Obstetrics Dr. Esraa
1
Diabetes Mellitus
DM in pregnancy:
Either :
• Pre-existing IDDM or NIDDM.
• Transient impaired glucose intolerance during pregnancy.
CHO metabolism in pregnancy
During pregnancy there is significant change in CHO metabolism due to
• hormonal changes, these hormones are produced by placenta which
include oestrogen, progesterone, human placental lactogen,&cortisole (all
antagonise action of insulin).
• increased metabolic demand of gravid uterus, its content & mother.
• Placenta breaks down insulin.
As a result of this diabetogenichormones , insulin production is increased
progressively from 2
nd
trimester through term
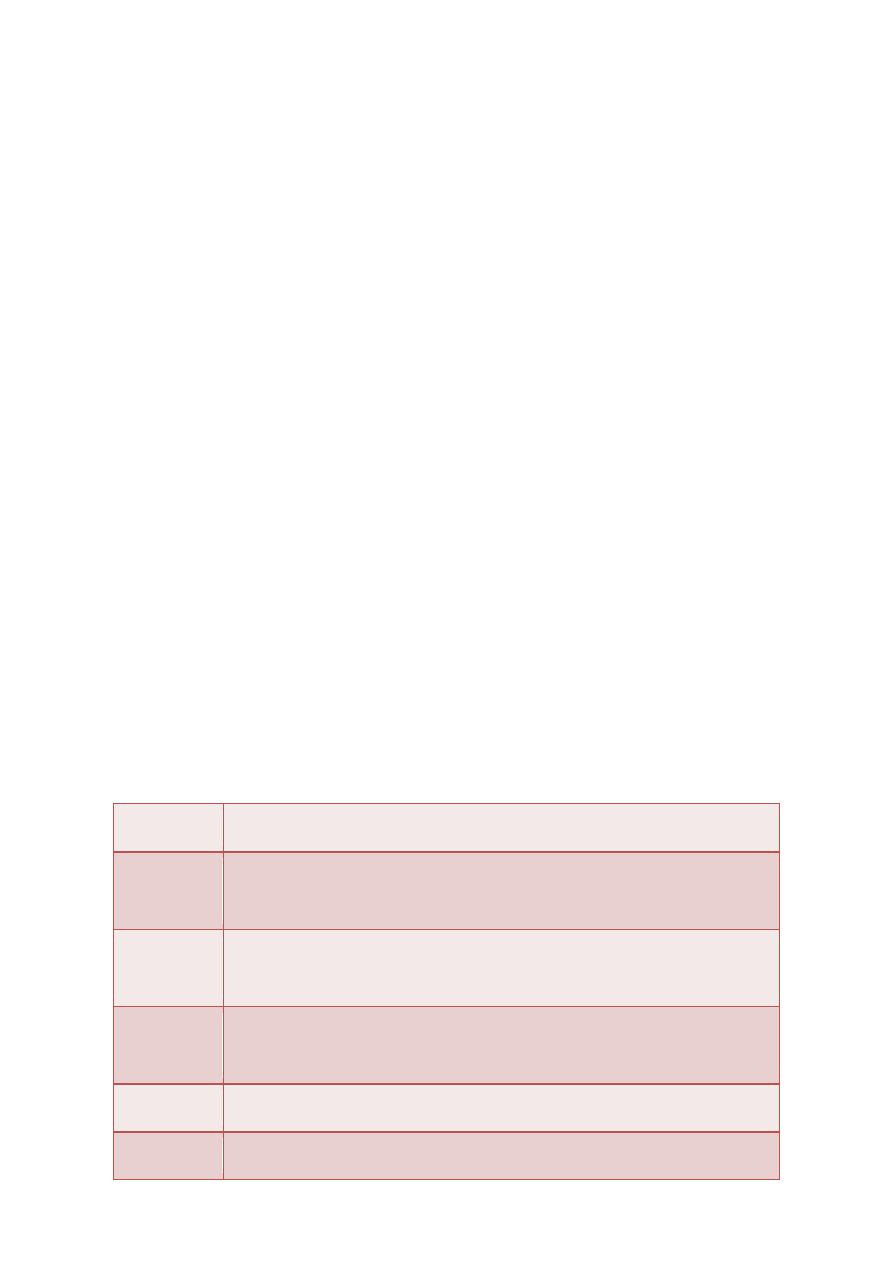
White s classification of DM
A
Asymptomatic but abnormal GTT
B
Onset age ≥ 20 yr, duration ˂ 10 yr , no vascular
complication
C
Onset age10-19 yr, duration 10-19 yr, no vascular
complication.
D
Onset age ˂ 10 yr, duration≥20 yr, vascular
complication or benign retinopathy
E
nephropathy
F
Proliferative retinopathy
Obstetrics Dr. Esraa
2
Effect of pregnancy on diabetes:
Change in eating pattern.
Increase in insulin dose requirement.
Greater importance of tight glycemic control.
Increase risk of sever hypoglycemia.
Risk of deterioration of pre-existing retinopathy.
Risk of deterioration of established nephropathy.
Effect of diabetes on pregnancy:
Increased risk of miscarriage.
Risk of congenital malformation.
Risk of macrosomia.
Increased risk of pre-eclampsia.
Increased risk of stillbirth.
Increased risk of infection.
Increased operative delivery.
Maternal &fetal complication
Fetal complications:
• Congenital abnormalities: cardiac & NTD
• Miscarriage
• Polyhydramnios
• Preterm delivery
• Respiratory distress syndrome.
• Unexplained IUD.
• Neonatal : jaundice, polycythemia, tetany, hypocalcaemia,
hypomagnesaemia, hypoglycemia.
Maternal complication:
• Retinopathy
• Nephropathy
• Cardiac disease
• PIH or PE
• Recurrent vulvo-vaginal infection
• Increased risk of operative delivery
• Obstructed labour.
Obstetrics Dr. Esraa
3
Polyhydramnios : due to fetal polyuria & osmotic diuresis
Macrosomia: due to unsatisfactory metabolic environment
Preterm labour :due to iatrogenic delivery
Still birth after 36 wk :
chronic intra utrine hypoxia (due to vasculopathy that cause decreased in
uterine blood flow or Hyperinsulinaemia)
Flucuation in random blood sugar
Infection
Hyperglycemia
Pre - gestational diabetes
Management
1. pre-pregnancy:
• Patient information leaflets about risk of pregnancy in diabetic women.
• High dose folic acid 5 mg preconception & 1
st
12 wk of pregnancy because
pericoceptionalhyperglycemia has teratogenic effect on fetus.
• HbA1C should be less than 6.5 % before conception. Level of HbA1C in
early pregnancy correlate with risk of fetal loss & congenital malformation.
• Tight glycemic control before pregnancy& adequate contraception used
until glucose control is good .
• Screening for retinopathy & nephropathy: chance of successful pregnancy
is reduced as serum creatinine increase, the higher pre-pregnancy
creatinine concentration , the higher the risk of permanent loss of renal
function.
2. pregnancy:
A- Glucose control: most pt with pre-pregnancy DM are taking insulin & this
therapy should be maintained in pregnancy, while pt taking OHD before
pregnancy should change to insulin, because OHD cross placenta & may have
teratogenic effect, also associated with difficult glycemic control & neonatal
hypoglycemia

Obstetrics Dr. Esraa
4
Insulin dose =
1
st
trimester→ body wt X 0.6.
2
nd
trimester→ body wt x 0.7.
3
rd
trimester → body wt X 0.8.
Dosage schedule: ⅔ in AM and ⅓ in PM
Before breakfast ⅔ intermediate acting & ⅓ soluble
Before dinner 1\2 intermediate& 1\2 soluble or regular.
Or short acting insulin before each meal & intermediate acting before bedtime
Regular glucose measurement: fasting, 2hr postprandial
(breakfast, lunch, dinner)
The aim is :FPG 3.5-5.5 mmol\l
RBG 4-6.5 mmol\l
HbA1c ˂ 7%
In women presented with PTL , steroid should be given but it may induce
hyperglycemia, increase dose by 40% at time of 1
st
dose & until 24 hr after 2
nd
dose.
B – fetal surveillance:
• Early dating us .
• Detailed anomaly scan
• Fetal echocardiography
• Serum screening for congenital anomaly(Maternal serum alpha feto
protein DM& maternal wt affect the level)
• Us soft markers for chromosomal abnormalities such as nuchal translucency
• Any concern of fetal wellbeing should lead to increase fetal surveillance
by doppler us or CTG
C – maternal surveillance:
• monitoring of BP.
• frequent measurement of renal function test.
• Regular ophthalmic examination.
• Neurological examination.
Obstetrics Dr. Esraa
5
3. Labour & delivery:
• Timing of delivery: 38-39 wk .
• Mode of delivery: vaginal delivery is preferable but because of
macrosomia , failed induction of labour, maternal complication such as PE
& fear of shoulder dystocia, the rate of cs is high (50%).
EFW˃4500 g-------- elective cs
EFW 4000-4500 g, additional factors should be taken into consideration such
as past obstetrical history
• During labour:
insulin infusion should given via infusion pump & consist of 50 units short
acting insulin in 49.5 ml normal saline.
Start 500ml of 10% dextrose & 20 mmol of potassium chloride.
Perform ARM when possible & start oxytocin if indicated , this should be
given in 5% dextrose & via infusion pump.
measure capillary glucose every 1 hr in 1
st
stage ,every 15 min in 2
nd
stage
of labour , maternal blood glucose maintained at 4-7 mmol\L. If blood
glucose ˂4mmol\l stop infusion but continue 10 % dextrose & repeat
blood glucose after 15 min , restart insulin infusion when glucose more
than 7 mmol\l.
It is a high risk pregnancy ,so that continuous electronic fetal monitoring is
indicated.
4.postpartum:
• Insulin dose should be halved after delivery.
• Contiue insulin infusion until pt is eating.
• Aim 4-9mml\L.
• Start pre-pregnancy insulin dose ,for those who are NIDDM revert to OHD.
• Monitor blood glucose hourly for 2 hr then postprandially for 48 hr.
• Contraception: option to be discussed COCP if not lactating , progesterone
only contraception , barrier methods, IUCD & sterilization

Obstetrics Dr. Esraa
6
Gestational diabetesIs
defined as CHO intolerance that begins or is first recognized during pregnancy &
most cases resolve after delivery.
Risk factors for GDM
Glucoseuria in the 1
st
trimester.
• Glucoseuria on 2 occasion in 2
nd
or 3
rd
trimester.
• Polyhydramnios in current pregnancy.
• Macrosomia( AC above 95
th
centile) in current pregnancy.
• Large for gestational age ( EFW above 95
th
centile)
• Previous unexplained stillbirth.
• Previous macrosomic baby.
• Previous GDM
• Family history in 1
st
degree relative.
• BMI˃25. orwt ˃85 kg.
• Age ˃ 35.
• Recurrent miscarriage.
For 1
st
5 factors , oral glucose tolerance test should be performed at any stage
up to 32 wk.
For the remaining factors OGTT should be performed at 26-28 wk
OGTT
The test should be performed after overnight fast
• With 75 g glucose.
• The women should be seated throughout the procedure.
• 2 venous blood samples (FPG before glucose load & 2hr plasma glucose).
WHO diagnosis of GDM
• FPG ≥ 5.5 mmol\L.
• 2 hr plasma glucose ≥ 8mmol\L

Obstetrics Dr. Esraa
7
Management during pregnancy
1.Monitoring of glycaemic control: regular blood glucose measurement ( fasting
& 2 hr postprandial after each meal).
2. Fetal monitoring:-
Twice weekly NST & AFI
Daily record of fetal movement from 28 wk
BPP
Doppler ultrasound
3. Glucose control :
-- dietary control:
40-60% of energy from CHO, 20-30% from protein & remaining
from fat . during pregnancy there is accelerated starvation , therefore at least 3
meals& 4 snacks with last snack at bedtime to avoid overnight hypoglycaemia.
-- insulin control:-Indication for insulin therapy:
1. FPG ˃ 5.8mmol\L
2. Post prandial ˃ 7.2 mmol\L
3. Fetalmacrosomia in 3
rd
trimester.
4. Failed dietery treatment for 2 wk.
Insulin dose =
1
st
trimester→ body wt X 0.6.
2
nd
trimester→ body wt x 0.7.
3
rd
trimester → body wt X 0.8.
Dosage schedule: ⅔ in AM and ⅓ in PM
Before breakfast ⅔ intermediate acting & ⅓ soluble
Before dinner 1\2 intermediate& 1\2 soluble or regular.
Or short acting insulin before each meal & intermediate acting before bedtime
The aim is :FPG 3.5-5.5 mmol\l
RBG 4-6.5 mmol\l
HbA1c ˂ 7%
In women presented with PTL , steroid should be given but it may induce
hyperglycemia,
increase dose by 40% at time of 1
st
dose & until 24 hr after 2
nd
dose.
OHD: are not recommended because cross placenta & have teratogenic effect ,
tight glycemic control is difficult.

Obstetrics Dr. Esraa
8
Management in labour & delivery
Women with GDM on diet only require no specific measures during labour
Women with GDM on insulin should be managed in similar way to pre
GDM........
Management in postpartum
• In women with GDM on diet therapy , there is no need to control diet
while women using insulin must reduce their insulin requirement. If they
are breast feeding insulin should be reduced by 75% before being
discontinued , in those not breast feeding , insulin can be discontinued
when the pt can eat or drink
• Contraception: in breast feeding mother , COCP are relatively
contraindicated , so progesterone only contraception, IUCD & barrier
methods are useful option.
• At end of puerperium FPG should be estimated , if this abnormal , OGTT
should be done.
• 50% of women developed type 2 DM in the next few years.
