
Abdominal Examination
Tabarek Yeshar
Ali Abdulazeem
2015/2016

Exposure:
- From 5
th
intercostal space (the nipple) to knee with cover over genitalia, Because some
intra-abdominal organs lie behind thoracic cage which includes liver, spleen, gastro-
oesophageal sphincter and part of the stomach.
- 5
th
intercostal space is the level of the diaphragmatic dome.
- The facial covering of the abdomen extends to mid-thigh.
- During general examination concentrate on anemia jaundice and supraclavicular lymph
node enlargement
To contract the abdominal muscles:
▪
Ask the patient to lift his head and shoulders off the couch.
▪
Lift the patient’s heels yourself and then ask the patient to hold them in that
position.
The anatomical names of these nine regions are:
▪
The epigastrium;
▪
The right hypochondrium;
▪
The left hypochondrium;
▪
The umbilical region;
▪
The right lumbar region;
▪
The left lumbar region;
▪
The hypogastrium or suprapubic region;
▪
The right iliac fossa;
▪
The left iliac fossa.
Inspection:
- From the end of the bed
1. Contour:
scaphoid
normal
distended (uniform or asymmetrical)
- Note the lateral border of flanks:
distended
concave (normal)
2. Skin:
redness, pigmentation
scar, striae
dilated veins
nodules branding
marks tattoos

- Redness:
a.
Over lump local inflammation Around umbilicus in acute abdomen acute
haemorrhagic pancreatitis (Cullen's sign)
.
b.
Branding marks chronic or long term pain
.
- Hard SC nodules:
secondary separate of malignancy to skin.
- Dilated veins:
a.
around the umbilicus with the centrifugal follow suggest portal hypertension (caput
medusae).
b.
Vertical femoraxillary veins seen in the vena cava obstruction.
- Scar of previous operation:
- Ask detail for routine of previous operation.
- Scar at McBurney Point grid-iron incision (may suggest appendicectomy).
- The scar on the right costal margin (may suggest cholecystectomy).
- Lower median scar (suprapubic may suggest cystectomy) or prostectomy.
- Widening of scar wound: infection after previous operation
.
3. Umbilicus:
position
shape (eversion or stretching)
hernia
- Position:
- Normally Midway between xiphoid process to the tip of symphysis pubis.
- Displaced upward by lumps arising from pelvis.
- Displaced downward in ascitis (Tanyol sign)
- Shape:
▪
Transversely stretched in ascitis (laughing Umblicus).
▪
Everted in umbilical hernia.
- Hernia:
Ask the patient to cough, note visible expansile impulse (umbilical or para-umbilical
hernia)
4. Movement:
movement during respiration
visible pulsation
visible peristalsis

Movement during respiration:
Note abdominal wall movement with respiration and
compare it with chest expansion
a.
Thoraco-abdominal common in females.
b.
Abdominal thoracic common in males
.
c.
Absence of abdominal movement during respiration and only chest expansion is
present generalized peritonitis
.
d.
Localized portion of abdomen immobile with respiration localized peritonitis
.
- If there is visible lump observed as it moves up and down with respiration:
a.
Lumps connected to the diaphragm (from liver, gallbladder, spleen and stomach)
move well with respiration.
b.
Renal lumps move slightly.
c.
Retro-peritoneal lumps and intra-abdominal lamps are not connected to the
diaphragm, they don't move with the respiration.
Visible pulsation (epigastric pulsation):
Its maybe
a.
abdominal aortic aneurysm.
b.
Transmitted pulsation from aorta through a mass (CA stomach or pancreas).
c.
Normal in thin patients.
d.
Right ventricular hypertrophy.
Visible peristalsis:
- Peristaltic waves in epigastrium moving from left to right is characteristic sign of pyloric
stenosis.
- Distended coils of intestine with visible peristalsis suggest intestinal obstruction.
Palpation
:
- Warm your hands by rubbing them against each other before palpation, because cold
hands are noisy to the patient and also may induce spasm of the abdominal muscles.
1) Superficial palpation:
for
superficial tenderness
superficial masses
- Start to palpation from non-tender area, and usually from left iliac fossa, anticlockwise,
palpating each quadrant with noticing patient's face, Note if there is any:

- Tenderness:
localize the exact site
- Gardening:
which is contraction of abdominal muscle on pressure voluntarily guarding
due to fear or oversensitivity disappear by directing the patient away from palpation
- Rigidity:
substation contraction even without palpation which suggests peritonitis (bored
like
).
- Rebound tenderness:
release tenderness that is acute pain felt on releasing hand after the
pressure, suggests inflammation of parietal peritoneum due to underlying inflamed organ
(In the presence of intestinal obstruction rebound tenderness suggests strangulation).
2) Deep palpation:
- The liver:
To feel the liver, place your right hand transversely and flat on the right side of the
abdomen at the level of the umbilicus, parallel with the right costal margin. Then ask the
patient to take a deep breath, if liver is enlarged it will move downward and touch radial
side of your index finger, If nothing is the felt repeat the process after moving your hand
upwards inch by inch until the costal margin is reached.
- Normal liver is not palpable except in paediatric age group
- The spleen:
Place your right hand on right iliac fossa with fingers parallel to left costal margin ask the
patient to take a deep breath, if nothing abnormal is felt move your hand in stage toward
the left costal margin.
- normal spleen is not palpable
- The kidney:
Normal kidney is impalpable except in very thin patients
- For right kidney:
a.
Place your left hand behind patient's right loin and lift it forward and place your
right hand on the abdomen;
b.
Palpate with both hands
.
- For left kidney:
place left hand behind left loin and place right hand on the anterior
abdomen
.
Balloting:
enlarged kidney can be pushed back and forth between anterior and posterior
hands.
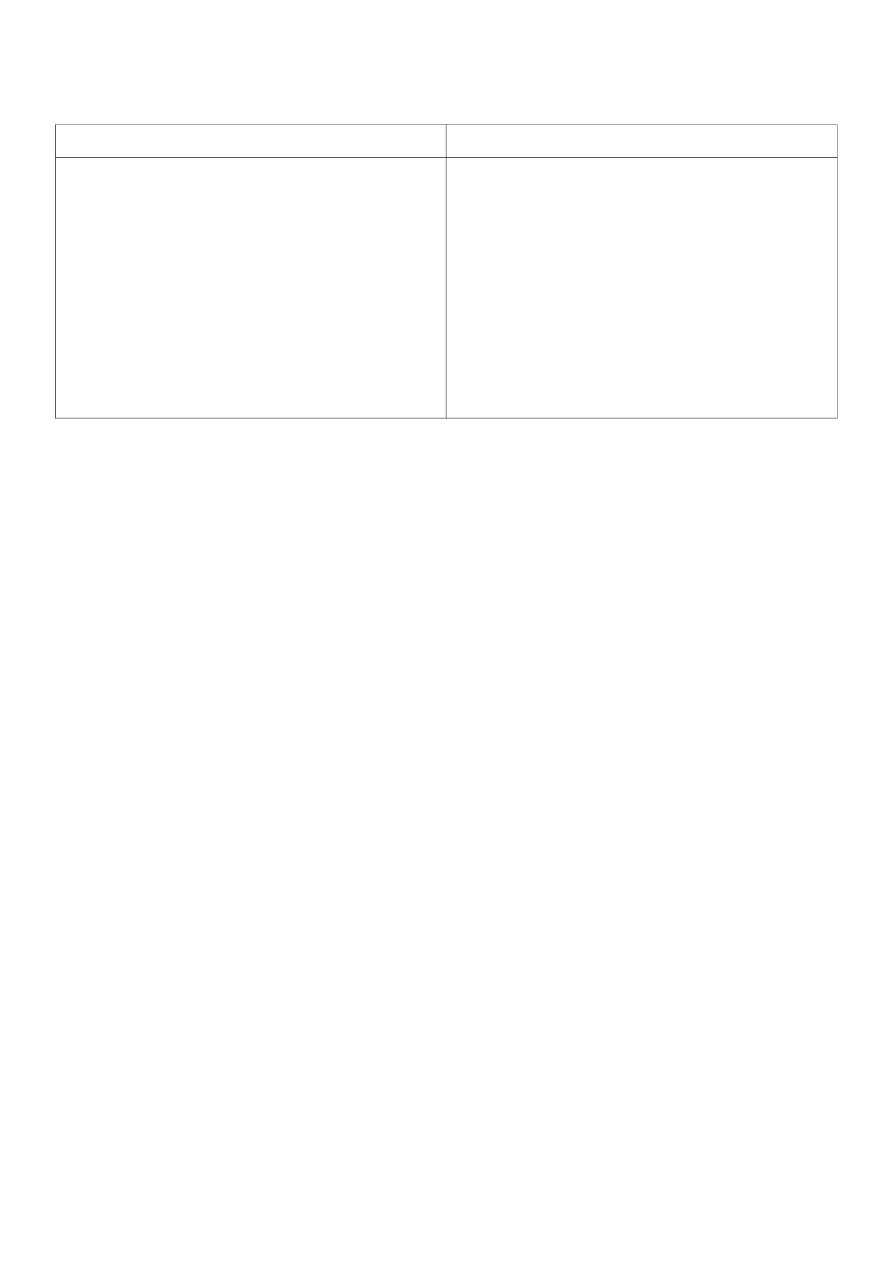
How to differentiate kidney enlargement from spleenic enlargement?
Kidney
Spleen
Has no notch
You can get above it
Enlarges
vertically down to left iliac
fossa.
Resonant on percussion because of
loops of bowel colon covering it it
Can be felt bimanually and be balloted
Has the spleenic notch
You cannot get above it
Enlarged obliquely toward right iliac
fossa
Dull on percussion
Cannot be felt bimanually or be
ballotable
If there is a lump:
First:
determine whether it is Intra-abdominal or extra-abdominal (within abdominal wall),
By either:
- By asking the patient to raise his head against the resistance of your hand usually used in
female or in conscious patient.
- Or raising the lower limbs by flexion of hip usually used in males or an unconscious
patient.
- Both manoeuvres contract abdominal muscles, so if lump disappeared or become less
prominent, it is intra abdominal mass.
Second:
Lump examination: SET CFR DPB
- Rise in temperature of the lump suggests local inflammation
Percussion:
-If abdomen is distended there is to see if there is
ascitis
by:
1. Transmitted thrill (fluid thrill):
Ask the patient or an assistant to press his ulnar border
of his hand vertically over the midline, Keep your left hand gently over one side of the
swelling and tap the opposite side with the right hand, If there is a fluid then the left hand
will feel thrust after a small delay following the tap with the right hand
.
2. Shifting dullness:
is
more sensitive, Percuss from umbilicus to the flanks, if there is
dullness in the flanks keep your finger on the point of dullness and roll the patient to the
opposite side wait for 60 seconds and percuss again, if it becomes resonant, this means

that the presence of fluid in abdomen is confirmed.
- Percuss for liver Span
1.
Starting in the midclavicular line at about the 3rd intercostal space, lightly percuss
and move down.
2.
Percuss inferiorly until dullness denotes the liver's upper border (usually at 5th
intercostal space in MCL).
3.
Resume percussion from below the umbilicus on the midclavicular line in an area of
tympany.
4.
Percuss superiorly until dullness indicates the liver's inferior border.
5.
Measure span in centimeters (the distance between upper and lower border of liver).
6.
Normal liver span is 6 – 12 cm.
- May be useful for rebound tenderness
Auscultation:
For
1) bowel sound
:
- The best site to hear it is at McBurney's point, because it is a site of narrow-wide tube
junction (lower ileum cecum).
- You should keep your stethoscope for at least 2 minutes on each side.
- Normal bowel sound is low pitch (gurgles), every 30 seconds one bowel sound.
- High pitch, more frequent (intestinal obstruction, hypermobile and even irritable bowel
syndrome).
- Tingling (water coming down a tube) paralytic ileus best heard on bell.
2) Bruits:
- in abdominal aorta by placing stethoscope above umbilicus in midline.
- For renal artery stenosis, between umbilicus and xiphisternum lateral to midline.
3) Venus hump:
if there is a large hemangioma in liver, you can hear a venus hump, which is indication of
hyperdynamic circulation in the area.
4) Can be useful for organomegaly
Never forget to examine:
1) The back:

Note if there is kyphosis, scolosis, hyphoscohosis, lordosis or any abnormalities of skin or
visible swelling.
- Palpate the spine and renal angles for any tenderness.
- Renal angle the space between 12 slip and edge of erector spine (sacrospinalis) muscle.
2) External genitalia and inguinal orifices.
3) Supraclavicular lymph nodes
: particularly the left one which is enlarged in case of
abdominal malignancy virchow's node
(troisier's sign)
.
4) Per-rectal examination.
5) Per-vaginal examination.
Additional Notes:
The anatomical positions of appendix
:
▪ Retrocaecal 74%
▪ Pelvic 21%
▪ Paracaecal 2%
▪ Subcaecal 1.5%
▪ Preileal 1%
▪ Postileal 0.5%
Acute Appendicitis signs:
1.
The pointing sign:
The patient is then asked to point to where the pain began and
where it moved.
2.
Tenderness:
McBurney’s point.
3.
Rebound tenderness
.
4.
Rovsing’s sign:
Deep palpation of the left iliac fossa may cause pain in the right
iliac fossa.
5.
The psoas sign:
the patient, often a young adult, will lie with the right hip flexed for
pain relief.
6.
The obturator test:
Spasm of the obturator internus is sometimes demonstrable
when the hip is flexed and internally rotated. If an inflamed appendix is in contact
with the obturator internus, this manoeuvre will cause pain in the hypogastrium (the
obturator test; Zachary Cope).

Abdominal hernia
A
hernia
is the protrusion of an organ through its containing wall.
The common ones in order of frequency in adult life are:
▪
Inguinal
▪
Umbilical
▪
Incisional
▪
Femoral
▪
Epigastric.
In childhood, umbilical hernia is more common than inguinal hernia.
Rarities:
▪
Spigelian
▪
Obturator
▪
Lumbar
▪
Gluteal
physical signs and diagnosis:
▪
Site: they occur at congenital or acquired weak spots in the abdominal wall;
▪
most herniae can be reduced;
▪
most herniae have an expansile cough impulse.
- The last two signs may be absent, especially if the hernia is tightly constricted at its neck.
Examination of umbilical, incisional and femoral hernias:
Position:
Examine on supine position
- Examine as lump
Inguinal herniae:
An inguinal hernia is the protrusion of part of the contents of the abdomen through the
inguinal region of the abdominal wall.
Anatomy:
!
Examination of an inguinal hernia:
Position:
Ask the patient to stand up
Inspection:
(in general examine as lump)
- site and shape of the lump
- Dose the lump extend down into the scrotum?
- Is there are any other scrotal swellings?
- Are there any swellings on the ‘normal’ side?
Palpation:
First:
Feel from the front:
1)
Examine the scrotum and its contents. It is not unusual to find an epididymal cyst or a
hydrocele as well as a hernia.
2)
In men, first decide if the lump is a hernia or a true scrotal lump by examining its upper
edge:
▪
If you can ‘get above it’ (i.e. feel its upper edge between your thumb and index
finger and a normal spermatic cord above it), it must be a scrotal swelling and not a
hernia.
▪
If you cannot feel the upper edge of the lump because it passes into the inguinal
canal, it is likely to be a hernia
Second:
Feel from side:
- Stand at the side of the patient, on the same side as the hernia. Place one hand in the
small of the patient’s back to support him, and your examining hand on the lump with
your fingers and arm roughly parallel to the inguinal ligament.
1) Ascertain:
▪
Position
▪
Temperature
▪
Tenderness
▪
Shape
▪
Size
▪
Tension
▪
Composition (solid, fluid, or gaseous)
▪
Reducibility.
2) Is the swelling reducible?
▪
If the hernia can be held reduced only by pressure over the external inguinal ring, it
is a direct inguinal hernia.
▪
If it can be controlled by pressure over the internal ring, it is an indirect inguinal
hernia.
3) Expansile cough impulse:
Compress the lump firmly with your fingers, then ask the
patient to cough:
▪ If the swelling becomes tense and expands with coughing, it has a ‘cough impulse’;
▪ Movement of the swelling without expansion or an increase in tension is not a
cough impulse.
4) Direction of movement of the swelling after removal of the hand:
▪
A reappearing indirect hernia will seem to slide obliquely downwards along the line
of the canal;
▪
Direct hernia will project directly forwards.
Three finger test:
to distinguish between direct and indirect inguinal hernias
a.
Reduce the lump;
b.
Place three fingers on the internal inguinal opening, 1.5 cm above midway between
the superior anterior iliac spine and the pubic tubercle;
c.
Ask the the patient to cough or to strain;
d.
If the lump reappears, it is direct inguinal hernia;
e. If it doesn't, it's indirect inguinal hernia.
Third:
Feel the other side
Percuss and auscultate the lump:
If there is gut in the sac, it may be resonant and
there may be audible bowel sounds.
Don't forget to examine the abdomen:
Look particularly for anything that may be raising the intra-abdominal pressure, such as a
large bladder, an enlarged prostate, ascites, chronic intestinal obstruction or pregnancy.
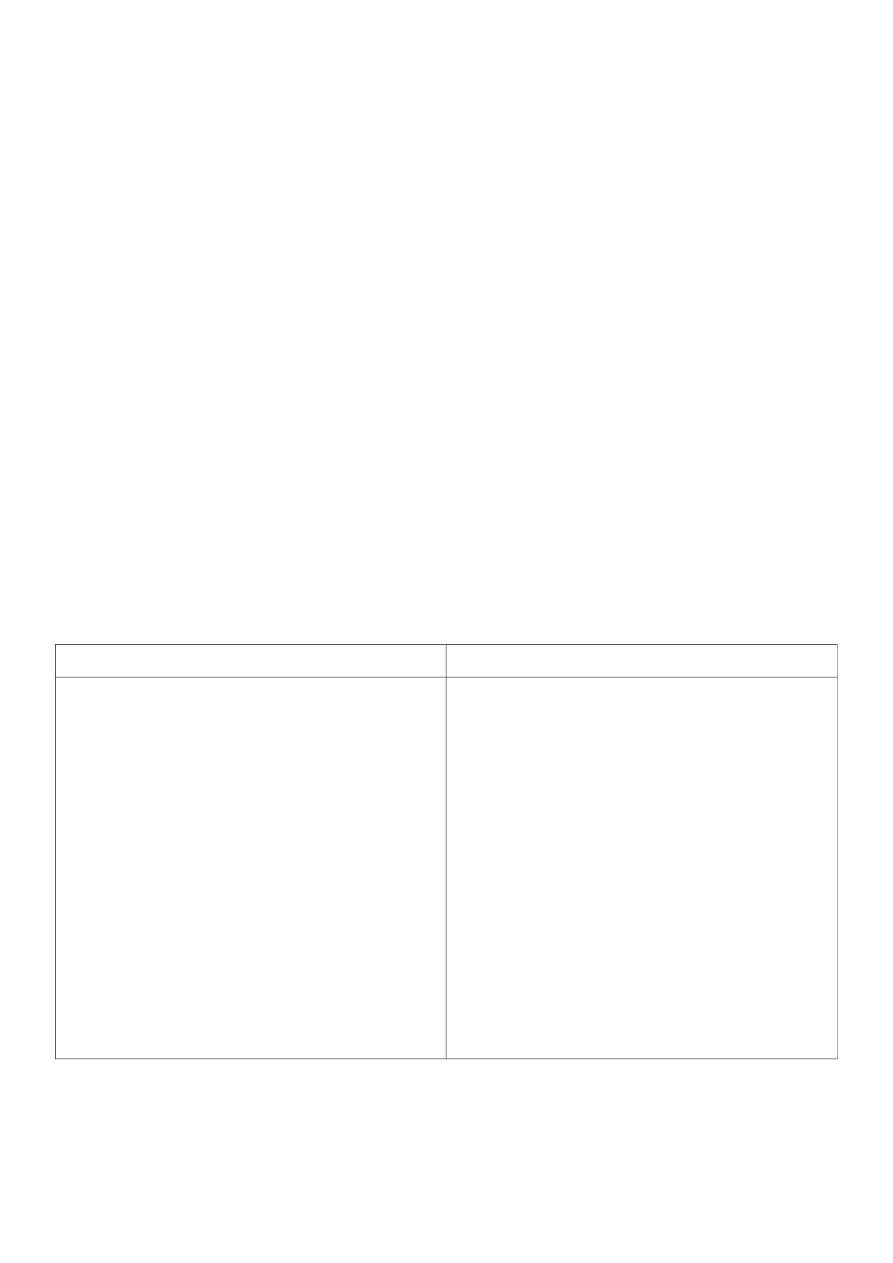
Features of an indirect inguinal hernia
Features of a direct inguinal hernia
▪
Can (and often does) descend into the
scrotum
▪
Reduces upwards, then laterally and
backwards
▪
Controlled, after reduction, by
pressure over the internal inguinal ring
▪
The defect is not palpable, as it is
behind the fibres of the external
oblique muscle
▪
After reduction, the bulge reappears in
the middle of the inguinal region and
then flows medially before turning
down to the neck of the scrotum
▪
Does not (hardly ever) go down into
the scrotum
▪
Reduces upwards and then straight
backwards
▪
Not controlled, after reduction, by
pressure over the internal inguinal ring
▪
The defect may be felt in the
abdominal wall above the pubic
tubercle
▪
After reduction, the bulge reappears
exactly where it was before
▪
Uncommon in children and young
adults
The differential diagnosis of inguinal hernia:

▪
Femoral hernia
▪
Vaginal hydrocele
▪
Hydrocele of the cord or the canal of Nuck
▪
Undescended testis
▪
Lipoma of the cord
