Obstetrics Lec 1 Dr. Eman
1
Management of
Normal Labour
By:brwa
Preparation for labor
1. lightening: 2 or more weeks before labour , fetal head in primigravida settles
into pelvic brim. In multigravida lightening occur early in labour .Lightening
can be noted by mother as flattening of upper abdomen and increase
prominence of lower abdomen.
2. False labour: during last 4-8 weeks of pregnancy uterus undergoes irregular
contractions which are painless.
Such contractions are unpredictable, Sporadic ,of mild intensity & painless.
These Braxton Hicks contraction are considered false labour because they are
not associated with Progressive cervical dilatation or effacement . They serve a
physiologic role in preparing uterus and cervix for true labor.
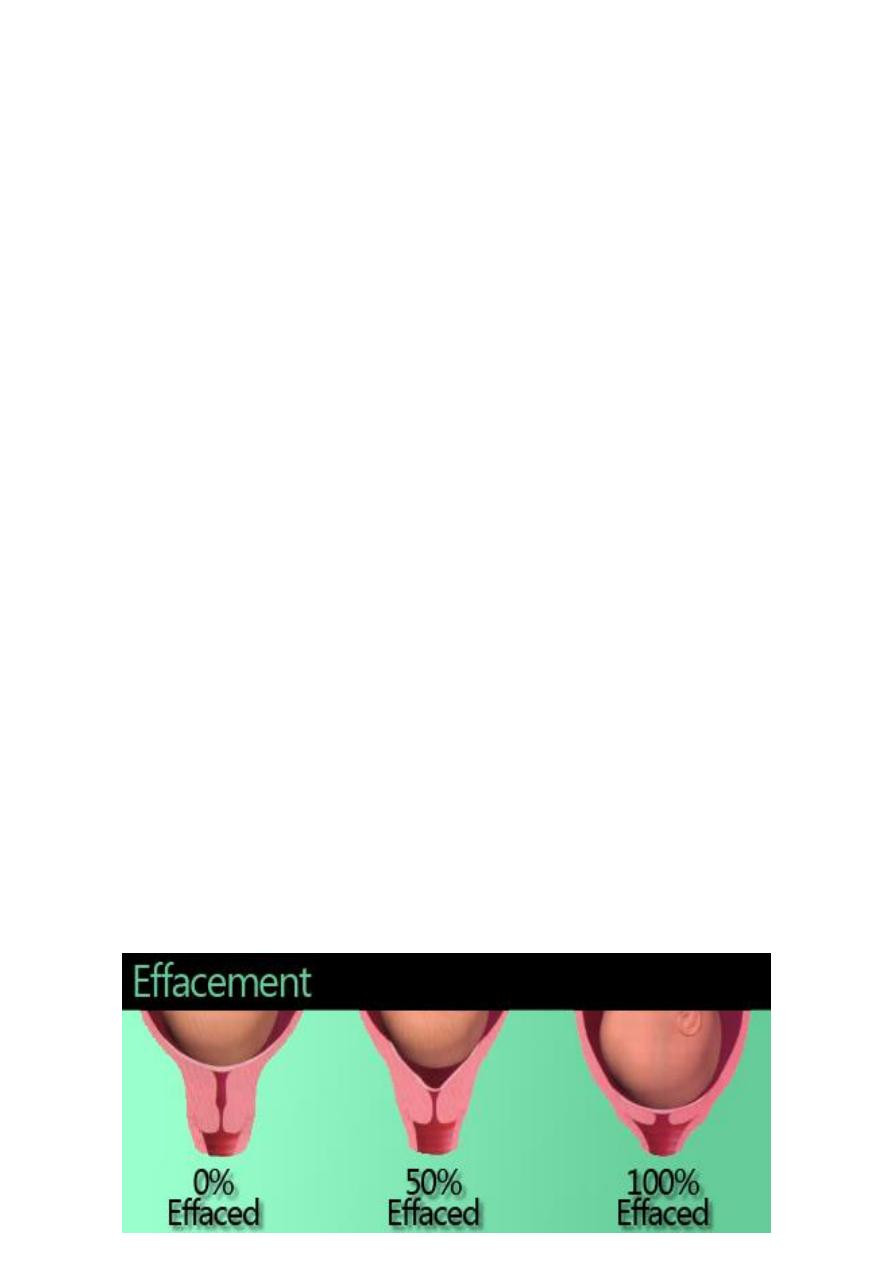
3. Cervical effacement: before onset of labor, cx is noted to soften as a result of
increased water content and collagen lysis , effacement or thinning of cx occurs
as it is taken up into the lower uterine segment. Patient usually present early in
labour with partially effaced cx. As a result of cx effacement , the mucus plug
within cervical canal may be released . The onset of labour is heralded by
passage of a small amount of blood-tinged mucus from vagina (bloody show)
Obstetrics Lec 1 Dr. Eman
2
Stages of labour :
1
st
stage: from onset of labour to complete dilatation of cervix.
2
nd
stage : from complete dilatation of cx to birth of baby .
3
rd
stage : from birth of baby to delivery of placenta .
4
th
stage : from delivery of placenta to stabilization of maternal condition
usually at about 6 hours post partum.
1
st
stage:
consist of 2 phases, a latent phase during which cx effacement and early
dilation occur, and active phase which begins when the cx is 3-4 cm dilated .
The minimal dilation during active phase is nearly similar for primi and multi : 1
and 1.2 cm\hr respectively . If progress is slower than this , evaluation for
uterine dysfunction , fetal malposition , or CPD should be undertaken.
Measurement of progress:
In 1
st
stage of labour progress can be measured in term of cx effacement , cx
dilation , and descent of fetal head , while in 2
nd
stage of labor progress can be
assessed in term of descent, flexion, and rotation of presenting part.
Clinical management of 1
st
stage:-
1. Maternal position: the mother may ambulate provided that intermittent
monitoring ensures fetal wellbeing and presenting part is engaged in patient
with ruptured membrane. If she is lying in bed , left lateral position should be
encouraged to ensure adequate uteroplacental perfusion.
2. Administration of fluid: because of decreased gastric emptying during labour ,
oral fluid are best to be avoided, fasting is associated with more rapid
development of ketosis , so i.v fluid is given in form 10%dextrose in normal
saline at rate of 125ml\hr , thus i.v route is used to hydrate the patient with
crystalloid , to provide calories , to administer oxytocin after delivery of placenta
, and to deal with unexpected emergency.

Obstetrics Lec 1 Dr. Eman
3
3. Investigation : every women admitted in labour should have Hb
measurement , cross match , blood group &Rh, and MSU should be sent for
protein and glucose.
4. Maternal monitoring: PR, BP, RR, Temp, should be recorded every 1 hr in
normal labour and more frequently if indicated. Fluid balance including input
and urine output should be monitored.
5. Analgesia : adequate analgesia is important in 1
st
stage of labour.
6. Fetal monitoring: in patient with no significant obstetric risk factor , the fetal
heart rate should auscultated every 30 minute in the active phase and at least
every 15 minute in 2
nd
stage. In patient with obstetric risk factor , FHR should be
auscultated every 15 minute in active phase (immediately following uterine
contraction) , and at least every 5 minute during 2
nd
stage.
7. Uterine activity :uterine activity should be monitored every 30 minute by
palpation for their frequency , duration , and intensity.
for high risk pregnancy , uterine contraction should be monitored continuously
with FH . This can be done either by external tocodynamometer or by internal
pressure catheter in amniotic cavity
8. Vaginal examination : in latent phase, especially when there is ROM , pv
should be done sparingly to decrease risk of infection while in active phase , pv
can be done every 2 hr
9. ARM: ARM provide information on volume of AF , presence of meconium and
cause increase in uterine contraction but increase risk of infection if labour is
prolonged , risk of cord compression or cord prolapse if presenting part is not
engaged.
Obstetrics Lec 1 Dr. Eman
4
Second stage :
at beginning of 2
nd
stage , mother has desire to bear down with each
contraction, this abdominal pressure with uterine contraction , combines to
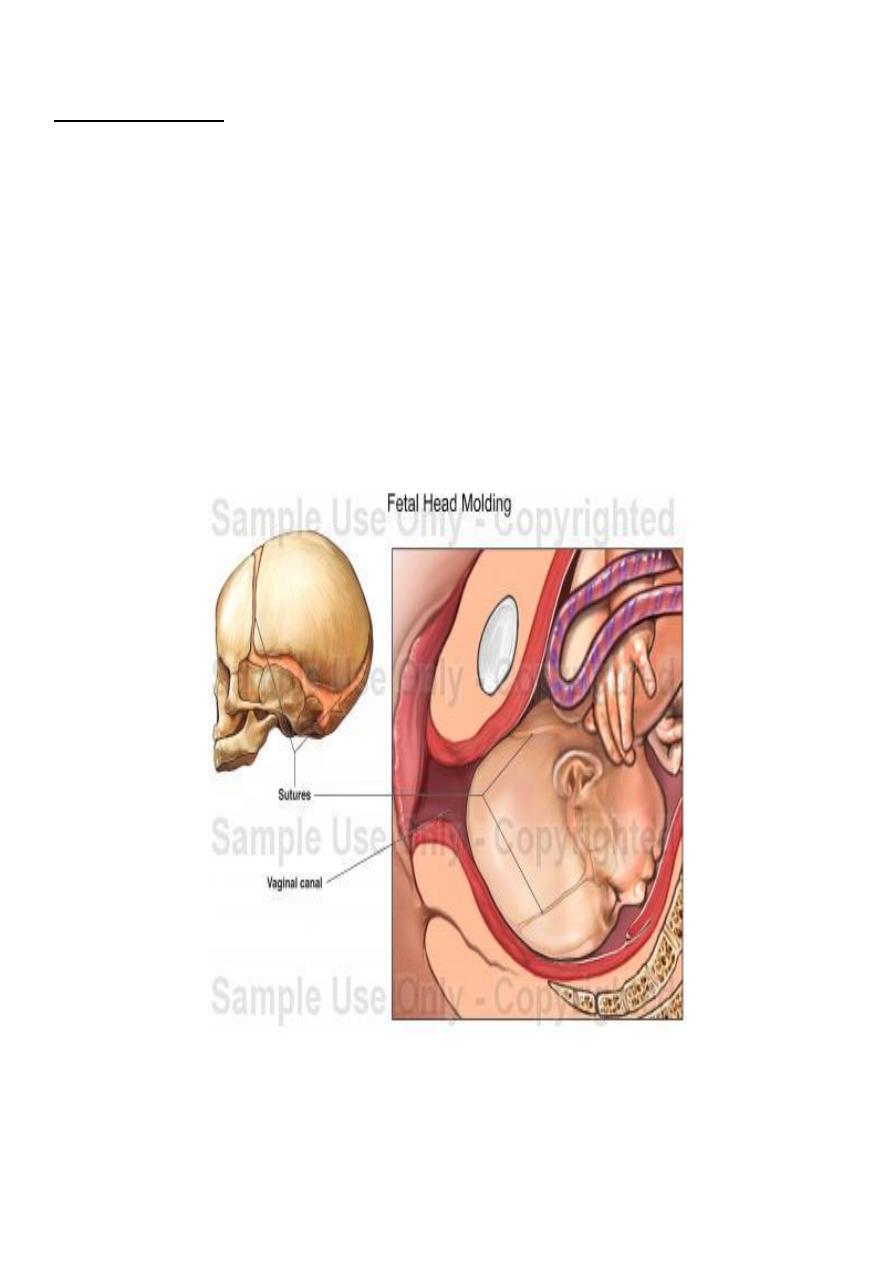
expel fetus .In cephalic presentation , shape of fetal head may be altered during
labour .
molding is alteration of relationship of fetal cranial bone to each other as a
result of compressive forces exerted by bony pelvis. Some molding is essential
for delivery , in CPD the amount of molding is excessive.
Caput : is a localized , oedematous swelling of scalp caused by pressure of cervix
on presenting part of fetal head.
Obstetrics Lec 1 Dr. Eman
5
Management of 2
nd
stage of labor:
1. Maternal position: with exception of avoiding supine position , mother can
assume any comfortable position for effective bearing down.
2. Bearing down: with each contraction mother should be encouraged to
hold her breath &bear down with expulsive efforts
3. Fetalmonitoring :FHR should be monitored in 2
nd
stage continuously or
every 5 min in pt with risk factor .
4. 4. Vaginal examination :pv in second stage can be made every 30 min,
attention should be given to descent , flexion of presenting part , molding,
caput.
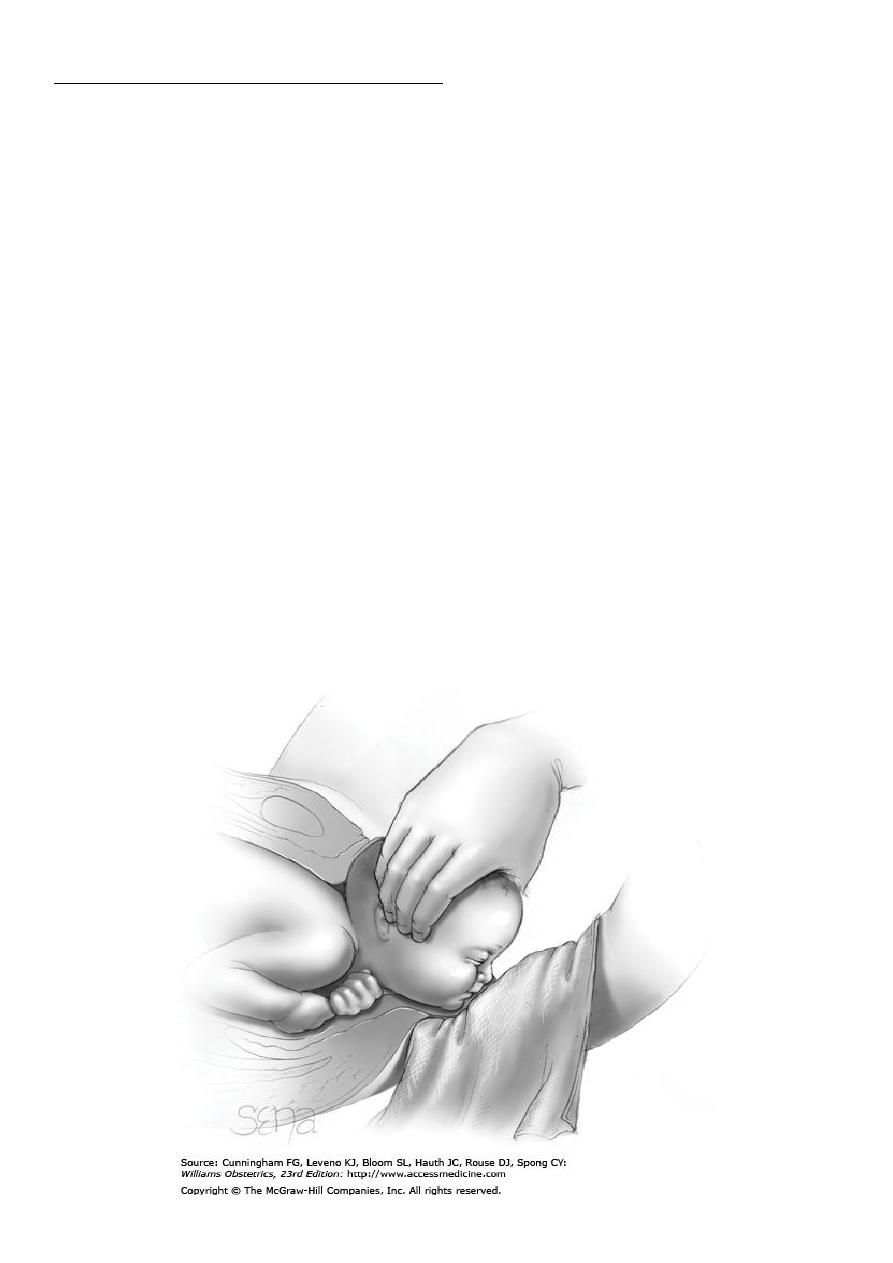
5. 5. Delivery of fetus : when delivery is imminent, pt is placed in lithotomy
position and skin over lower abdomen, vulva, anus & upper thigh in
cleansed with antiseptic solution. With crowning episiotomy can be
performed if indicated .
6. To facilitate head delivery , ritgenmaneuver may be performed in which Rt
hand , draped with a towel , exerts upward pressure through distended
perineal body this increase extension of head and prevent it slipping back
between contraction is counteracted by downward pressure on occiput
with left hand.
Obstetrics Lec 1 Dr. Eman
6
Once head is delivered , airway is cleared of blood and amniotic fluid using bulb
suction , oral cavity &nares are cleared. Suction of nares is not performed if
meconium –stained liquor or fetal distress is present because it may result in
gasping and aspiration of pharyngeal content. 2
nd
towel is used to wipe
secretion from face and head.
Index finger is used to check presence of cord around neck. If so cord can be
slipped over fetalhead &if too tight it can be cut between 2 clamps.
After head delivery anterior shoulder is delivered by downward traction and
posterior by upward elevation of head
After delivery blood will be infused from placenta to newborn if baby is held
below introitus . Cord is clamped in 15-20 sec , delayed cord clamping lead to
neonatal hyperbilirubinemia as additional blood pass from placenta to baby.
The newbornis placed then under infant warmer
Third stage:
After delivery of baby , cx, vx, & perineum should be inspected for any
laceration before placental separation because no uterine bleeding present to
obscure visualization.
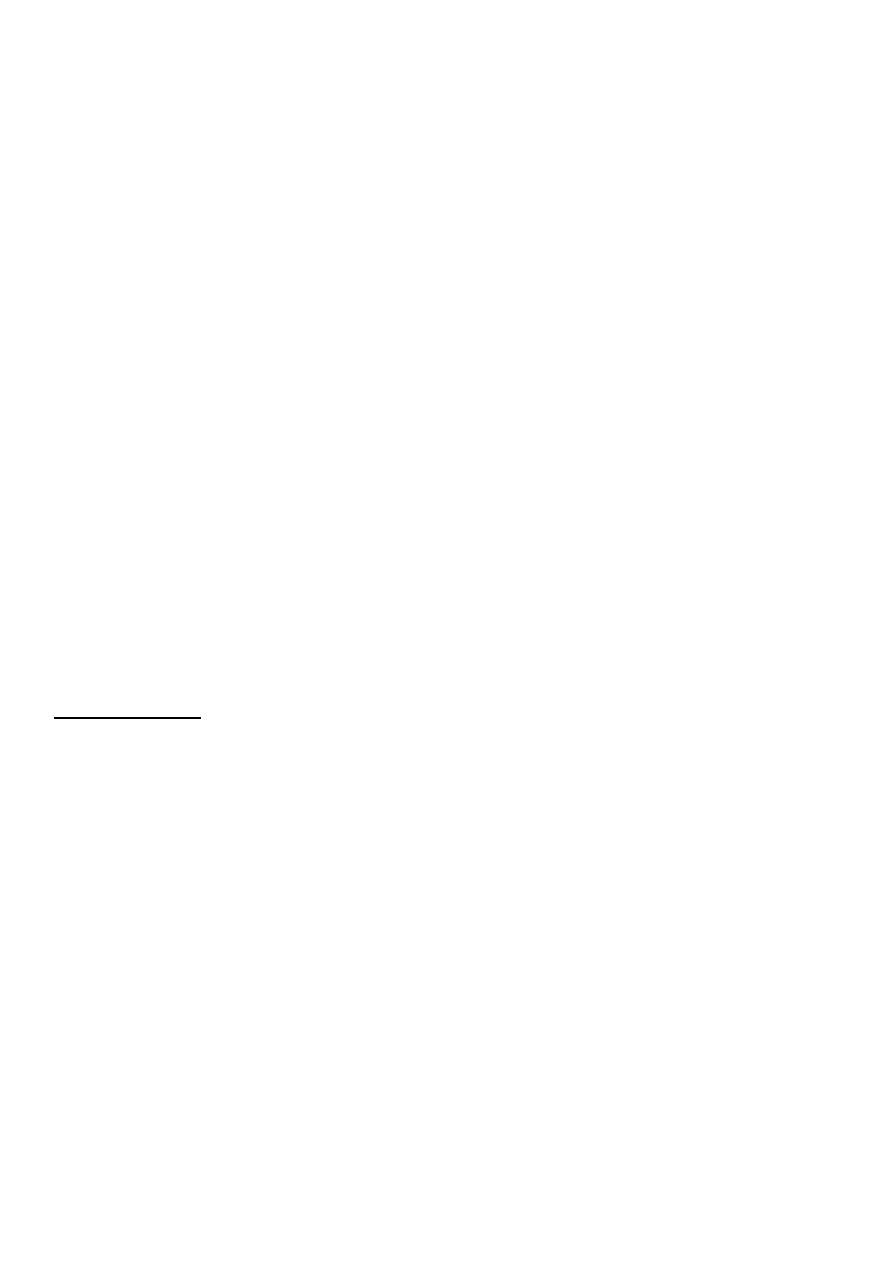
Delivery of placenta----separation of placenta occurs within 2- 10 min.
Squeezing of fundus to hasten placental separation is not recommended
because increase risk of passage of fetal cells to maternal circulation.
Signs of placental separation
• Fresh show of blood from vagina .
• Umbilical cord lengthens outside vagina.
• Fundus of uterus rises up.
• Uterus become firm and globular.
When these signs appear , placenta can be delivered by CCT (cord is pulled
upward while abdominal hand press the fundus upward).
Obstetrics Lec 1 Dr. Eman
7
• Following placental delivery, attention should be given to any uterine
bleeding from placental site. Uterine contraction can reduce bleeding and
this can be stimulated by uterine massage & use of oxytocin. It is routine
to add 20 U of oxytocin to iv infusion after delivery ob baby
Placenta should be examined for complete removal & to detect placental
abnormalities. ifpt at risk of PPH (anaemia, prolonged labour, multiple
pregnancy and polyhydramnios) active mx of 3
rd
stage should be done (5U
Oxytocin+0.5 mg ergometrine) im with delivery of anterior shoulder of baby.
if episiotomy has been performed , should be sutured by absorbable sutures,
after suturing episiotomy PR should be performed to ensure that rectal mucosa
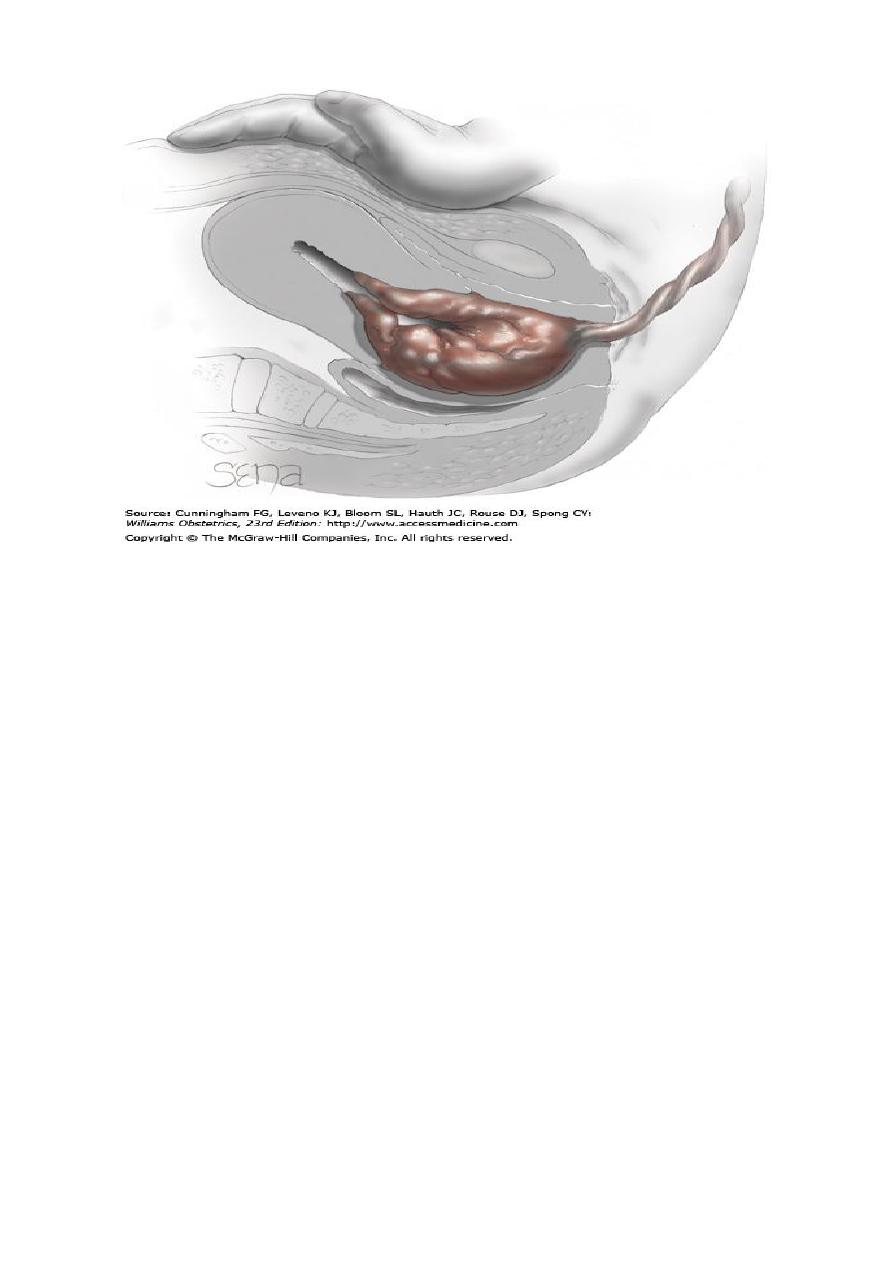
is not involved by stitches.Perineal tears:
1
st
degree—involve vaginal epithelia or perineal skin only.
2
nd
degree--- involvement of vaginal subepithelial tissues with or without
involvement of perineal muscle.
3
rd
degree--- involve anal sphincter.
4
th
degree--- involve rectal mucosa
Obstetrics Lec 1 Dr. Eman
8
4
th
stage :
In this stage close observation of BP, PR,RR ,Temp , uterine bleeding should be
done. It is time for PPH because of uterine relaxation , retained placental pieces
or unrepaired laceration . Occult bleeding (hematoma) manifest as pelvic pain .
Increase in PR out of proportion to decrease in BP indicate hypovolemia.
