!
!
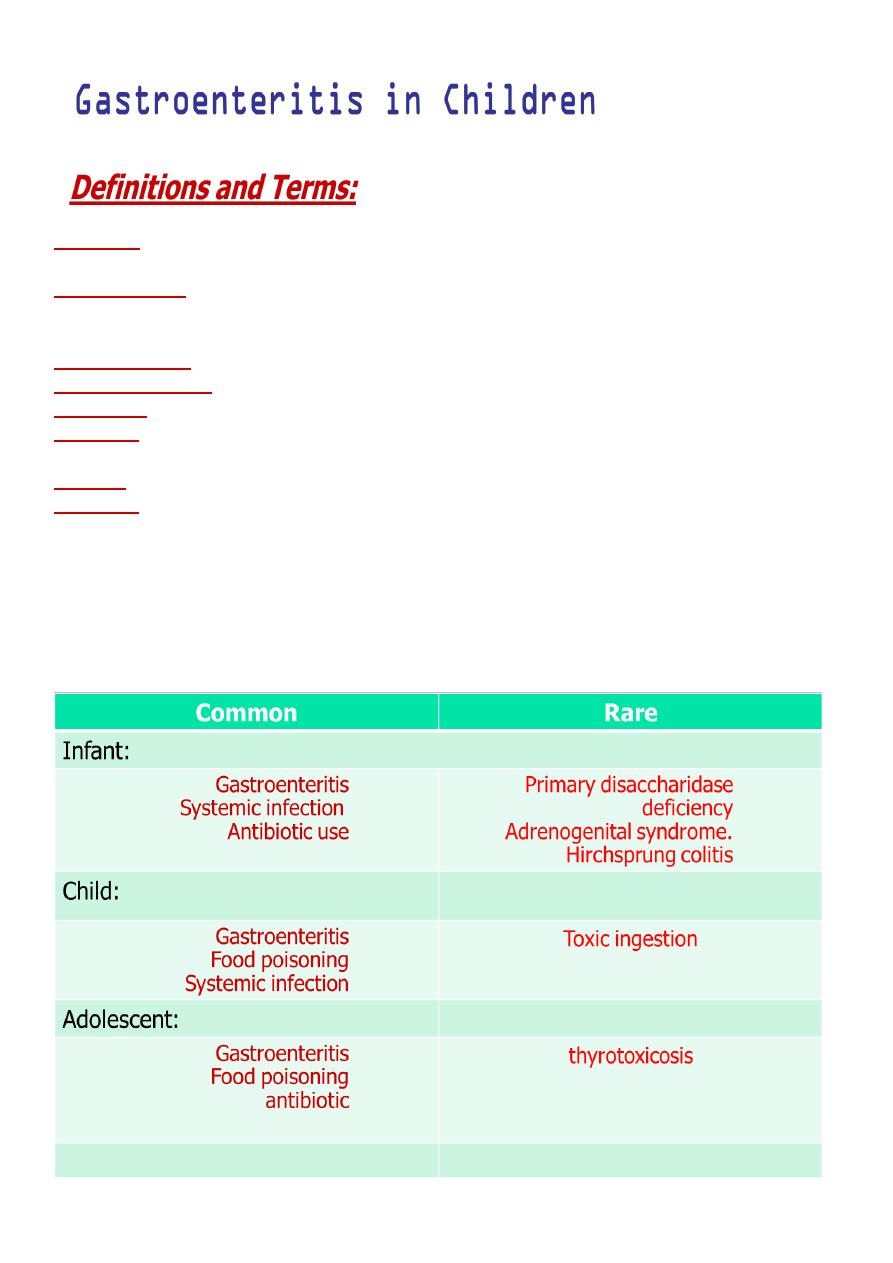
Diarrhea:
the frequent passage of unformed liquid stools (3 or more loose, watery stool per
day)
Acute diarrhea
is defined as the abrupt onset of increased fluid content of stool above the
normal value of 10 mL/kg/day. In practical terms it is associated with increased frequency
and fluid consistency of stools.
Acute diarrhea:
Short in duration (less than 2 weeks).
Chronic diarrhea:
6 weeks or more.
Dysentery:
blood or mucus in stools.
Vomiting:
forceful expulsion of contents of the stomach and often the proximal small
intestine.
Nausea:
Felling of revulsion for food and an imminent desire to vomit.
Retching:
Spasmodic respiratory movements conducted with a closed glottis.
Acute diarrhea
Second leading causes of all death worldwide
Most common cause of morbidity and mortality in children worldwide
Accounts for 9% of hospitalizations in children <5 years old.
Etiology of Acute diarrhea
!
:causes of diarrhea
1- Viruses:
70-80% of infectious diarrhea in developed countries Rotavirus is the most
common cause of acute childhood Norwalk virus, cytomegalovirus, viral hepatitis and
the herpes simplex virus. Viral diarrhea spreads easily.
2- Bacteria and parasites:
bacterial diarrhea account for 10-20% of infectious diarrhea but
responsible for most cases of severe diarrhea Common bacterial causes of diarrhea
include campylobacter, salmonella, shigella and Escherichia coli.
Parasites such as Giardia lamblia and cryptosporidium account for less than 10% of cases of
diarrhea.
3- Medications:
antibiotics. Antibiotics destroy both good and bad bacteria, which can
disturb the natural balance of bacteria in intestines. This disturbance sometimes leads to
an infection with Clostridium difficile, which can also cause diarrhea.
4- Lactose:
A sugar found in milk and milk products, lactose is a common cause of diarrhea
in some people.
5- Fructose:
Fructose, a sugar found in many fruits, is a common cause of diarrhea,
especially in children.
6- Artificial sweeteners:
Sorbitol and mannitol.
7- Surgery:
Some people may experience diarrhea after undergoing abdominal surgery.
8- Other digestive disorders:
Chronic diarrhea has a number of other causes, such as
Crohn's disease, ulcerative colitis, celiac disease and irritable bowel syndrome.
GASTROENTERITIS
Gastroenteritis (GE)
is inflammation of the mucous membranes of the gastrointestinal
tract, and is characterized by vomiting and/or diarrhoea.
OR
diarrheal disease of rapid onset, with or without accompanying symptoms, signs,
such as nausea, vomiting, fever, or abdominal pain.
:Clinical features
viral GE typically present with
watery diarrhoea
without the presence of blood, with or
without
vomiting
, low grade
fever
and
anorexia
. Most are less than 5 years of age.
The typical peak period is in the
Autumn or Winter
months. A history of contact
with GE may be present.
Viral Diarrhea
Rotavirus
Norovirus (Norwalk-like)
Enteric Adenovirus
Astrovirus
Rotavirus
Leading cause of hospitalization for diarrhea in children
Most prevalent during winter season
Fecal-oral transmission: viral shedding can persist for 21 days

Acute onset of fever followed by watery diarrhea (10-20 BM/day) and can persist
for up to a week
Norovirus
Common cause of diarrheal outbreaks/epidemics
Acute onset of nausea and vomiting, watery diarrhea with abdominal cramps and
can persist for 1-3 days
Enteric Adenovirus
Primarily affects children < 4 years old
Fecal-oral transmission
Clinical picture similar to rotavirus (fever and watery diarrhea).
much less contagious than rotavirus or noroviruses
Astrovirus
Primarily affects children < 4 years old and immunocompromised
Seasonal peak in the winter
Fecal-oral transmission: viral shedding can occur for several weeks
Fever, nausea and vomiting, abdominal pain, and diarrhea lasting up to a week
Summary of Viral Diarrhea
Most likely cause of infectious diarrhea
Rotavirus and Norovirus are most common
Symptoms usually include low grade fever, nausea and vomiting, abdominal
cramps, and watery diarrhea lasting up to 1 week
Viral shedding can occur for weeks after symptoms resolve
Bacterial GE may be associated with
food or water born infections
.
It is usually characterised by the presence of
bloody diarrhoea
,
mucous
in the stools
and a
high fever
. A travel history should be sought.
Bacterial Diarrhea
Campylobacter
Salmonella
Shigella
Enterohemorrhagic Escherichia coli
Campylobacter

Most common bacterial pathogen
Transmitted through ingestion of contaminated food or by direct contact with
fecal material
Symptoms include diarrhea (+/- blood), abdominal cramps (can be severe),
malaise, fever
Most patients recover in less than 1 week but 20% relapse or have a prolonged
illness.
Treatment usually shortens the duration of bacterial shedding in the stool.
Salmonella
Most common in children <4 years old and a peak in the first few months of life
Transmitted via ingestion of contaminated food and contact with infected animals
Symptoms include fever, diarrhea, and abdominal cramping
Antimicrobial therapy can prolong fecal shedding but is recommended for those
at increased risk of invasive disease or complications, including infants <3m/o,
those with chronic GI disease, or who are immunosuppressed.
Complications include bacteremia, osteomyletis, and meningitis.
Shigella
Fecal-oral transmission
Symptoms include fever, abdominal cramps, tenesmus, and mucoid stools with or
without blood
Can lead to serious complications
Antimicrobial treatment shortens duration of illness and limits fecal shedding.
Complications: include bacteremia, toxic megacolon and perforation, and toxic
encephalopathy
E. Coli O157:H7
Transmission via contaminated food and water
Symptoms include bloody diarrhea, severe abdominal pain, and sometimes fever
Can lead to serious complications (HUS)
Antibiotics have no proven benefit and may increase the risk of complications
Summary of Bacterial Diarrhea
Can affect all age groups
Fecal-oral transmission, often through contaminated food
Typical symptoms include bloody diarrhea, severe cramping, and malaise
Antibiotic treatment not always necessary
TREATMENT
Children without dehydration can be managed at home and should be offered
their normal fluids. These can be given as small volumes but more frequently.
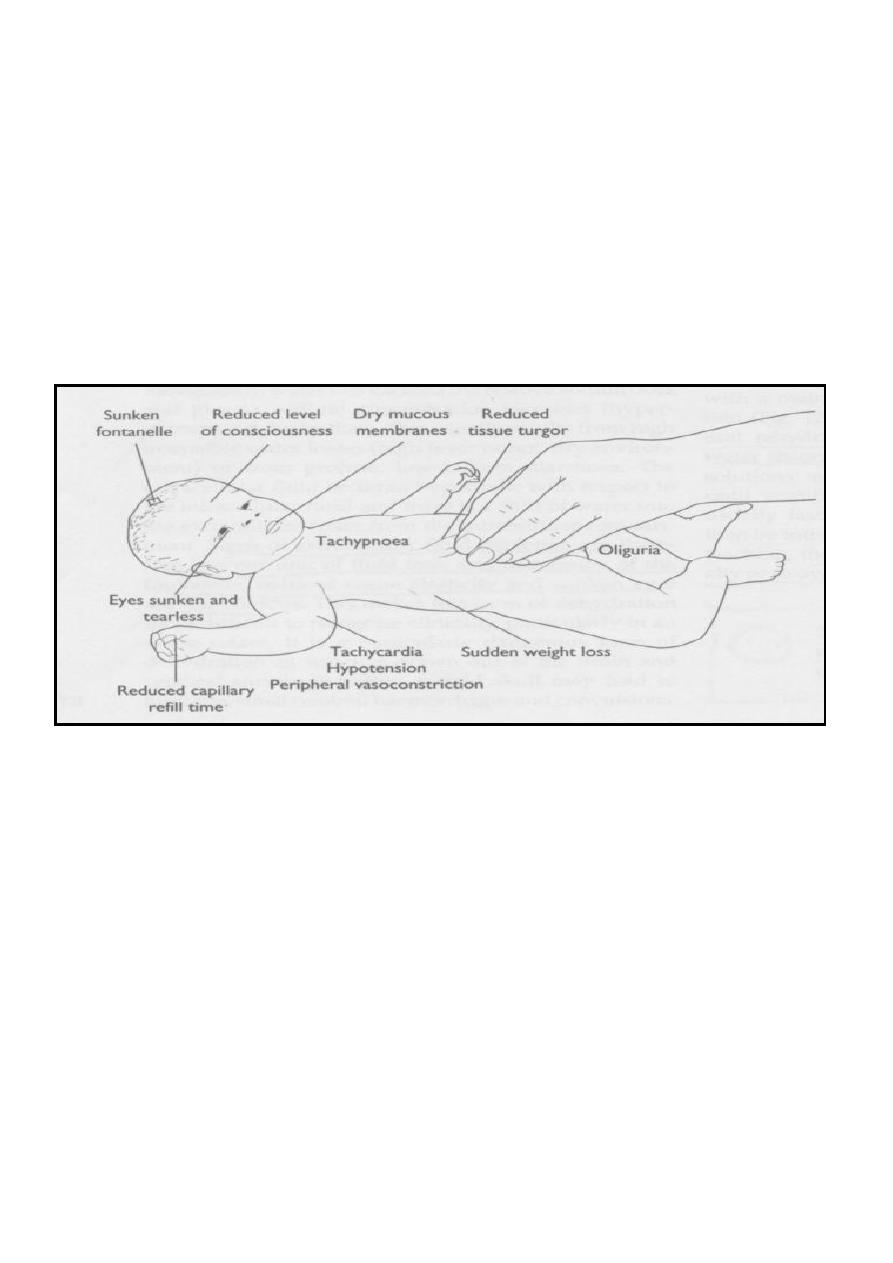
Children with mild to moderate dehydration should be observed for
4–6
hours to
ensure successful rehydration
(2–4 hours)
and maintenance of
hydration (1–2
hours)
Children at high risk of dehydration on the basis of age
(<6 months)
, high
frequency of stools
(>8 per 24 hours)
or vomits
(>4 per 24 hours)
should be
observed for at least
4–6
hours to ensure adequate maintenance of hydration and
hospital admission should be considered.
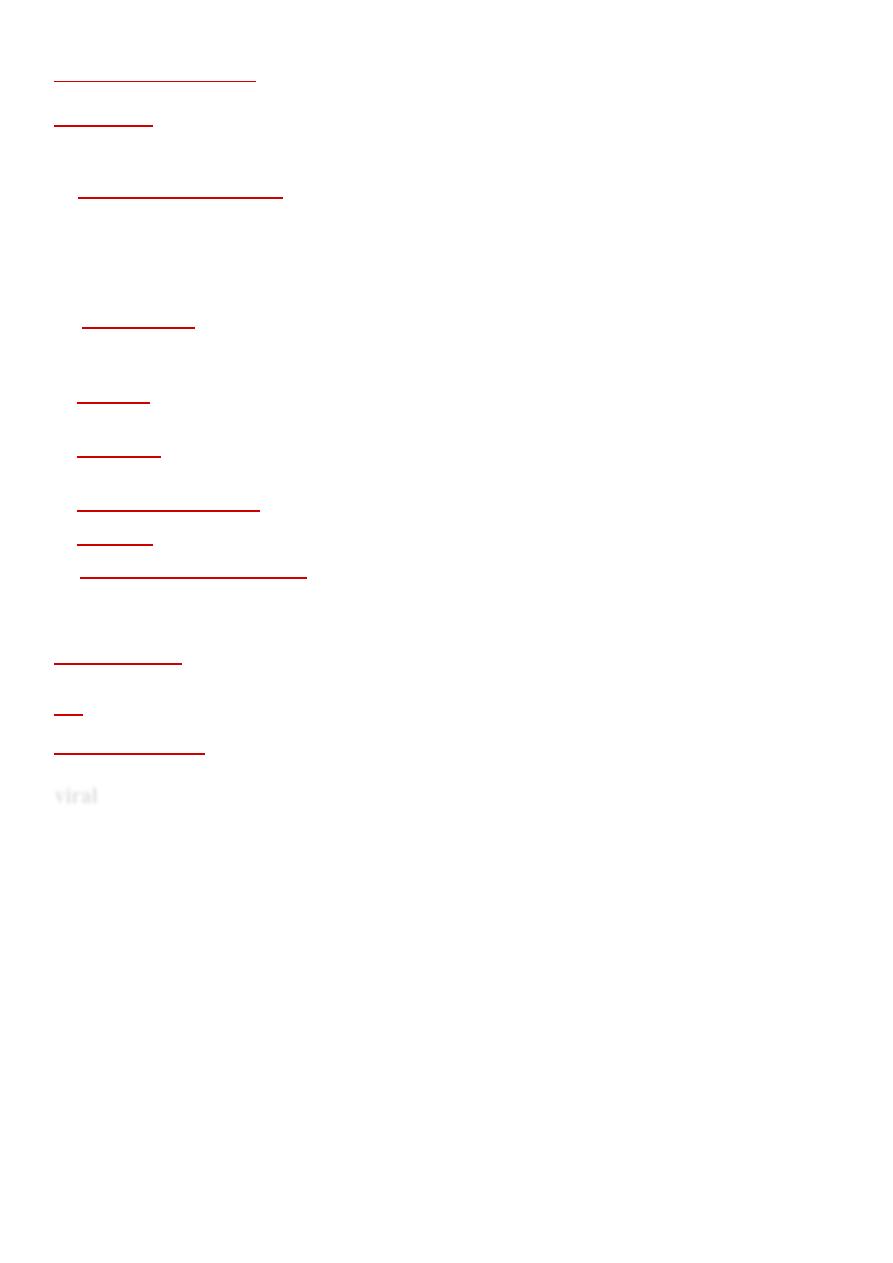
:Hospital admission is required for children
1. With severe dehydration (>9% body weight loss)
2. Whose careers or parents are thought to be unable to manage the child’s condition
at home.
3. Children with significant comorbidity (e.g. short bowel syndrome, diabetes,
congenital heart disease).
!
!
Laboratory Management
Routine cases of AGE do not require extensive laboratory workup.
1.
Stool samples
- for microscopy (include ova, cysts and parasites), culture and
sensitivity.
2.
Serum electrolytes
should be considered in cases of moderate to severe dehydration,
when the case is not straightforward, or when IV fluids are required, Also consider
electrolytes if symptoms of hyernatremia (irritability, doughy skin)
:Fluid Management
Oral rehydration therapy has repeatedly been proven to be as effective as intravenous
fluids in treatment of mild to moderate dehydration both outpatient and inpatient.
Methods of delivery include oral and via nasogastric tube.
Oral dehydration solutions contain glucose plus electrolytes. Many easily available solutions.
ORT is not effective only in the following situations
:
(1) When the patient is severely dehydrated or in shock.
(2) When oral fluid is not tolerated due to severe vomiting or ileus.
(3) When the child is unconscious or extremely fatigued.
(4) When supervision on oral fluid replacement by reliable parents is not available.
Types of ORS
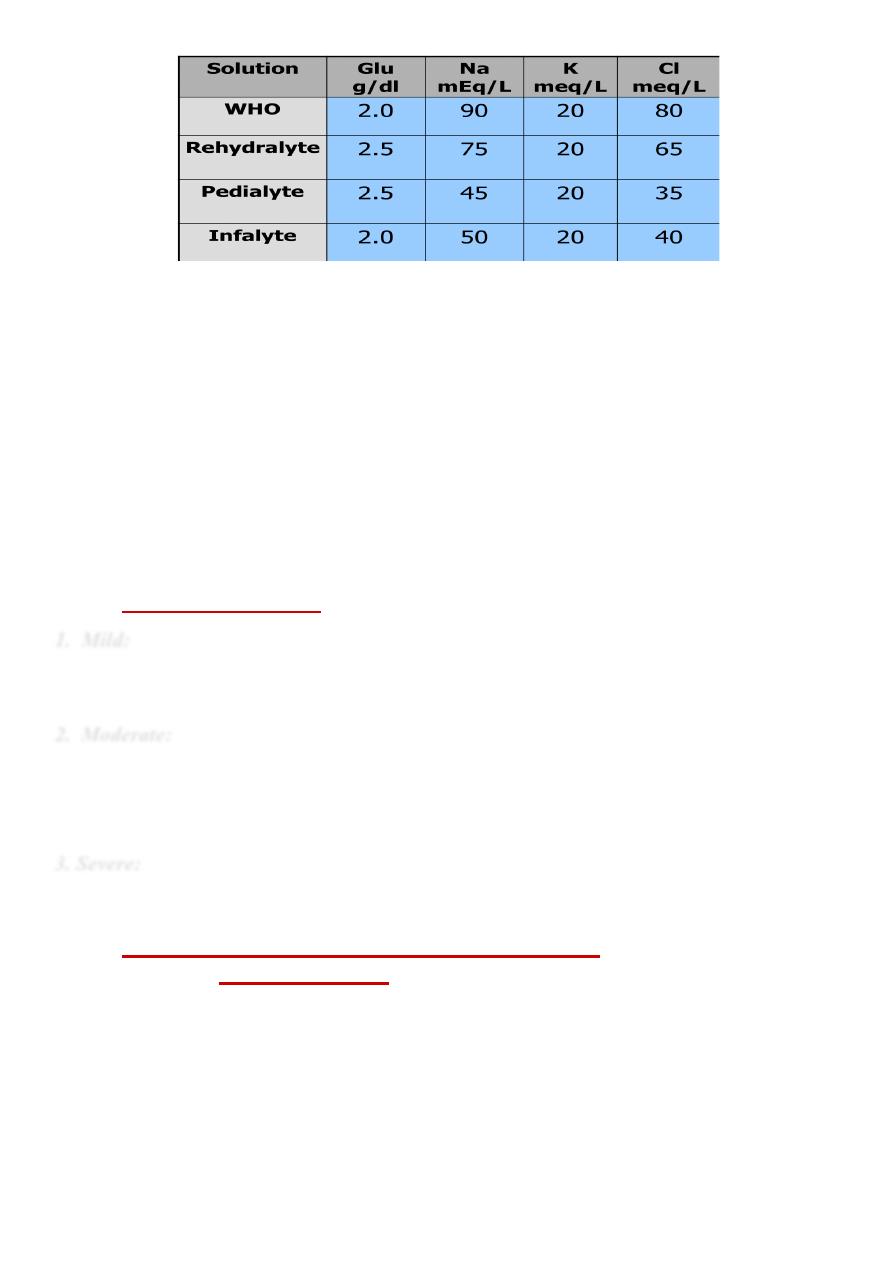
!
Physiologic Basis for ORT
Although three principle mechanisms of sodium absorption have been described,
the mechanism essential to the efficacy of ORS is the coupled transport of
sodium and glucose molecules at the intestinal brush border.
This mechanism remains intact, even in patients with severe diarrhea.
Osmolarity is important!
Solutions with a high concentration of co-transporters increase the
risk from hypertonic solutions that decrease rather than improve
sodium and water transport into the bloodstream.
However, solutions of lower osmolarity, but that maintain the 1:1
glucose to sodium ratio, perform optimally as oral solutions for
diarrhea management.
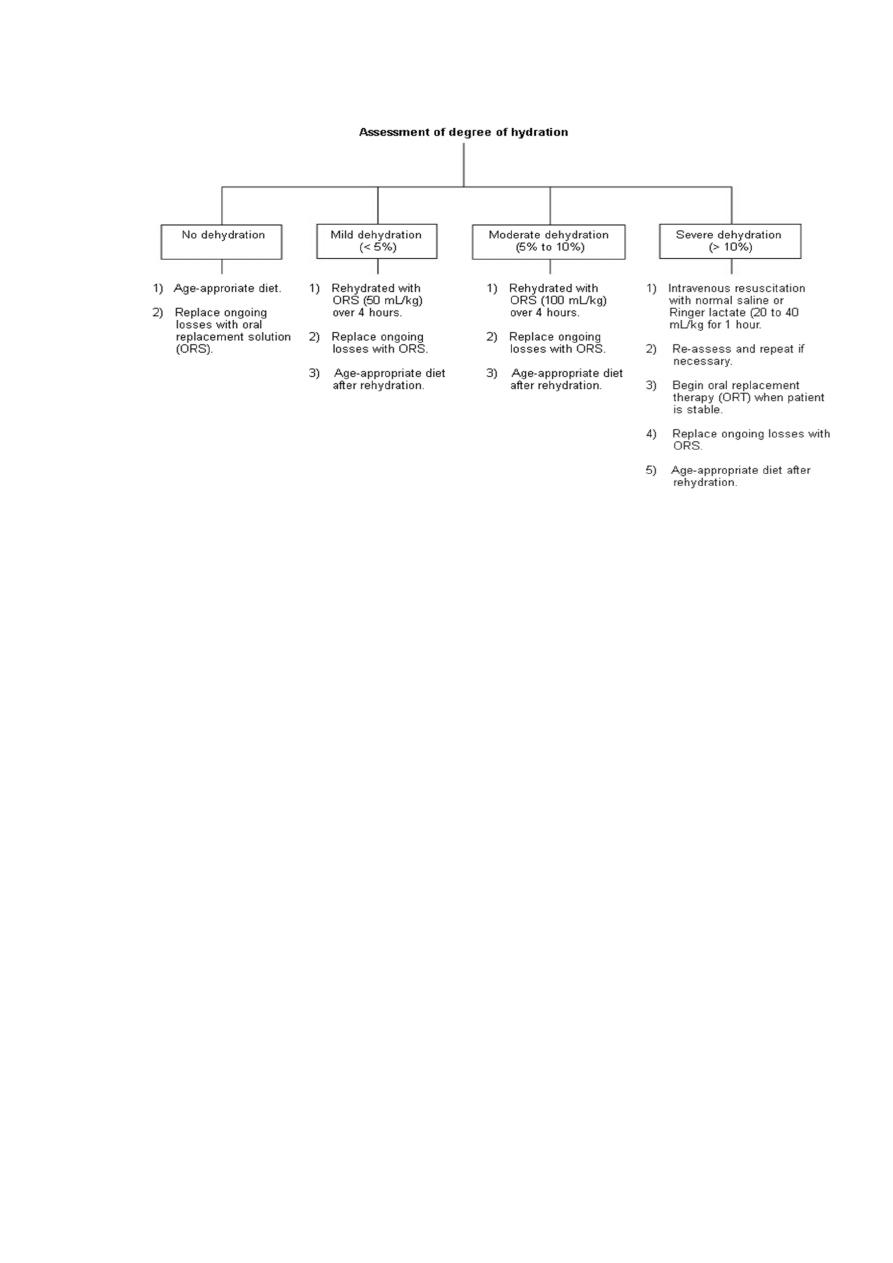
Rehydration protocols:
1. Mild:
* 50cc/kg of ORS plus replacement over 4 hours. begin with 5cc aliquots q12 min with
volumes increasing as tolerated.
2. Moderate:
* 100cc/kg of ORS plus replacement over 4 hours, As for mild, but should be in supervised
setting (ER, office)
3. Severe:
20cc/kg of isotonic IV fluids over one hour Repeat as necessary, Continue replacement for
stools, ongoing losses can be matched at approximately 10cc/kg for each stool.
Dietary, Medical and Other Adjuvant Therapy
1.
Dietary Therapy:
All children should be returned to age appropriate diets upon initial
rehydration.
“Resting the gut” is an inappropriate approach; early refeeding has been
shown to reduce illness duration, improve nutritional outcomes and
decrease changes to intestinal permeability
Diluting formula has been shown to prolong symptoms and delay
nutritional recovery
Lactose free formulas are largely unnecessary
Foods high in simple sugars should be avoided due to osmotic load.(drinks,
juice, gelatin desserts, etc)
2.Medications:
*Antidiarrheals:
(e.g. loperamide, opiates, bismuth subsalicylate) are not
recommended for use in AGE. Opiates are contraindicated, and the others
have limited scientific evidence to outweigh risks)
**
Antiemetics:
➢
currently antiemetics are not recommended in the treatment of AGE. Though some
clinical studies have demonstrated that ondansetron can decrease vomiting and
hospitalization.
*** Probiotics:
➢
Normally, gut flora (saccharolytic bacteria) ferment dietary carbohydrates
that have not been absorbed. Diarrhea reduces fecal flora. Probiotics (e.g.
Lactobacillus GG) alter the composition of gut flora and assist in restoring
normal gut function. More studies are supporting the use of probiotics,
specifically Lactobacillus GG, as an adjuvant therapy in AGE.
Complications Of Gastrointeritis
Dehydration and electrolyte imbalance:
This is the most common
complication. If a child drinks well then it is unlikely to occur,
Occasionally, if a child becomes severely dehydrated, they need to be
admitted to hospital for fluid to be given directly into a vein.
Haemolytic-uraemic syndrome (HUS):
This is is rare. It is a disorder that
can lead to renal failure. Most cases occur following a gut infection caused
by a bacteria called E. coli O157.
Haemolytic uraemic syndrome
should be considered in any child with bloody
diarrhoea, pallor, and poor urine output.
Haemolytic uraemic syndrome characterised by:
➢
acute renal impairment
➢
Thrombocytopenia, reticulocytosis
➢
microangiopathic haemolytic anaemia.
Reactive complications:
Rarely, other parts of the body
'react' to an infection that occurs in the gut. This can
cause symptoms such as arthritis, skin inflammation, eye
inflammation (conjunctivitis and uveitis).
Spread of infection
to other parts of the body.
Malnutrition:
mainly a risk in developing countries.
Persistent diarrhoea syndromes
may rarely develop.
Irritable bowel syndrome
is sometimes triggered by a
bout of gastroenteritis.
!
