DR.EMAN
ANTEPARTUM HAEMORRHAGE
Antepartum haemorrhage:-
Bleeding that occur after 24th week of gestation but prior to onset of labour.
Incidence: - 5%
!
Causes
Placenta previa(PP)
Placental abruption(PA)
Vasa previa
Cervicitis
Trauma
Vulvovaginal varicosities
Genital tumour
Genital infection
50% due to PP & PA
!
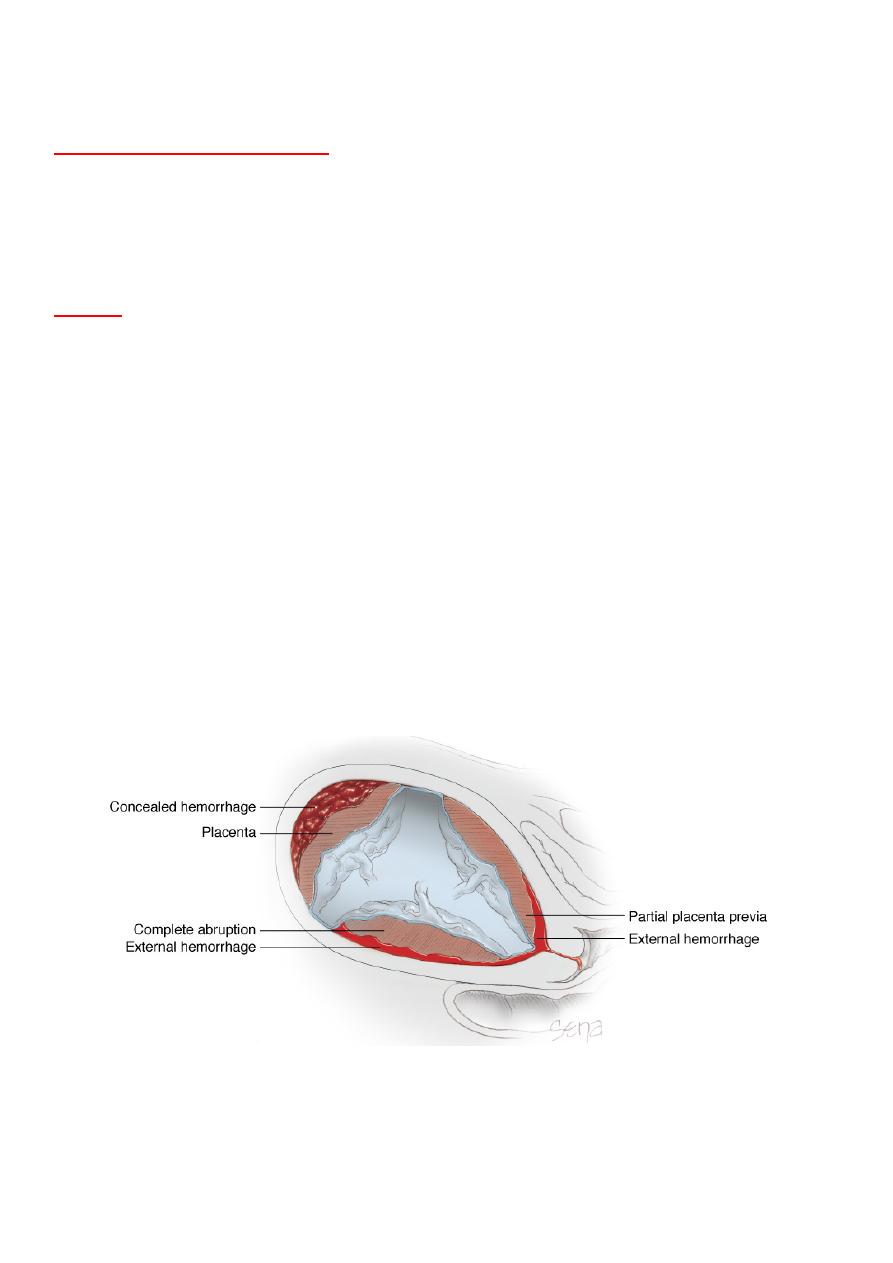
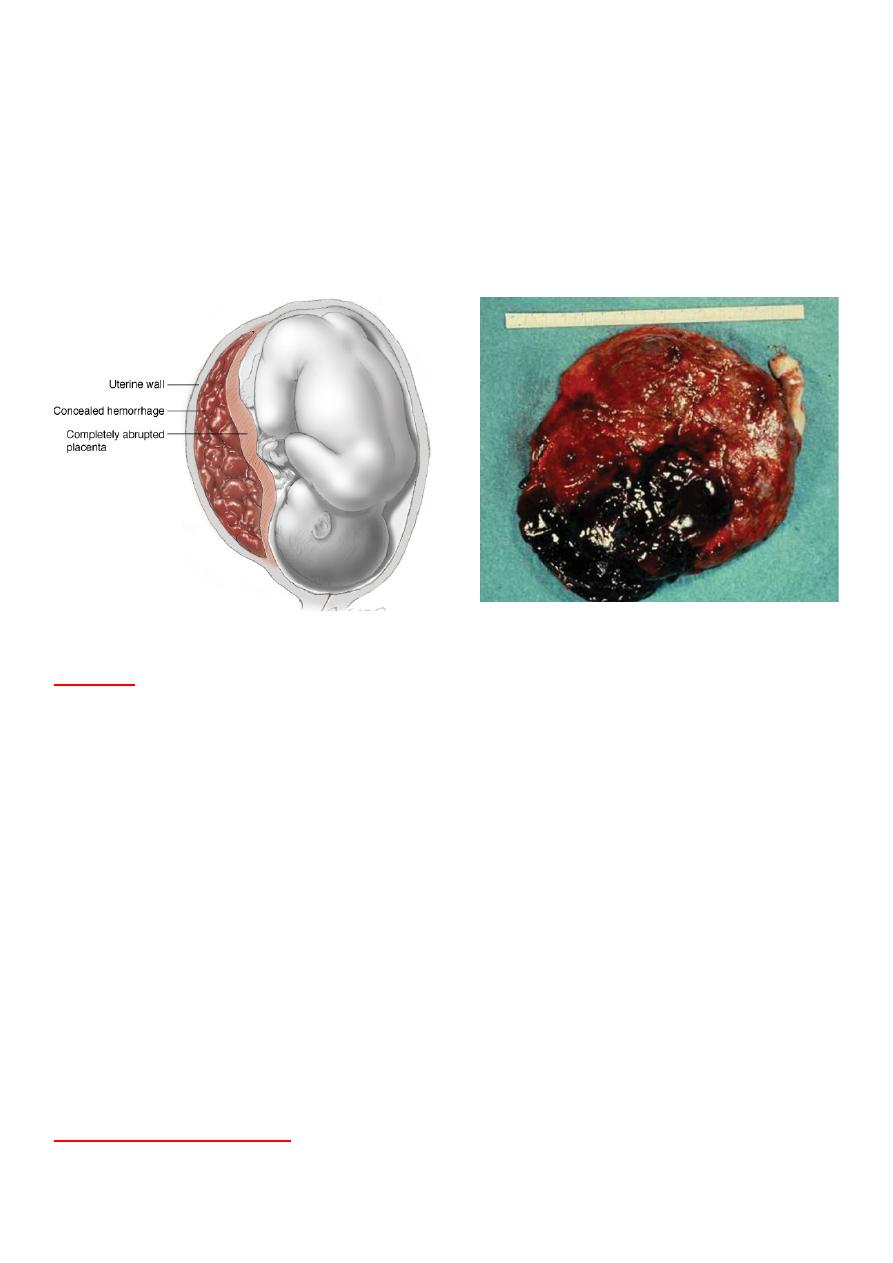
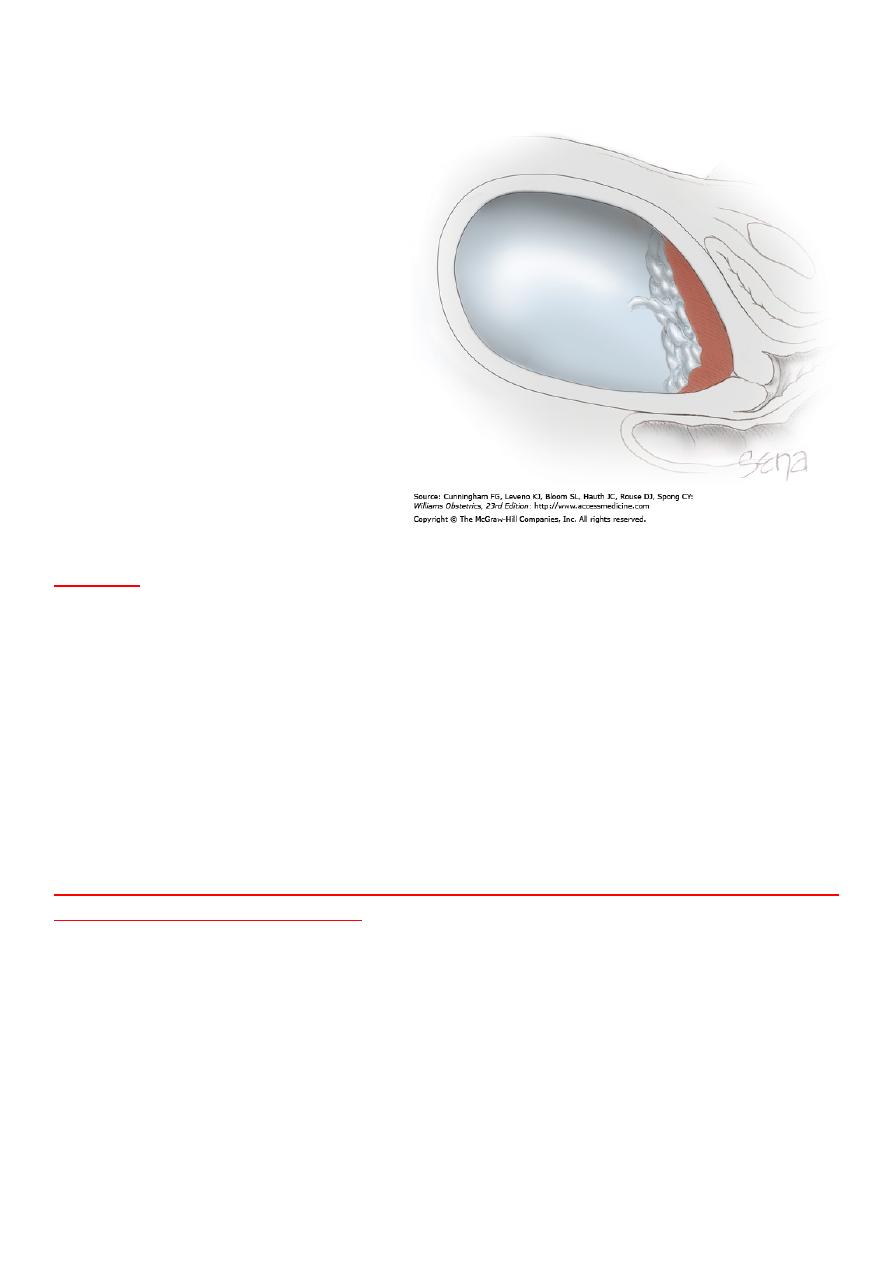
Abruptio placentae (AP):-
Is the premature separation of the normally
implanted placenta from the uterine wall due to uterine vessel hemorrhage
into the decidua basalis.
-Incidence :-
1.5%.
-It is of 2 types:-
Revealed:-
with external bleeding.
Concealed:-
occurs when the placental margins remain adherent, retaining
blood between the placenta and the uterus.
!
Etiology
•
Idiopathic
•
Inherited thrombophilias.
•
Maternal hypertension
•
Advanced maternal age
•
Multiparity
•
Smoking
•
Trauma.
•
Rapid contraction of an over distended uterus may lead to abruption, such
as with rupture of membranes with polyhydramnios, or delivery of an
infant in a multiple gestation.
!
Maternal Complications
•
Hemorrhagic shock leading to ischemic necrosis of distant organs.
•
Disseminated intravascular coagulation(D IC)
•
Couvelaire's uterus (extra vasation of
blood into uterine muscle) leading to
uterine atony; rarely, Couvelaire's uterus
may lead to uterine atony and massive
haemorrhage, which necessitates
aggressive measures, such as caesarean
hysterectomy to control the bleeding.
!
Fetal complications include:-
hypoxia leading to growth
restriction, anemia, prematurity, fetal
distress, hypoxic-ischemic
encephalopathy, and death.
!
Diagnosis
History and Physical Examination
AP presents with vaginal bleeding and acute onset of constant abdominal
pain(The presence of blood in the basalis stimulates uterine contractions,
which results in abdominal pain). Maternal vital signs, fetal heart pattern,
and uterine tone should be monitored. Fundal height can also be followed to
look for concealed hemorrhage.
!
Pelvic Examination:
If placenta previa is ruled out, perform a speculum
examination to look for vaginal or cervical lacerations and evaluate vaginal
bleeding.
Ultrasonography:
Although ultrasonography is relatively insensitive in
diagnosing AP, a hypoechoic area between the uterine wall and placenta may
be seen with large abruptions.
!
Management.
•
establishment of intravenous access with two large-bore catheters.
•
fluid resuscitation.
•
blood type and cross-match determination.
•
continuous foetal monitoring.
•
Rho (D) immunoglobulin should be administered to Rh-negative individuals.
•
maternal vital signs should be assessed frequently.
!
Term Gestation, Maternal and Fetal Hemodynamic Stability
✇
One should plan for vaginal delivery with cesarean section reserved for the
usual obstetric indications.
✇
If the patient does not present in labor, induction of labor should be
initiated.
✇
Serial hematocrits, coagulation evaluation, fetal scalp electrode.
!
Term Gestation, Maternal and Fetal Hemodynamic Instability
✇
Aggressive fluid resuscitation should be performed as well as transfusion of
packed red blood cells, fresh frozen plasma, and platelets as appropriate.
✇
Once maternal stabilization is achieved, caesarean section should be
performed, unless vaginal delivery is imminent.
!
Preterm Gestation, Maternal and Fetal Hemodynamic Stability.
•
Preterm, Absence of Labor. These patients should be followed closely with
serial ultrasonographic examination for fetal growth starting at 24 weeks'
gestation and antepartum fetal testing. Steroids should be administered to
promote fetal lung maturity.
•
Preterm, Presence of Labor:- If both maternal and fetal hemodynamic
stability are established, tocolysis may be used in selective mild cases.
!
Preterm Gestation, Maternal and Fetal Hemodynamic Instability.
Delivery should be performed after appropriate resuscitation.
!
Placenta previa (PP)
Is defined as the presence of placental tissue over or
near the internal cervical os. PP can be classified into four types based on
the location of the placenta relative to the cervical os:
Complete or total previa,
in
which the placenta covers the
entire cervical os.
Partial previa,
in which the
margin of the placenta covers
partially cover internal os
marginal previa
, in which the
edge of the placenta lies
adjacent to the internal os;
Low-lying placenta,
in which the
placenta is located near (2 to 3
cm) to the internal os.
Incidence: - 0.5%
!
Etiology.
•
Endometrial scarring
•
Advancing maternal age
•
Multiparity
•
Multiple pregnancy.
Placenta previa is associated with a doubling of the rate of congenital
malformations.Previa is also associated with fetal malpresentation.
!
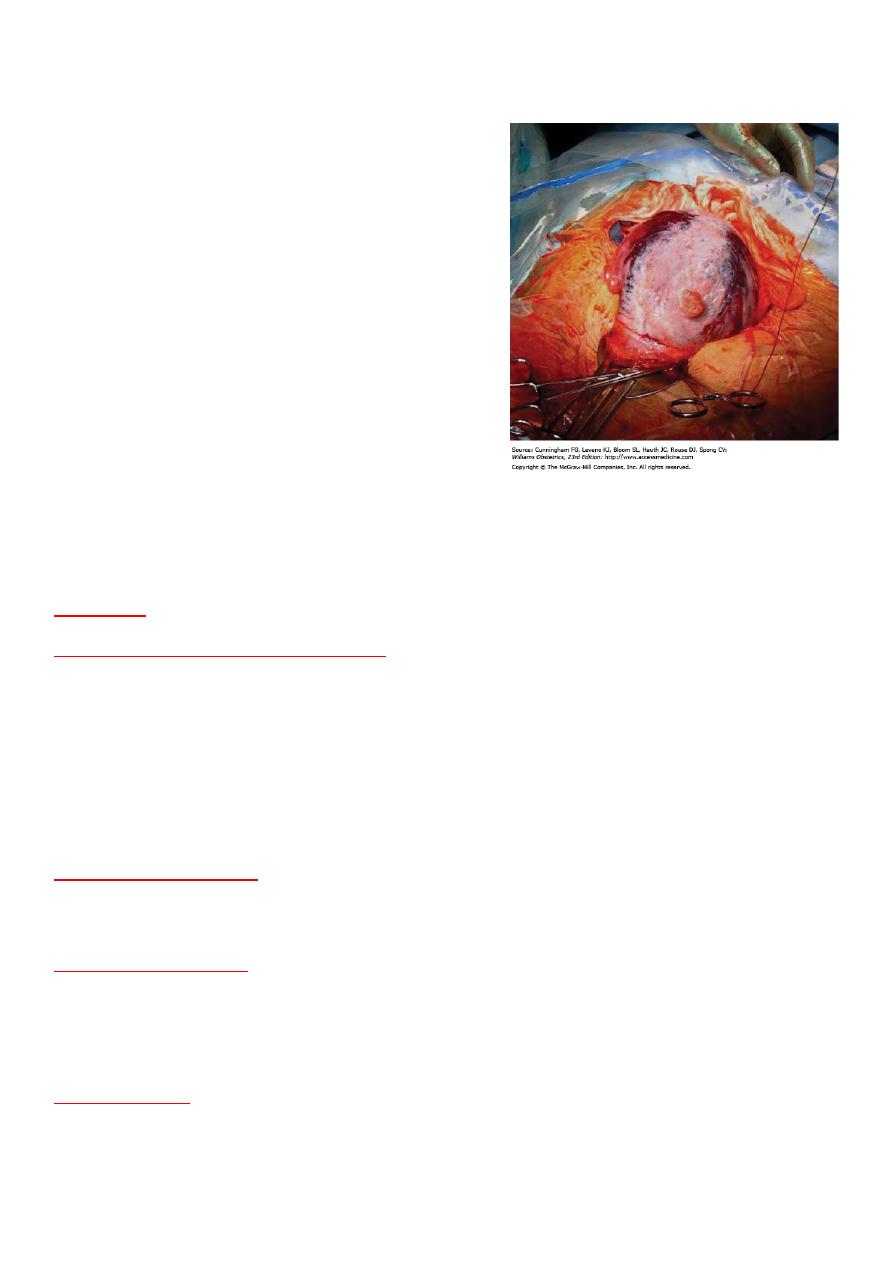
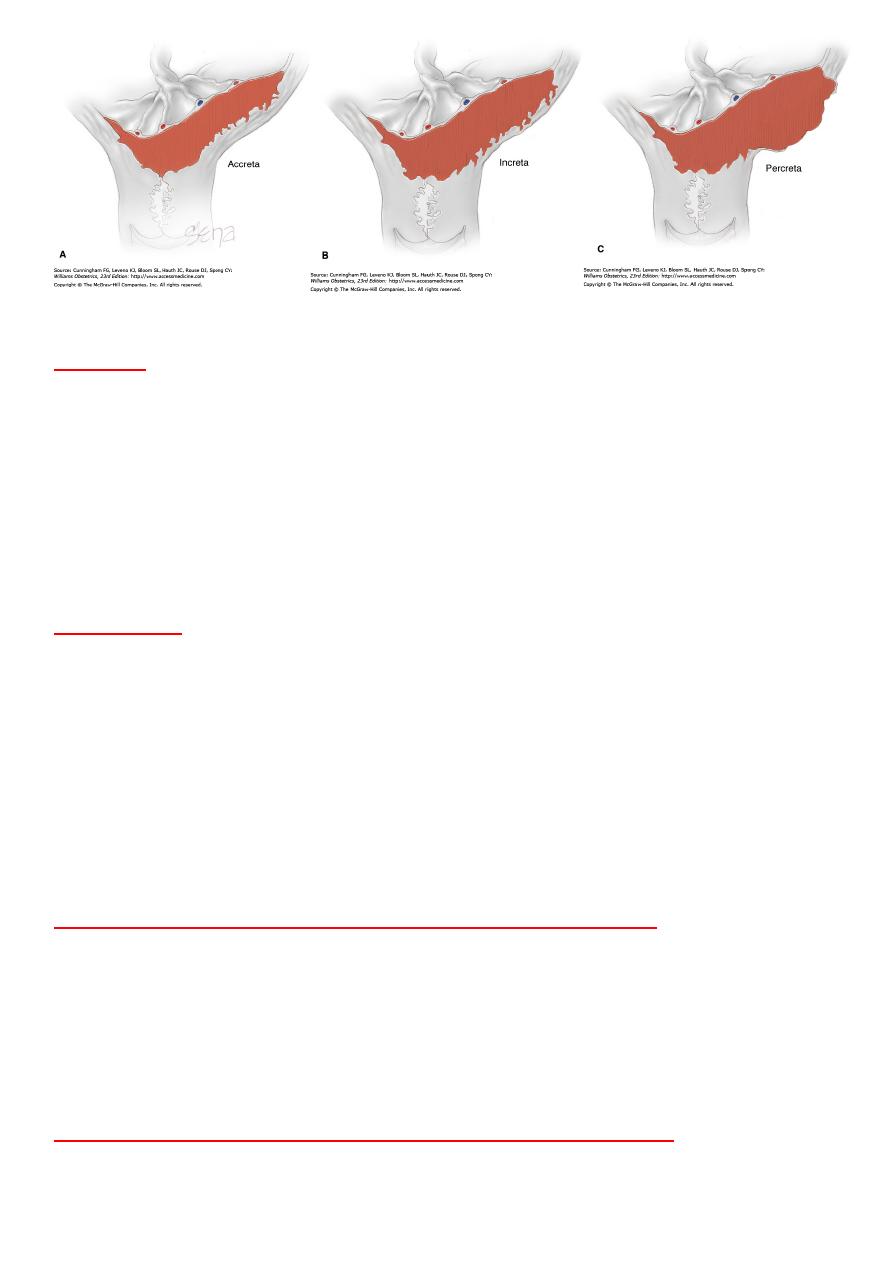
Abnormal growth of the placenta into the uterus can result in one of the
following three complications:
Placenta Previa Accreta.
placenta adheres to the uterine wall without the
usual intervening decidua basalis.
Placenta Previa Increta.
placenta invades the myometrium.
Placenta Previa Percreta.
placenta penetrates the entire uterine wall, into
bladder or bowel.
!
!
!
Diagnosis
History
. PP presents with acute onset of painless vaginal bleeding.
Examination.
If PP is present, digital examination iscontraindicated, a
speculum examination can be used to evaluate the presence and quantity of
vaginal bleeding, maternal vital signs, abdominal exam, uterine tone, and
fetal heart rate monitoring should be evaluated. Vaginal sonography is the
gold standard for diagnosis of previa.
!
Management
•
Standard Management of symptomatic patients with PP includes initial
hospitalization with hemodynamic stabilization.
•
continuous maternal and fetal monitoring.
•
Steroids should be given to promote lung maturity for gestations between
24 and 34 weeks.
•
Rho (D) immunoglobulin should be administered to Rh-negative mothers.
!
Term Gestation, Maternal and Fetal Hemodynamic Stability.
Complete Previa. Patients with complete previa at term require caesarean
section.
Partial, Marginal Previa. These patients may deliver vaginally; however, a
double setup in the operating room is recommended.
!
Term Gestation, Maternal and Fetal Hemodynamic Instability.
Delivery is indicated with evidence of non reassuring fetal heart rate tracing,
life-threatening maternal haemorrhage, Delivery should then occur via
caesarean section.
!
Preterm Gestation, Maternal and Fetal Hemodynamic Stability
Labor Absent. Patients at 24 to 37 weeks' gestation with PP who are
hemodynamically stable can be managed expectantly until fetal lung
maturity has occurred. Current recommendations for each episode of
bleeding include
•
Hospitalization until stabilized
•
Bed rest
•
Blood transfusions to keep pcv above 30%
•
Fetal testing with serial ultrasounds
•
Tocolysis is usually not warranted unless used for the administration of
antenatal steroids .
•
After initial hospital, care as an outpatient may be considered if the
bleeding has stopped for more than 1 week, and the following criteria are
met:
•
The patient can maintain bed rest at home.
•
The patient has a responsible adult present at all times who can assist in
an emergency situation.
•
The patient lives near the hospital with available transportation to the
hospital.
•
Once a patient has been hospitalized for three separate episodes of
bleeding, she remains in the hospital until delivery. Labor Present. If the
patient and fetus are stable, tocolysis may be considered
!
Preterm Gestation, Maternal and Fetal Hemodynamic Instability.
Maternal stabilization with resuscitative measures. Once stable, the patient
should be delivered by cesarean section.
!
!
!

Placenta previa
• Painless
• Less distress
• Soft abdomen
• abnormal lie & presentation
• CTG usually normal
• No pre eclampsia
• No coagulation defect
• Most dangerous for mother
!
!
Vasa previa (VP)
Vasa previa (VP) can occur when the umbilical cord inserts into the
membrane of the placenta instead of the central region of the placenta.
When one of these vessels is located near the internal os, it is at risk of
rupturing and causing fetal hemorrhage.
Incidence :- 0.03%
!
Clinical Manifestations.
Although VP is a rare cause of bleeding, patient usually presents with an
acute onset of vaginal bleeding in the setting of ruptured membranes.The
bleeding is associated with an acute change in fetal heart pattern;
emergency caesarean section is indicated. If VP is diagnosed antenatally,
elective caesarean section should be scheduled at 36 to 38 weeks.
!
!
BY: Hazha F.Rasheed
Edited By Mohammed Musa
Placental abruption
• Painful
• More distress
• Tense tender abdomen
• Normal lie & presentation
• CTG abnormal
• Ass with preeclampsia
• Coagulation defect
• More dangerous for fetus.
