
Respiratory System

*LUNG BUDS
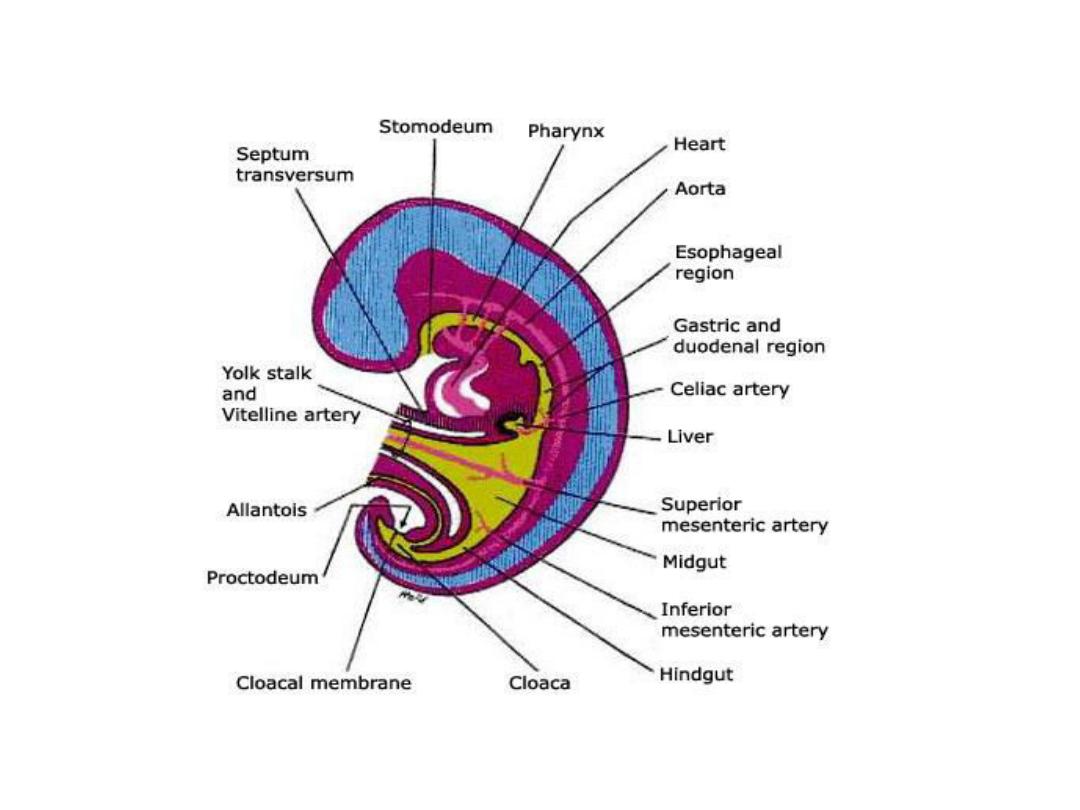
• When the embryo is approximately 4 weeks old, the respiratory
diverticulum (lung bud) appears as an outgrowing from the ventral
wall of the foregut.
• The epithelium of the internal lining of the larynx, trachea, &
bronchi, as well as that of the lungs, is entirely of endodermal
origin.
• The cartilaginous, muscular, & connective tissue components of the
trachea & lungs are derived from splanchnic mesoderm
surrounding ^ foregut.
• Initially, ^ lung bud is in open communication with ^ foregut, when
^ diverticulum expands caudally, however, 2 longitudinal ridges
separate it from ^ foregut called tracheo-esophageal ridges.

• Subsequently, when these ridges fuse to form ^
tracheoesophageal septum, ^ foregut is divided into a dorsal
portion, ^ esophagus, & a ventral portion, ^ trachea & lung
buds.
• ^ Respiratory primordium maintains its communication with
^ pharynx through ^ laryngeal orifice.


larynx
• ^ internal lining of ^ larynx from endoderm,
but ^ cartilages & muscles originate from
mesenchyme of ^ 4
th
& 6
th
pharyngeal arches.
• As a result of rapid proliferation of
mesenchyme, ^ laryngeal orifice changes in
appearance from a sagittal slit to a T-shaped
opening.
• ^ mesenchyme of ^ 2 arches transforms into:
thyroid, cricoid, & arytenoid cartilages.

• Laryngeal epithelium also proliferate resulting in
a temporary occlusion of ^ lumen. Later,
recanalization produce a pair of lateral recesses, ^
laryngeal ventricles. these recesses are bounded
by folds of tissue that differentiate into ^ false &
true vocal cords.
•
• since ^ muscle originate from 4
th
& 6
th
arches, all
laryngeal m. are innervated by vagus n. (10
th
cranial n.), superior laryngeal n. innervates
derivatives of 4
th
pharyngeal arch, while
recurrent laryngeal n. innervates derivatives of
6
th
pharyngeal arch.


Trachea, bronchi, & lungs
• During ^ separation from ^ foregut, ^ lung bud
forms ^ trachea & 2 lateral outpocketings, ^
bronchial buds.
• At ^ beginning of 5
th
week, each of these buds
enlarges to form right & left main bronchi. The
right then forms 3 secondary bronchi, & ^ left,
two. Thus foreshadowing ^ 3 lobes on ^ right
& 2 on ^ left.

• On each side of ^ foregut, expanding lung buds
are filling the space for lung; which are called
pericardioperitoneal canals.
• ^ mesoderm , which covers ^ outside of ^ lung
develops into visceral pleura. ^ somatic
mesoderm layer covering ^ body wall from ^
inside, becomes ^ parietal pleura, ^ space
between both called pleural cavity.
• During further development, secondary
bronchi divide repeatedly forming 10 tertiary
(segmental) bronchi in the Rt. Lung & 8 in Lt.
forming bronchopulmonary segments.

• By ^ end of ^ 6
th
month, approximately 17
generations of subdivisions have formed.
Before ^ bronchial tree reaches its final shape,
however, an additional six divisions form
during postnatal life.


Maturation of lung
• Up to ^ 7
th
prenatal month, ^ bronchioles divide
continuously into more & smaller canals
(canalicular phase), & vascular supply increases
steadily.
• Respiration become possible when some of the
cells of cuboidal respiratory bronchioles change
into thin, flat cells.
• These cells are intimately associated with
numerous blood & lymph capillaries, & ^
surrounding spaces are now known as primitive
alveoli, so during 7
th
month sufficient no. of
capillaries are present to guarantee adequate gas
exchange, & premature infant able to survive.

• During ^ last 2 months of prenatal life & for
several years thereafter, ^ no. of terminal sacs
increase steadily.
• In addition cells lining ^ sacs known as type1
alveolar epithelial cells. Become thinner so ^
surrounding capillaries protrude into ^ alveolar
sacs, this intimate contact will make ^ blood-air
barrier.
• Mature alveoli are not present before birth.
• Another cell type develops at ^ end of 6
th
month
called type II alveolar epithelial cells, produce
surfactant, a phospholipid- rich fluid capable of
lowering surface tension at ^ air-alveolar
interface.

• Fetal breathing movements begin before birth &
cause aspiration of amniotic fluid, these
movements are important for stimulating lung
development & conditioning respiratory muscles.
• At ^ beginning of respiration ^ lung fluid is
resorbed except for ^ surfactant coat, which
prevents ^ collapse of ^ alveoli during expiration
by reducing ^ surface tension at ^ air-blood
interface.
• So absent or insufficient surfactant in ^
premature baby causes RDS, bec. Of collapse of
primitive alveoli.

• Growth of ^ lungs after birth is primarily due
to an increase in ^ no. of respiratory
bronchioles & not to an increase in size of ^
alveoli. New alveoli are formed during ^ 1
st
10
years of postnatal life.
