Obstetrics
Lec 3
Dr.
Aseil
1
The placenta
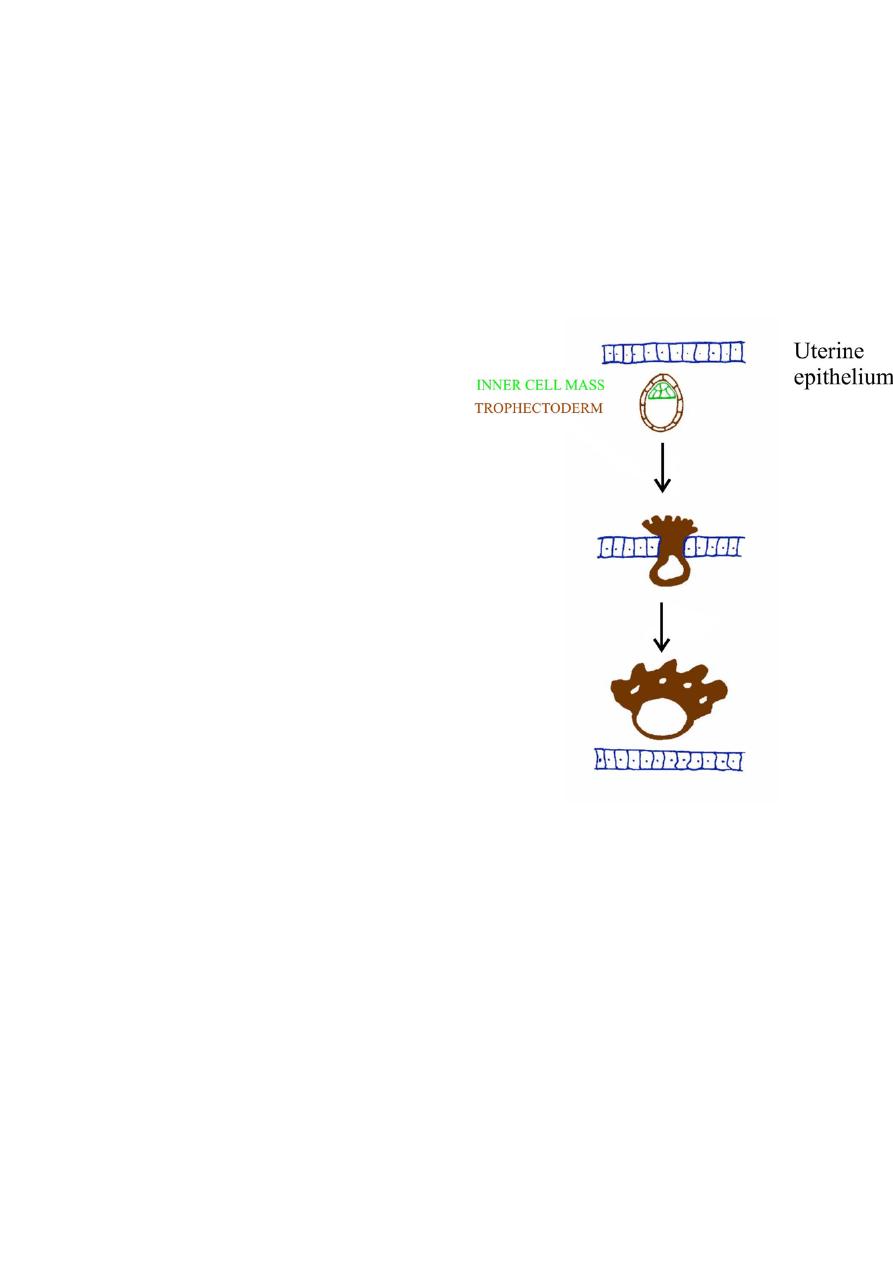
Attachment and implantation into uterine wall
• Blastocyst passes between uterine
epithelial cells
• Trophectoderm around outside of
blastocysts gives rise to placenta
• Inner cell mass to embryo
• Trophoblast cells (from
trophectoderm) proliferate
• Migrate into uterine wall to establish
placenta
• Uterine epithelium closes behind
• Early placental (trophoblast) cells
secrete HCG – to maintain corpus
luteum
How does placenta form?
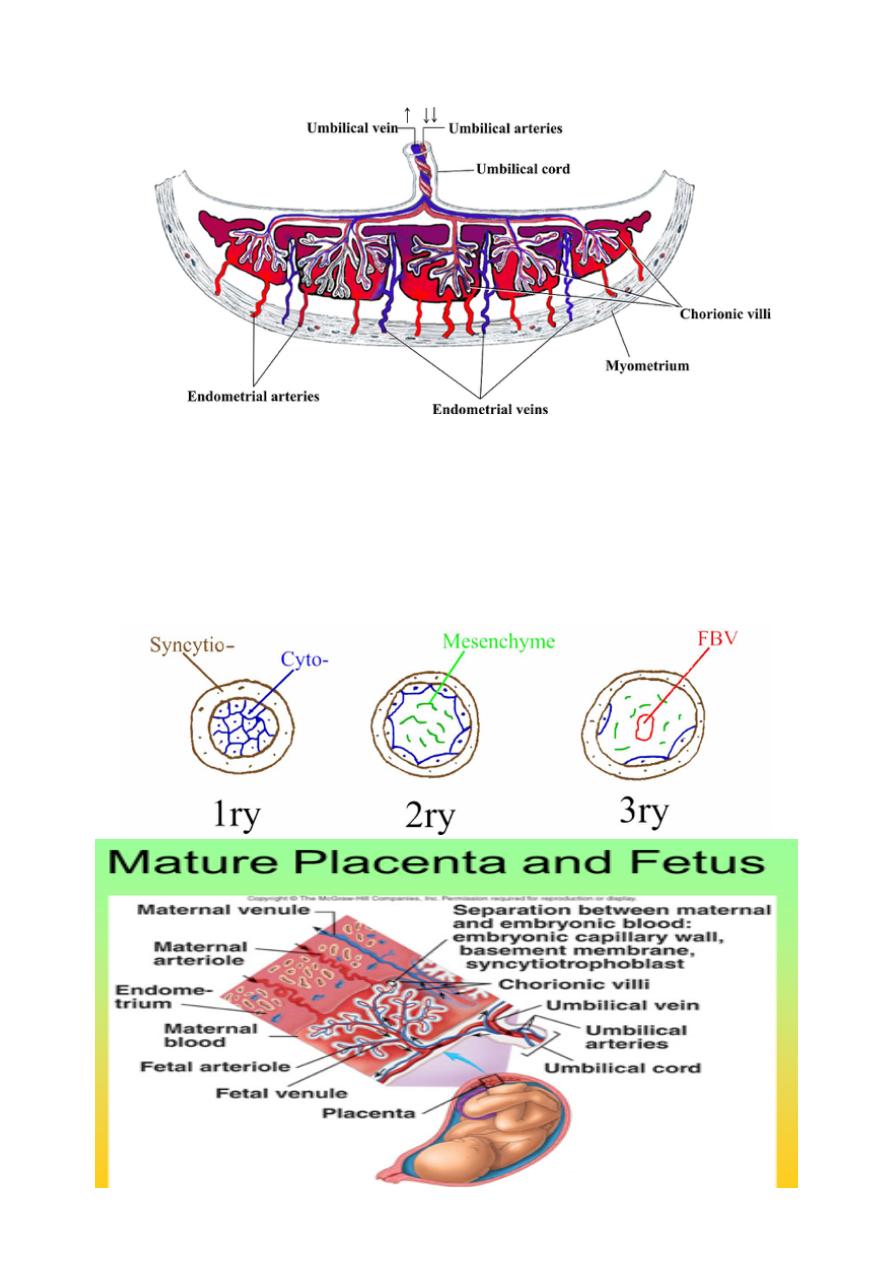
• Proliferated trophoblast on embryonic pole differentiates into outer
layer of syncytio-trophoblast and inner cyto-trophoblast
• Lacunae develop on syncytiotrophoblast layer into which maternal
blood passes
• Villi of syncytiotrophoblast with inner core of cytotrophoblast develop
floating in sinuses
Obstetrics
Lec 3
Dr.
Aseil
2
Placenta
Floating villi
Primary to secondary to tertiary villi by end of 3
rd
week of gestation consist of
2 layers of trophoblast; cytotrophoblast and syncytiotrophoblast, with an inner
core of mesoderm inside which fetal blood is running. The thickness will
decrease after 20 th weeks because of disappearance of mesoderm and
cytotrophoblast.

Obstetrics
Lec 3
Dr.
Aseil
3
What is a placenta?
• Generally regarded as the site at which there is exchange of gasses and
nutrients between maternal and foetal blood
• Site has separate maternal and foetal blood circulations which do not mix :
• It is a discoid shaped organ of 15 -20 lobules. It‘s fetal surface covered with
amnion while maternal surface consist of lobules of compressed villi
separated from each other by sulci.
Placental function
1-Placenta provides anchorage, establishes fetal vascular network in association
with maternal blood supply but without mixing.
2-
Gaseous exchange(Respiratory function) umb .vein carry O2 from placenta to the
fetus while umb. Artery carry deoxygenated blood from the fetus to the mother
3-
Nutritional function: transferring substance important for fetal growth e.g
glucose ,a.a , lipids, Ab also synthesize and store some substances like glycogen.
4-Placenta act as endocrine gland :secraeting hormones & enzymes
5-Barrier function: the placental filters out some substances which could harm
the foetus e.g blood borne pathogens, Drugs but not all (alcohol, soscial drugs
&some viruses e.g CMV)
6-Immunological protection?:it protects fetus from rejection .
Placenta as a filter/transfer organ
Receives nutrients, oxygen, antibodies and hormones from the mother and passes
out waste There are many factors influencing the placental transfer as:
1- Nature of the substance whether fat- solube or not &their molecular size.
2- Thickness of the barrier which depend on gestational age.
3- Surface area available for transfer.
4- Rate of circulation across the barrier.
Obstetrics
Lec 3
Dr.
Aseil
4
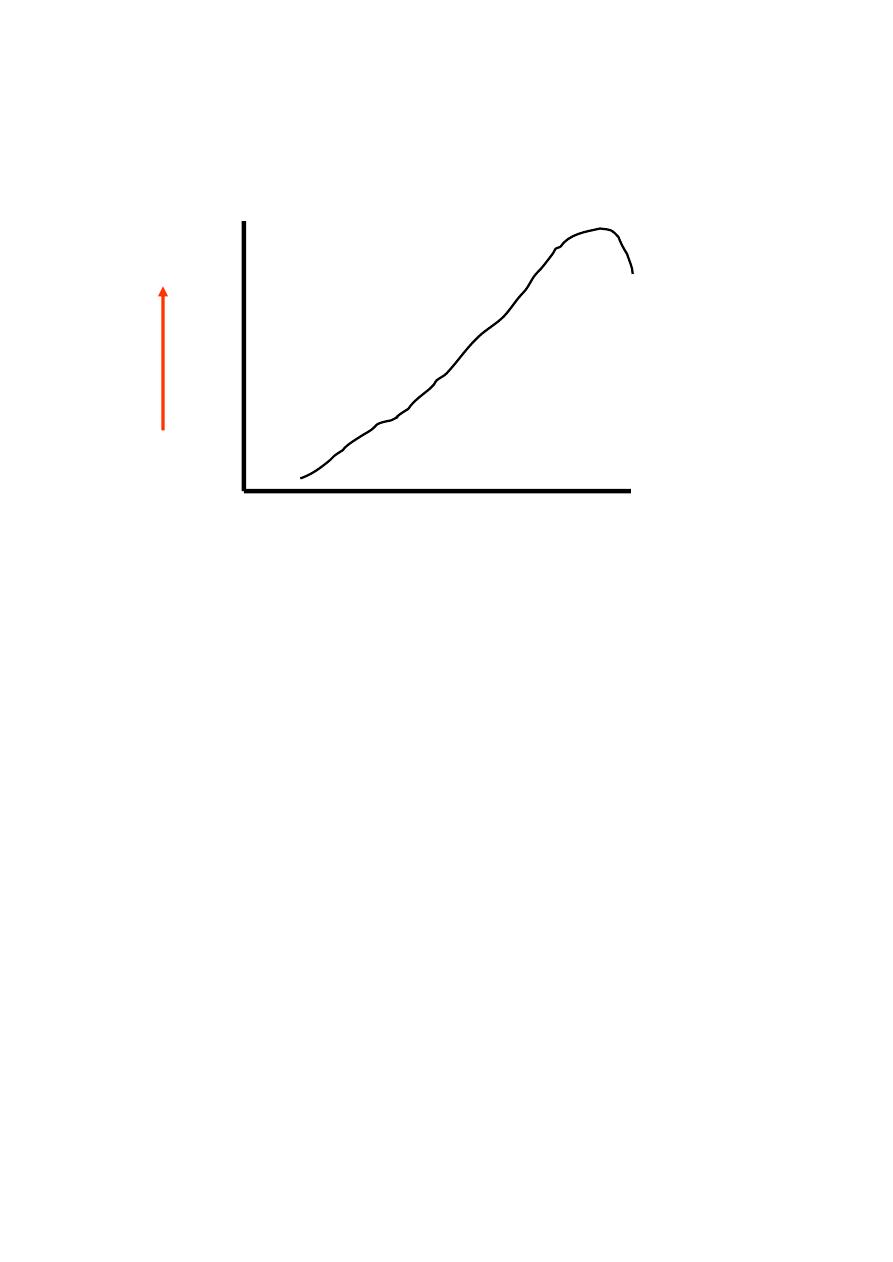
The Placenta
• The transfer of substance across the placenta occurs by several mechanisms
• Permeability of the placenta increases constantly – reaches a peak in the last
month – sharp decrease in permeability.
Mechanism of transfer
1- Simple diffusion : transport from high to lower pressure e.g CO2, O2 H2O and
electrolyte.
2- Facilitated diffusion : by carrier system as glucose, vitamins & minerals .
3- Active transport : in which high energy is required to carry substance against
pressure gradient e.g. Heavy materials , Iron& amino acids..
Placenta as an endocrine gland
• HCG (Human chorionic gonadotropin) - maintains ovariean corpus luteum
• Progesterone – maintains pregnancy (especially after 1
st
trimester)
• Sommatomammotropin (Placental lactogen – increases maternal blood
glucose and lipids
• Oestrogen
• Relaxin
• Prostaglandins
• Enzymes&proteins e.g alkaline phosphates, oxytokinase, lactic
dehydrogenase and Insulinase.
P
er
m
e
a
bi
lit
y
0
8
20
40

Obstetrics
Lec 3
Dr.
Aseil
5
HCG
It is produced by cytotrophoblast detected in maternal blood from 10 th day of
fertilization &peaks at 60-90ds then decline to amoderate constant level
1-For the 1
st
6-8w of pregnancy it maintains the corpus luteum to ensure
continued progesterone out put until production shifts to the placenta
2-regulate steroid biosynthesis in the placenta & fetal adrenal gland
&stimulates the fetal testicle to secrete testosterone .
Human placental lactogen (HPL)
It is protein produced by syncytotrophoblast found in blood. It is level rise slowly
up to 40 weeks of pregnancy.
It is like growth hormone, it thought to be one of causes of big baby. Decreases
maternal insulin sensitivty &Promotes release of FFA from maternal stores –
alternative source of energy for her metabolism. HPL level is low in case of;
threatended abortion , antpartum hemorrhage& IUGR
Oestrogen
It is steroid produced by feto-placental units from fetal liver , adrenals and
placental cytotrophoblast.
The level increase in early pregnancy up to 38 weeks reaching static level then
after 39 weeks it decrease. It originates from corpus luteum in early pregnancy
then from the placenta. Estriol is the most abundant form in pregnancy &can be
used as indicator for placentl function sudden decline of esteriol in maternal
circulation indicate fetal compromise.
Progesterone:
It is steroid produced by CL in 1
st
6-7w of pregnancy thereafter by placental
syncytiotrophoblast ( no fetal role ).
The level of progesterone increase in the pregnancy from early stage until the
onset of labour.

Obstetrics
Lec 3
Dr.
Aseil
6
It is important for support of pregnancy and increased vascularity of the placental
bed.It prevents uterine contraction &play acentral role in maintaining uterine
quiescence throught pregnancy.
a- Feto-protein
It is a protein that has certain level in every person, but it increased in cases of
liver tumor & during pregnancy. Secreted by; fetal membrane and yolk sac.
It is increased from 10 th week of pregnancy. It is increased in: Threatened
abortion, Twin, Fetal abnormality as neural tube defect. It is low IUD & Dawins
syndrom
Amniotic fluid
It surrounds the fetus, produced by:
1- In early pregnancy secreated by amnion,but by 10
th
w it is mainly atransudate
of fetal serum via the skin & umbilical cord .
2- From 16w the net increase in AF is through asmall imbalance between urine &
lung fluids secreation& removal by fetal swallowing.
It’s volume increases progressively(10w:30ml, 20w:300ml,38w:1000ml) but from
term there is rapid fall in volume(40w:800ml,42w:350ml)
Function of amniotic fluid
1-It protect fetus mechanical injury
2-Allows room for fetal growth movement &development while preventing limb
contracture
3-Is of value for assessing fetal well being when it is reduced in renal agenesis,
cystic kidneys or fetal growth restriction oligohydramnios results but when there
is reduced removal of fluid in conditions like anencephaly & esophageal/
duodenal artesia polyhydramnios results.
4-Permits fetal lung development as there is two-way movement of fluide into the
fetal bronchioles & its absence in 2
nd
trimester is associated with pulmonary
hypoplasia.
