
1
Dr. Esraa
Puerperium:- consist of period following delivery of baby & placenta to 6 week postpartum. During
puerperium reproductive organs and maternal physiology return toward prepregnancy state, although
menses may not return for much longer .
Anatomical & physiologic changes:
1.Involution of uterus: is the process by which post partum uterus decreases in weight (weighing
about 1000 g to 100 g), immediately after delivery uterine fundus lies 12 cm above symphysis pupis
or 4cm below umbilicus. within 2 weeks uterus is no longer palpable above symphysis.
Involution is accelerated by release of oxytocin in women who are breast feeding , as the uterus is
smaller than in those who are bottle feeding
Causes of delayed involution (subinvolution)
1. Full bladder
2. Loaded rectum
3. Uterine infection
4. Retained product of conception
5. Fibroid
6. Broad ligament hematoma
2. Genital tract changes:. In 1
st
few days , cervix can admit 2 fingers , but by end of 1
st
week it
difficult to pass more than one finger , by end of 2
nd
week internal os should be closed , external os
can remain open permanently giving characteristic of parous cervix.
Puerperium
2
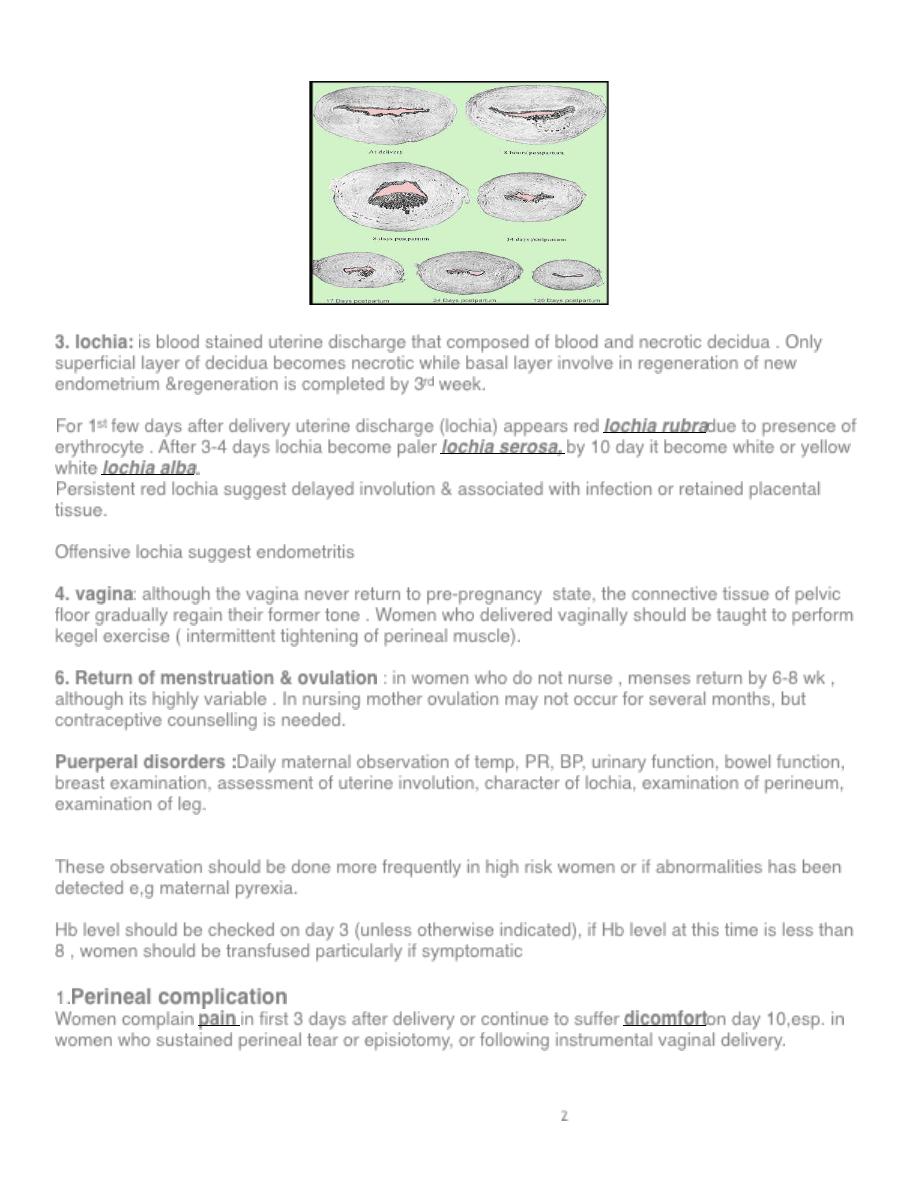
3. lochia: is blood stained uterine discharge that composed of blood and necrotic decidua . Only
superficial layer of decidua becomes necrotic while basal layer involve in regeneration of new
endometrium ®eneration is completed by 3
rd
week.
For 1
st
few days after delivery uterine discharge (lochia) appears red lochia rubradue to presence of
erythrocyte . After 3-4 days lochia become paler lochia serosa, by 10 day it become white or yellow
white lochia alba.
Persistent red lochia suggest delayed involution & associated with infection or retained placental
tissue.
Offensive lochia suggest endometritis
4. vagina: although the vagina never return to pre-pregnancy state, the connective tissue of pelvic
floor gradually regain their former tone . Women who delivered vaginally should be taught to perform
kegel exercise ( intermittent tightening of perineal muscle).
6. Return of menstruation & ovulation : in women who do not nurse , menses return by 6-8 wk ,
although its highly variable . In nursing mother ovulation may not occur for several months, but
contraceptive counselling is needed.
Puerperal disorders :Daily maternal observation of temp, PR, BP, urinary function, bowel function,
breast examination, assessment of uterine involution, character of lochia, examination of perineum,
examination of leg.
These observation should be done more frequently in high risk women or if abnormalities has been
detected e,g maternal pyrexia.
Hb level should be checked on day 3 (unless otherwise indicated), if Hb level at this time is less than
8 , women should be transfused particularly if symptomatic
1.
Perineal complication
Women complain pain in first 3 days after delivery or continue to suffer dicomforton day 10,esp. in
women who sustained perineal tear or episiotomy, or following instrumental vaginal delivery.
3
Local cooling such as crushed ice & topical anasthesia can provide short term relief. Paracetamol,
oral or rectal diclofenac are also effective , codiene should not be used because they may cause
constipation
Infection of perineum may occur due to bacterial contamination, swab should be taken for
microbiological culture and broad spectrum antibiotic should be started .
Spontaneous opening of repaired episiotomy is result of secondary infection, surgical repair
should never be attempted in presence of infection. The wound should be irrigated daily and healing
is allowed to occur by secondary intention . If there is large gaping wound, secondary repaired can be
done after the infection has been cleared
2.Care of the Bladder
factors predisposing to increased urine production in the puerperium
1. with regional anesthesia bladder may take up to 8 hours to regain sensation
2.Fluid overloading prior to epidural analgesia
3. Antidiuretic effect of high concentration of oxytocin during labour
4. Increase post partum diuresis
5. Increase fluid intake by breast feeding mother.
Causes of difficulty to void :
1. Instrumental vaginal delivery
2. Multiple or extended laceration
3. Vulvovaginal hematoma
4. Stool impaction of rectum
5. Abdominal wall hematoma
VD is strongly implicated in development of urinary stress incontinence but rarely cause a problem in
early puerperium, therefore incontinence should be investigated to exclude vesicovaginal or
urethrovaginal or uretrovaginal fistula , fisula occurs due to pressure necrosis of urethra or bladder
following obstructed labour.
Presentation occur usually in 2
nd
week , small fistula heal spontaneously while large one require
surgical repair.
3.
Bowel Function
: mild ileus follows delivery, together with perineal discomfort & postpartum fluid
loss by other routes, predisposes to constipation during the puerperium.
Hemorrhoidal discomfort is a common complaint & responds to conservative treatment with
suppositories containing corticosteroids, local anesthetic.
4.Secondary PPH
Genital tract bleeding between 24 hr and 6 wk after delivery
•
Retained placental tissue
•
Endometritis
•
Hormonal contraception
•
Bleeding disorder
•
choriocarcinoma
5.Complication of breast feeding
4
Blood stained nipple discharge: usually bilateral due to epithelial proliferation . Occur in 2
nd
or 3
rd
trimester & resolve after 3
rd
months postpartum , no treatment is required only reassurance
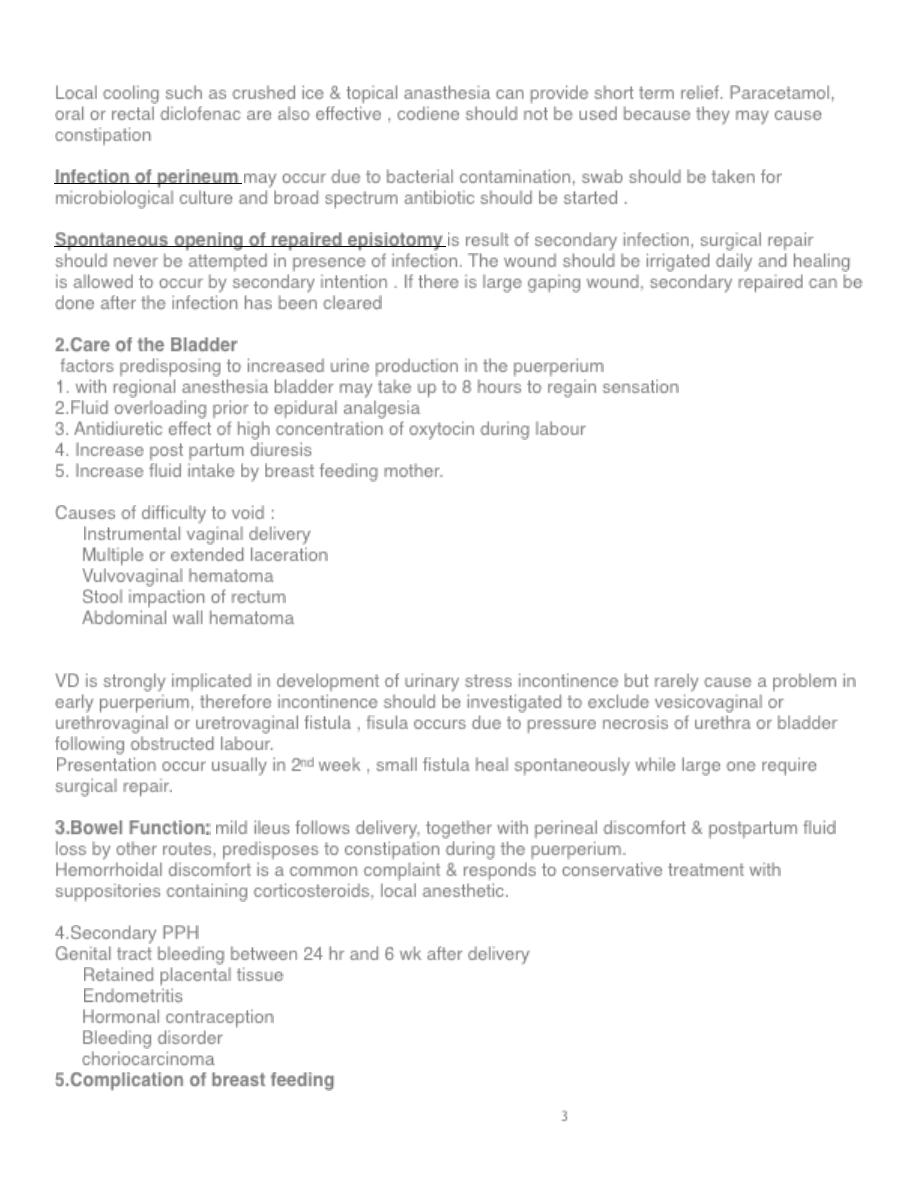
Cracked Nipples : occurs due to poor positioning of baby on breast leading to difficult breast feeding.
because fissures are portal of entry for bacteria they should be treated aggressively with nipple shield
and cream . Breast feeding can be stopped and milk can be expressed manually until nipples heal.
Breast engorgement:-
Bilateral pain 2 to 3 days after child birth and if breast feeding is not effectively established leading to
hard, painful breasts.
Breast engorgement can give rise to puerperal fever but other causes should be excluded.
Manual expression, firm support, application of ice pack, elastic breast pump are recommended in the
past but allowing baby easy access to breast is most effective treatment.
Mastitis : occur when a blocked duct obstructs the flow of milk, so milk extravasates in to perilobular
tissue , intiating inflammatory process. The affected segment of breast will be painful, red
&oedematous with pyrexia which persist longer than 24 hr in contrast to fever due to engorgement
which last less than 24 hour
Causative agent : staph aureus
The sources of infection : babys nose or throat.
Management: cessation of breast feeding from affected breast , expression of milk manually or by
pump.
breast milk should be sent for c&s . Flucloxacillin can be used while awaiting for result. Whenever
breast abscess is developed, should be drained surgically under GA.
6.Thromboembolism
The risk of thrombo embolism is increased by 5- folds during pregnancy &puerperium. If DVT or
pulmonary embolism is suspected full anticagulant therapy should be started & lower limb ultrasound,
lung scan should be carried out.
Postpartum Immunization
Prevention of Rh Isoimmunization
5
postpartum injection of Rh
o
(D) immunoglobulin will prevent sensitization in Rh-negative woman
who has had Rh-positive fetal red cells is given intramuscularly to the mother within 72 hours after
delivery.
Rubella Vaccination
Women who are susceptible to rubella can be vaccinated with a live attenuated rubella virus
vaccine during the immediate puerperium.
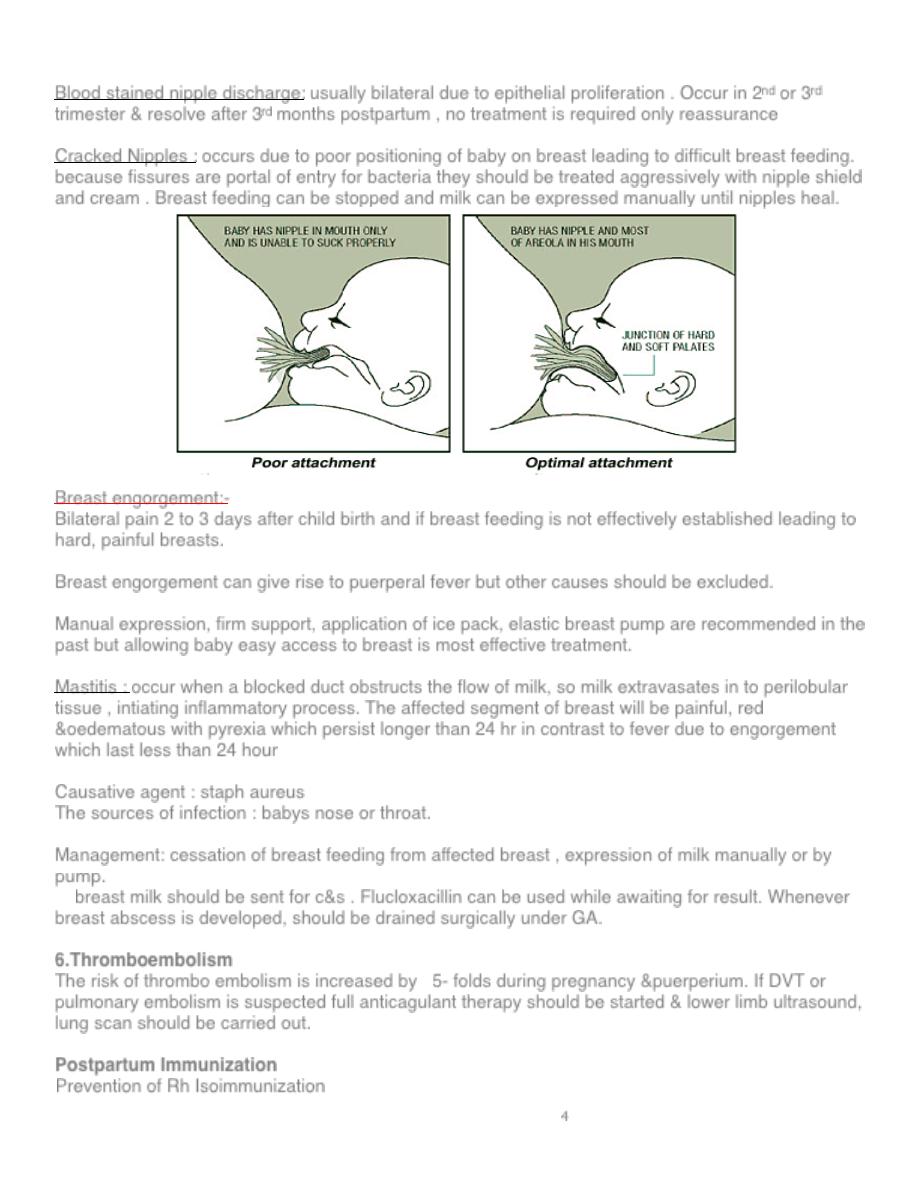
Contraception & Sterilization
Lactational amenorrhea occur because lactation inhibit LH release from anterior pituitary , lactation
can provide effective contraception but not totally reliable (full breast feeding is associated with 2%
risk of pregnancy in first 6 months).
IUCD :it is best to wait at least 4-8 wk to allow involution .
Combined contraceptive pills increase risk of thrombosis in early puerperium & decrease amount of
breast milk. women who are not breast feeding can start COCP within 6 weeks of delivery.
Progesterone only pills is preferable &can be taken at day 21 post delivery.
Injectable contraception is also effective e,g depot medroxyprogesterone given 3 monthly or
norethisterone enanthate given 2 monthly. injectable contraception are preferable to be given at 5-6
wk post partum
Sterilization in form of tubal ligation can be performed for women who have completed her family,
either during CS or by minilapartomy in first few post partum days or by laparscopy at 6 wk post
partum
Postnatal examination
carried out at 6 week postpartum include direct question must be asked
about urinary or anal incontinence or dyspareunia.
, blood pressure should be checked.
General, abdominal& pelvic examination is performed.
If cervical smear is due , it can be taken, although it is preferable after 3 months.
Contraception & pelvic floor exercise should be discussed.
