket covering the
infant is a safe alternative with careful monitoring to avoid the risk of serious hypothermia
when incubators are unavailable or when the infant is stable and the parent desire close
contact with their infant.
Maintaining a relative humidity of 40-60% aids in:
1. Stabilizing body temperature by reducing heat loss at lower environmental
temperatures.
2. Preventing drying and irritation of the lining of respiratory passages, especially during
the administration of oxygen and after or during endotracheal intubation.
3. Thinning viscid secretion and reducing insensible water loss from the lungs.
Administering oxygen to reduce the risk of injury from hypoxia and circulatory insufficiency
must be balanced against the risk of hyperoxia to the eyes (retinopathy of prematurity) and
oxygen injury to the lungs.
Oxygen should be administered via a head hood, nasal cannula, continuous positive air way
pressure apparatus, or endotracheal tube to maintain stable and safe inspired oxygen
concentrations.
Although cyanosis must be treated immediately, oxygen is a drug and its use must be
carefully regulated to maximized benefit and minimize potential harm.
The concentration of inspired oxygen must be adjusted in accordance with the oxygen
tension of arterial blood (Pao2) or non invasive methods such as continuous pulse oxymetry
or transcutaneuos oxygen measurements. Capillary blood gases are inadequate for
estimating arterial oxygen measurement.
