ATHEROSCLEROSIS
Assistant Prof. Dr .Ghazi F. HajiSenior lecturer of cardiology
Baghdad university -Al-Kindy College of Medicine
Atherosclerosis is a progressive inflammatory disorder of the arterial wall that is characterized by atheroma ( focal lipid-rich deposits) .
*In the heart, it may cause angina, myocardial infarction ( MI )and sudden death;
*In the brain, cause stroke and transient ischemic attack;*In the limbs, cause claudication and critical limb ischemia.
Layers of vessel
1- tunica intimae(basement membrane +endothelium cell)This layer is same in artery ,vein and capillaries
2- tunica media (elastic fibers + smooth muscle cells )
3- tunica adventia (tough collagen fibrous layer )
Epidemiology of coronary heart diseases1:5 men death
1:7 women death
Still the most common of death
In UK 94000 annually death
In last 10 year there is decline in this disease in UK and some developed countries (due to orientation of the risk factors)
In our country ,the disease represent a major issue
Because the risk factors are not managed (HTN.DM.HYPERLIP.SMOKE.OBESITY ……
Modified risk factors Hypercholesterolaemia
Smoking.Hypertension..
Physical activity- Obesity
Diabetes mellitus .
Non modified risk factors
Age
sex.(male > female )
Family history
CONTRIBUATED RISK FACTORS :Haemostatic factors. Alcohol. Other dietary factors. Personality,STRESS
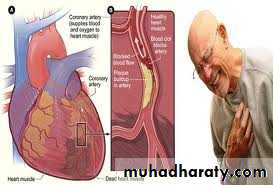
Ischemic heart diseases Atherosclerotic coronary diseases
Pathalogy1- imbalanc imbalance between myocardial oxygen demand and myocardial oxygen supply
O 2 delivery = CO x HB x O2 saturation
2- atherosclerosis and plague rupture
Pathology: atherosclerosis
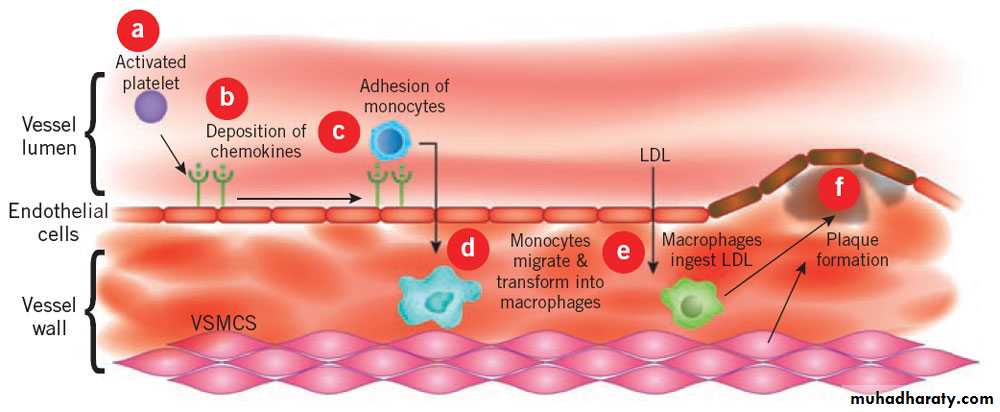
abnormal endothelial function trigger by smoke ,high BP,DM,high LDL-foam cell
fatty streak-
pluga -surface defect +haemorrhage +thrombus
Narrowing of lumen
Plague rupture
InflammationPlatelets
adhesion ,activation ,aggregationActivation of clotting cascade
Thrombosis(fibrin---plasmin)XIII
Down steamMI
Emotion stress
Phsical stress
Vulerable plague
.
Vulnerable' plaques are characterized by a
1-Large lipid-rich core,
2-Thin fibrocellular cap
3-An increase in inflammatory cells
4- Less calcification
In contrast, stable plaques are typified by a small lipid pool, a thick fibrous cap, calcification and plentiful collagenous cross-struts.
Atherosclerosis
Chronic stable anginaAcute coronary syndrome
Unstable angina
NSTEMI
STEMI
Coronary heart disease: clinical manifestations and pathology
Clinical problem PathologyStable angina : Ischaemia due to fixed atheromatous stenosis of one or more coronary arteries
Unstable angina : Ischaemia caused by dynamic obstruction of a coronary artery due to plaque rupture or erosion with superimposed thrombosis
Myocardial infarction : Myocardial necrosis caused by acute occlusion of a coronary artery due to plaque rupture or erosion with superimposed thrombosis
Stable angina
Stable angina
A 62 y old male presented with substernal chest pain on exertion and relive by rest .He has been having this on and off for 7months.last episode occurred 3days ago while he was running to be far away from explosion .He has a history of well control DM and dyslipidemia .the vital signs ,physical examination and EKG are all normal ,exercise stress test is done and shows 2 mm ST-depression
Diagnosis : stable angina why ? What next ?
Stable angina(sudden diffuse chest pain beneath sternum- squeezing, heaviness often radiated to left shoulder , arm, back ,neck and epigastrium ) might associated with nausea ,vomiting .sweating ,dizzness lasting less than 15-20 minutes and aggravated by trigger factors and is promptly relieved by rest,
Trigger factors: exertion or other forms of stress , Cold exposure. Heavy meals ,Intense emotion ,Physical exertion
Causes : Coronary atherosclerosis; spasm .embolism ,dissection vasc;litis
Other causes : anemia .hyperthyrodism, aortic stenosis .hypertrophic cardiomyopathyPathalogy
1- imbalanc imbalance between myocardial oxygen demand and myocardial oxygen supplyO 2 delivery = CO x HB x O2 saturation
2- atherosclerosis
Stable angina classificationExertional
Variant angina (decubitus angina, nocturnal angina)
Angina equivalent syndrome
prinzmetal angina: vasospasm without angiographically detectable atheroma
Syndrome –x
Silent angina
Syndrome X:
The constellation of typical angina on effort, objective evidence of myocardial ischaemia on stress testing, and angiographically normal coronary arteries. It carries a good prognosisPhysical examination is :
Frequently unremarkableMay have S4
Search for important risk factors (e.g. hypertension, diabetes mellitus . xanthoma indicating hyperlipidaemia), )
OR evidence of valve disease (particularly aortic hypertrophic cardiomyopathy. ),
OR left ventricular dysfunction (cardiomegaly, gallop rhythm),
OR other manifestations of arterial disease (carotid bruits, peripheral vascular disease)
OR unrelated conditions that may exacerbate angina (anaemia, thyrotoxicosis)
Investigation in Stable angina
#A full blood count,
#fasting blood glucose, lipids, thyroid function tests
#cardiac markers : NO change in stable angina
#Resting ECG
Is often normal, there is T-wave flattening or inversion in some leads during attack#Exercise ECG
An exercise tolerance test (ETT) is usually performed using a standard treadmill or bicycle ergometer protocol( Planar or down-sloping ST segment depression of ≥ 1 mm is indicative of ischaemia) .exercise capacity 220-age = >85%.
Indication of positivity :>2mmSTdepression.hypotension.
(Contrindication: (acute MI, unstable angina ,acute mypcarditis .severe aortic stenosis ,heart failure ,severe hypertension,cardiac dysaarythmia)If no exercise #Myocardial perfusion scanning.
An equivocal or uninterpretable exercise testThose who are unable to exercise
If cannot read EKG (LBBB,LVH,DIGIOXIN.PACING)
(either exercise testing or pharmacological stress, such as a controlled infusion of dobutamine) after the administration of an intravenous radioactive isotope, such as 99technetium
TMT:False positive? In female
False negative?#Stress echocardiography:dopamine ,dypridimol (positiv entrope .increase contractility ).Decrease contractility ,left ventricular dysfunction
#-Coronary arteriography( what benefit)
..#CT coronary angiography
Risk stratification :CCS classification :
Class I: angina with extreme exertionclassII: angina with walking 1-2 blocks
classIII: angina with walking 1-2 blocks
Class IV: angina with minimal activity
@Medical therapy :feel better +live longer
1-Antiplatelet therapy :Low-dose (75 mg) aspirin .Clopidogrel (75 mg daily) (prusgrel)
2-Lipid lowering agents (statin )
(Antipalatels,b bloker,statin ) reduce mortality
@Anti-anginal drug treatment :
@Four groups of drug are used to help relieve or prevent the symptoms of angina:
Nitrates, β-blockers, Calcium antagonists,
Potassium channel activators
@Revascularization( after coronary angiography do either CABG or angioplasty )
Nitrates
These drugs act directly on vascular smooth muscle to produce venous and arteriolar dilatation.
(lower preload and afterload) and an increase in myocardial oxygen supply (coronary vasodilatation).
S.E: headache, dizziness ,symptomatic hypotension and, rarely, syncope
Erectile dysfunction medications (eg, Viagra®, Cialis®, Levitra®) must be avoided while taking a nitrate medication (short or long-acting).Nitrate preparations:
Sublingual glyceryl trinitrate (GTN) has a short duration of actionTranscutaneously as a patch (5-10 mg daily),
Slow-release buccal tablet (1-5 mg 6-hourly).
Isosorbide dinitrate (10-20 mg 8-hourly)
Isosorbide mononitrate (20-60 mg once or twice a day) can be given by mouth \IV -GTN
pharmacological tolerance.
Beta-blockers@These lower myocardial oxygen demand by reducing heart rate, BP and myocardial contractility,
bronchospasm in patients with asthma.
cardioselective metoprolol , bisoprolol ,atenolol).
Beta-blockers should not be withdrawn abruptly.
Calcium channel antagonistslower myocardial oxygen demand by reducing BP and myocardial contractility.
Dihydropyridine calcium antagonists, such as nifedipine and nicardipine, often cause a reflex tachycardia. it is best to use them in combination with a β-blocker.
Non-Dihydropyridine verapamil and diltiazem are particularly suitable for patients who are not receiving a β-blocker (e.g. those with airways obstruction)
S.E:
bradycardia. precipitate heart failure.
peripheral oedema, flushing, headache and dizziness.
lipid lowering agents
1-Statine( greatest effect upon mortality )S.E:myositis,elevate liver enzymes
2-Niacin
3-Fibrite
4-Cholysteramin
5-Ezetemibe
In CHD :The goal to reduce LDL<100 mg
HDL>40mg
TG<150 mg
In very high risk (CHD+one of following DM,SMOK acute coronary sy. LDL<70 mg )
Potassium channel activators
These have arterial and venous dilating properties
Nicorandil (10-30 mg 12-hourly orally) S.E. It induces bradycardiaRanolazine
IvabradineTrimetazidine
Start therapy with@Life style modification :
@antiplatelet :low-dose aspirin
@lipid lowering agents
@β-blocker, then add (nifidipine or nicardipine)
@ calcium channel blocker
@nitrite
@some time need add nicordinile.or iodine channal antigoism ivabaradin
@PCI or CABG
Invasive treatment Percutaneous coronary (PCI)‘ intervention
PCI (percutanous coronary intervention)is more effective than medical therapy in alleviating angina pectoris and improving exercise tolerance but does not reduce mortality.
CABG(cardiac arteries bypass graft)
Thank you for attentionDesperate Diseases need desperate remedies
QUIZEWhat are the symptoms of stable angina ?
Which are non modified risk factors?
Mention the strategy of treatment in stable angina ?Acute coronary syndrome
(unstable angina ,STEMI,NSTEMI)Unstable angina is characterized by new-onset or rapidly worsening angina (crescendo angina), angina on minimal exertion or angina at rest in the absence of myocardial damage(troponine negative ).
New pain –worse pain-rest pain ----- 50% go to MI
( STEMI,NSTEMI) occurs when symptoms occur at rest and there is evidence of myocardial necrosis, as demonstrated by an elevation in cardiac troponin or creatine kinase-MB isoenzyme
High risk -------go to nstemi or stemi
TIMI score (other score call Grace score)Prolong chest pain
Elevated cardiac markers
Persistence ECG changes
Hemodynamic instability –hypotension
Sustain VT
LV dysfunction
Prior PCI OR CABG
DM
CRF
GRACE ACS Risk
Age-Heart Rate/Pulse-
Systolic BP
Creatinine
Cardiac Arrest At Admission-YES-NO
ST Segment Deviation on EKG?YES-NO
Elevated/Abnormal Cardiac EnzymesYES-NO
Signs/Symptoms
No CHF+1
Rales and/or JVD+2
Pulmonary Edema+3
Cardiogenic Shock+4
unstable angina
Examination : unremarkable
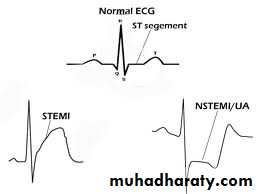
ECG : normal sometime ST segment depression or T wave inversion
Cardiac markers : negativeECHO; normal
AVOIDE EXERCISE TEST IN ?????Myocardial infarction (STEMI ,NSTEMI)
EXAMINATION: ECG:Cardiac markers :ECHO:AVOIDE TMTchest pain+Anxiety and fear of impending death +Nausea and vomiting Breathlessness.Collapse/syncope:
pallor, sweating, tachycardia .bradycardi
Hypotension, oliguria, cold peripheries -Narrow pulse pressure ,Raised JVP -Third heart sound -Quiet first heart sound,Diffuse apical impulse -Lung crepitations
Signs of tissue damage: fever
Signs of complications: e.g. mitral regurgitation,
pericarditis
Criteria to diagnosismyocardial infarction*
@Rise and/or fall of cardiac biomarkers (preferably troponin), together with at least one of the following:
-
@typical chest(Silent in DM,older)
@-ECG changes indicative of new ischaemia
@-ECHO:Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality by echo-
@Sudden unexpected cardiac death, and/or evidence of fresh thrombus by coronary angiography and/or at autopsy
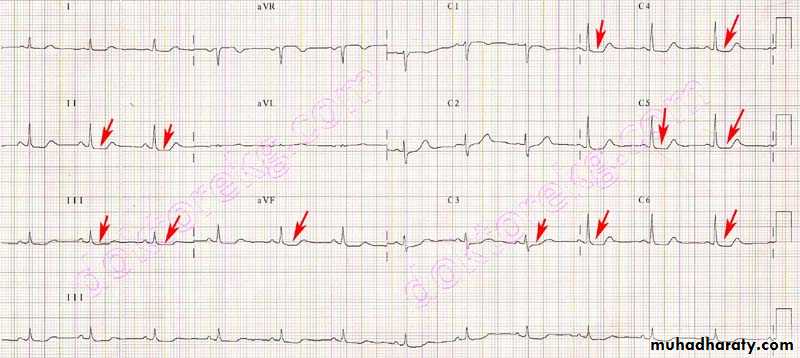
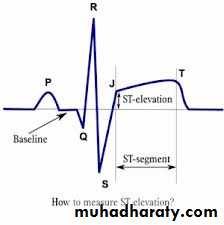
ECG shows bundle branch block or characteristic ST segment elevation > 1 mm in the limb leads or 2 mm in the chest leads
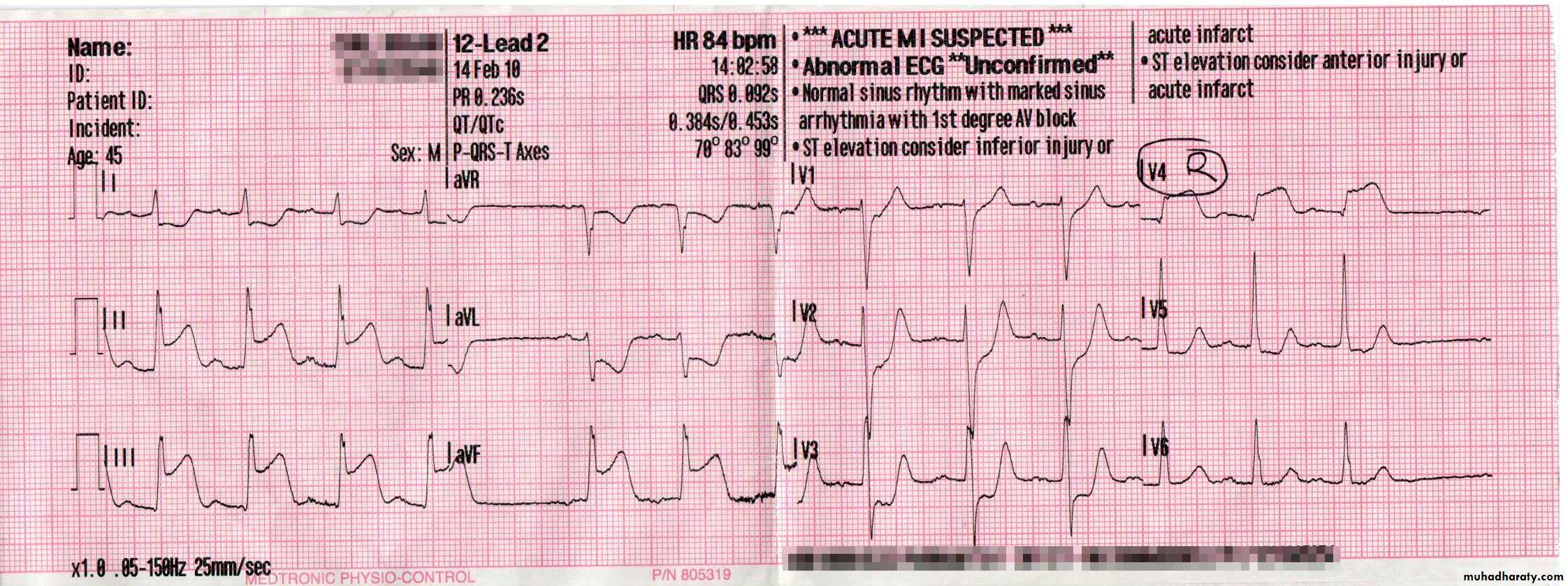
Investigations --Electrocardiography
The initial ECG may be normal in one-third of cases.@Repeated ECGs are important,.
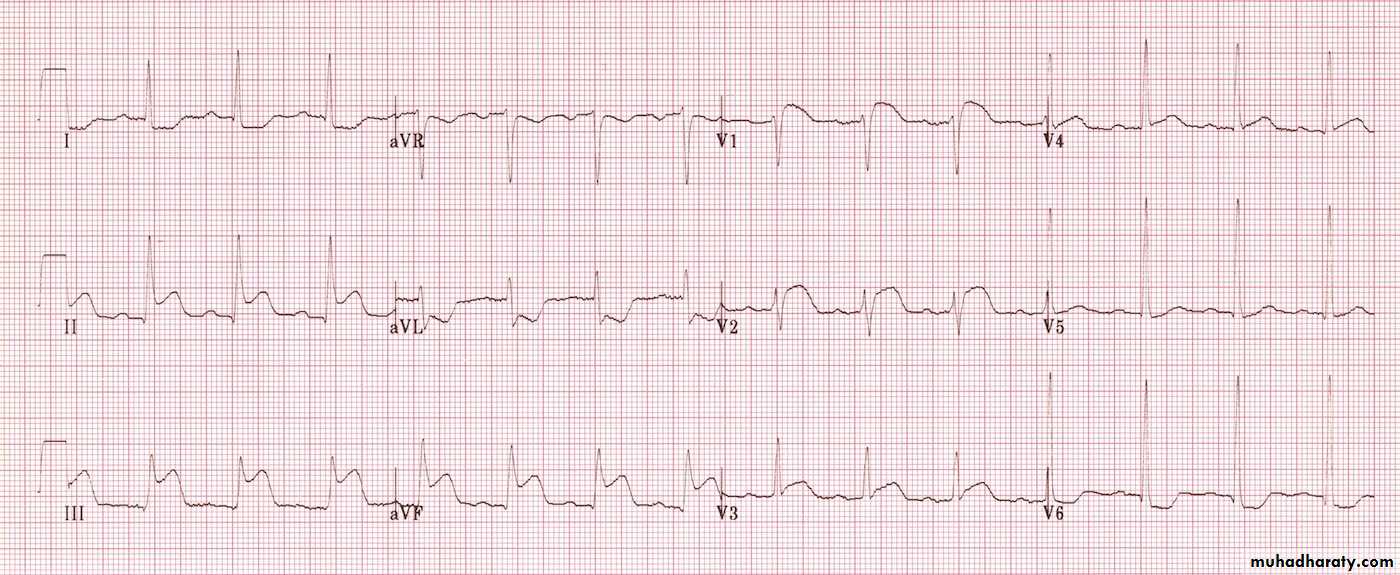
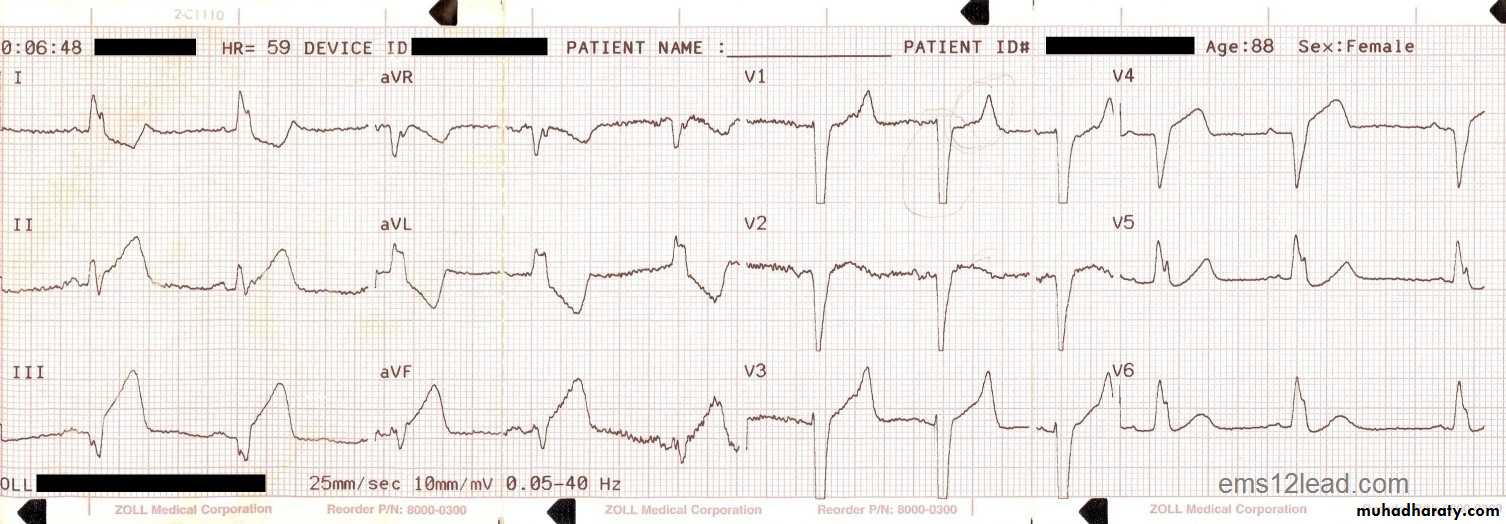
@NSTEMI(subendocardial) MI. This is usually associated with ST-segment depression and T-wave changes. In the presence of infarction, this may be accompanied by some loss of R waves in the absence of Q waves+ positive cardiac enzymes (troponine). NSTEMI - st segment flat or depression (sometime only -t -inversion)
.
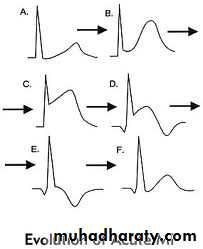
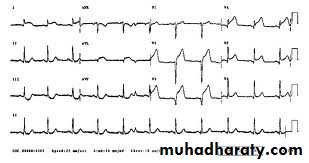
STEMI Stage a (normal), stage B(ste) appears within minutes, stage C(Progressive loss of the R wave, developing Q wave, resolution of the ST elevation and terminal T wave inversion within hours), stage D(Deep Q wave and T-wave inversion within days) stage E( Old or established infarct pattern; the Q wave tends to persist but the T wave changes become less marked.after several weeks or months). .
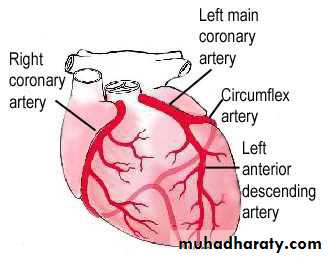
The ECG changes are best seen in the leads that 'face' the ischaemic or infarcted area
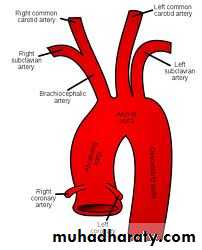
*Anteroseptal infarction: V1 to V4,*Anterolateral infarction:V4 to V6, in aVL and in lead I.
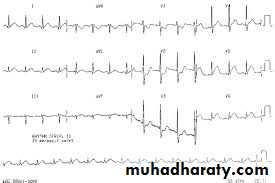
*Inferior infarction : II, III and aVF, while at the same time leads I, aVL and the anterior chest leads may show 'reciprocal' changes of ST depression.*Posterior Infarction : does not cause ST elevation or Q waves in the standard leads, but can be diagnosed by the presence of reciprocal changes (ST depression and a tall R wave in leads V1-V4).
*RV infarctions. :mostly with Inferior infarction right precordiumV4R.
Notes
1-A pattern of widespread ST depression plus ST elevation in aVR > 1 mm is suggestive of left main coronary artery occlusion2-Wellens’ syndrome is a pattern of inverted or biphasic T waves in V2-4 (in patients presenting with ischaemic chest pain) that is highly specific for critical stenosis of the left anterior descending artery.
3-A Subtle Sign of Something Sinister” — a case of NSTEMI presenting with islolated U-wave inversion
INFERIOR MI
ANTERIOR MI
POSTERIOR MI
INFERIOR MI +RV INFARCTION
V4R OF RV INFARCRTION
ANTERIOLATERAL MI
NEW LBBB MI
Plasma cardiac markers
@ creatine kinase (CK), a more sensitive and cardiospecific isoform of this enzyme (CK-MB), and the cardiospecific proteins, troponins T and I . LDH.myoglobulin
CK starts to rise at 4-6 hours, peaks at about 12 hours and falls to normal within 48-72 hours. CK is also present in skeletal muscle, and a modest rise in CK (but not CK-MB) may sometimes be due to an intramuscular injection, vigorous physical exercise or, particularly in older people,. Defibrillation causes significant release of CK but not CK-MB or troponins.
Cardiac troponins T and I is The most sensitive markers of myocardial cell damage are the, which are released within 4-6 hours and remain elevated for up to 2 weeks.
@A leucocytosis is usual, The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are also elevated.
@Chest X-ray :This may demonstrate pulmonary oedema , cardiomegaly .
@Echocardiography :This is useful for assessing left and right ventricular function and for detecting important complications such as mural thrombus, cardiac rupture, ventricular septal defect, mitral regurgitation and pericardial effusion.quize
1-How differentiate between unstable ,STEMI,NSTEMI?2- mention the markers in acute myocardial infraction?
3-Mention the ECG changes in:Unstable angina
STEMI
NSTEMI
Management
In the first 12 hours
Patients should be admitted urgently to hospital
because there is a significant risk of death or recurrent myocardial ischaemia during the early unstable phase, and appropriate medical therapy can reduce the incidence of these by at least 60%.
404
Analgesia-- not reduce mortalityABCDE(acess,asprin,analgesic ,bblocker ,coronary dilator , vasodilator,enough oxygen)
To relieve distress,.Intravenous opiates (initially morphine sulphate 5-10 mg ) and antiemetics (initially metoclopramide 10 mg) should be administere.
Intramuscular injections should be avoided
Antiplatelet therapy---- reduce mortality 25%75-300 mg aspirin(COXI)(irevesible) daily improves survival
75 mg clopidogrel (irreversible) to those untolerat or allergic
90 mg ticagrelor (reversible )--- prusagrel (irreversible) .
Canogrelor (iv)
Glycoprotein IIb/IIIa receptor antagonists, such as tirofiban and abciximab, block the final common pathway of platelet aggregation and are potent inhibitors of platelet-rich thrombus formation.
Indication:
1-acute coronary syndromes who undergo PCI ,
2-those with recurrent ischaemia
3-those at particularly high risk, such as patients with diabetes mellitus or an elevated troponin concentration
Antithrombotic (Anticoagulation)---- reduce mortality
reduces the risk of thromboembolic complications, and prevents reinfarction.1-unfractionated heparin,2- fractioned (low molecular weight) heparin
3-subcutaneous fondaparinux.4- direct thrombin inhibitor
Anticoagulation (heparin ,LMWH)should be continued for 8 days
Warfarin :
Indication for long term anticoagulant therapy (warfarin ):
1-If there is persistent atrial fibrillation or
2-Evidence of extensive anterior infarction, or
3-If echocardiography shows mobile mural thrombus.
Anti-anginal therapy---
1-Glyceryl nitrate;Glyceryl nitrate are useful to relief recurrent or persistent ischaemic pain.
2-B-blocker:
Intravenous β-blockers (e.g. atenolol 5-10 mg or metoprolol 5-15 mg given over 5 mins) relieve pain, reduce arrhythmias and improve short-term mortality
However, they should be avoided if there is heart failure (pulmonary oedema), hypotension (systolic BP < 105 mmHg) or bradycardia (heart rate < 65/min)
.
3-A dihydropyridine calcium channel antagonist (e.g. nifedipine or amlodipine) can be added to the β-blocker if there is persistent chest discomfort but may cause an unwanted tachycardia if used alone.
Because of their rate-limiting action, verapamil and diltiazem are the calcium channel antagonists of choice if a β-blocker is contraindicated.
@ACE inhibitor (e.g. enalapril 10 mg 12-hourly or ramipril 2.5-5 mg 12-hourly) can counteract ventricular remodelling, prevent the onset of heart failure, improve survival, reduce recurrent MI and avoid rehospitalisation., angiotensin receptor blockers (e.g. valsartan or candesartan ) are suitable alternative
@Lipid lowering agents – statine( zocor,crestor,atrovostatine )
ThrombolyticCan reduce hospital mortality by 25-50%
: 'minutes mean muscle'. ' ‘
Prompt thrombolytic treatment (within 12 hours, and particularly within 6 hours, of the onset of symptoms) reduces mortality in patients with acute MI and ECG changes of ST elevation or new bundle branch block when there is no hospital with PCI capabilities and there is contraindication to PCI or the time to reach hospital with PCI capabilities beyond 120 min .
Reperfusion therapy
#Non-ST segment elevation acute coronary syndrome Immediate emergency reperfusion therapy has no demonstrable benefit in patients with NTSEMI and thrombolytic therapy may be harmful..#ST segment elevation acute coronary syndrome
Immediate reperfusion therapy restores coronary artery patency, preserves left ventricular function and improves survival. Successful therapy is associated with pain relief, resolution of acute ST elevation and sometimes transient arrhythmias (e.g. idioventricular rhythm).Alteplase (human tissue plasminogen activator or tPA) is a genetically engineered drug that is given over 90 minutes (bolus dose of 15 mg, followed by 0.75 mg/kg body weight, over 30 mins and then 0.5 mg/kg body weight over 60 mins). Its use is associated with better survival rates than other thrombolytic agents, such as streptokinase, but carries a slightly higher risk of intracerebral bleeding
Analogues of tPA, such as tenecteplase and reteplase, have a longer plasma half-life than alteplase and can be given as an intravenous bolus..
contraindications to thrombolytic therapy:
Active internal bleeding
Previous subarachnoid or intracerebral haemorrhage
Uncontrolled hypertension
Recent surgery (within 1 month)
Recent trauma (including traumatic resuscitation)
High probability of active peptic ulcer
Primary percutaneous coronary intervention (PCI)
This is the treatment of choice for ST segment elevation MI (balloon inflation with intracoronary stent implantation).In comparison to thrombolytic therapy, it is associated with a greater reduction in the risk of death, recurrent MI or stroke
intravenous thrombolytic therapy remains the first-line reperfusion treatment in many hospitals, especially those in rural or remote areas. When primary PCI cannot be achieved within 2 hours of diagnosis, thrombolytic therapy should be administered.
The main long-term complication of PCI is restenosis , which occurs in up to one-third of cases.
This is due to a combination of elastic recoil and smooth muscle proliferation (neo-intimal hyperplasia) and tends to occur within 3 months.
Drug-eluting stents can reduce this risk even further by allowing an antiproliferative drug such as sirolimus or paclitaxel to elute slowly from the coating and prevent neo-intimal hyperplasia and in-stent restenosis
IF Typical chest pain ---do ECG+ troponine
cardiac rhythm monitor+ o2 if indicated+asprin 300mg or clopidogrel 600mg +metaprolol 5-15mg IV or 50-100mg +transfer to cardiac unit------LMWH or hepraine sc or foudopurnix +_nitrite infusion–
Do reperfusion therapy(primary PCI (GPIIb/IIIa receptor antiagonist iv)or thrombolytic)
IF medium or high risk or recurrent symptoms –
Do early in hospital coronary angiography – after that should mantaine asprin or clopidogrel+ LMWH or hepraine _+ b blocker + ACE inhibitor +statine
Complications of acute coronary syndrome
1-ArrhythmiasCommon arrhythmias in acute coronary syndrome
Ventricular fibrillation( about 5-10% of patients who reach hospital and is thought to be the major cause of death ) Implantable cardiac defibrillator (high-risk patients)
Ventricular tachycardia ,Accelerated idioventricular rhythm ,Ventricular ectopics
Atrial fibrillation(This is common but frequently transient),
Atrial tachycardia
Sinus bradycardia +Atrioventricular block
(particularly after inferior MI) (This does not usually require treatment,). Need atropine or transient pacemaker or permanent pacemaker) ,
.
2-Ischaemia(Patients who develop recurrent angina at rest or on minimal exertion following an acute coronary syndrome are at high risk and should be considered for prompt coronary angiography with a view to revascularisation.)
3-Acute circulatory failure: usually reflects extensive myocardial damage and indicates a bad prognosis
4-Pericarditis
common on the second and third days.. A pericardial rub may be audible. Opiate-based analgesia should be used. Non-steroidal and steroidal anti-inflammatory drugs may increase the risk of aneurysm formation and myocardial rupture in the early recovery period, and so should be avoided.The post-MI syndrome (Dressler's syndrome) is characterised by persistent fever, pericarditis and pleurisy, and is probably due to autoimmunity. The symptoms tend to occur a few weeks or even months after the infarct and often subside after a few days; prolonged or severe symptoms may require treatment with high-dose aspirin, NSAIDs or even corticosteroids
5-Mechanical complications
Rupture of the papillary muscle (severe valvular(mitral) regurgitation), which presents with a pansystolic murmur and third heart sound. The diagnosis is confirmed by echocardiographyRupture of the interventricular septum causes left-to-right shunting through a ventricular septal defect. accompanied by a new loud pansystolic murmur radiating to the right sternal border, but may be difficult to distinguish from acute mitral regurgitation
Doppler echocardiography and right heart catheterisation will confirm the diagnosis.
Rupture of the ventricle may lead to cardiac tamponade and is usually fatal ,.
6-Embolism
Thrombus often forms on the endocardial surface of freshly infarcted myocardium. This can lead to systemic embolism and occasionally causes a stroke or ischaemic limb. Venous thrombosis and pulmonary embolism may occur7-Impaired ventricular function, remodelling and ventricular aneurysm
Acute transmural MI is often followed by thinning and stretching of the infarcted segment (infarct expansion). This leads to dilatation and hypertrophy of the remaining ventricle ()..
left ventricular aneurysm develops in approximately 10% of patients with MI and is particularly common when there is persistent occlusion of the infarct-related vessel.., persistent ST elevation on the ECG, and sometimes an unusual bulge from the cardiac silhouette on the chest X-ray. Echocardiography is usually diagnostic. Surgical removal of a left ventricular aneurysm carries a high morbidity and mortality but is sometimes necessary.
Lifestyle modification
Cessation of smoking
Regular exercise
Diet (weight control, lipid-lowering)
Mobilisation and rehabilitation
The necrotic muscle of an acute myocardial infarct takes 4-6 weeks to be replaced with fibrous tissue and it is conventional to restrict physical activities during this period.
When there are no complications, the patient can mobilize on the second day, return home in 3-5 days and gradually increase activity with the aim of returning to work in 4-6 weeks.
The majority of patients may resume driving after 4-6 weeks, although in most countries vocational driving licence holders (e.g. heavy goods and public service vehicles) require special assessment. Emotional problems, such as denial, anxiety and depression, are common and must be addressed.,.
drugs
Asprin or other ------ long termB blocker --------------long term
Statine ---------------long term