Obstetrics Lec 19 Dr. Aseil
1
RHESUS ISO-
IMMUNIZATION
TWO WAYS OF BLOOD GROUP
1. Blood group (O, A, B, AB)
2. Rhesus system – C, D and Eantigens
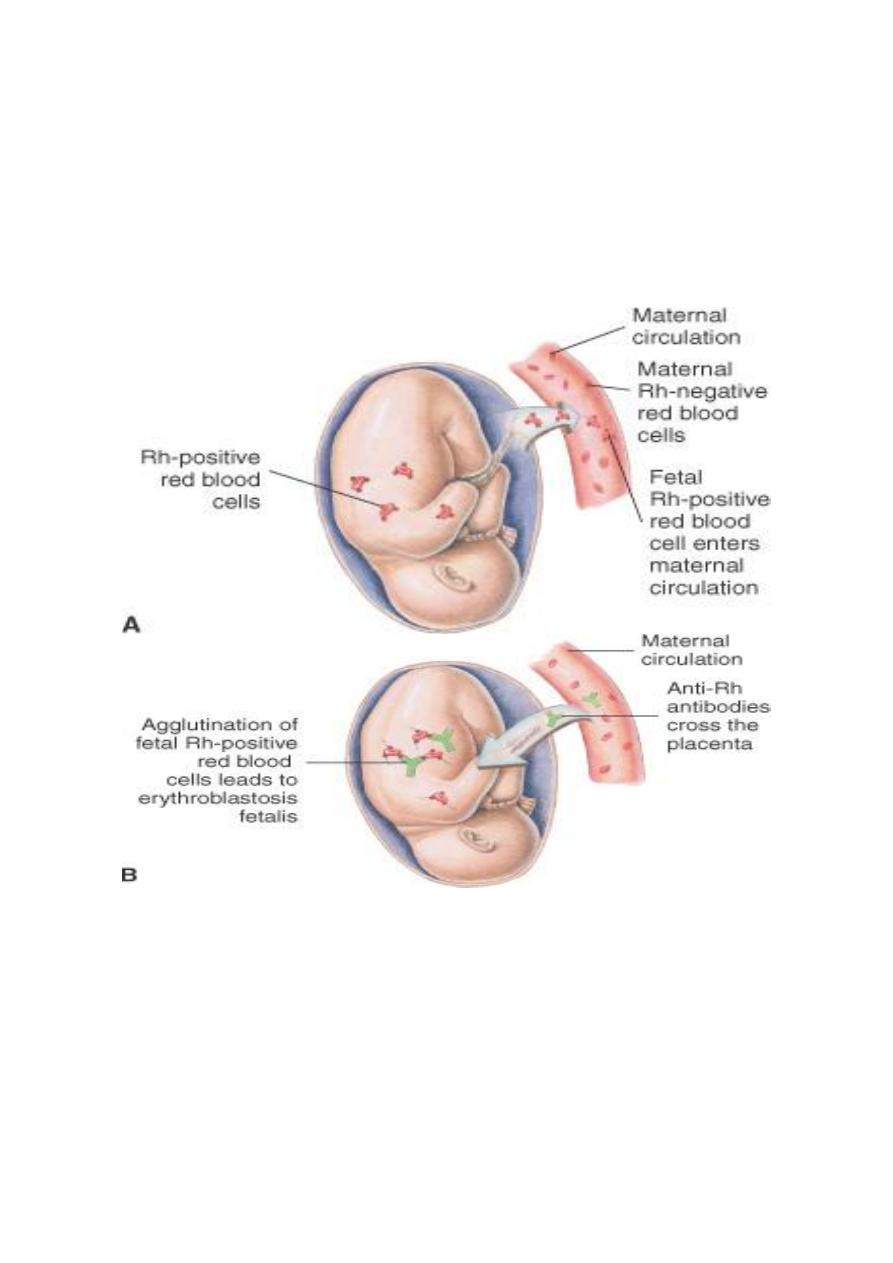
Miss match between the fetus & mother mean that when fetal red cells
pass across the placenta to the maternal circulation, as they do to a
greater or lesser extend during pregnancy, sensitization of the maternal
immune system to these fetal 'foreign' red blood cells may occur & leads
to HDFN.
TWO TYPES OF Iso -Immunization
ABO blood group iso-immunization may occur when the mother is blood
group O and the baby is blood group A or B. Anti-A and anti-B antibodies
are present in the maternal circulation naturally, and hence do not require
prior sensitization in order to be produced. This means that ABO
incompatibility may occur in a first pregnancy.
anti-A or anti-B antibodies pass to the fetal circulation, causing fetal
haemolysis and anaemia. ABO incompatibility causes mild
haemolyticdisease because most of the Abs are IgM& do not cross the
placenta , in addition A & B Ag are not fully developed in the fetus.
The anti-D & anti-c are associated most commonly with severe haemolytic
fetal disease. This can only occur if the mother is D rhesus negative and
the baby is D rhesus positive.
Obstetrics Lec 19 Dr. Aseil
2
THE AETIOLOGY OF RHESUS DISEASE
This does not affect the first pregnancy.
The mother must expose to RH +ve fetal RBC during the delivery of the first baby
in a sufficient volume to provoke immune response ,she will develop IgM at first
then IgG later is formed which remain dormant until the next pregnancy if the
baby is RH +ve then will be re-sensitization, The IgG pass to the fetal circulation
causing sever haemolysis, sever anemia and fetal death.
Prevalence :
RH negativity is 15% in Caucasian population.
But lower in all other ethnic groups.
Iso-immunization is more common in countries where anti D prophylaxis
not used like middle east and Russia.
Obstetrics Lec 19 Dr. Aseil
3
POTENTIAL SENSITIZING EVENTS FOR RHESUS DISEASE
Miscarriage
Termination of pregnancy
Antepartum haemorrhage
Invasive prenatal testing (chorion villus sampling, amniocentesis and
cordocentesis),ECV.
Delivery mainly during 3
rd
stage.
Complication of RH isoimmunization:
1- Abortion.
2- Preterm labour.
3- Hydropsfetalis.
4- Intrauterine death.
5- Less severely affected baby present with neonatal jaundice within few
hours after delivery.
SIGNS OF FETAL ANAEMIA(Hydropsfetals)
Polyhydramnios
Enlarged fetal heart ,hepatosplenomegally
Ascites and pericardial effusions
Hyperdynamic fetal circulation (can be detected by Doppler ultrasound by
measuring increased velocities in the middle cerebral artery or aorta).
Reduced fetal movements
Abnormal CTG with reduced variability, eventually a 'sinusoidal' trace.
Placenta edematous
PREVENTING RHESUS ISO-IMMUNIZATION
The intramuscular administration of anti-D Ig to a mother, preferably within 72
hr of exposure to fetal RBC The dose range from 100-500 IU .The exact dose is
determined by the gestation at which sensitization has occurred and the size of
the feto-maternal haemorrhage.
Kleihauer test of maternal blood to determined the proportion of fetal cells
present (relying on their ability to resist denaturation by alcohol or acid); it
willallow calculation of the extra amount of anti-D Ig required should a large
transfusion has occurred.In some countries Rhesus-negative women are given
anti-D at 28 and/or 34 weeks routinely.
Obstetrics Lec 19 Dr. Aseil
4
Causes why every women is not sensitized:
ABO incompatibility between the mother and fetus .
The mother immune system is non responder.
The amount and antigenisity of the D antigen.
Once she is sensitized , no amount of anti-D will ever turn the clock back,
there is therefore no role for anti-D
THE MANAGEMENT OF RHESUS DISEASE
The woman has been sensitized to the D rhesus antigen, manifesting itself by
raised Ab titer or an adverse pregnancy outcome & follow up by Ab level every
2-4w from booking.
Anti-D titer more than 4 iu /mlOr previous history of hydrops
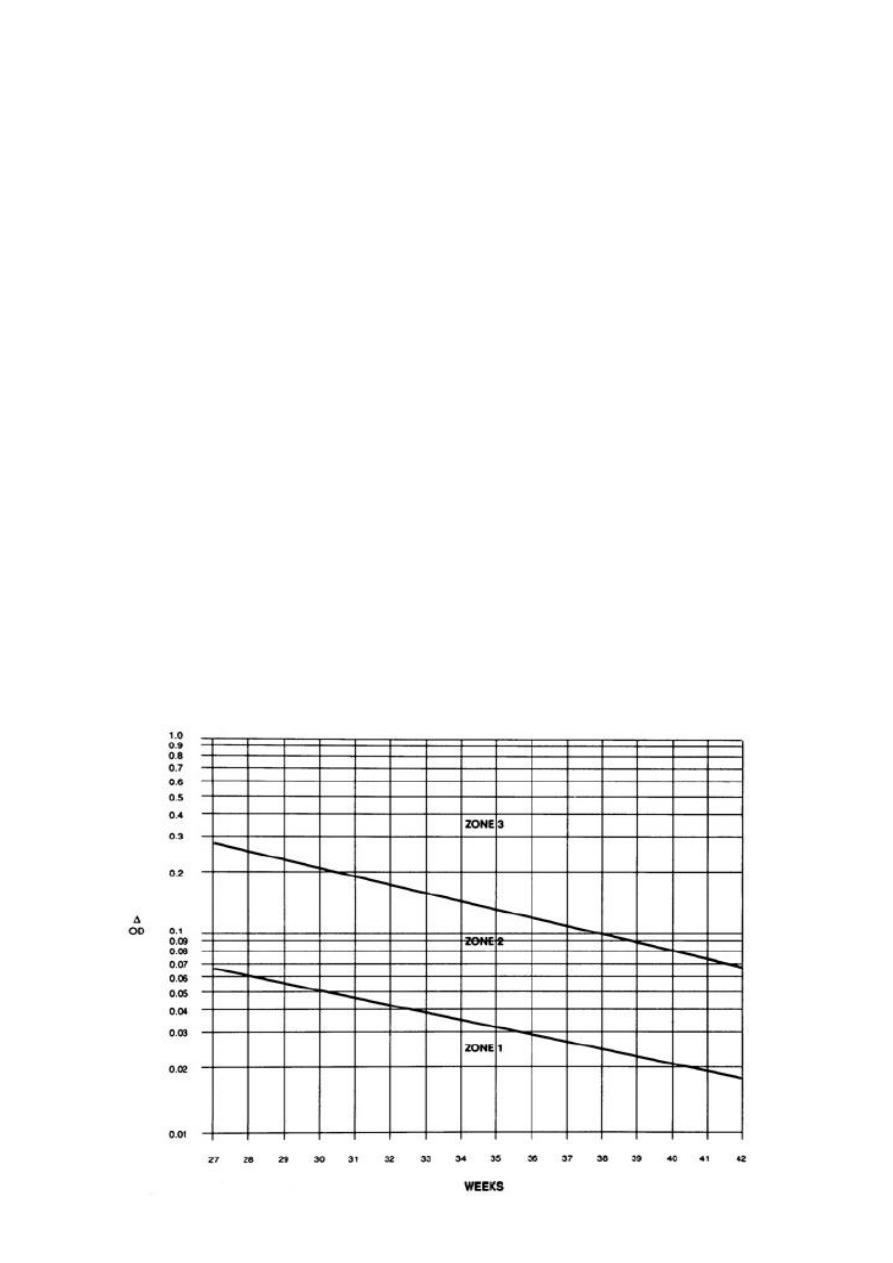
The follow up by serial amniocentesis to determined bilirubin concentration by
spectrophotometer analyzed at absorbance (optical density) of 450( OD 450)
and plotted on Liley chart.
According to the lileys chart divided to 3 zone.
Zone 1 mild affected baby needs follow up by monthly amniocentesis.
Zone 2 moderate affected baby so repeat the amiocentesis 2 weekly.
Zone 3 severly affected baby need blood transfusion by cordocentesis ,
according to the level of the Hb and gestational age.

Obstetrics Lec 19 Dr. Aseil
5
In the last decade,middle cerebral artery Doppler have been shown to correlate
reliably with fetal anaemia. This means that invasive tests to monitor disease
progression have been replaced by non-invasive assessment using MCA doppler.
Then Rx options are either delivery(if sufficiently mature fetus ) or fetal Bd
transfusion( if severlyanaemic& too premature
BLOOD TRANSFUSION
Blood may be given to the baby by a needle introduced through the mother's
abdomen. Blood is given either intravascularly (into the umbilical
vein,intrahepatic vein or heart) or intraperitoneally (in low gestations).
Blood transfused to the fetus must be:
- densely packed (Hb around 30g/dL)
-screend for infection including CMV
- rhesus negative cross matched with maternal Bd
-WBC irradiated (to reduce the risk of graft-versus-host disease)
Management of the baby after delivery:
If the baby known to be anemic with multiple intra-uterin transfusions
neonatologist must be present at delivery should exchange transfusion be
required.
Cord blood should be taken to estimate Hb level.
Blood group and RH.
Bilirubine level.
Direct coombs test
