
ENDOCRINE SYSTEM
By
Dr. Suhair Majeed
ENDOCRINE SYSTEM
:
The endocrine system consists of cells,
tissues, and organs that synthesize and secrete
hormones directly into blood and lymph
capillaries, endocrine glands and organs are
ductless because they do not have excretory
ducts, the cells in most endocrine tissues and
organs are arranged into cords and clumps, and
are surrounded by an extensive capillary network.
HORMONES:
Hormones produced by endocrine cells include
peptides, proteins, steroids, amino acid
derivatives, and catecholamines. Because
hormones act at a distance from the site of their
release, the hormones first enter the bloodstream
to be transported to the target organs, they
influence the structure and the programmed
function of the target organ cells by binding to
specific hormone receptors. Hormone receptors
can be located either on the plasma membrane,
cytoplasm, or nucleus of target cells.
CONT
.
Numerous organs contain individual
endocrine cells or endocrine tissues. Such
mixed(endocrine-exocrine) organs are the
pancreas, kidneys, reproductive organs of both
sexes, placenta, and gastrointestinal tract.
There are also complete endocrine organs or
glands. These include the hypophysis or pituitary
gland, thyroid gland, adrenal (suprarenal) glands,
and parathyroid glands.
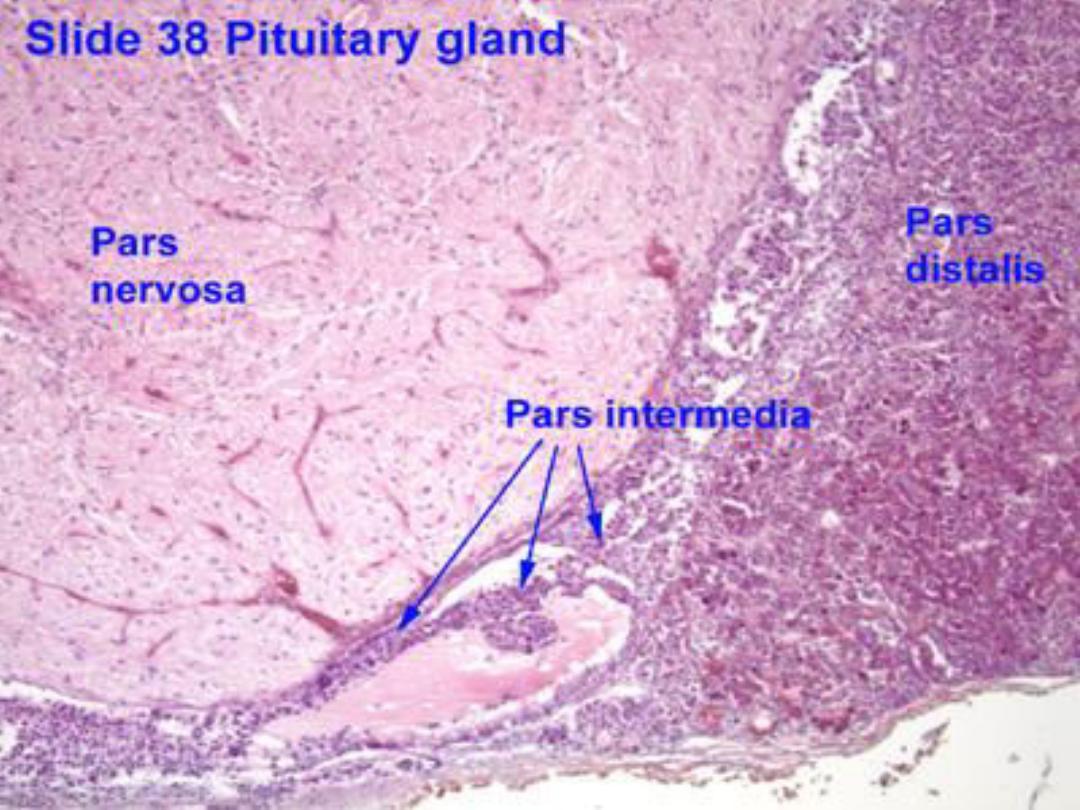
SUBDIVISIONS OF THE HYPOPHYSIS:
After development, the hypophysis rests in a
bony depression of the sphenoid bone of the
skull, called the sella turcica, located inferior to
the hypothalamus.
The adenohypophysis (anterior pituitry )has
three subdivisions:
- pars distalis,
- pars tuberalis,
- pars intermedia.
CONT.
The pars distalis is the largest part of the
hypophysis. The pars tuberalis surrounds the
neural stalk. The pars intermedia is a thin cell
layer between the pars distalis and the
neurohypophysis.
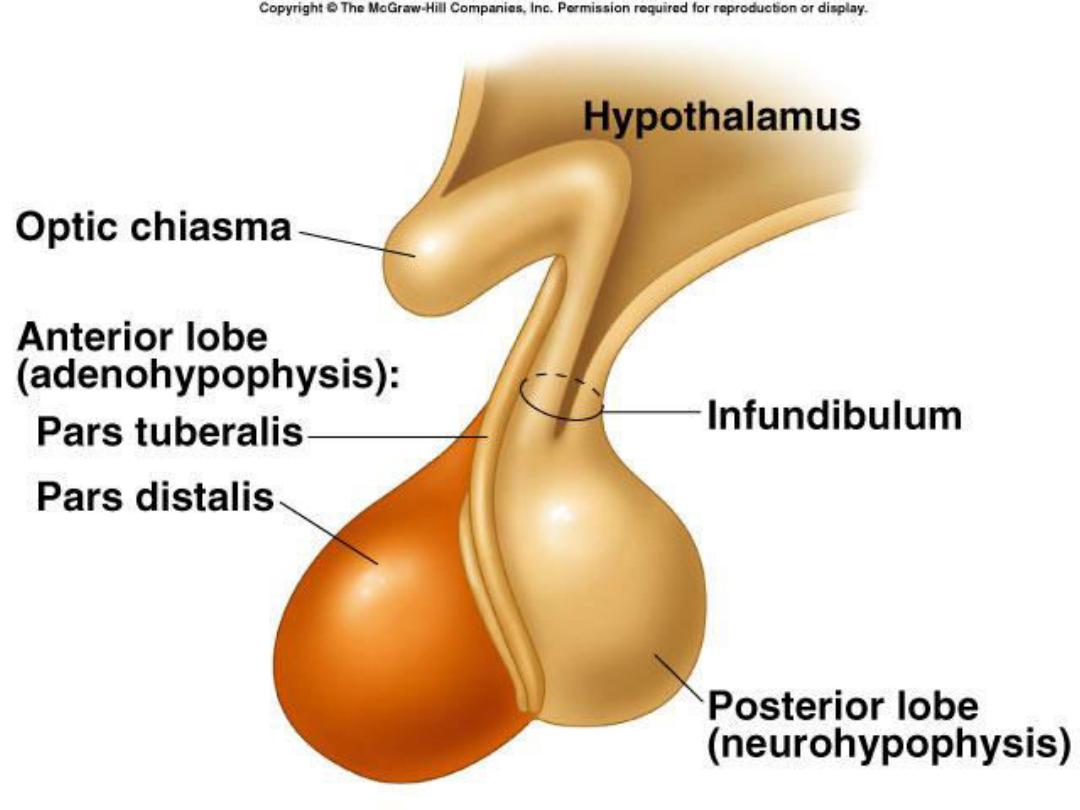
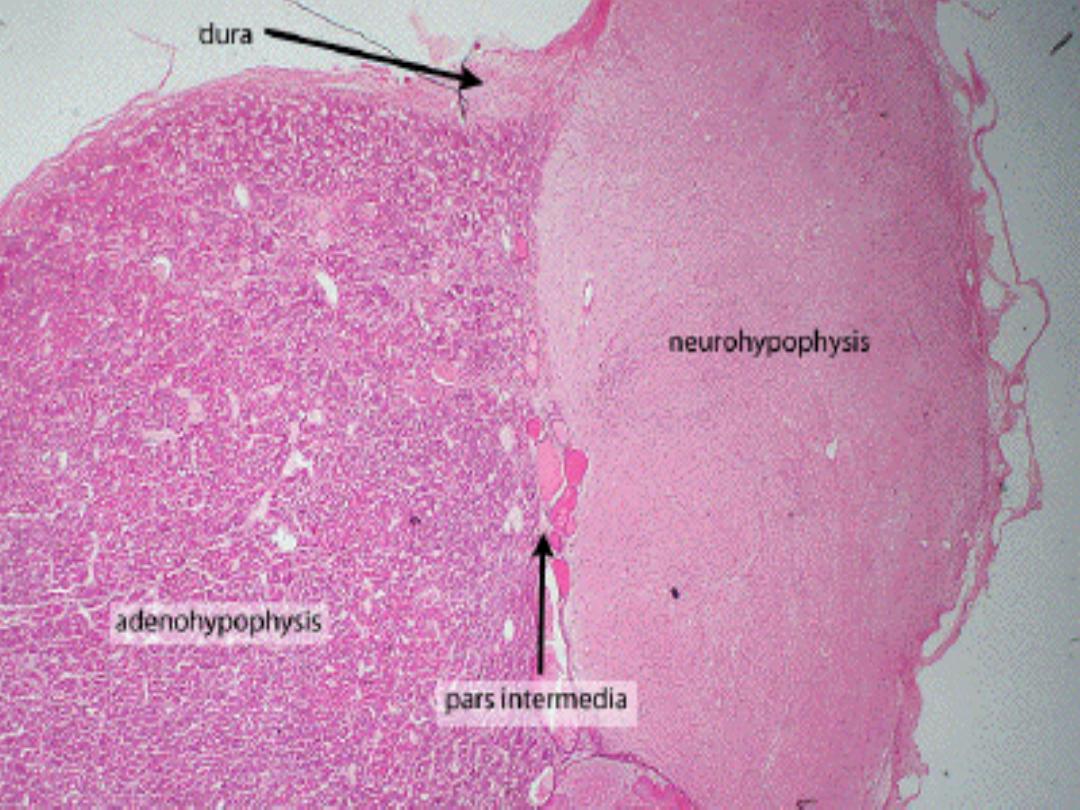
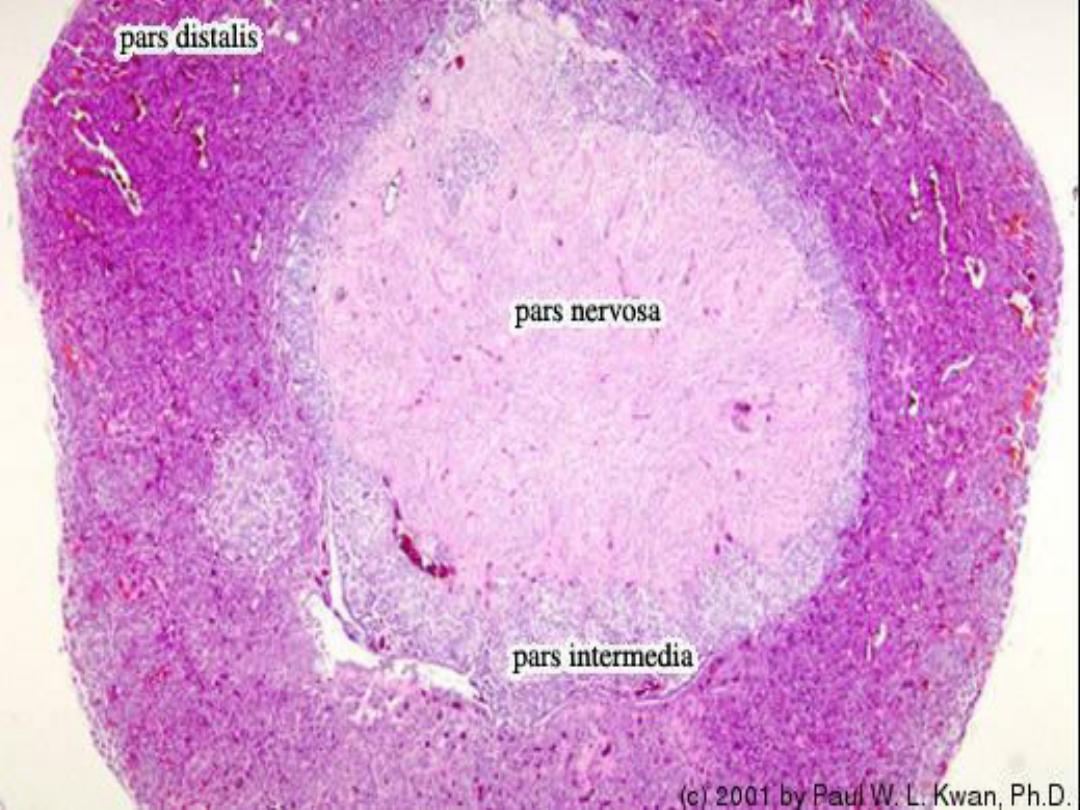
CONT.
The neurohypophysis (posterior pituitry),
situated posterior to the adenohypophysis, also
consists of three parts:
the median eminence, infundibulum, and pars
nervosa. The median eminence is located at the
base of the hypothalamus from which extends the
pituitary stalk or infundibulum, in which are
located the unmyelinated axons that extend from
the neurons in the hypothalamus.
CONT.
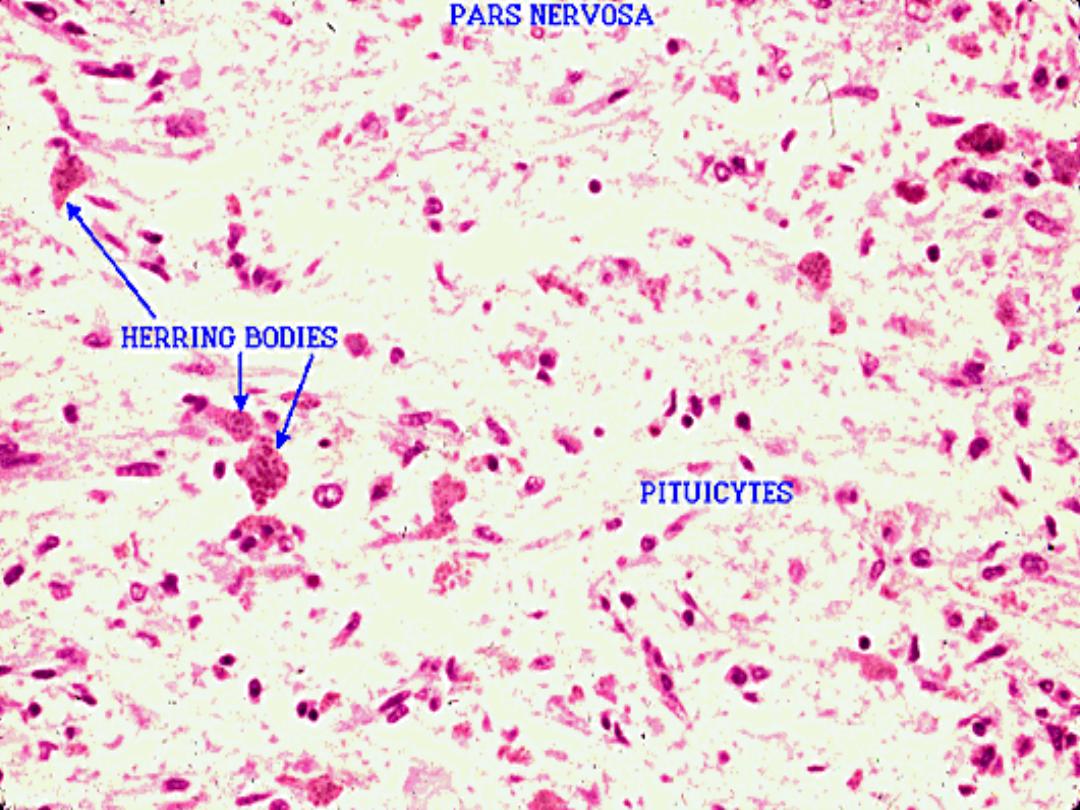
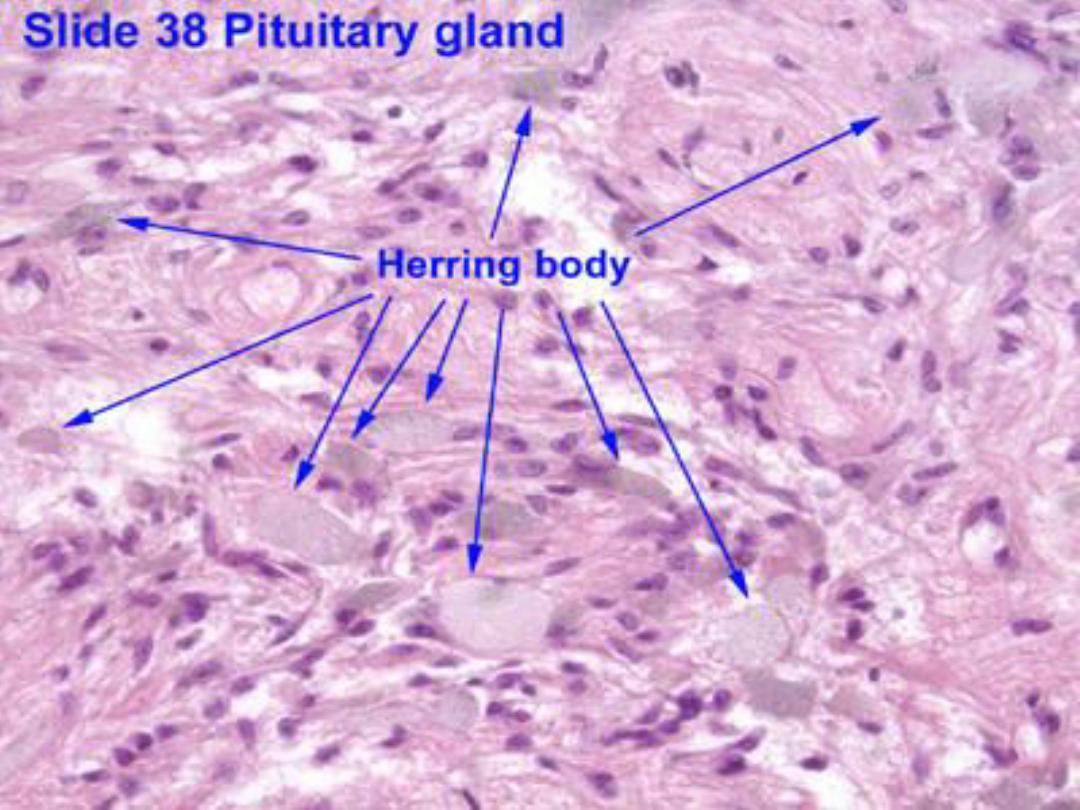
The large portion of the neurohypophysis is the
pars nervosa. This region contains the
unmyelinated axons of secretory hypothalamic
neurons, their endings with hormones, and the
supportive cells, called pituicytes.
CELLS OF THE ADENOHYPOPHYSIS :
The cells of the adenohypophysis were
initially classified as chromophobes and
chromophils,based on the affinity of their
cytoplasmic granules for specific stains.
Chromophobes are believed to be either
degranulated chromophils with few granules or
undifferentiated stem cells.
The chromophils were further subdivided into
acidophils and basophils because of their staining
properties.
CHROMOPHOBES
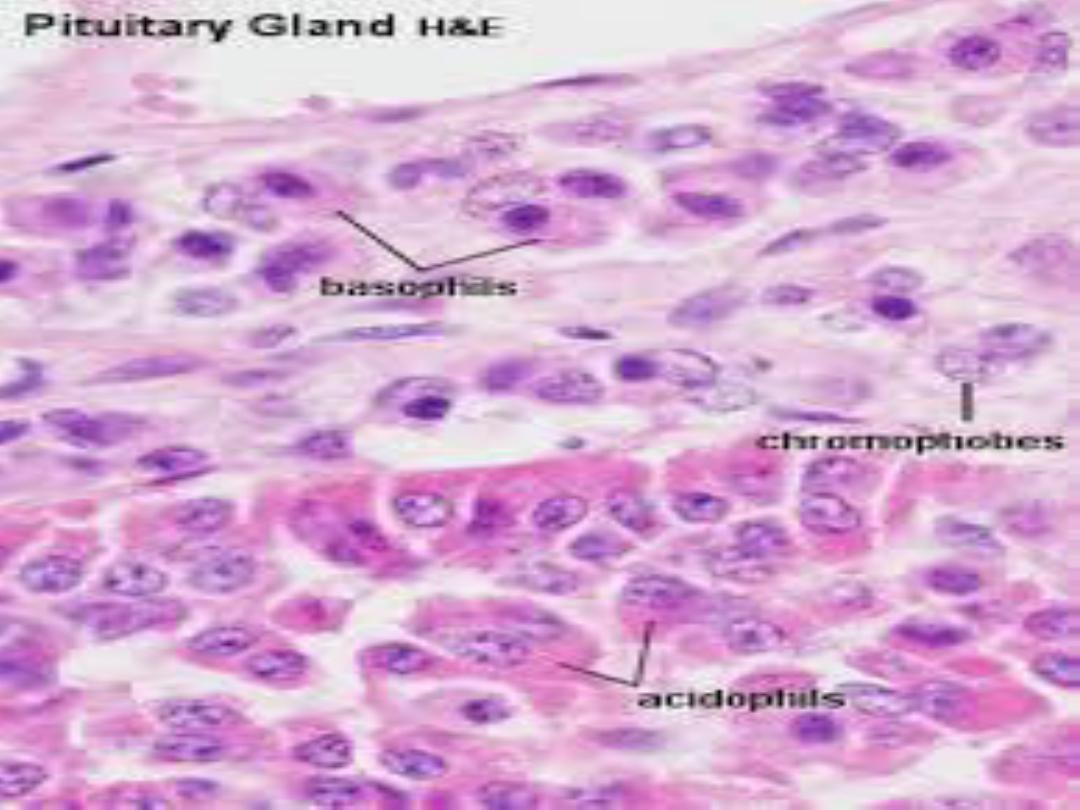
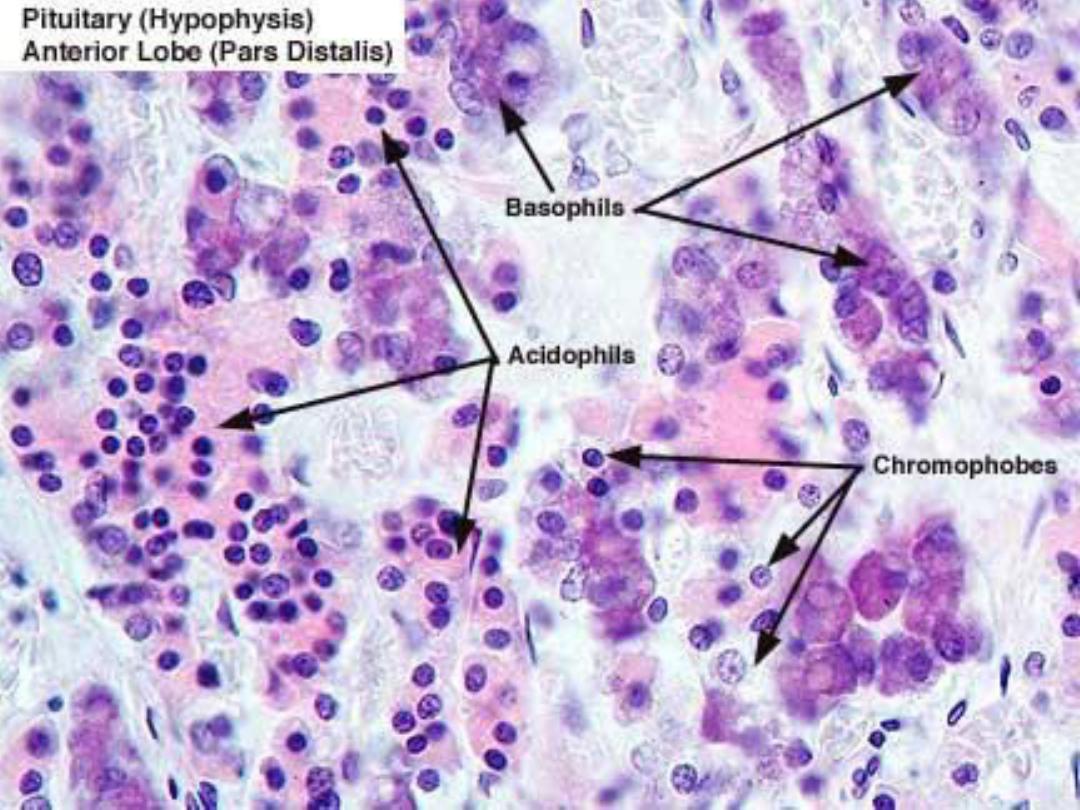
CONT.
In the adenohypophysis, there are two types
of acidophils,
somatotrophs and mammotrophs,
and three types of basophils,
gonadotrophs, thyrotrophs, and corticotrophs.
The hormones released from these cells are
carried in the bloodstream to the target organs,
where they bind to specific receptors that
influence the structure and function of the target
cells.
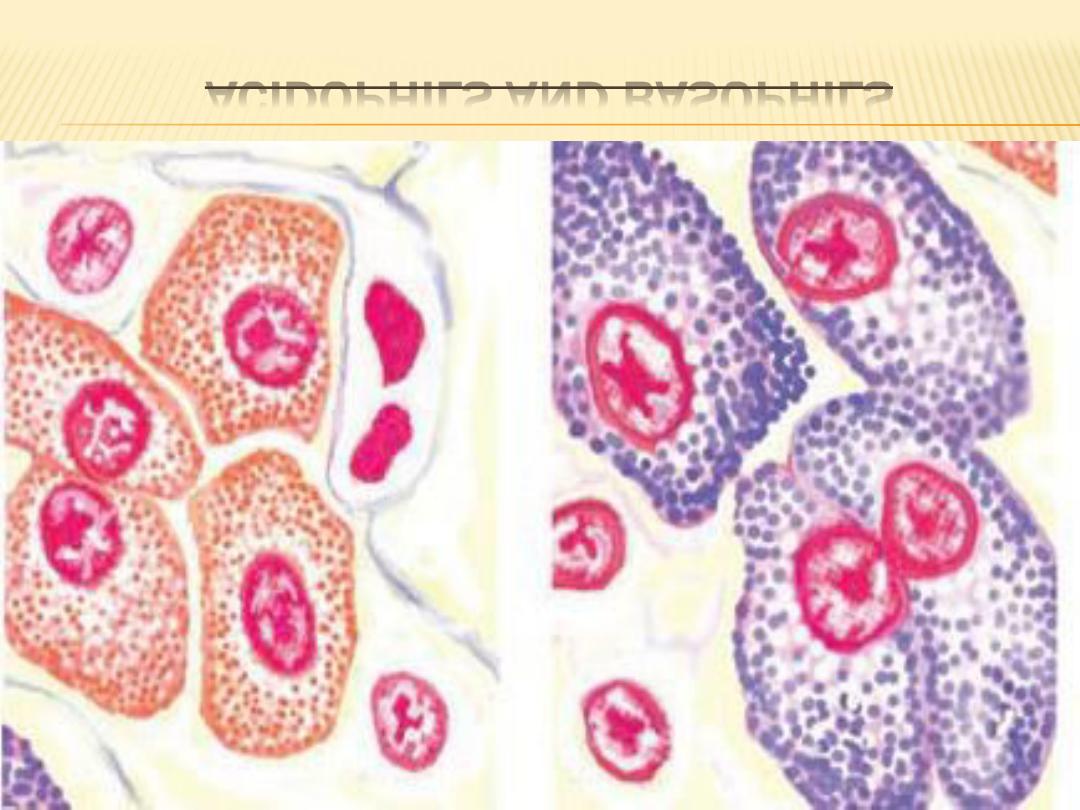
ACIDOPHILS AND BASOPHILS
CONT.
Once the target cells are activated, a
feedback mechanism (positive or negative) can
further control the synthesis and release of these
hormones by directly acting on cells in the
adenohypophysis or neurons in the hypothalamus.
FUNCTIONAL CORRELATIONS:
HYPOPHYSIS
Hormones produced by neurons in the
hypothalamus directly influence and control the
synthesis and release of six specific hormones
from the adenohypophysis. Releasing hormones
are produced by neurons in the hypothalamus for
each hormone that is released from the
adenohypophysis. For two hormones, growth
hormone and prolactin,
inhibitory hormones, as well as releasing
hormones, are produced.
CONT.
The releasing and inhibitory hormones secreted
from the hypothalamic neurons are carried from
the primary capillary plexus to the second
capillary plexus in the adenohypophysis via the
hypophyseal portal system. On reaching the
adenohypophysis, the hormones bind to specific
receptors on cells and either stimulate the cells to
secrete and release a specific hormone into the
circulation or inhibit this function.
CONT.
In contrast, the neurohypophysis does not
secrete hormones. Instead, the neurohypophysis
stores and releases only two hormones, oxytocin
and vasopressin (antidiuretic hormone or ADH) .
CONT.
These hormones are then transported along
unmyelinated axons and stored in the axon
terminals of the neurohypophysis as Herring
bodies, from which they are released into the
capillaries of the par nervosa as needed. Herring
bodies are visible with a light microscope.
FUNCTIONAL CORRELATIONS:
CELLS AND HORMONES OF THE
ADENOHYPOPHYSIS
1- Acidophils:
Somatotrophs secrete somatotropin, also called
growth hormone or GH. This hormone stimulates
cellular metabolism, general body growth, uptake
of amino acids, and protein synthesis.
Somatotropin also stimulates the liver to produce
somatomedins, also called insulin-like
growth factor (IGF-I).
CONT.
These hormones increase proliferation of
cartilage cells (chondrocytes) in the epiphyseal
plates of developing or growing long bones to
increase bone length. There is also an increase in
the growth of the skeletal muscle and increased
release of fatty acids from the adipose cells for
energy production by body cells. Growth hormone
inhibiting hormone,also called somatostatin,
inhibits the release of growth hormone from
somatotrophs in the pituitary gland.
CONT.
Mammotrophs produce the lactogenic
hormone prolactin that stimulates development
of mammary glands during pregnancy. After
(birth), prolactin maintains milk production in the
developed mammary glands during lactation.
Release of prolactin from mammotrophs is
inhibited by prolactin release inhibitory hormone,
also called dopamine .
2- BASOPHILS :
Thyrotrophs secrete thyroid-stimulating hormone
(thyrotropin, or TSH).TSH stimulates synthesis
and secretion of the hormones thyroxin and
triiodothyronine from the thyroid gland.
Gonadotrophs secrete follicle-stimulating
hormone (FSH) and luteinizing hormone (LH).
In females, FSH promotes growth and
maturation of ovarian follicles and subsequent
estrogen secretion by developing follicles.
CONT.
In males, FSH promotes spermatogenesis in the
testes and secretion of androgen-binding protein
into seminiferous tubules by Sertoli cells.
In females, LH in association with FSH induces
ovulation, promotes the final maturation of
ovarian follicles, and stimulates the formation of
the corpus luteum after ovulation. LH also
promotes secretion of estrogen and progesterone
from the corpus luteum.
CONT.
In males, LH maintains and stimulates the
interstitial cells (of Leydig) in the testes to produce
the hormone testosterone. As a result, LH is
sometimes called interstitial cell-stimulating
hormone (ICSH).
Corticotrophs secrete adrenocorticotropic
hormone (ACTH). ACTH influences the function of
the cells in adrenal cortex. ACTH also stimulates
the synthesis and release of glucocorticoids from
the zona fasciculata and zona reticularis of
adrenal cortex.
PARS INTERMEDIA :
In lower vertebrates (amphibians and fishes),
the pars intermedia is well developed and
produces melanocyte-stimulating hormone (MSH).
MSH increases skin pigmentation by causing
dispersion of melanin granules. In humans and
most mammals, the pars intermedia is
rudimentary.
OXYTOCIN :
The two hormones, oxytocin and antidiuretic
hormone (ADH), that are released from the
neurohypophysis are synthesized in the
hypothalamus.Release of oxytocin is stimulated by
vaginal and cervical distension before birth, and
nursing of the infant after birth. The main targets
of oxytocin are the smooth muscles of the
pregnant uterus. During labor, oxytocin is released
to induce strong contractions of smooth muscles
in the uterus, resulting in childbirth .
CONT.
After birth, the suckling action of the
infant on the nipple activates the milk-ejection
reflex in the lactating mammary glands. Afferent
impulses from the nipple stimulate neurons in the
hypothalamus, causing oxytocin release. Oxytocin
then stimulates the contraction of myoepithelial
cells around the alveoli and ducts in the lactating
mammary glands, ejecting milk into the excretory
ducts and the nipple.
ANTIDIURETIC HORMONE (ADH) OR
VASOPRESSIN :
The main action of antidiuretic hormone (ADH) is
to increase water permeability in the kidney. As a
result, more water is reabsorbed from the filtrate
and retained in the body, creating a more
concentrated urine. A sudden decrease of blood
pressure is also a stimulus for release of ADH.
large doses,ADH may cause smooth muscle
contraction in arteries and arterioles. However,
physiologic doses of ADH appear to have minimal
effects on blood pressure.
THYROID GLAND
is located in the anterior neck inferior to the
larynx. It is a single gland that consists of large
right and left lobes, connected in the middle by an
isthmus.
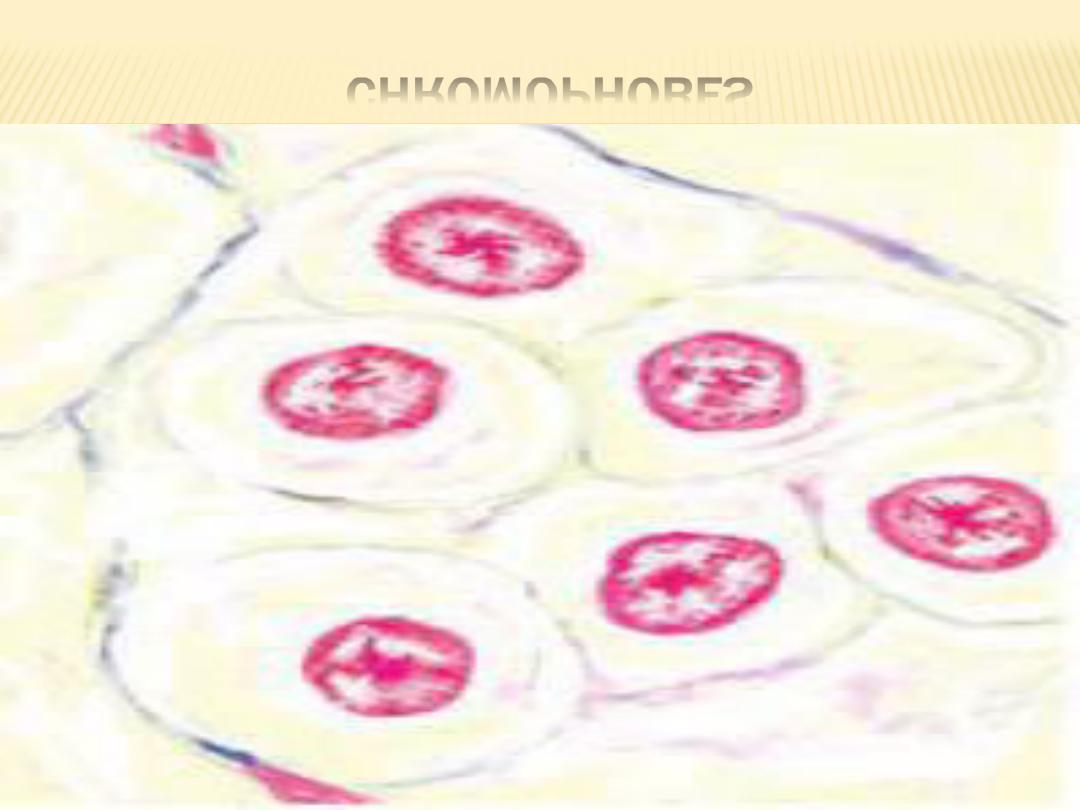
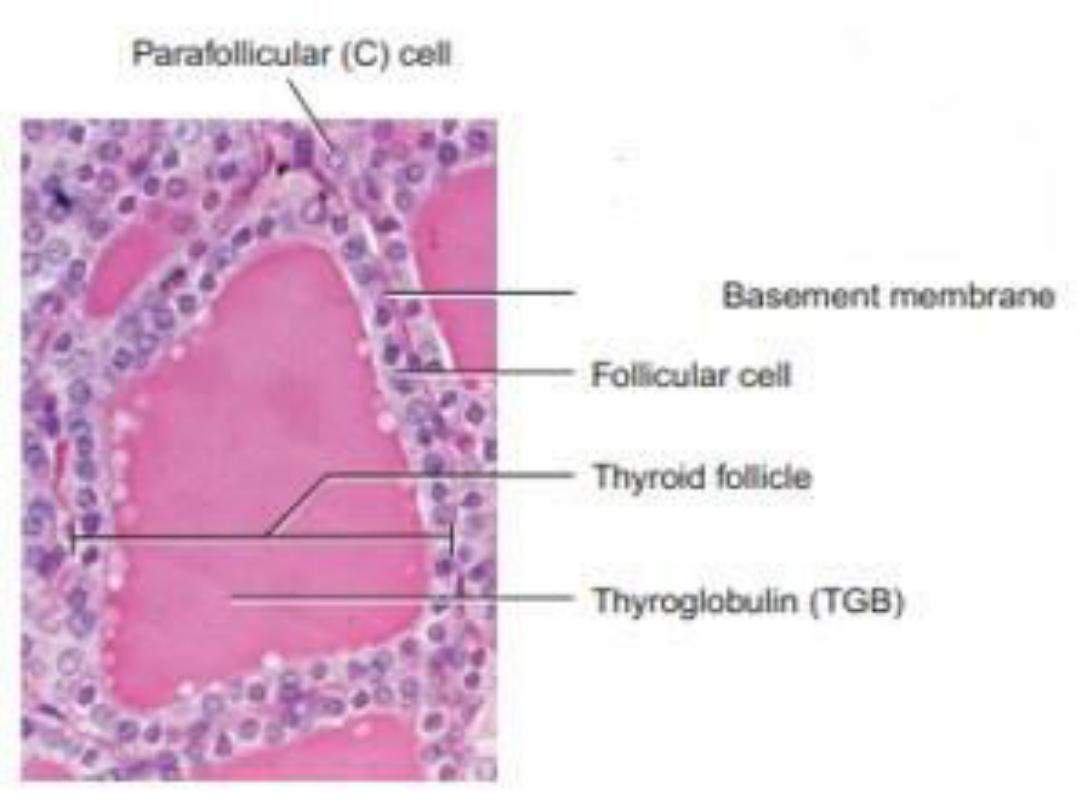
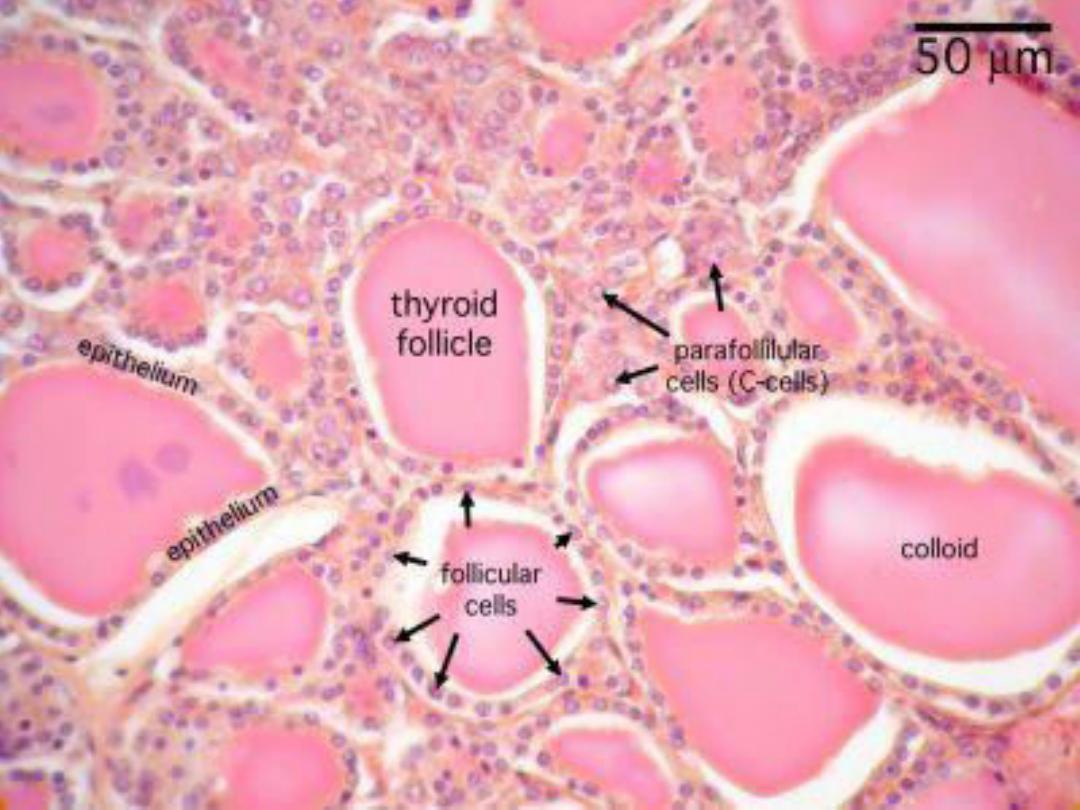
Most endocrine cells,tissues, or organs are
arranged in cords or clumps, and store their
secretory products within their cytoplasm. The
thyroid gland is a unique endocrine organ in that
its cells are arranged into spherical structures,
called follicles.
CONT.
Each follicle is surrounded
by reticular
fibers and a
network of capillaries that allows
for easy entrance of thyroid hormones into
the bloodstream. The follicular epithelium can
be simple squamous, cuboidal, or low
columnar, depending on the state of activity
of the thyroid gland.
CONT.
Follicles are the structural and functional
units of the thyroid gland. The cells that surround
the follicles, the follicular cells, also called
principal cells, synthesize, release, and store
their product outside of their cytoplasm, or
extracellularly, in the lumen of the follicles as a
gelatinous substance,called colloid.
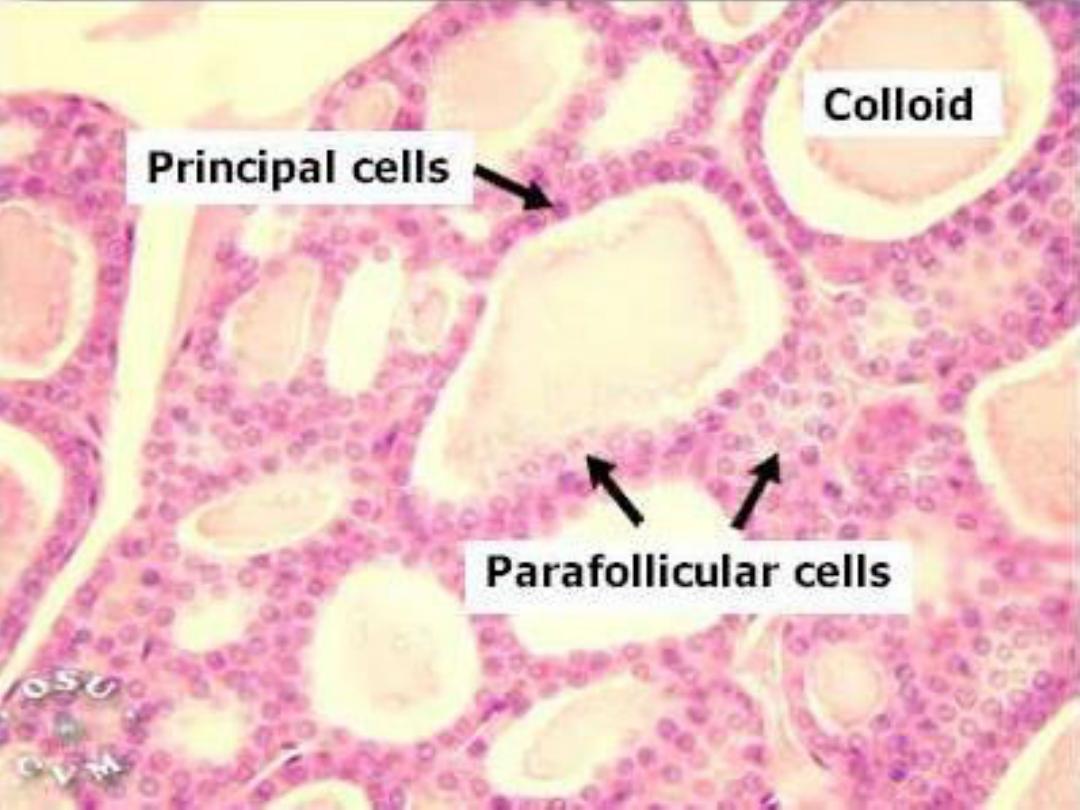
CONT.
Colloid is composed of thyroglobulin, an
iodinated glycoprotein that is the inactive storage
form of the thyroid hormones.
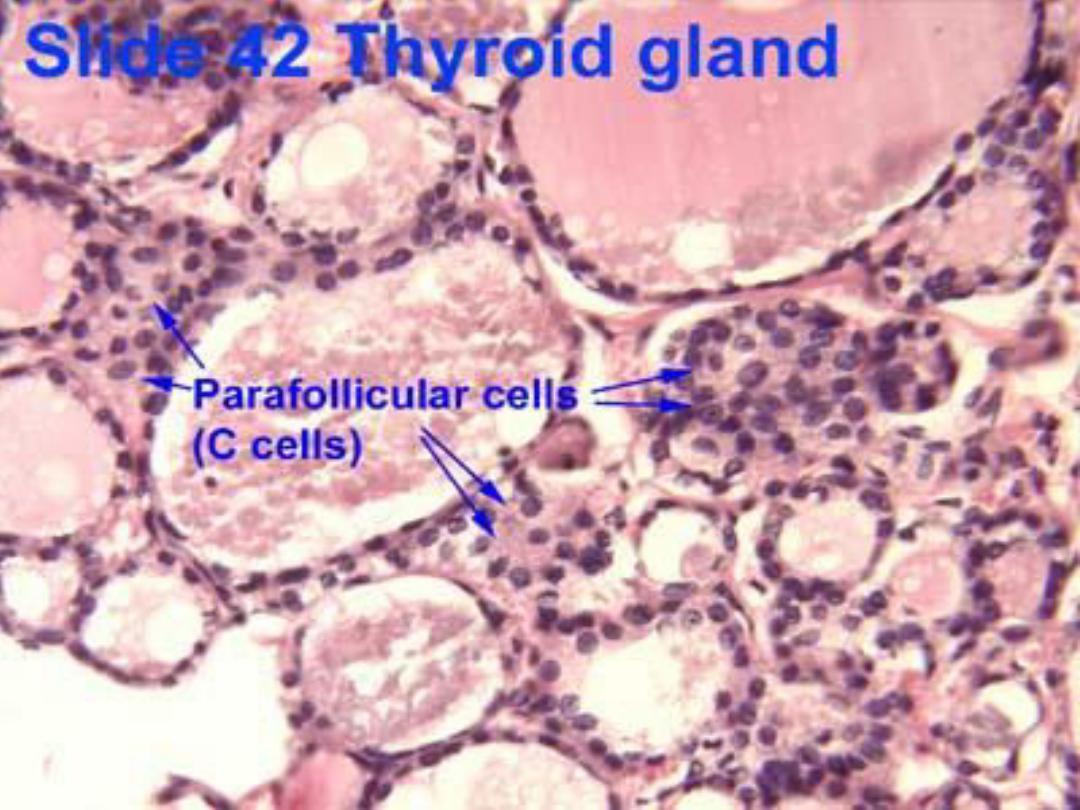
In addition to follicular cells, the thyroid gland
also contains larger, pale-staining parafollicular
cells. These cells are found either peripherally in
the follicular epithelium or within the follicle.
When parafollicular cells are located in the
confines of a follicle, they are always separated
from the follicular lumen by neighboring follicular
cells.
FORMATION OF THYROID HORMONES :
The secretory functions of follicular cells, which
are responsible for the production of thyroid
hormones in the thyroid gland, are controlled by
thyroid-stimulating hormone (TSH) released from
the adenohypophysis. Iodide is an essential
element for production of the active thyroid
hormones triiodothyronine (T3) and
tetraiodothyronine or thyroxine (T4) that are
released into the bloodstream by the thyroid
gland.
C0NT.
Low levels of thyroid hormones in the blood
stimulate the release of TSH from the
adenohypophysis. In response to TSH stimulus,
the follicular cells take up iodide from the
circulation . T3 and T4 remain in thyroid follicles
in an inactive form until needed. TSH released
from the adenohypophysis stimulates the thyroid
gland cells to release the thyroid hormones into
the bloodstream.
RELEASE OF THYROID HORMONES :
Release of thyroid hormones involves
endocytosis (uptake) of thyroglobulin by follicular
cells, hydrolysis of the iodinated thyroglobulin by
lysosomes, and release of the principal thyroid
hormones (T3 and T4) at the base of follicular
cells into the surrounding capillaries.
The presence of thyroid hormones in the general
circulation accelerates the metabolic rate of the
body and increases cell metabolism,growth ,
CONT.
differentiation, and development throughout
the body.
In addition, thyroid hormones increase the rate
of protein, carbohydrate, and fat metabolism.
PARAFOLLICULAR CELLS :
The thyroid gland also contains parafollicular
cells. These cells appear on the periphery of the
follicular epithelium as single cells or as cell
clusters between the follicles. Parafollicular cells
are not part of thyroid follicles and are not in
contact with colloid.
The parafollicular cells synthesize and secrete
the hormone calcitonin (thyrocalcitonin) into
capillaries.
CONT.
The main function of calcitonin is to lower
blood calcium levels in the body. This is primarily
accomplished by reducing the number of
osteoclasts in the bones, inhibiting bone
resorption, and thereby reducing calcium release.
Calcitonin also promotes increased excretion of
calcium and phosphate ions from the kidneys into
the urine. The production and release of calcitonin
by the parafollicular cells depends only on blood
calcium levels and is completely independent of
the pituitary gland hormones.
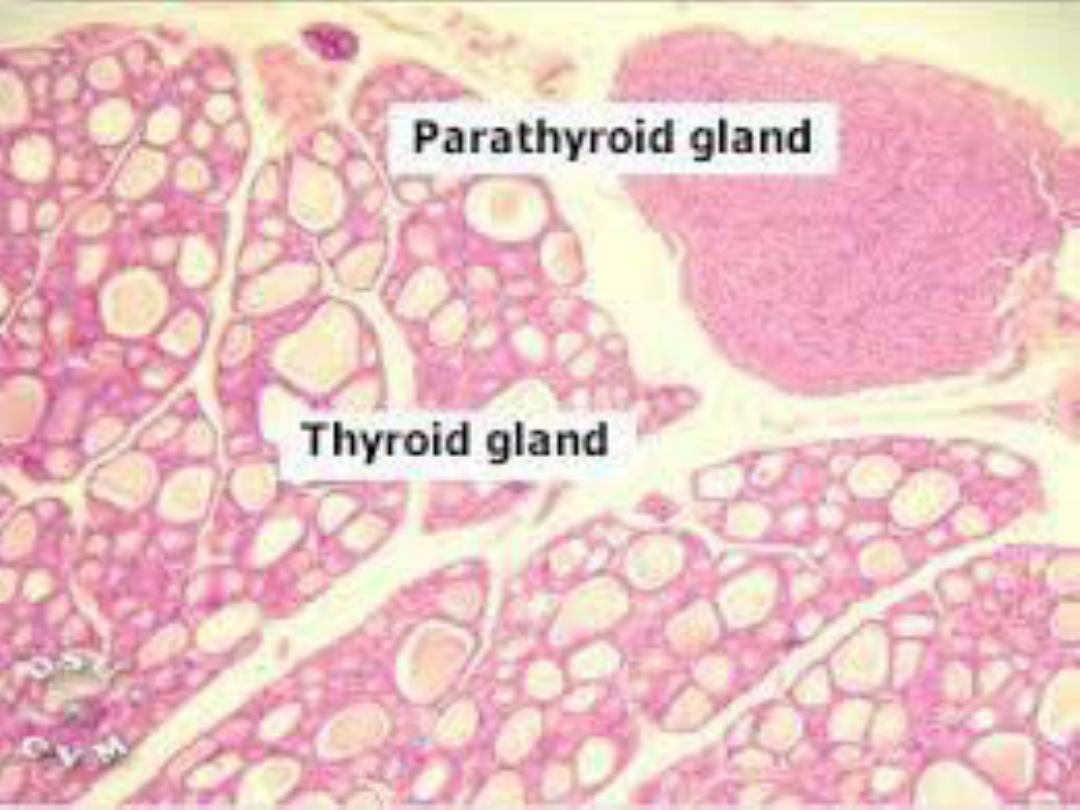
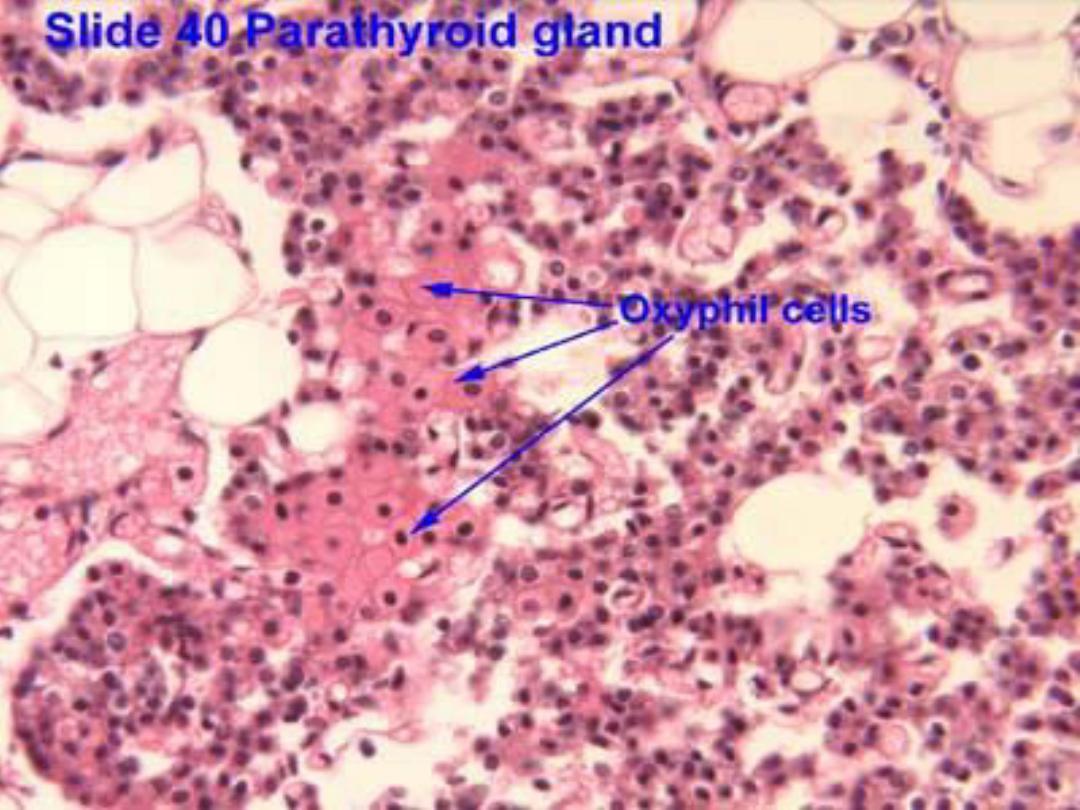
PARATHYROID GLANDS :
Mammals generally have four parathyroid
glands. These small oval glands are situated on
the posterior surface of the thyroid gland, but
separated from the thyroid gland by a thin
connective tissue capsule. In contrast to the
thyroid gland, cells of the parathyroid glands are
arranged into cords or clumps, surrounded by a
rich network of capillaries.

CORDS OF CELLS & ADIPOSE TISSUE
CONT.
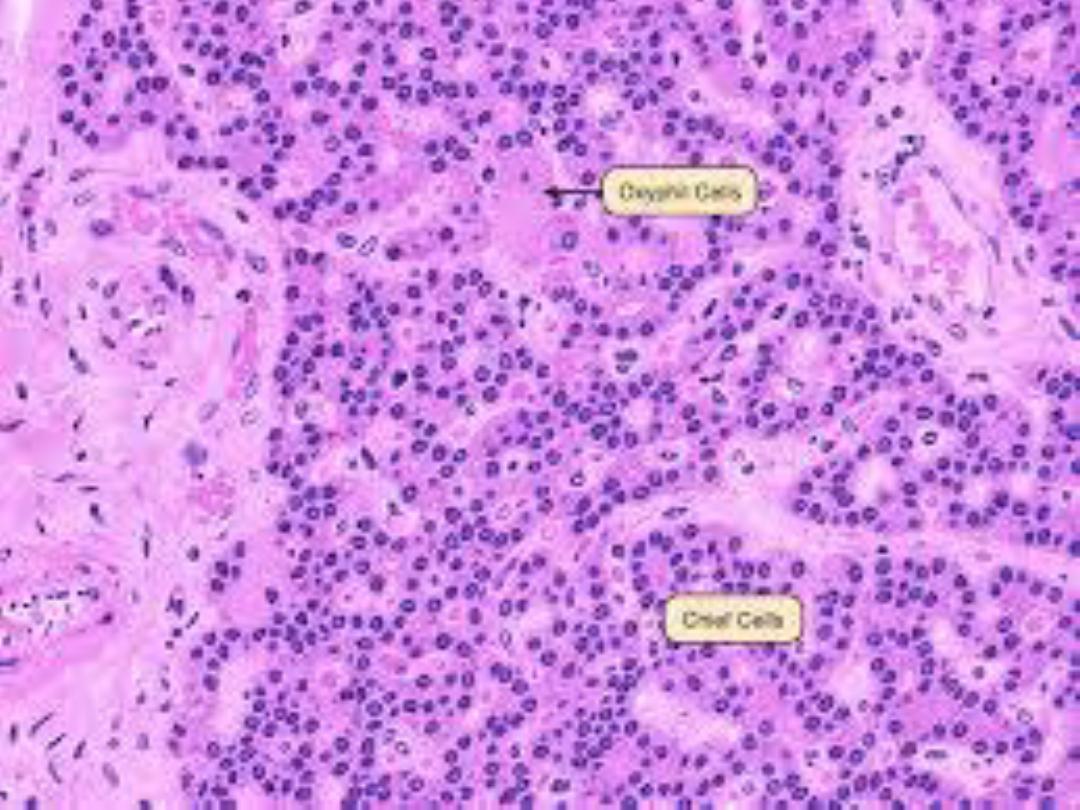
There are two types of cells in the parathyroid
glands: functional principal or chief cells and
oxyphil cells.
Oxyphil cells are larger, are found singly or in
small groups, and are less numerous than the
chief cells. In routine histologic sections, these
cells stain deeply acidophilic. On rare occasions,
small colloid-filled follicles may be seen in the
parathyroid glands.
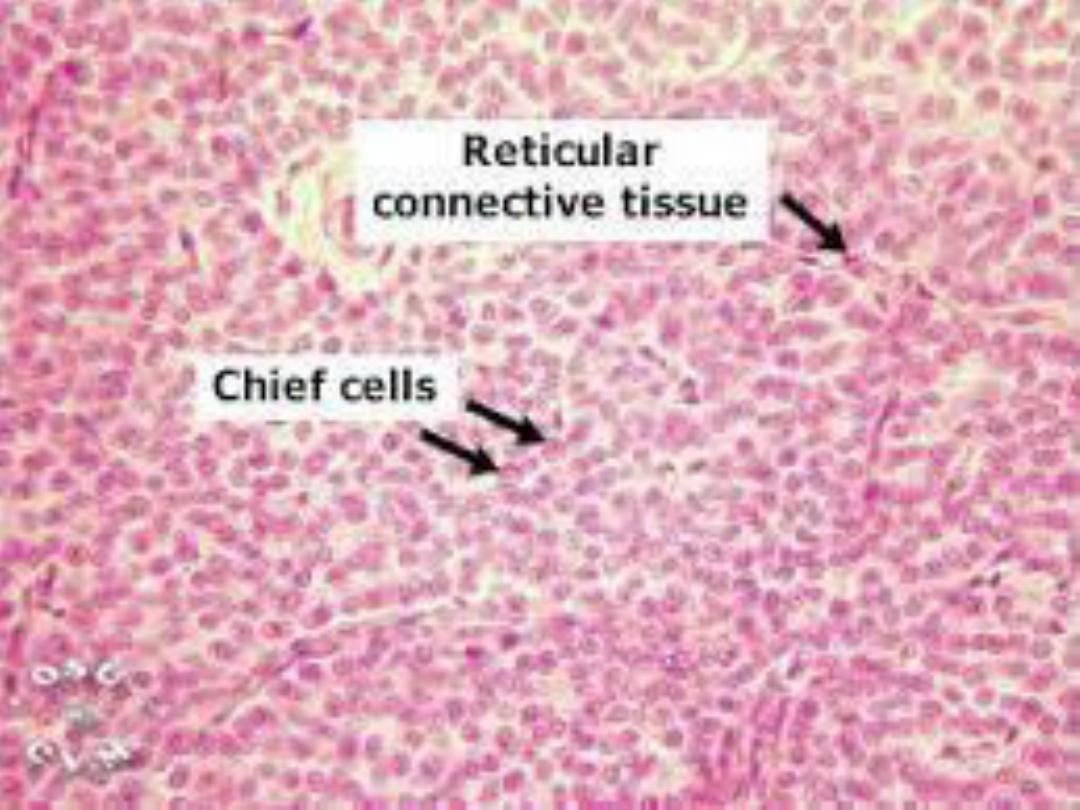
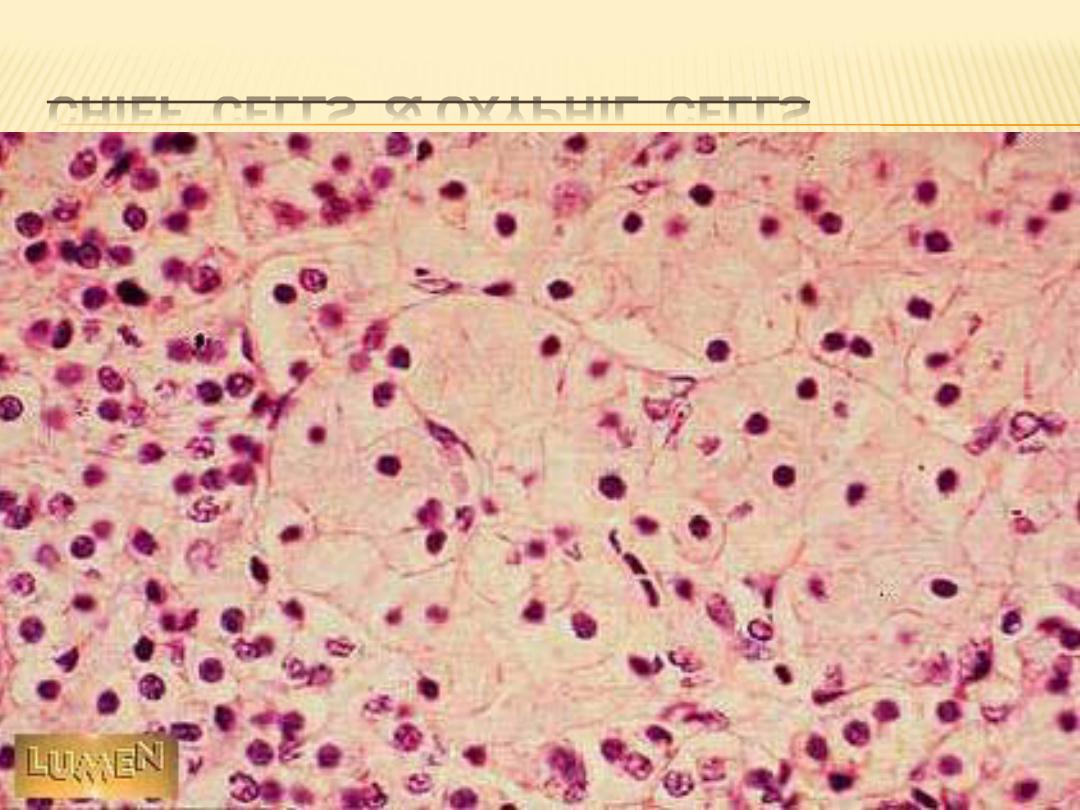
CHIEF CELLS & OXYPHIL CELLS
FUNCTIONAL CORRELATIONS:
PARATHYROID GLANDS
The chief cells of the parathyroid glands produce
parathyroid hormone (parathormone). The main
function of this hormone is to maintain proper
calcium levels in the extracellular body fluids. This
is accomplished by elevating calcium levels in the
blood. This action is opposite or antagonistic to
that of calcitonin,which is produced by
parafollicular cells in the thyroid glands.
CONT.
Release of parathyroid hormone stimulates
proliferation and increases the activity of the
osteoclasts in bones. This activity releases more
calcium from the bone into the bloodstream,
thereby maintaining proper calcium levels. As the
calcium concentration in the bloodstream
increases, further production of parathyroid
hormone is suppressed. Parathyroid hormone also
targets the kidneys and intestines.
CONT.
The distal convoluted tubules in the kidneys
increase reabsorption of calcium from the
glomerular filtrate and elimination of phosphate,
sodium, and potassium ions into urine.
Parathyroid hormone also influences the kidneys
to form the hormone calcitriol, the active form of
vitamin D, resulting in increased calcium
absorption from the gastrointestinal tract into the
bloodstream.
CONT.
The secretion and release of parathyroid
hormone depends primarily on the concentration
of calcium levels in the blood and not on pituitary
hormones. Because parathyroid hormone
maintains optimal levels of calcium in the blood,
parathyroid glands are essential to life.
The function of oxyphil cells in the parathyroid
glands is presently not known.
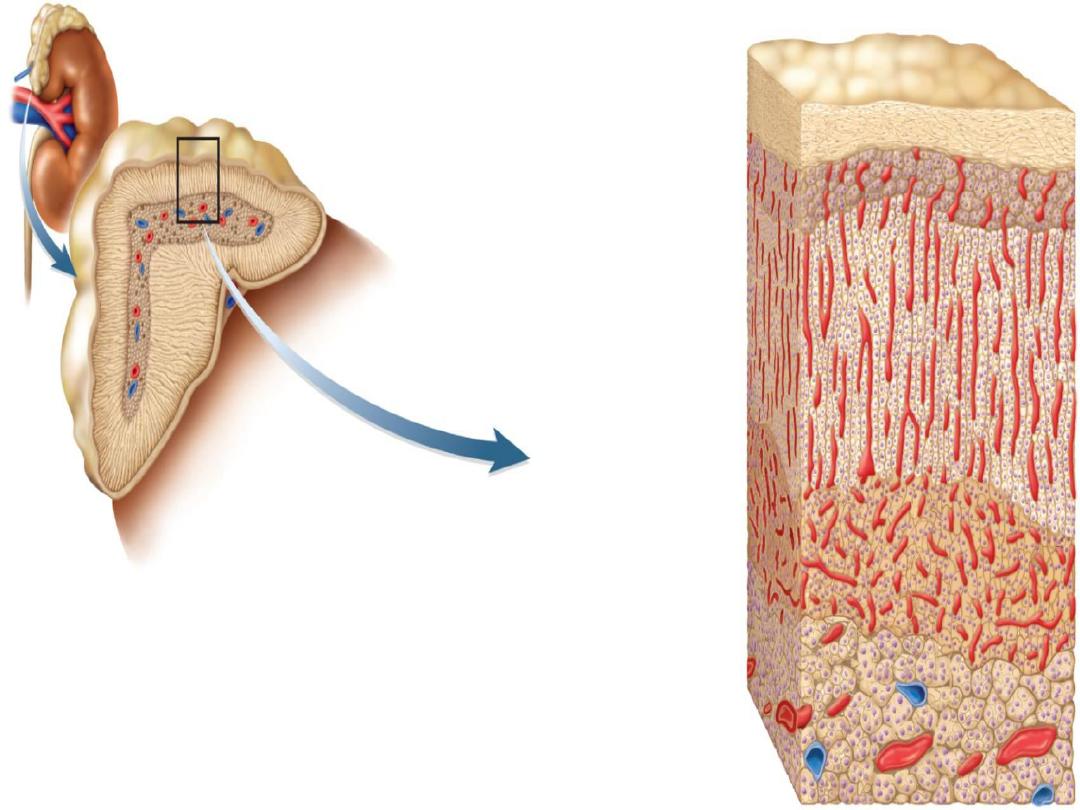
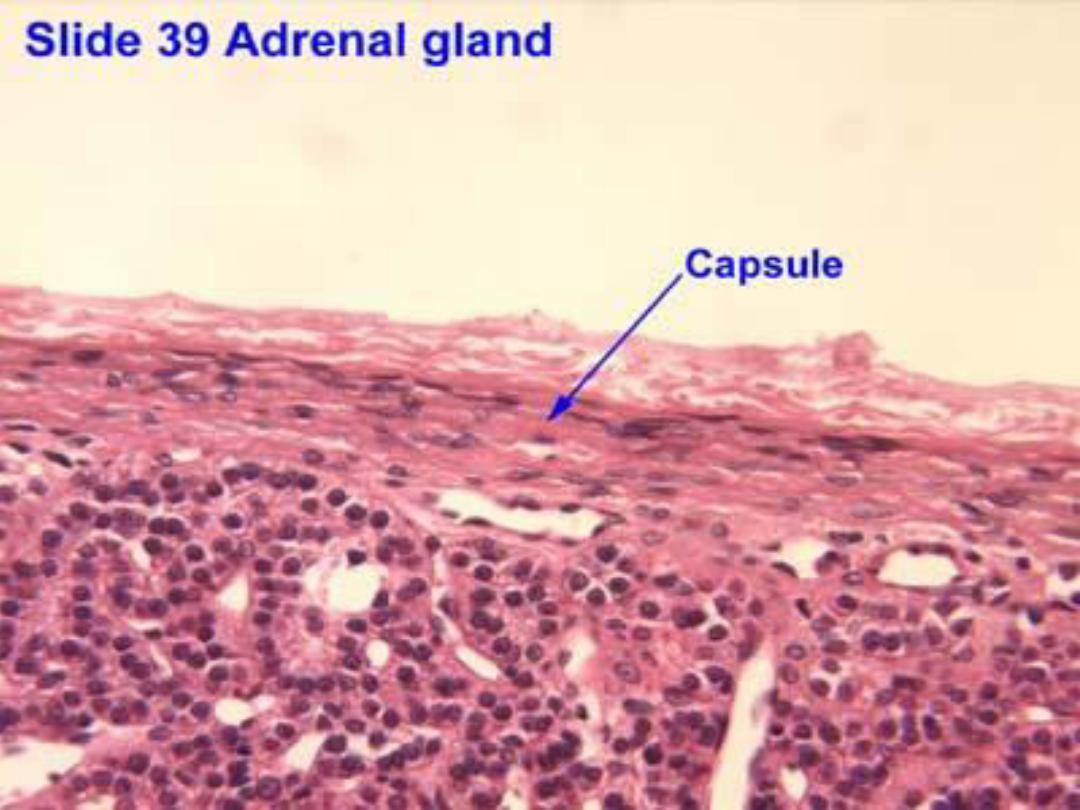
ADRENAL (SUPRARENAL) GLANDS :
The adrenal glands are endocrine organs
situated near the superior pole of each kidney.
Each adrenal gland is surrounded by a dense
irregular connective tissue capsule and
embedded in the adipose tissue around the
kidneys. Each adrenal gland consists of :
-- outer cortex
- inner medulla.
CONT.
Although these two regions of the adrenal
gland are located in one organ and are linked
by a common blood supply, they have separate
and distinct embryologic origins, structures,
and functions.
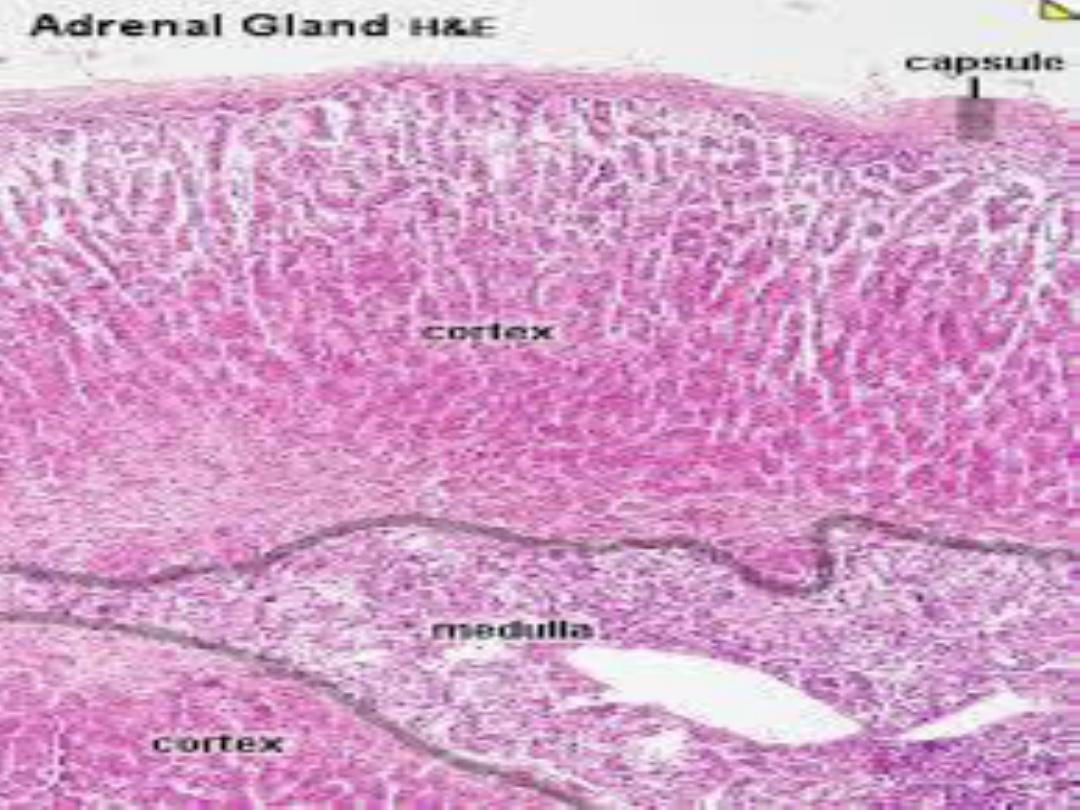
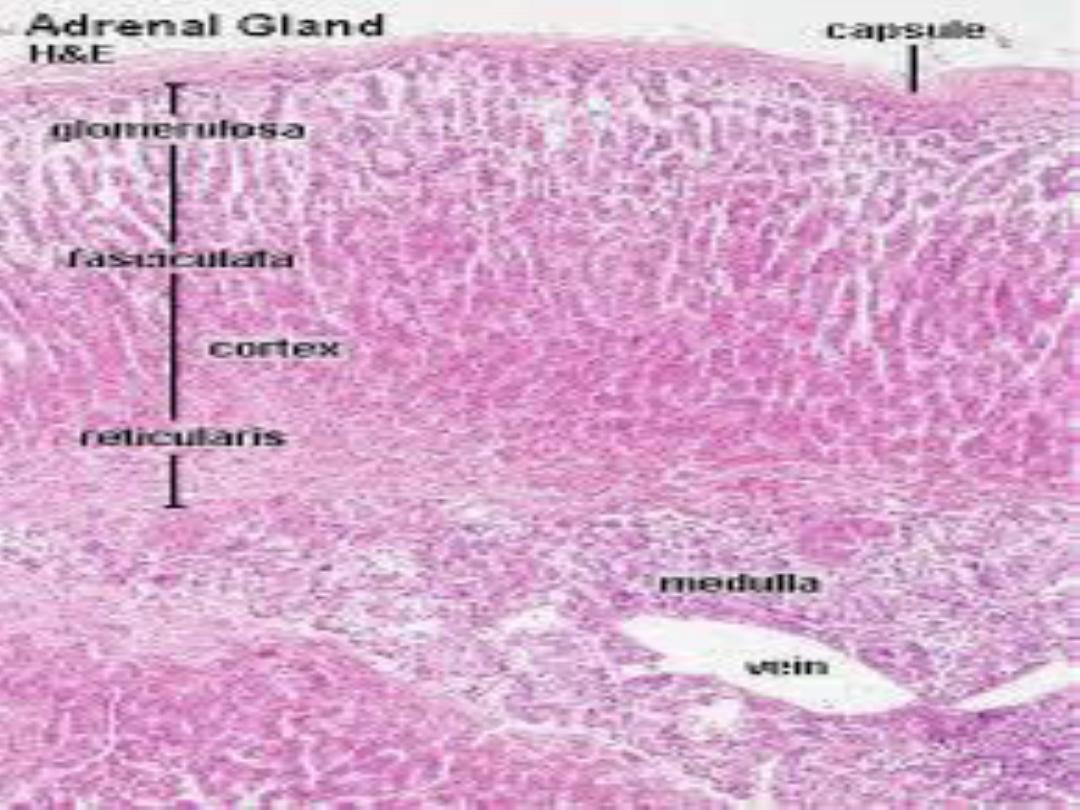
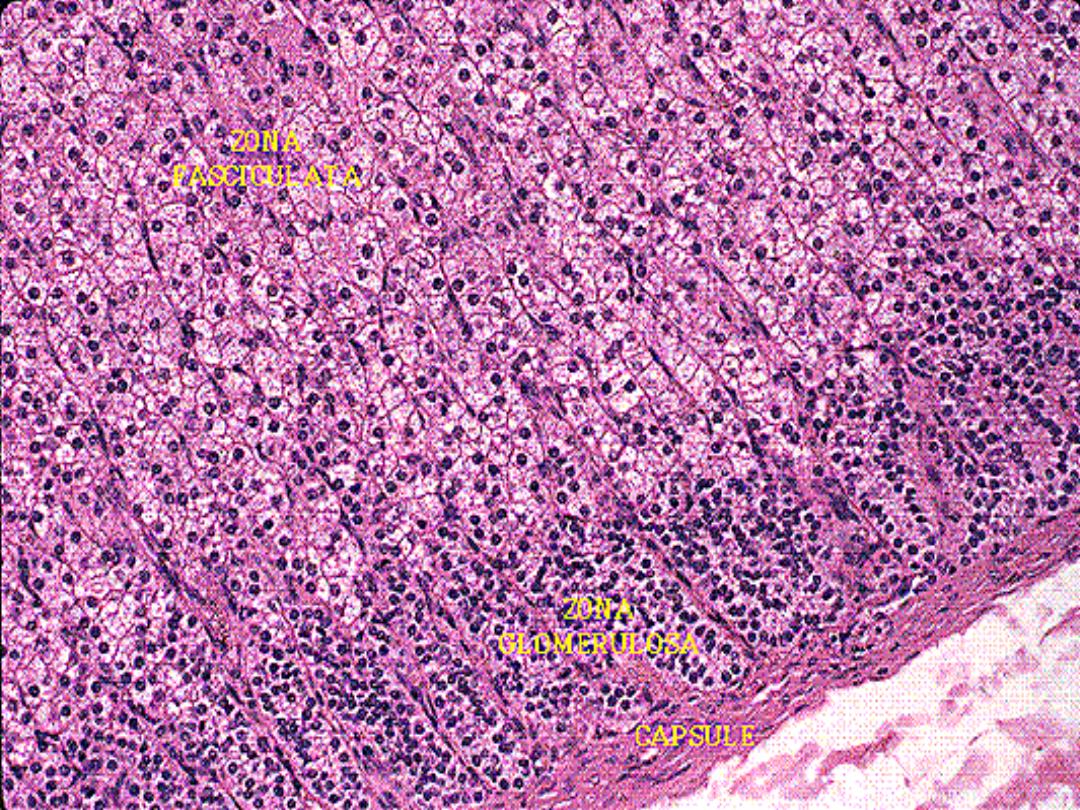
CORTEX :
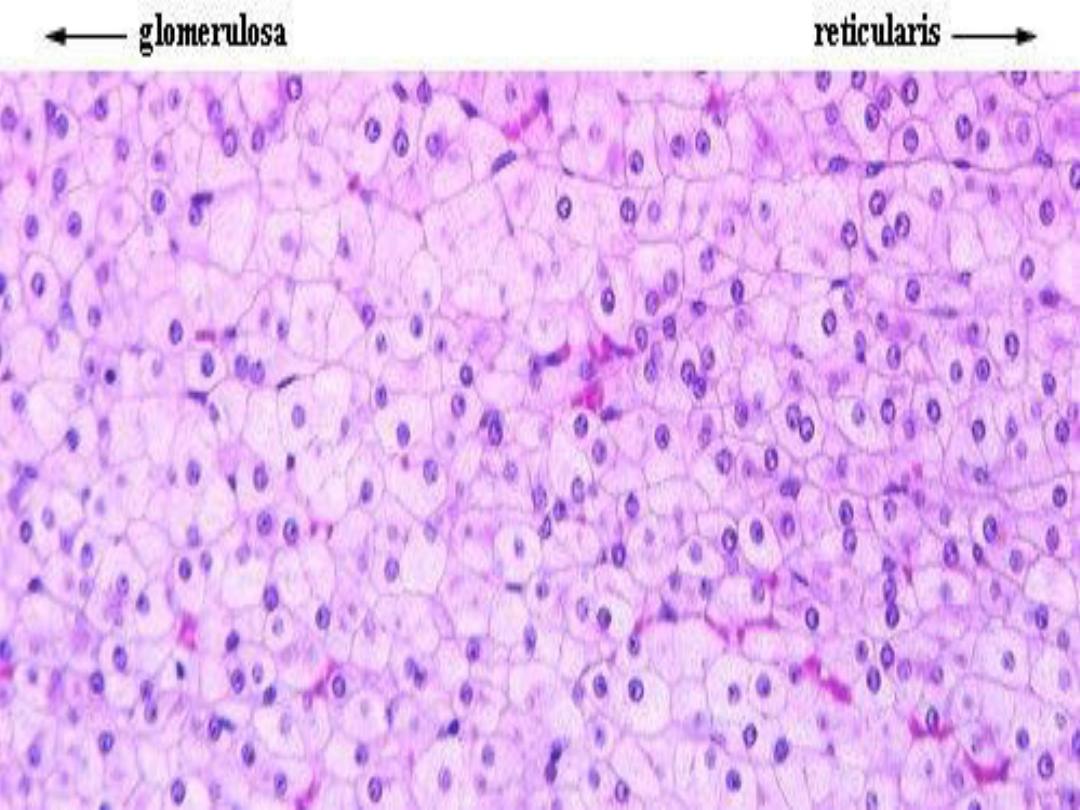
The adrenal cortex exhibits three concentric
zones:
- zona glomerulosa,
- zona fasciculata,
- zona reticularis.
The zona glomerulosa is a thin zone inferior to
the adrenal gland capsule. It consists of cells
arranged in small clumps.
The zona fasciculata is intermediate and the
thickest zone of the adrenal cortex.
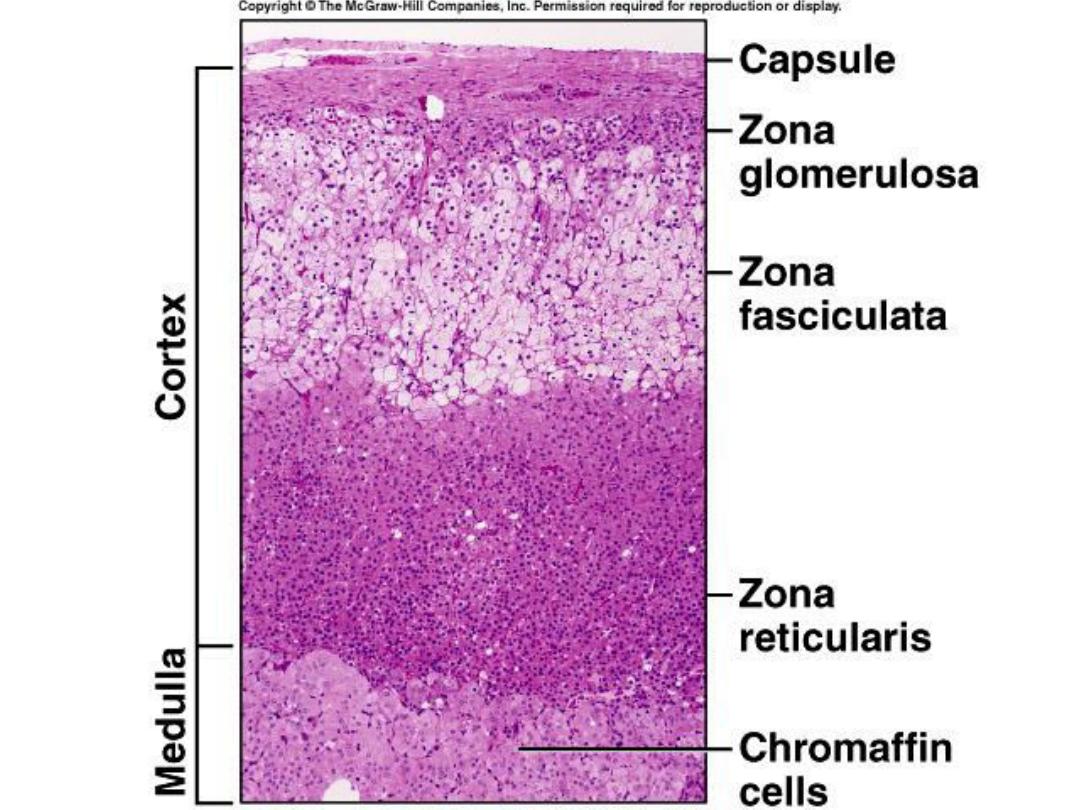
CONT.
This zone exhibits vertical columns of one cell
thickness adjacent to straight capillaries. This
layer is characterized by pale-staining cells owing
to the increased presence of numerous lipid
droplets.
The zona reticularis is the innermost zone that
is adjacent to the adrenal medulla. The cells in
this zone are arranged in cords or clumps.
CONT.
In all three zones, the secretory cells are
adjacent to fenestrated capillaries. The cells of
these zones in the adrenal cortex produce
three classes of steroid hormones:
mineralocorticoids,
glucocorticoids,
sex hormones
MEDULLA :
The medulla lies in the center of the adrenal
gland. The cells of the adrenal medulla, also
arranged in small cords, are modified
postganglionic sympathetic neurons that have lost
their axons and dendrites during development.
Instead, they have become secretory cells that
synthesize and secrete catecholamines (primarily
epinephrine and norepinephrine).
CONT.
Preganglionic axons of the sympathetic neurons
innervate the adrenal medulla cells, which are
surrounded by an extensive capillary network. As
result, the release of epinephrine and
norepinephrine from the adrenal medulla is under
direct control of the sympathetic division of the
autonomic nervous system.
FUNCTIONAL CORRELATIONS:
ADRENAL GLAND CORTEX AND MEDULLA :
Adrenal Gland Cortex:
The adrenal gland cortex is under the
influence of the pituitary gland hormone ACTH
(adrenocorticotropic hormone). Cells of the
adrenal gland cortex synthesize and release three
types of steroids:
mineralocorticoids,
glucocorticoids,
androgens.
CONT.
The cells of the zona glomerulosa in the adrenal
cortex produce mineralocorticoid hormones,
primarily aldosterone.
Aldosterone release is initiated via the renin-
angiotensin pathway in response to decreased
arterial blood pressure and low levels of sodium
in the plasma. These changes are detected by the
juxtaglomerular apparatus (juxtaglomerular cells
and macula densa) located in the kidney cortex
near the renal corpuscles.
CONT.
Aldosterone has a major influence on fluid and
electrolyte balance in the body, with the main
target being the distal convoluted tubules in the
kidneys. The primary function of aldosterone
is to increase sodium reabsorption from the
glomerular filtrate by cells in the distal
convoluted tubules of the kidney and increase
potassium excretion into urine.
CONT.
As water follows sodium, there is an increase in
fluid volume in the circulation. The increased
volume increases blood pressure and restores
normal electrolyte balance.
The cells of the zona fasciculata
—and probably
those of the zona reticularis
—secrete
glucocorticoids,of which cortisol and cortisone are
the most important.
Glucocorticoids are released into the circulation
in response to stress.
CONT.
These steroids stimulate protein, fat, and
carbohydrate metabolism, especially by increasing
circulating blood glucose levels.
Glucocorticoids also suppress inflammatory
responses by reducing the number of circulating
lymphocytes from lymphoid tissues and
decreasing their production of antibodies. In
addition, cortisol suppresses the tissue response
to injury by decreasing cellular and humoral
immunity
CONT.
Although the cells of the zona reticularis are
believed to produce sex steroids, they are mainly
weak androgens and have little physiologic
significance. Glucocorticoid secretion, and the
secretory functions of zona fasciculata and zona
reticularis, are regulated by feedback control
from the pituitary gland and adrenocorticotropic
hormone (ACTH).
ADRENAL GLAND MEDULLA :
The functions of the adrenal medulla are
controlled by the hypothalamus through the
sympathetic division of the autonomic nervous
system. Cells in the adrenal medulla are activated
in response to fear or acute emotional stress,
causing them to release the catecholamines
epinephrine and norepinephrine.
CONT.
Release of these chemicals prepares the
individual for a “fight” or “flight” response,
resulting in increased heart rate, increased
cardiac output and blood flow, and a surge of
glucose into the bloodstream from the liver for
added energy. Catecholamines produce the
maximal use of energy and physical effort to
overcome the stress.
Thank you
