Non pharmacological methods:
One- one care in labour: from a midwife or partner can reduce need for analgesia
Relaxation & breathing exercise but prolonged hyperventilation can lead to alkalosis.
Acupuncture & hypnosis.
Relaxation in warm water in first stage of labour
TENS : trans-cutaneous electrical nerve stimulation block pain fibres in posterior
ganglia of spinal cord.
Pharmacological:
Opiates such as pethidine & dimorphine can be used as a pain relief in labour but
associated with significant side effects:
1. Nausea & vomiting: they should be used with antiemetic.
2. Maternal drowsiness& sedation.
3. Delayed gastric emptying increasing risk if GA is subsequently used.
4. Short term respiratory depression in baby.
5. Possible interference with breast feeding.
Inhalational analgesia:
Nitrous oxide in form of entonox (a mixture of NO & oxygen)
Rapid onset & short duration of action
More effective than pethidine
Cause light headedness & nausea
It is not suitable for prolonged use because hyperventilation can cause tetany &
fetal hypoxia
- Suitable later in labour or while awaiting epidural analgesia.
Epidural analgesia: Indications:
1. Prolonged labour
2. Maternal hypertensive disorders
3. Multiple pregnancy
4. Certain maternal medical disorder
5. High risk for operative intervention
Contraindications:
1. Coagulation disorders
2. Local or systemic sepsis
Obstetric analgesia &anaesthesia
3. Hypovolemia
4. Insufficient numbers of trained staff.
Women must be informed:
1. About risk & benefit
2. warn the women that she may lose sensation & movement in her legs
3. Need for intravenous access
4. Need for more intensive maternal & fetal monitoring.
Epidural cause prolonged 2nd stage of labour & increase chance of IVD , which may be
reduced by oxytocin infusion
Epidural in 2nd stage relax the women & allow time for head to rotate & descend
Epidural will limit mobility.
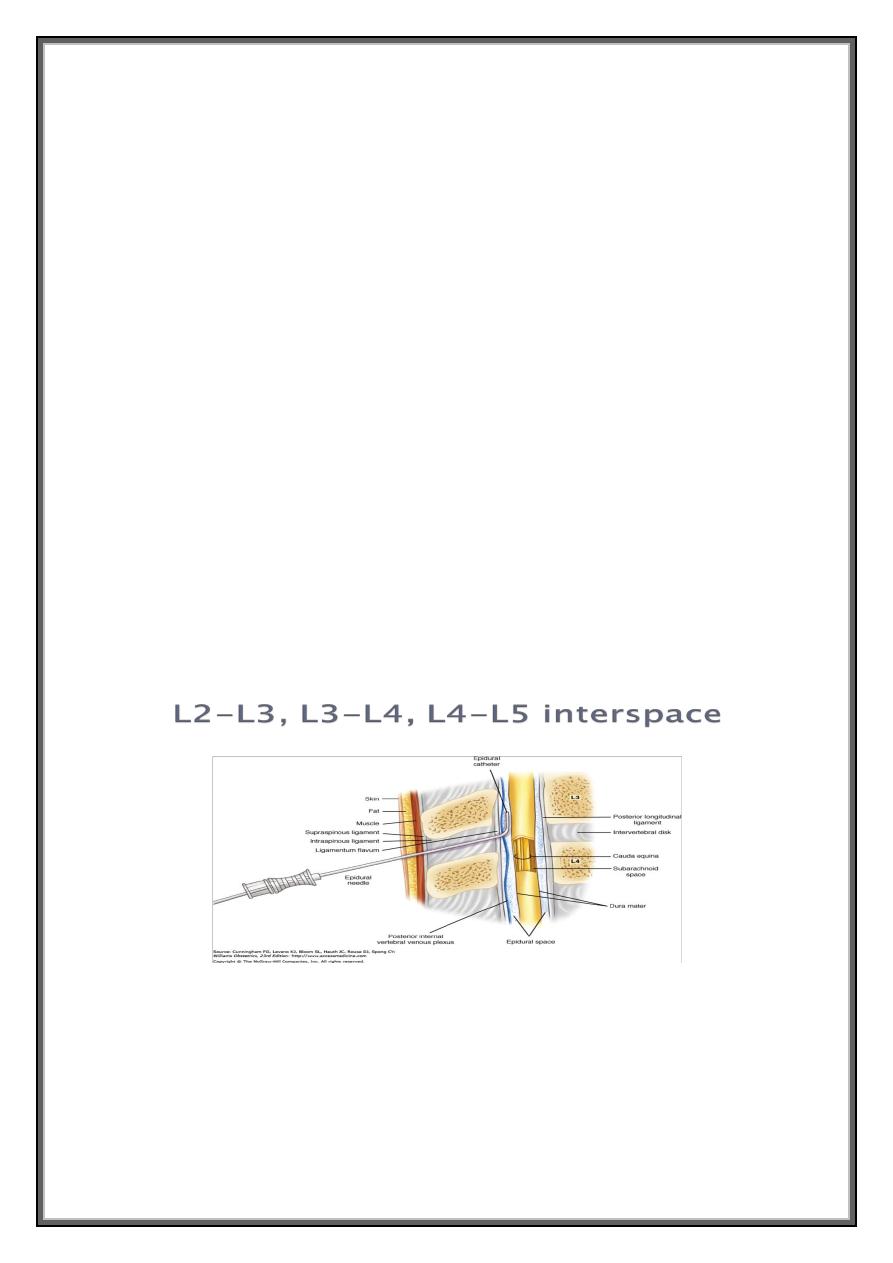
Complications of regional analgesia
1. Accidental dural puncture: the needle used for epidural is wider bore than used for
spinal. If subarachnoid space is reached with epidural needle , there will be a large
hole that lead to leak of CSF.
This result in spinal headache which occur on the top of head & relieve by lying
flat & aggravated by sitting upright . If the headache is severe , a blood patch is
necessary which involve injecting small volume of women s blood at level of
accidental puncture , resulting in blood clot.
2. Accidental total spinal anaesthesia : injection of epidural doses of local A into
subarachnoid space causing severe hypotension & respiratory failure . The mother
require intubation , ventilation , iv fluid , vasopressor , left uterine displacement &
urgent delivery of baby to permit maternal resuscitation.
3. Spinal hematoma is rare complication & usually associated with other factors
4. Drug toxicity: due to accidental placement of catheter within blood vessels & this
noticed by aspiration of blood prior to injection
5. Bladder dysfunction: this occur because the women unaware of need to micturate.
To avoid overdistension of bladder , catheterization of bladder should be carried out.
6. Hypotension : more common with spinal can be corrected IV fluid & vasopressor.
7. Short term respiratory depression of baby because all epidural solution contain
opioid that reach maternal circulation & cross the placenta.
Spinal anaesthesia:
Faster onset & more effective than epidural
A fine needle is passed through epidural space, dura into subarachnoid space
which contain CSF & a small volume of LA is used.
This type of anasthesia is used for delivery by CS or IVD, manual removal of
retained placenta, repair of difficult vaginal or perineal tear .
Combined spinal-epidural :
Provide rapid onset of pain relief
Prolonged analgesia.
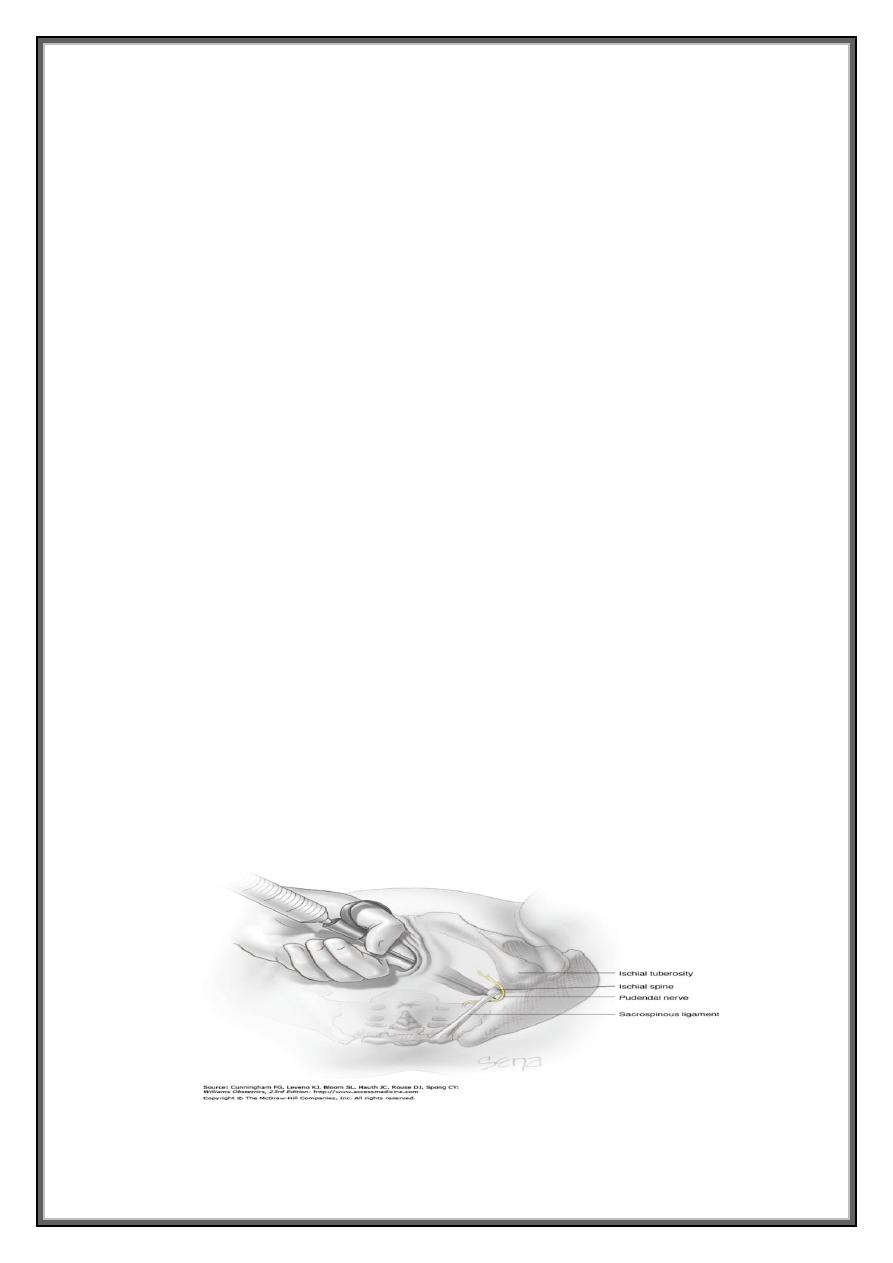
Pudendal Block:
This block is a relatively safe and simple method of providing analgesia for
spontaneous delivery. Involve injection of local anaesthesia to pudendal nerve that
locate behind ischial spine. Providing anaesthesia to lower vagina and posterior vulva
bilaterally without pain.
Pudendal block usually does not provide adequate analgesia when delivery requires
extensive obstetrical manipulation &such analgesia is inadequate for women in
whom complete visualization of the cervix and upper vagina or manual exploration of
the uterine cavity is indicated. Complication: intravascular injection, hematoma ,
infection.
Paracervical Block:
This block usually provides satisfactory pain relief during the first stage of labor. LA is
injected into the cervix laterally at 3 and 9 o'clock. Because these anesthetics are
relatively short acting, paracervical block may have to be repeated during labor.
Complications: Fetal bradycardia :Bradycardia usually develops within 10 minutes
and may last up to 30 minutes. For these reasons, paracervical block should not be
used in situations of potential fetal compromise.
General Anesthesia:
Patient Preparation: Prior to anesthesia induction, several steps should be taken to
minimize the risk of complications for the mother and fetus. These include the use of
antacids, lateral uterine displacement, and preoxygenation.
Induction of Anesthesia:
Thiopental: given intravenously, offers easy and rapid induction, prompt recovery,
and minimal risk of vomiting.
Ketamine: This agent also may be used to render a patient unconscious. ketamine
may be used to produce analgesia and sedation just prior to vaginal delivery.
Ketamine may also prove useful in women with acute hemorrhage because, unlike
thiopental, it is not associated with hypotension.
Conversely, it usually causes a rise in blood pressure, and thus it generally should be
avoided in women who are already hypertensive. Unpleasant delirium and hallucinations
are commonly induced by this agent.
Intubation: Immediately after a patient is rendered unconscious, a muscle relaxant is given
to aid intubation. Succinylcholine, a rapid-onset and short-acting agent, commonly is used.
Cricoid pressure is used by a trained assistant to occlude the esophagus from the onset of
induction until intubation is completed. Before the operation begins, proper placement of
the endotracheal tube must be confirmed.
Gas Anesthetics: Once the endotracheal tube is secured, a mixture of nitrous oxide and
oxygen is administered to provide analgesia. Usually, a volatile halogenated agent is added
to provide amnesia and additional analgesia .
Extubation: The tracheal tube may be safely removed only if the woman is conscious to a
degree that enables her to follow commands and is capable of maintaining oxygen
saturation with spontaneous respiration.
