1
Ante-partum fetal imaging & assessment
Antenatal assessment of fetal wellbeing
S The purpose of fetal testing is to assess the fetal wellbeing that
considered to be at increased risk, with the primary goal is to
prevent fetal death.
Methods of Fetal Assessment:
1. Maternal Assessment of Fetal Movement (Kick Counts):-
S The mother is asked to count the number of times she feels her
fetus move within a certain period of time, usually recommend
that this be done with the mother lying on her left side, after
having eaten.
S One approach is to have the mother count fetal movements
over the course of 1 hour. 4 or more movements are considered
reassuring.
S A second approach is to have the mother begin counting fetal
movements when she wakes up in the morning and record the
number of hours required to feel 10 movements. On average,
this takes 2 to 3 hours.
2
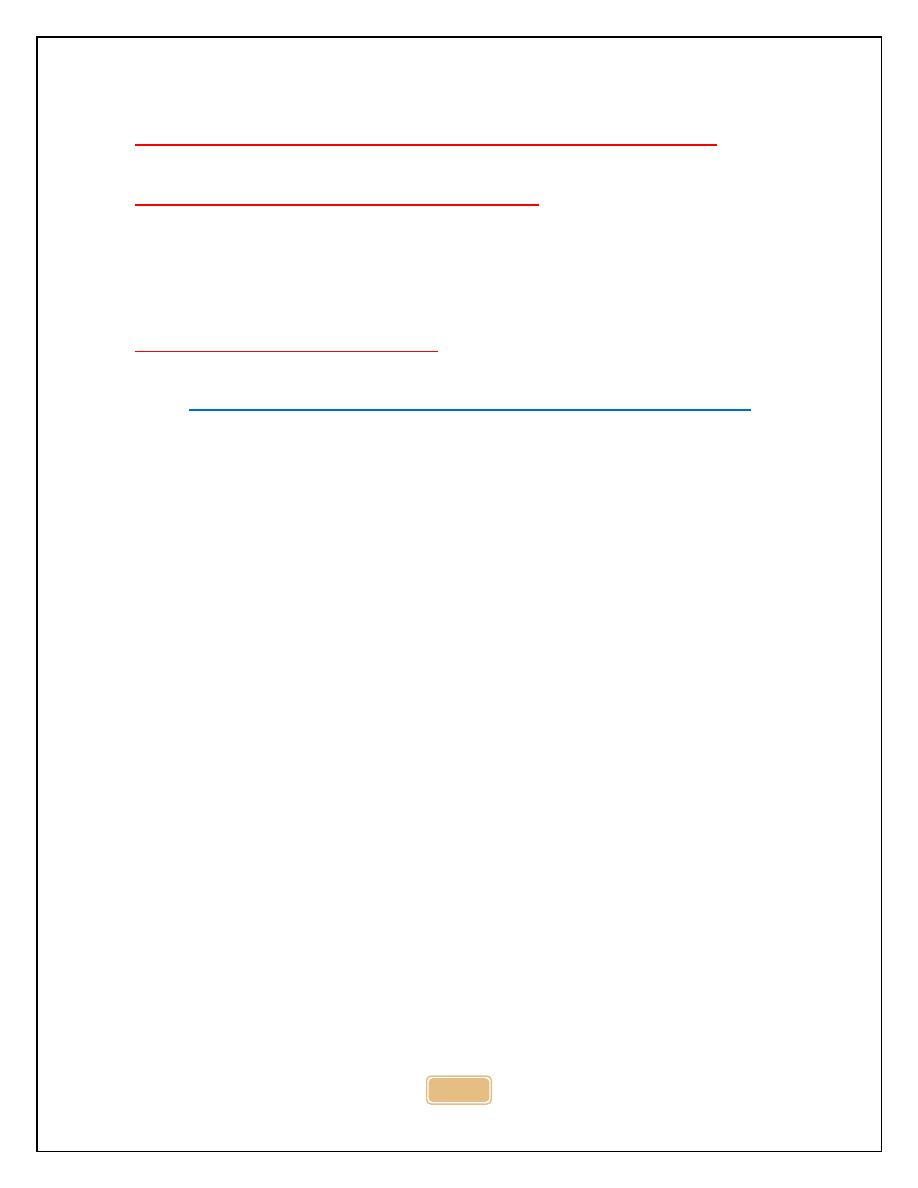
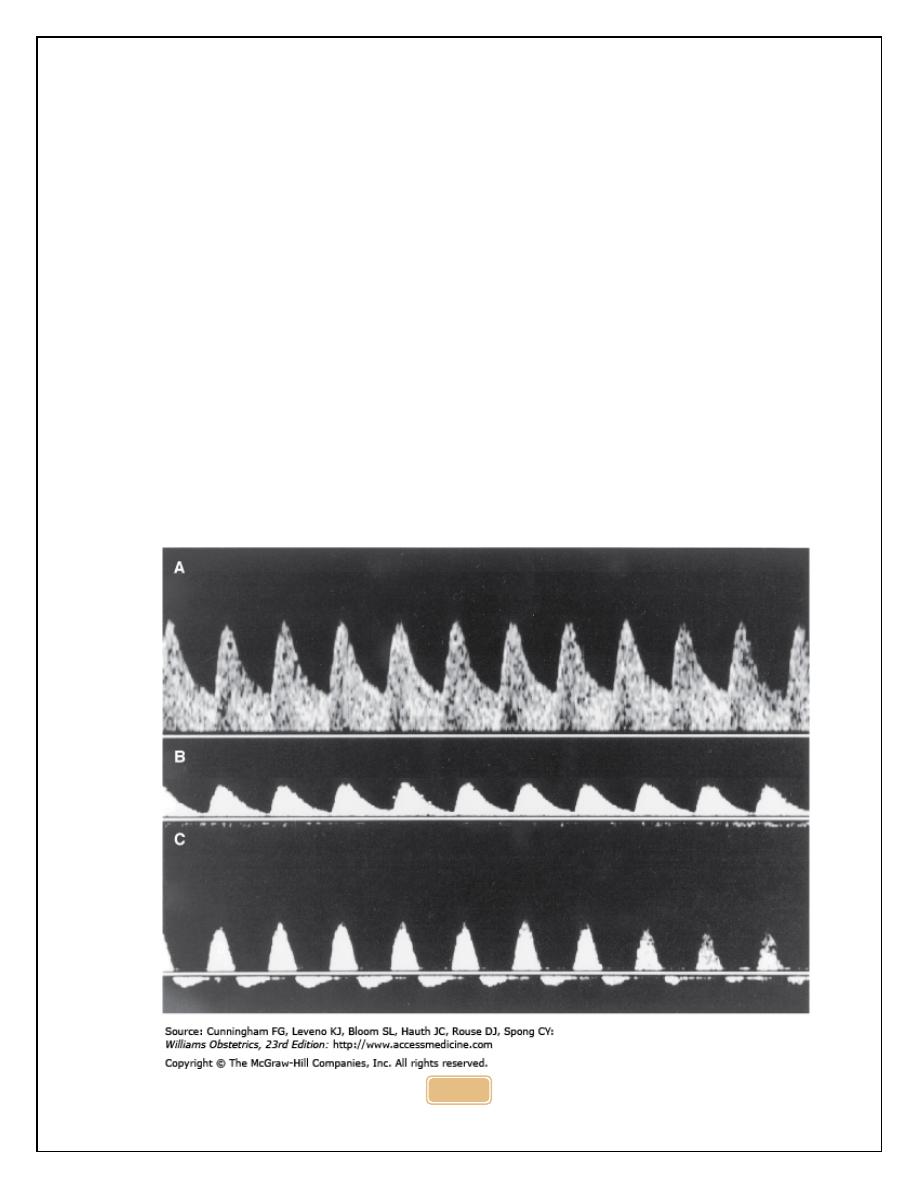
2. Nonstress Test (NST).
S The FHR is monitored with an external cardiotocometer. A
reactive NST is one that demonstrates at least 2 accelerations
of the FHR in 20 minutes, associated with fetal movement as
recorded by the mother . Each of the 2 accelerations must last
at least 15 seconds and reach a peak 15 beats above the
baseline level .
S A reactive NST is highly predictive of low risk for fetal mortality
in the subsequent 1 week. It may be normal to have a
nonreactive tracing as late as 32 weeks' gestation. After 32
weeks, a nonreactive tracing should prompt further evaluation .
S Normal baseline of fetal heart=110-160 bpm, above 160----fetal
tachycardia, less than 110----fetal bradycadia. baseline is
decreased as gestation is advance.
S Causes of fetal tachycardia: maternal or fetal infection, acute
fetal hypoxia, fetal anaemia, drug e,g B-agonist.
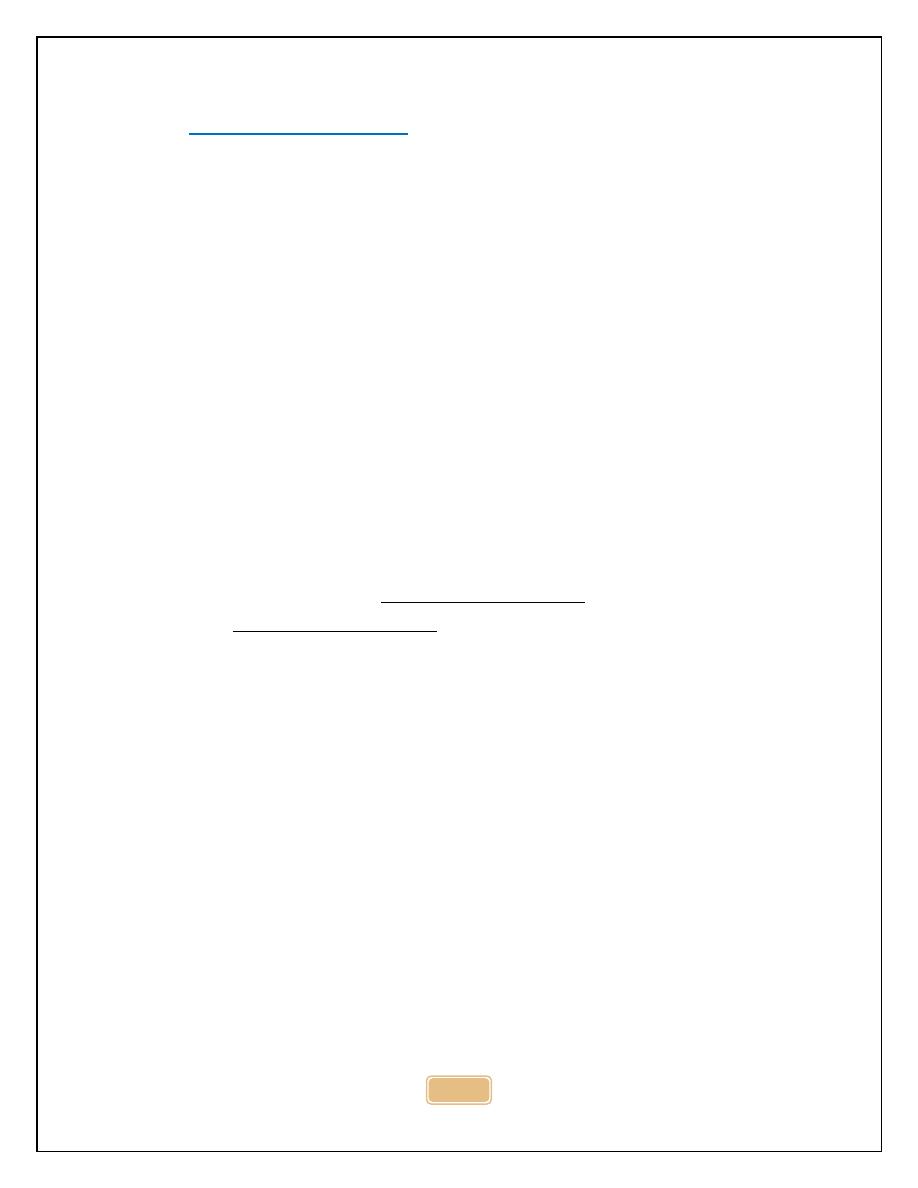
S Baseline variability: short term variability : beat-beat variability
and Long term variability : fluctuation in fetal heart rate occur
between 2-6 times per minute.
S Baseline variability below 5 is considered abnormal, baseline
variability affected by gestational age, fetal sleep, hypoxia, fetal
infection, drug suppressing CNS. Fetus display sleep cycles
every 20-30 min, base line var.may be reduced for this length of
time .
S Reduced baseline, absence of acc, presence of deceleration ---
--suspicious CTG, if no risk factor repeated investigation should
be performed, in presence of risk factors, suspicious CTG
warrant delivery.
3
4
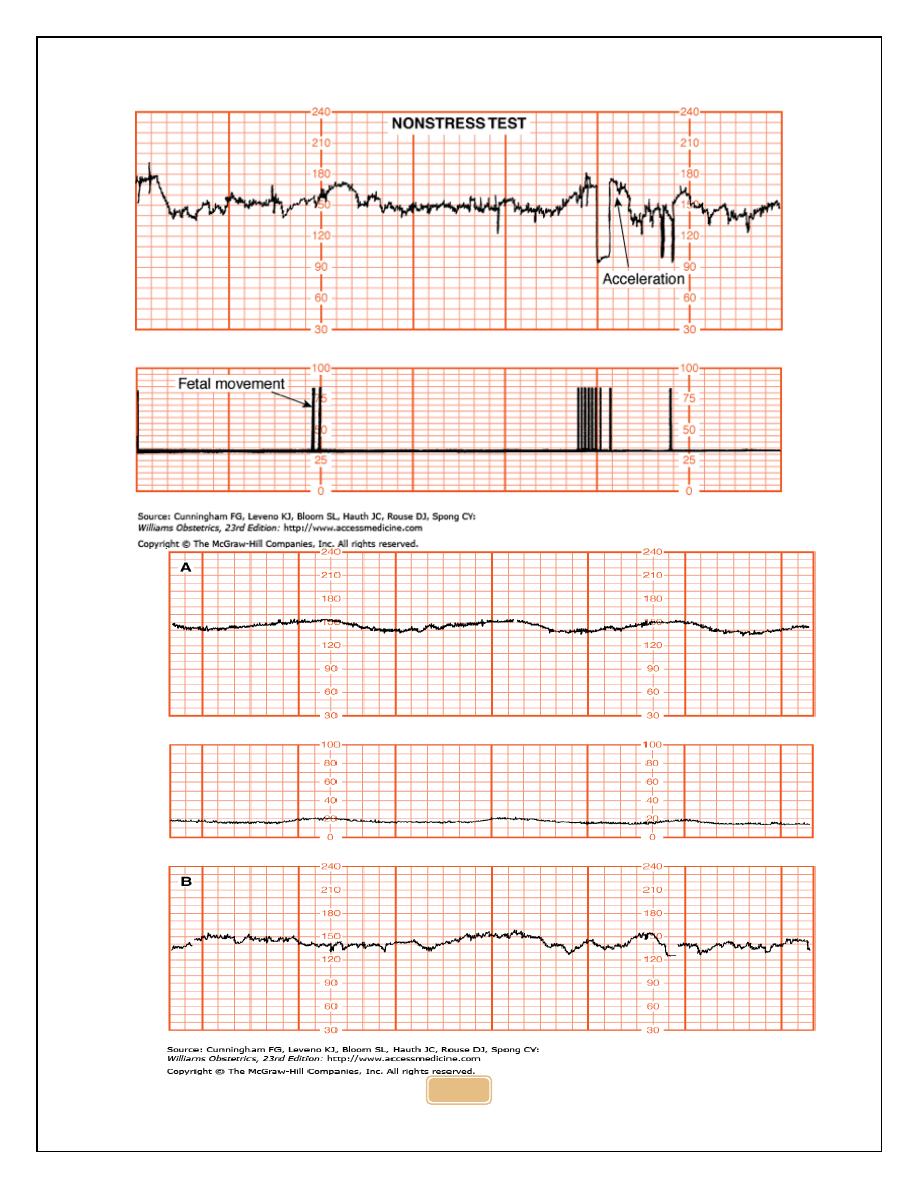
3. Biophysical Profile (BPP).
S The BPP has 5 components, each scored 0 or 2 for a maximum
score of 10. All of the sonographic criteria (not including the
NST) must be observed within a 30-minute period.
BPP score, interpretation & management
5
S 10---Normal, non-asphyxiated fetus: No fetal indication for
intervention; repeat test weekly except in diabetic patients and
post-term pregnancy (twice weekly)
S 8/10 (Normal AFV), 8/8 (NST not done)----Normal, non
asphyxiated fetus: no fetal indication for intervention; repeat
testing per protocol
S 8/10 (Decreased AFV)---Chronic fetal asphyxia: Deliver
S 6---Possible fetal asphyxia:
S If amnionic fluid volume abnormal, deliver
S If normal fluid at >36 weeks with favorable
S cervix, deliver
S if repeat test ≤ 6, deliver
S If repeat test >6, observe and repeat per protocol
S 4----Probable fetal asphyxia: Repeat testing same day; if
biophysical profile score ≤ 6, deliver
S 0 to 2---Almost certain fetal asphyxia----Deliver
4. Nonstress Test and Amniotic Fluid Index (AFI).
S This test is also known as the modified biophysical profile. The
AFI is the sum of the maximum vertical pockets of umbilical-
cord-free amniotic fluid in each of the four quadrants of the
uterus.
S A normal test has a reactive NST and an AFI greater than 5
(and less than 25). An abnormal test lacks one or both of these
findings.
5. Doppler ultrasonography
6
S a non-invasive method of assessing fetal vascular impedance.
Umbilical artery Doppler has been used to assess fetal well-
being, based on observations that growth-restricted fetuses
have different Doppler characteristics than normal fetus.
S In normal pregnancy blood flows through placenta without
difficulty ,while in diseased placenta blood will reflect back from
the placenta, in the former there is forward blood flow in
diastole, while in diseased placenta there will be absent or
reversed diastolic flow.
S Significant elevations in the S/D ratio have been associated
with IUGR, fetal hypoxia or acidosis, and higher rates of
perinatal morbidity and mortality. Absent and reversed end-
diastolic flows are the more extreme examples of abnormal S/D
ratio and may prompt delivery in some situations.
7
6. amniotic fluid volume:-
S reduction in AFV is called oligohydramnios, while excess is
called polyhydramnios , AFV can be assessed by US by 2
means : AFI & DVP.
S AFI can be measured by dividing the uterus into 4 quadrants ,a
vertical measurement is taken of deepest cord free pool in each
quadrant &results are summated, normal 5-25 cm, less than 10
indicate reduced liquor ,less than 5 indicate oligo. Values above
25 indicate poly. DVP, less than 2 cm indicate oligo, more than
8 cm indicates poly.
Factors Affecting NST Results
1- Sleep Cycles. Fetuses may have sleep cycles 20 to 80 minutes
in duration. During these periods, the tracing is likely to be
nonreactive. To rule out sleep cycle as a cause for a
nonreactive NST, prolonged monitoring is often required
(longer than 80 minutes at times).
8
2- Medications taken by the mother, e,g narcotics and sedatives,
steroids, and beta-blockers, will also reach the fetus,
resulting in decreased FH rate variability. Magnesium sulfate
can also have this effect in high doses.
3- Maternal smoking results in a transient decrease in fetal heart
rate variability.
4- Maternal hypoglycemia may reduce long-term fetal heart rate
variability as well as fetal movement.
5- Prematurity. The NST is not expected to be routinely reactive
before 32 weeks. If fetal surveillance is required at earlier
gestational ages, obtaining a biophysical profile may be
helpful.
Antenatal
S
S fetal
S
S imaging
S
S Ultrasound
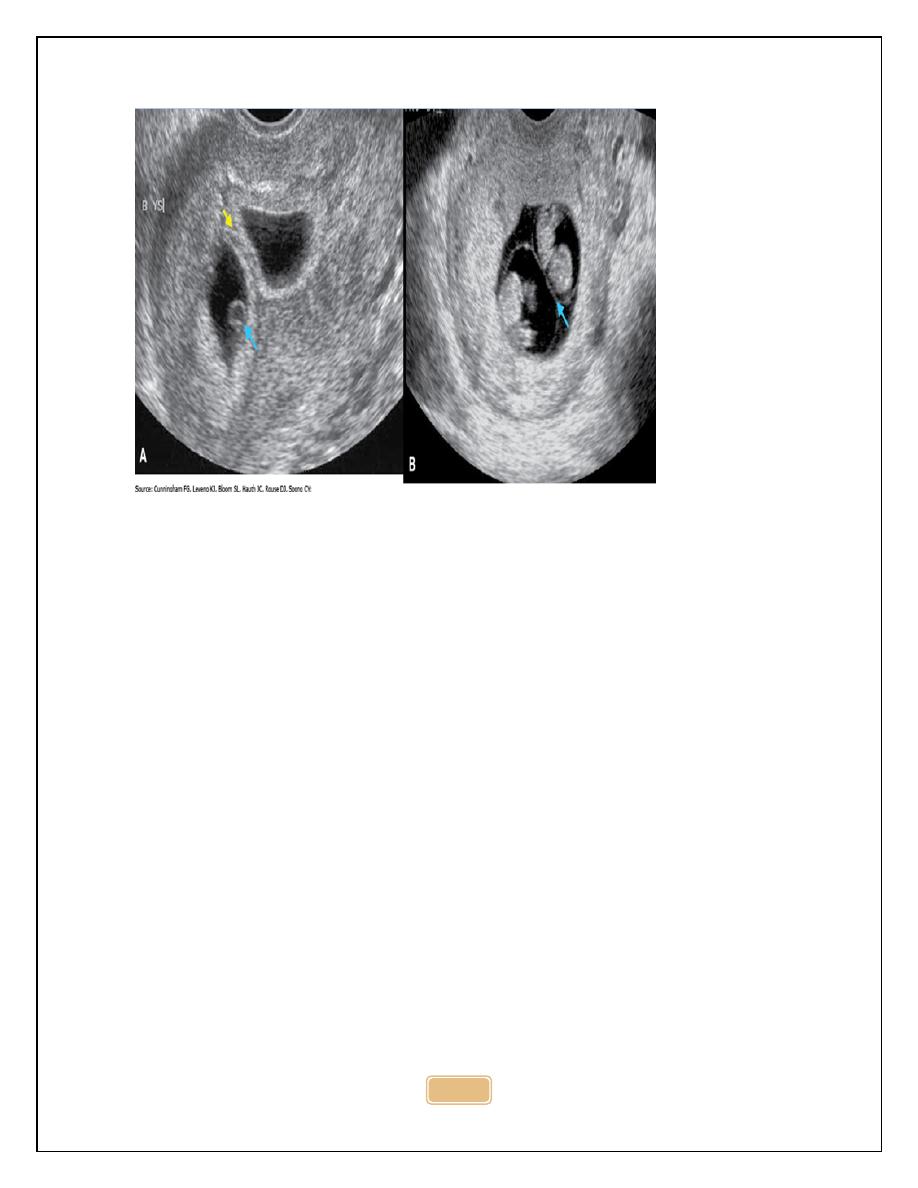
S To confirm fetal viability and to diagnose early pregnancy
problems :
S G .sac can be seen at 4-5 wk, yolk sac at 5 wk , embryo at 5-6
wk, FHR at 6wk.
S In blighted ovum: no fetus is present(empty G sac).
S In missed miscarriage: fetus can be identified but no FHR.
S In ectopic pregnancy: there will be +ve PT with absence of
intrauterine G sac, adnexal mass with or without fetal pole and
fluid in pouch of douglas.
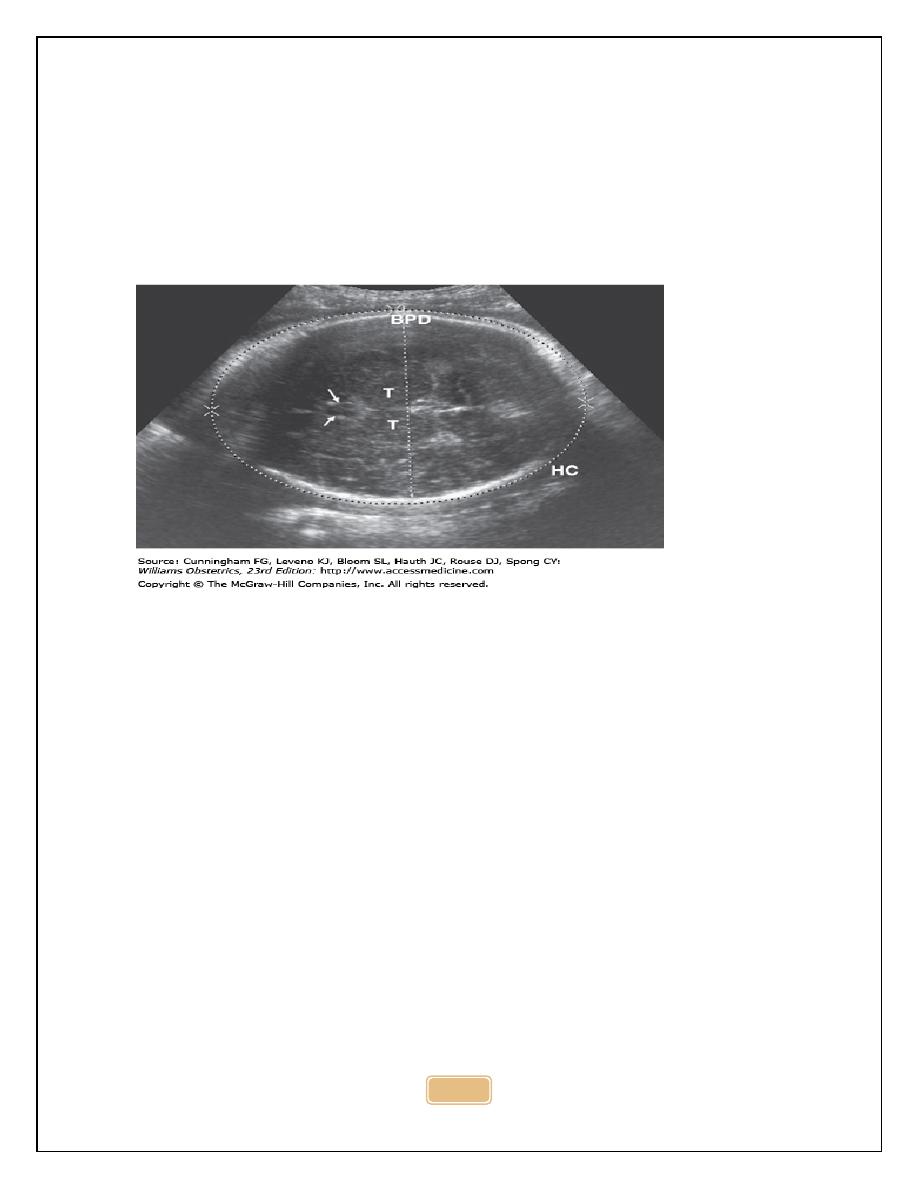
S Accurate estimation of gestational age:
S CRL can be used up to 13wk +6 days,
S HC from (14-20)wk,
S BPD &FL can also be used.
9
S CRL at 1
st
TMS (accurate -\+ 5days), while BPD at 20 wk (-\+7
days), this mean the earlier the measurement is made, the
more accurate the prediction.
S Assessment
of
fetal
size
and
growth:
by
abdominal
circumference (AC)&head circumference(HC) to assist in
diagnosis & management of pregnancy at risk of IUGR or
macrosomia.
S Asymmetry between HC&AC occur in FGR where brain sparing
effect will result in large HC compared to AC, the opposite will
occur in diabetic pregnancy , where the abdomen is large due
to effect of insulin on fetal liver and fat stores.
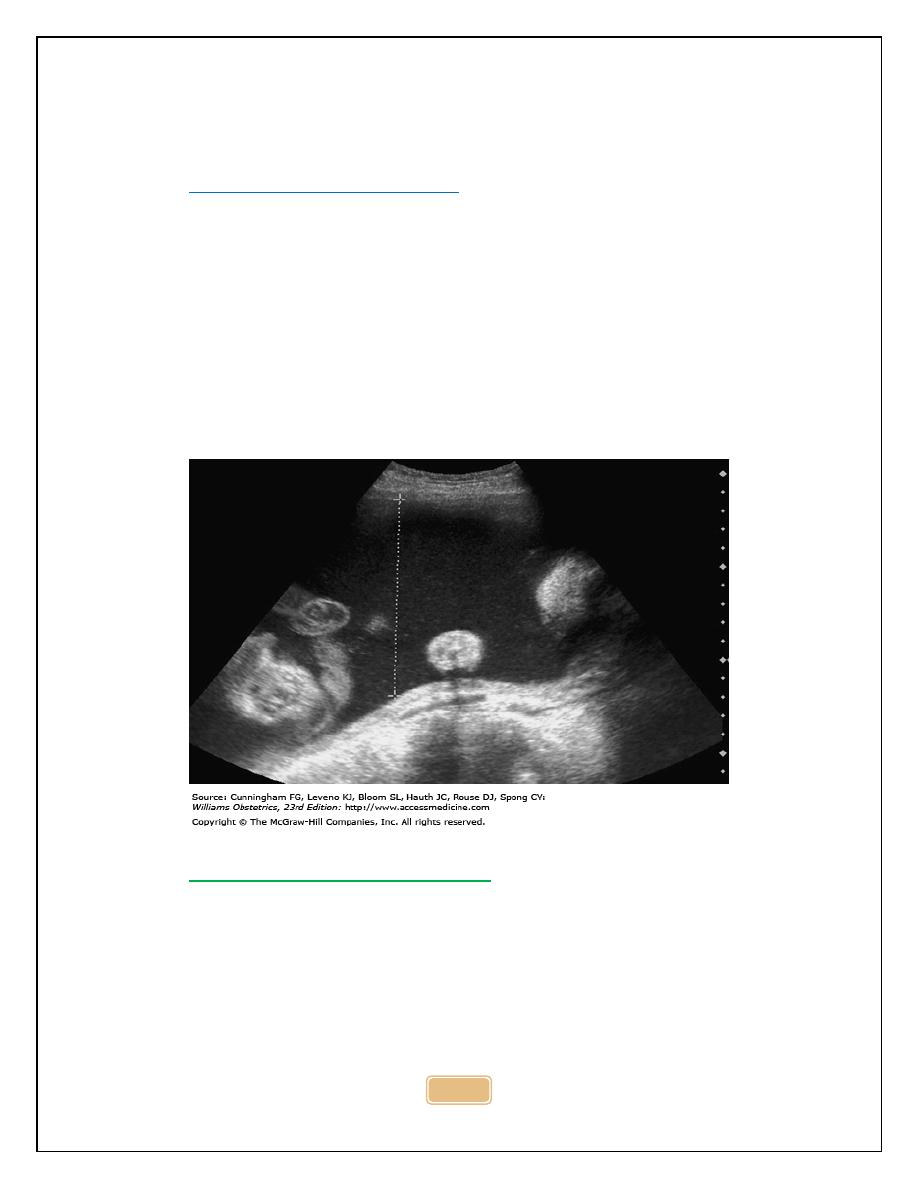
S To diagnose multiple pregnancy and to determine chorionicity:
ultrasound can detect the presence of more than one fetus. In
presence of
MP, it is necessary to determine chorionicity
because monochorionic twin are at higher risk of pregnancy
complication and higher perinatal motality compared to
dichorionic twin
S In MC twin the dividing membrane is formed by 2 layers of
amnion , while in DC by 2 layers of chorion & 2 layers of
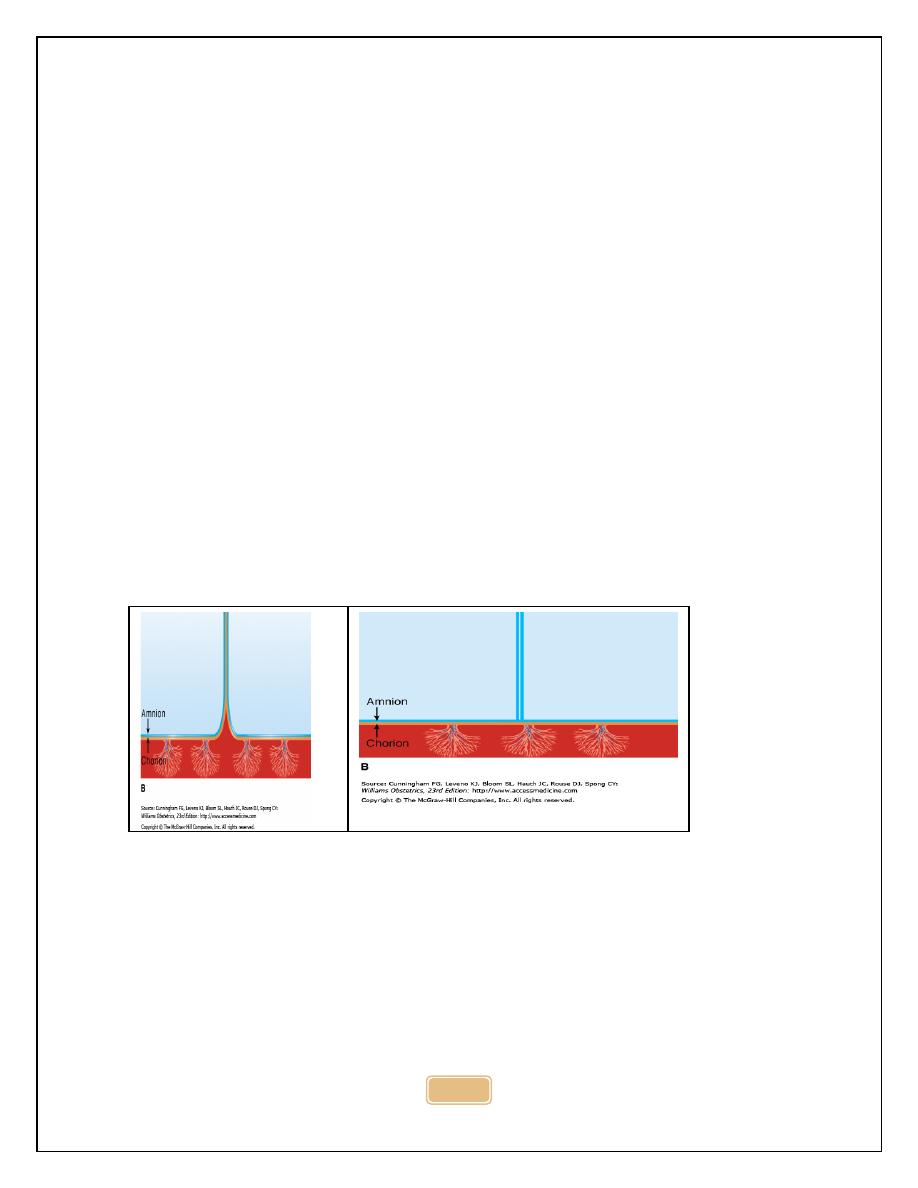
10
amnion. So DC twin have thick inter-twin membrane, in contrast
to MC twin there is a thin inter twin membrane. In ultrasound a
tongue of placental tissue within the base of DC membrane is
called twin peak or lambda sign.
S Determination of chorionicity is at 9-10 wk, later in pregnancy,
dichorionicity is confirmed by presence of 2 placental masses
and different sex foetuses.
S US in twin pregnancy is used also for:
1- Confirming fetal presentation because it may be difficult on
abdominal ex.
2- DX of growth restriction.
3- Fetal anomaly.
4- Placenta previa.
5- Twin –twin transfusion syndrome.
11
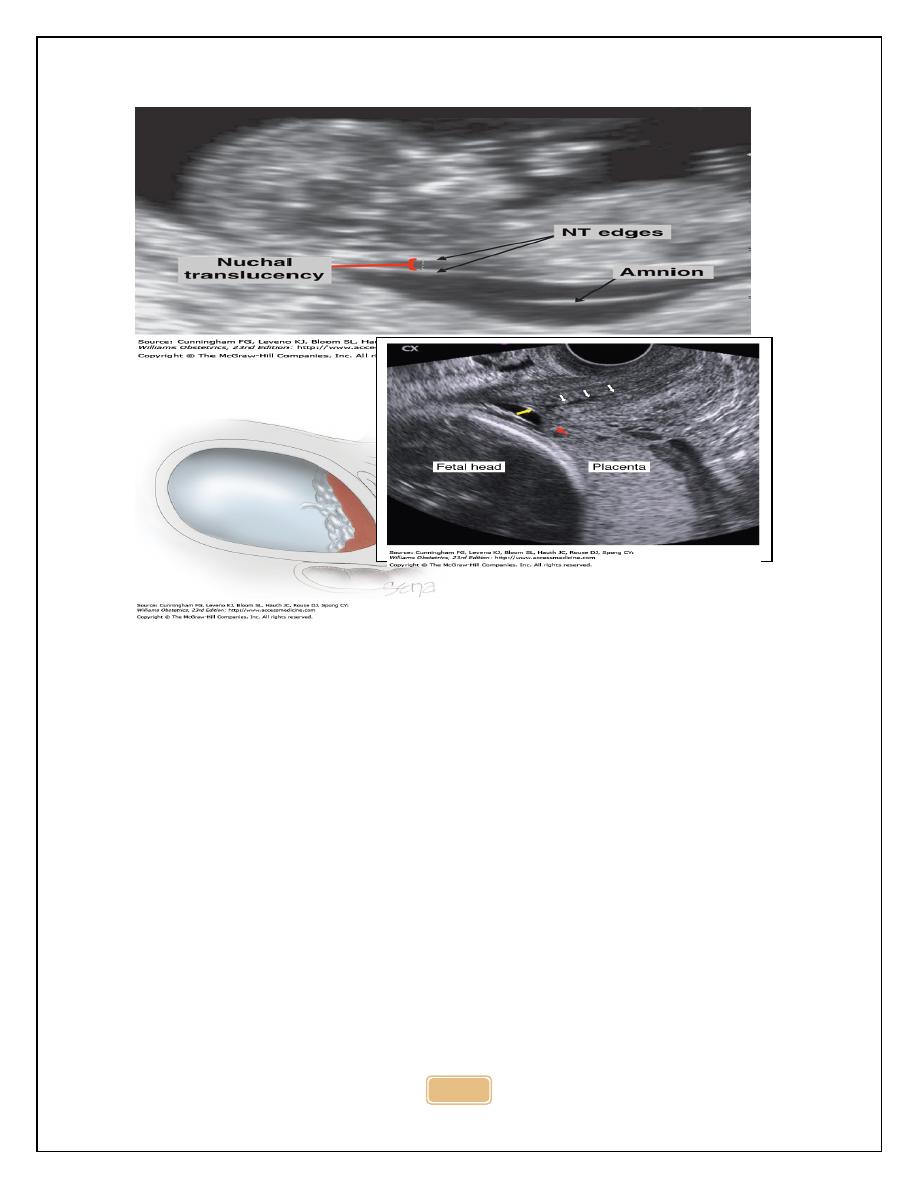
S To detect fetal anomaly: major structural abnormality occur in 2-
3 % of pregnancy, these anomalies may be detected by US at
around or before 20 wk. e.g spina bifida, congenital heart
disease, In addition soft markers can be identified by US such
as increased nuchal translucency(At 11-13 wk), absence of fetal
nasal bone, these are called soft markers and used for
detection of foetuses at risk of chromosomal abnormalities such
as down s syndrome.
S Placental localization : placenta previa (PP) is Implantaion of
placenta in lower uterine segment can cause life threatening
haemorrhage , ultrasound is used for placental localization by
identification of lower edge of placenta by TVS approach.
S The lower uterine segment is not yet formed and most low lying
placenta
will migrate upward as lower uterine segment
stretches in late 2
nd
and 3
rd
TMS.
S About 5% 0f pregnant women have a low lying placenta at 20
wk , only 5% will have PP
12
13
S Assessment of amniotic volume : by measuring DVP or AFI ,
the fetus swallows amniotic fluid , absorb it in gut and excrete
urine into amniotic sac . Congenital abnormalities that impair
ability of fetus to swallow e.g anencephaly or esophageal
atresia result in polyhydramnios. Congenital anomaly that result
in failure of urine production or passage e.g renal agenesis or
posterior urethral valve
will result in oligohydramnios or
anhydramnios, similarly IUGR is associated with oligo. due to
reduced renal perfusion and reduced urine production.
Assessment of fetal wellbeing : BPP & Doppler
S Measurement of cervical length: cervical length can be
assessed by TVS or TAS, trans-vaginal route is preferable
because trans-abdominal sonography require full urinary
bladder which cause false lengthening of cervix.
S In 1
st
TMS cervical length less than 26 is considered to be short,
while in 2
nd
TMS we should search for presence of funnelling
Uses of ultrasound in 1
st
TMS
1- To confirm fetal viability.
2- To provide accurate estimation of gestational age.
3- To diagnose multiple gestation & to determine chorionicity.
4- To detect markers that indicate risk of chromosomal
abnormality such as Down s syndrome.
5- To identify gross structural abnormalities.
14
Aims of ultrasound at 18-22wk
1- To provide accurate estimation of gestational age if early scan
has not been performed.
2- To perform a detailed anatomical survey, to detect any
structural abnormalities
or
markers for
chromosomal
abnormalities.
3- To locate placenta, identify women with low lying placenta for
repeat scan at 34 wk to exclude placenta previa.
4- To assess amniotic fluid volume
5- To screen for adverse pregnancy outcome e,g preeclampsia or
IUGR using Doppler ultrasound of uterine artery.
6- To measure cervical length and to assess risk of preterm labour.
Ultrasound in 3
rd
TMS:
1- To assess fetal growth.
2- To assess fetal wellbeing.
