• Carcinoma of the Prostate
• الدكتور• حارث محمد قنبر السعداوي
• اختصاص جراحة الكلى والمسالك البولية والتناسلية والعقم
• كلية طب الكندي - جامعة بغداد
Carcinoma of the prostate
• Epidemiology• Histology
• Etiology
• Clinical Feature
• Spread
• Investigations
• Staging
• Treatment
Epidemiology:
• Ca. prostate is the most common malignant tumour in men over the age of 65 y. It is rare below the age of 40 y.
• Peak incidence is at 70 y. While in testicular ca. the peak incidence is between 25-35 y.
Histology:
• >95% of prostatic neoplasms are adenocarcinomas arising from prostatic acinar cells at the periphery of the gland.
• Squamous cell carcinoma & transitional cell carcinoma of the prostate occur only rarely.
• Ca. prostate usually originates in in the peripheral zone of the prostate, so prostatectomy for benign enlargement of the gland confers no protection from subsequent carcinoma.
Etiology:
• the cause is unknown, but several factors have been noted to play a role in its development• Genetic influences: The risk for development of prostate cancer is increased two to three times if a father or brother has had the disease.
• Hormonal factors: All prostate cancer cells exhibit some degree of androgen dependence. This is supported by the observation that prostate cancer does not occur in castrated persons.
• Chemical factors: Workers in the rubber, fertilizer, textile, and batteries industries have increased rates of prostate cancer.
• Diet: A diet high in saturated fat and cigarette smoking have also been suggested to have an association with prostate cancer.
Clinical features:
• Symptoms of obstruction ( like BPH); patient presented with frequency, acute retention, haematuria, & may had hydronephrosis• Symptoms of local invasion like pelvic pain & infiltration of the ureters back pressure with hydroureter & later hydronephrosis uremia & renal insufficiency
• Symptoms of distant metastasis into bones ( sacrum, spines, femur, ribs)
• DRE → hard nodule in one lobe or the whole prostate is hard
Route of spread:
• Haematogenous: usually to the bones, lungs, liver, and kidneys.
• Lymphatic: First to external iliac (obturator group), internal iliac, presacral nodes.• Local spread: Extra-capsular spread to the surrounding tissues
note: Prostate Ca. differs from other types of carcinoma because it is osteoblastic (osteosclerotic type) i.e. Bone forming carcinoma. So we will notice high density areas on X-ray.
Investigation:
• GUE, HB, blood urea, S.creatinine• Liver function tests: these will be abnormal if there is extensive metastatic invasion of the liver . Alkaline phosphetase may be increase either from hepatic involvement or from secondaries in the bone
• PSA (prostatic specific antigen):
• secreted by prostatic cells which is a tumor marker that increase in carcinoma.
• Normal level is 0 - 4 ng/ml.
• PSA may increase in some conditions such as carcinoma, infection, BPH, and instrumentation like catheterization but in the last 3 the level is increased less than in carcinoma.
• It is related to the size of prostate gland, where the bigger the size the more the secretion of PSA.
• It is normally secreted to the semen but some goes to blood & this is the measured one.
• Prostatic acid phosphatase (PAP):
• It is elevated in 75% to 80% of patients with metastatic prostate cancer & in 10% to 30% of patients with local disease.• It lacks the specificity & sensitivity needed to be a reliable screening test for prostate cancer.
• It remains occasionally useful in detecting metastatic disease & in monitoring therapy.
• Transrectal ultrasonograply (TRUS):
• It is more accurate than abdominal US in assessing the presence and extent of prostate cancer.
• It is very accurate in the assessment of capsular invasion, especially into the seminal vesicles.
• Also we can do transrectal needle biopsy under local anesthesia.
• X-ray:
• chest X-ray may reveal metastases either in the lung fields or the ribs
• Abdominal X-ray may show the characteristic sclerotic metastases that occurs commonly in the lumber vertebrae & pelvic bones
• Bone scanning:
• this is achieved by injection of TC- 99m, which is then monitored using a gamma camera.
• It is more sensitive in the diagnosis of metastases than a skeletal survey, but false positives occur in areas of arthritis, osteomyelitis or a healing fracture.
• CT scan & MRI: to detect L.N. involvement.
• Bone marrow biopsy :- when there is metastases.
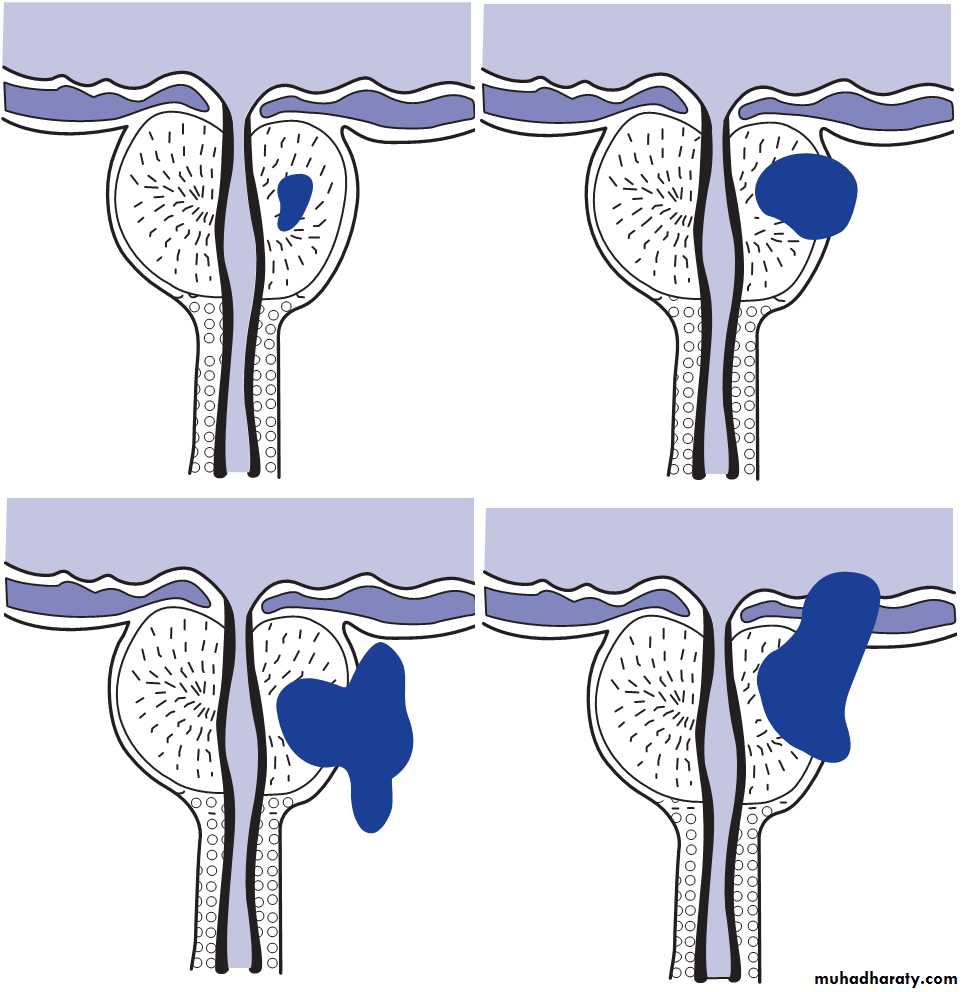
Staging of the disease
Primary tumor:• T1 (non-palpable tumor)
• T1a (A1): Tumor found incidentally at TURP (<5% of resected tissue)
• T1b (A2): Tumor found incidentally at TURP (>5% of resected tissue)
• T1c (B0): Non palpable tumor identified because of an elevated PSA
• T2 (palpable tumor)
• T2a ( B1): Tumor involves one lobe
• T2b (B2): Tumor involves both lobes
• T3 (locally advanced)
• T3a (C1): Extra capsular extension (unilateral or bilateral)
• T3b (C2): Seminal vesicle involvement
• T4 (locally advanced)
• T4 (C2): Tumor invades adjacent structures other than seminal vesicle
like bladder neck, external sphincter, rectum, or pelvic side wall
Lymph nodes:
• N0: No regional L.N. metastases
• N1 (D1): Metastases to regional ( pelvic) L.N.
Metastases:
• M1a (D2): Metastases to nonregional L.N.
• M1b (D2): Metastases to bone
• M1c (D2): Metastases to other sites
• (D3): Hormone-refractory metastatic disease
Grading Of Prostatic Adenocarcinoma:
Microscopically, adenocarcinoma is graded as a pattern 1 to 5.Adenocarcinoma of the prostate is graded using the Gleason system, Since most prostatic Carcinoma are multifocal, an allowance is made by adding the two dominant grades to give a sum score between 2 and 10. If only one pattern is observed, the grade is simply doubled. The system is used with needle biopsies, TURP, and radical prostatectomy specimens
Treatment:
The following factors should be considered:• Patient’s life expectancy and overall health status.
• Tumor characteristics, including Gleason score, tumor stage, PSA levels, PSA velocity and PSA doubling times.
• Risk stratification.
• Outcome tools such as nomograms.
Treatment Options Include:
• Watchful waiting and active Surveillance.
• Radical prostatectomy.
• Radiotherapy (External Beam Radiotherapy).
• Brachytherapy (BT).
• Cryotherapy & High Intansity Focused Ultrasound (HIFU).
• Hormonal Therapy.
• Chemotherapy.
• Immunotherapy.
Radical Prostatectomy:
• Open Radical Prostatectomy• Abdominal
• Perineal
• Laparoscopic Radical Prostatectomy.
• Robotically Assisted Laparoscopic Radical Prostatectomy.
Hormonal Therapy:
• Surgical Castration (Bilateral Orchidectomy): Bilateral orchidectomy, whether total or sub capsular, will eliminate the major source of testosterone production.• Medical castration
• Luteinizing hormone-releasing hormone agonists: as effectively as surgically removing the testicles. E.g. goserelin (Zoladex).
• Nonsteroidal antiandrogens: such as flutamide, and bicalutamide.
• Combination hormone therapy: or total androgen blockade.
• Estrogenic compounds: such as diethylstilbestrol, for the negative feedback effect of testosterone and suppress the secretion of LH. this results in lowering of serum testosterone to castrate levels.
• Steroidal antiandrogens: such as cyproterone acetate.