
The placenta & fetal membranes

• ^ placenta is ^ organ that facilitates nutrient & gas exchange
between ^ maternal & fetal compartments.
• As ^ fetus begins ^ 9
th
week of development, its demands for
nutritional & other factors increase, causing major changes in
^ placenta.
• Foremost among these is an increase in surface area between
maternal & fetal components to facilitate exchange.
• ^ disposition of fetal membranes is also altered as production
of amniotic fluid increases.

Changes in ^ trophoblast
• ^ fetal component of ^ placenta derived from ^ trophpoblast
& extraembryonic mesoderm (chorionic plate).
• ^ maternal component is derived from ^ uterine
endometrium.
• By ^ beginning of ^ second month, ^trophoblast characterized
by a great no. of secondary & tertiary villi, which give it radical
appearance.
• Stem (anchoring ) villi extend from ^ chorionic plate to ^
cytotrophoblast shell.
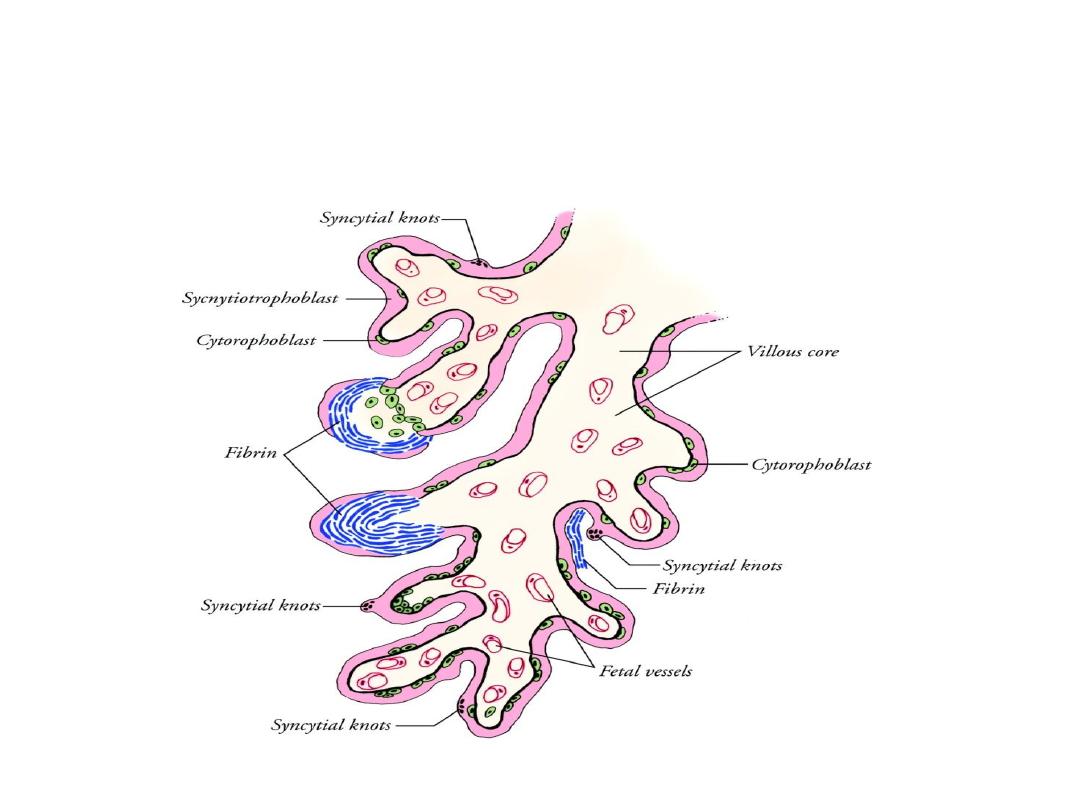
• ^ surface of ^ villi is formed by ^ syncytium resting on a layer
of cytotrophoblastic cells that in turn cover a core of vascular
mesoderm.
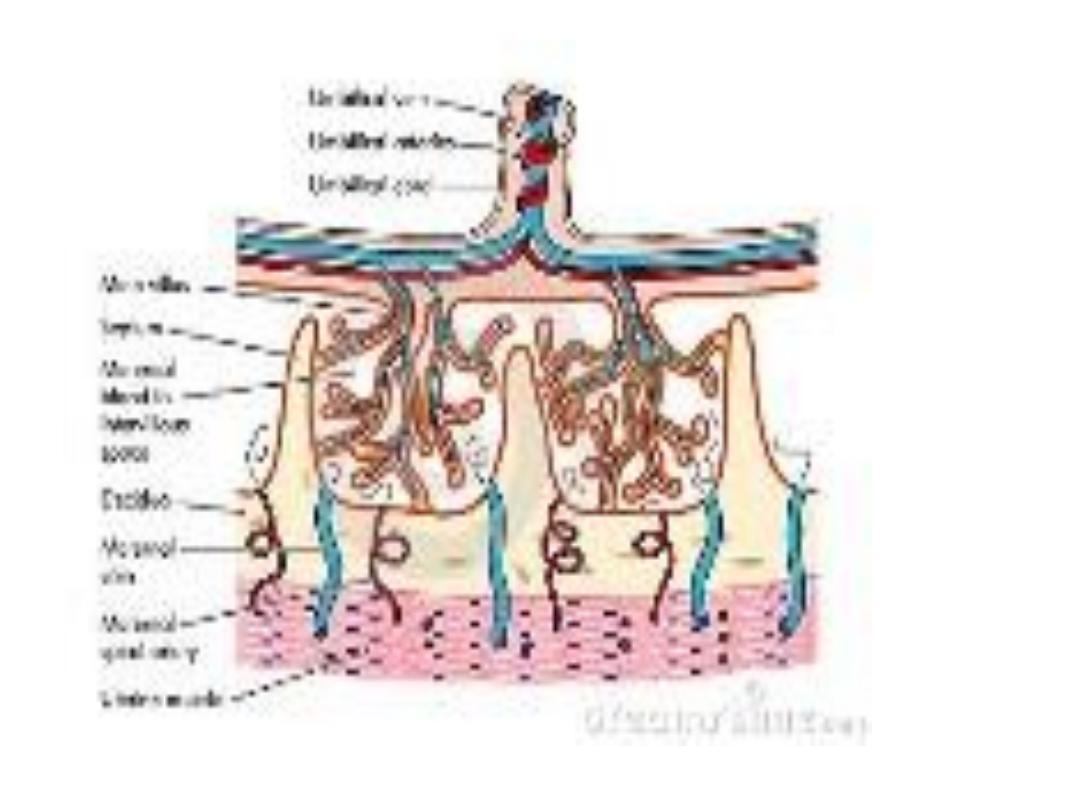

• ^ capillary system developing in ^ core of ^ villous stems soon
comes in contact with ^ capillaries in chorionic plate &
connecting stalk, thus giving rise to -extraembryonic
vascular system.
• Maternal blood is delivered to ^ placenta by spiral arteries in
^ uterus.
• Erosion of these maternal vessels to release blood into
intervillous spaces, is accomplished by
endovascular invasion
by cytotrophoblast cell, this process needs ^ cytotrophoblast
cells to undergo an epithelial-endothelial transition.
• This invasion transforms these vessels from small-diameter
high-resistance to large-diameter, low-resistance vessels that
can provide increased amount of maternal blood to
intervillous space.
• During ^ following months, numerous small extensions extend
as
free villi
into ^ surrounding
lacunar or intervillous space.
Initially, these newly formed free villi are primitive, but by ^
beginning of 4
th
month, cytotrophoblast cells & connective
tissues disappear, ^ syncytium & endothelial wall of blood
vessels are ^ only layers that separate ^ maternal & fetal
circulations.
• Frequently, ^ syncytium becomes very thin, & large pieces
may break & drop into ^ intervillous blood lakes, these pieces
known as
syncytial knots
enter ^ maternal blood & usually
degenerates without causing any symptoms.
• Disappearance in ^ cytotrophoblastic cells progress from
smaller to larger villi, although some persist in ^ large villi but
they do not participate in ^ exchange between ^ 2
circulations.
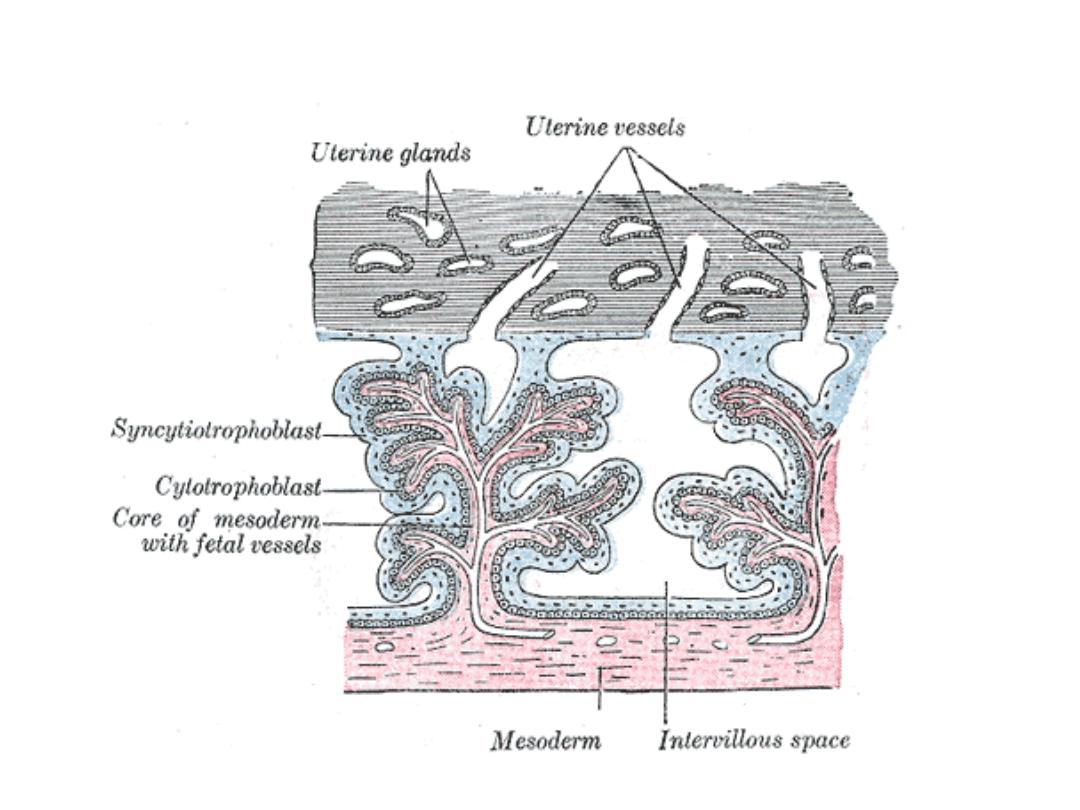

Structure of ^ placenta
• By ^ beginning of ^ 4
th
month, ^ placenta has 2 components:
• (1) a
fetal portion,
formed by ^ chorion frondosum&
• (2) a
maternal portion,
formed by ^ decidua basalis.
• On ^ fetal side, ^ placenta is bordered by ^
chorionic plate,
on
its maternal side, it is bordered by decidua basalis (
decidual
plate).
In ^
junctional zone,
trophoblast & decidual cells
intermingle, this zone characterized by syncytial & decidual
giant cells, is rich in amorphous extracellular material.
• By this time most cytotrophoblast cells degenerated.

• Between ^ chorionic plate & decidual plate are ^ intervillous
spaces, which are filled with maternal blood, these spaces are
derived from ^ lacunae in ^ syncytiotrophoblast & are lined
with syncytium in of fetal origin.
• ^ Villous tree grow into ^ intervillous blood lakes.
• During ^ 4
th
& 5
th
month, ^ decidua forms a no. of decidual
septa, which project into intervillous spaces but do not reach
^ chorionic plate.
• These septa have a core of maternal tissue, but their surface
is covered by a layer of syncytial cells, so that at all times, a
syncytial layer separates maternal blood from fetal tissues.
• As a result of this septum formation, ^ placenta is divided into
a no. of compartments
(cotyledons)
.

• Because ^ decidual septa do not reach ^ chorionic plate,
contact between intervillous spaces in ^ various cotyledons is
maintained.
• As a result of continuous growth of ^ fetus & expansion of ^
uterus, ^ placenta also enlarges.
• Its increase in surface area roughly parallels that of expanding
uterus, & throughout pregnancy, it covers approximately 15%
-30% of ^ internal surface of ^ uterus.
• ^ increase in thickness of ^ placenta results from arborization
of existing villi& it is not caused by further penetration into
maternal tissues.
Full-term placenta
• At full-term, ^ placenta is discoid with a diameter of 15-25cm,
3cm thick, & weighs about 500-600 gm.
• At birth, it is torn from ^ uterine wall approximately 30
minutes after birth of ^ child, is expelled from ^ uterine cavity
as ^ afterbirth.
• When ^ placenta is viewed from ^ maternal side, 15-20
slightly bulging cotyledons covered by a thin layer of decidua
basalis, are clearly recognizable.
• Grooves between ^ cotyledons are formed by decidual septa.
• ^ fetal surface of ^ placenta is covered entirely by ^ chorionic
plate. A no. of large arteries & veins, ^
chorionic vessels,
converge toward umbilical cord. ^ chorion, in turn, is covered
by ^ amnion.
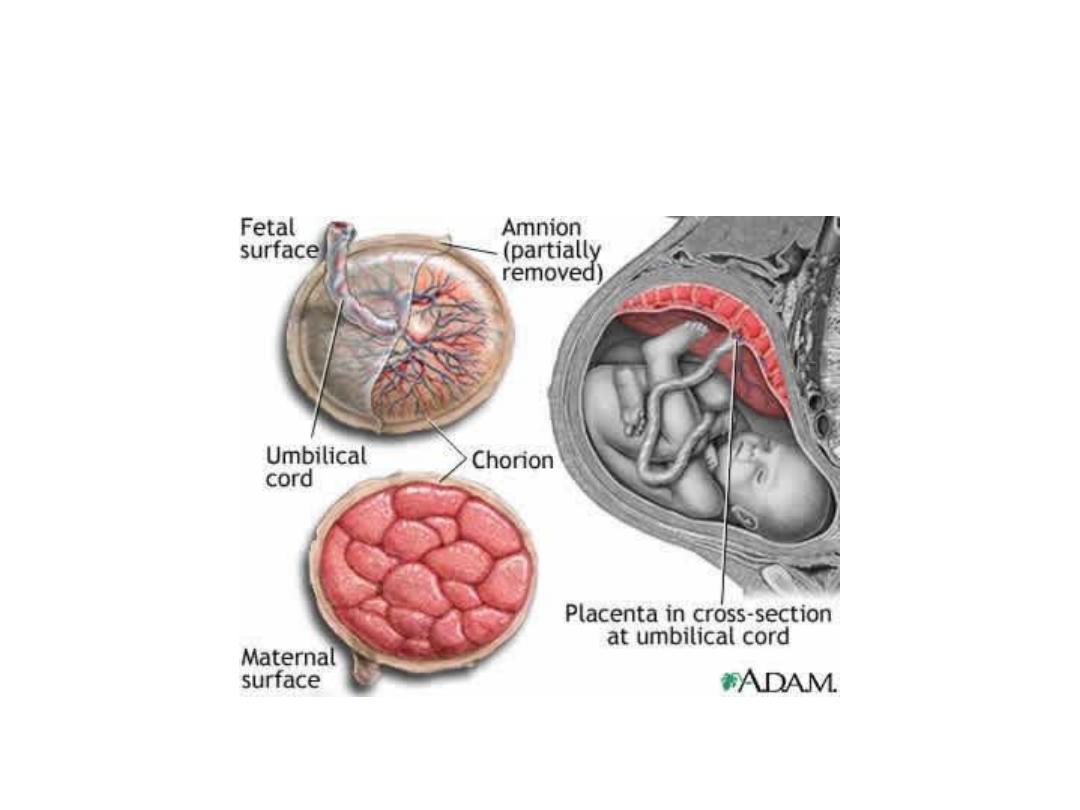
• Attachment of ^ umbilical cord is usually eccentric &
occasionally even marginal, rarely it inserts into ^ chorionic
memb. Outside ^ placenta velamentous insertion).
Circulation of ^ placenta
• Cotyledons receive their blood through 80-100 spiral arteries
that pierce ^ decidual plate & enter ^ intervillous spaces,
pressure in these arteries forces ^ blood deep into ^ inter
villous spaces & bathes ^ numerous small villi in oxygenated
blood.
• As ^ pressure decreases, blood flows back from ^ chorionic
plate toward ^ decidua, where it enters ^ endometrial veins.
^ placental membrane:
separates maternal & fetal
blood is initially composed of 4 layers:
1-endothelial lining of fetal vessels.
2- ^ connective tissue in ^ villous core.
3- cytotrophoblastic layer.
4- ^ syncytium.
From ^ 4
th
month on ^ placental memb. thins because ^
endothelial lining of ^ vessels come in direct contact with ^
syncytium (increasing in rate of exchange).
Sometimes it is called (placental barrier), although it is not a
true barrier, as many substances pass through it freely.

Function of ^ placenta
• Exchange of gasses.
• Exchange of nutrients & electrolytes.
• Transmission of maternal antibodies( IgG) at 14 weeks.
• Hormonal production : BY ^ syncytium
1-progesterone, by ^ end f 4
th
month to maintain pregnancy.
2-estrogen, until just before end of pregnancy , when it reaches
maximum levels, which stimulates uterine growth & development of
mammary glands.
3- HCG, during ^ 1
st
2 months of pregnancy, which maintain ^ corpus
luteum.
4- Somatomammotropin it is a growth hormone like substance, gives ^
fetus priority on maternal blood & makes ^ mother diabetogenic.

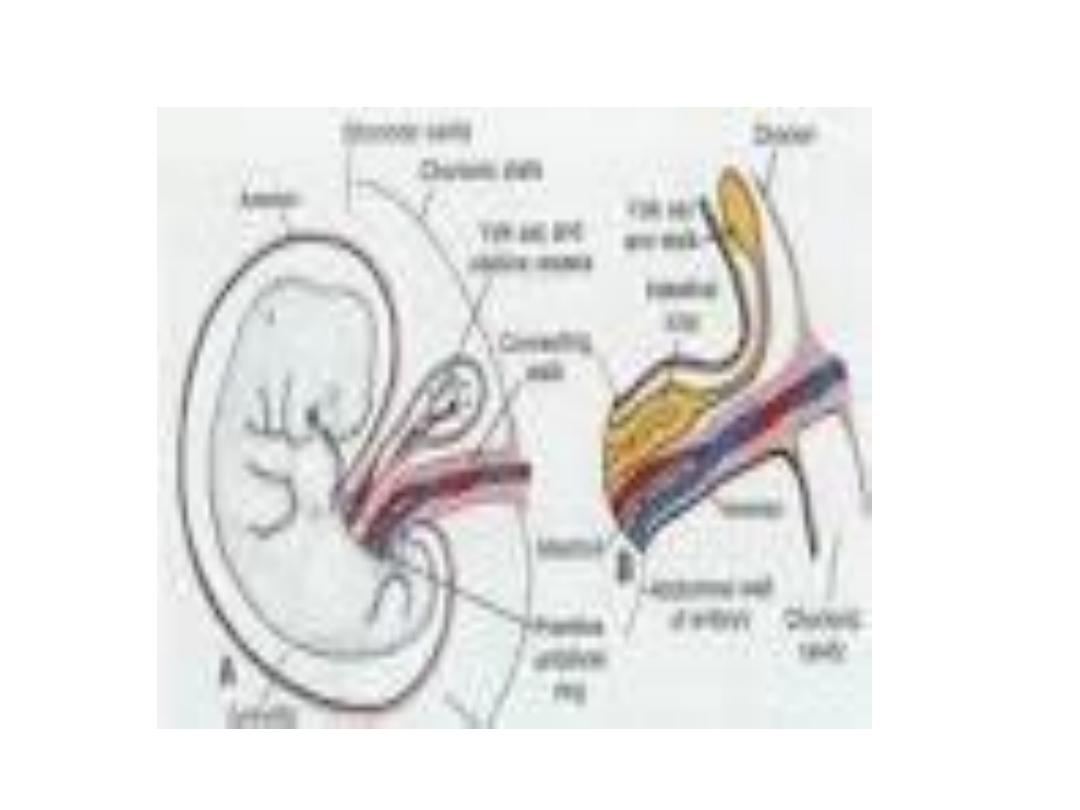
Amnion & umbilical cord
• ^ oval line of reflection between ^ amnion &embryonic
ectoderm (amnio-ectodermal junction) is ^ primitive umbilical
ring.
• At ^ 5
th
week of development ^ following structures pass
through ^ ring: (1) connecting stalk containing allantois &
umbilical vessels (2 arteries & 1 vein). (2) ^ yolk stalk (vitelline
duct) accompanied by vitellline vessels. (3) ^ canal connecting
intraembryonic & extraembryonic cavities.
• ^ yolk sac proper occupies a space in ^ chorionic cavity, that’s
between ^ amnion & chorionic plate.

• During further development ^ amniotic cavity enlarges rapidly
at ^ expense of ^ chorionic cavity, & envelops ^ connecting &
yolk sac stalks, crowding them together forming ^
primitive
umbilical cord.
• Distally ^ umbilical cord contains ^ yolk sac stalk & umbilical
vessels, while proximally, it contains some intestinal loops &
remnant of allantois.
• At ^ end of 3
rd
month, ^ amnion has expanded so that it
comes in contact with ^ chorion, obliterating ^ chorionic
cavity, && ^ yolk sac shrinks & obliterated.
• ^ abdominal cavity is temporarily too small for ^ rapidly
growing intestinal loops, & some of them are pushed into
extraembryonic space in ^ umbilical cord, this is called
physiological umbilical hernia.

• At approximately ^ end of ^ 3
rd
month, ^ loops are withdrawn into ^
body of ^ embryo, & ^ cavity in ^ cord is obliterated.
• When ^ allantois & vitelline duct & its vessels are obliterated, all
that remains in ^ cord is ^ umbilical vessels surrounded by a
protective layer
wharton’s jelly.
Amniotic fluid
Clear watery fluid produced partly by amniotic cells & is primarily
derived from maternal blood. ^ volume of amniotic fluid is replaced
every 3 hours. From ^ beginning of ^ 5
th
month, ^ fetus swallows its
own amniotic fluid 400ml/day)& urinate in it also.

Benefits of amniotic fluid
• Absorbs jolts.
• Prevents adherence of ^ embryo to ^ amnion.
• Allows for fetal movements.
