DIABETES MELLITUS
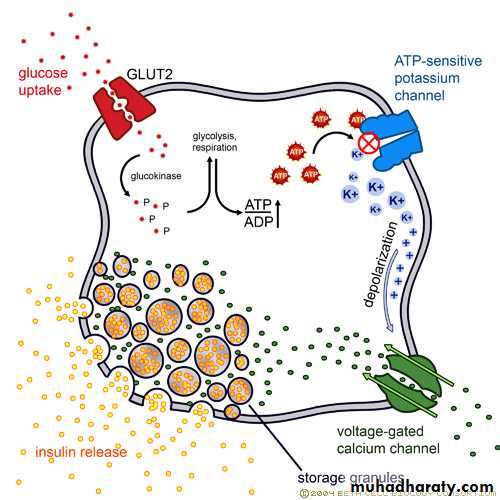
DR. FARIS ABDUL KAREEMInsulin Secretion
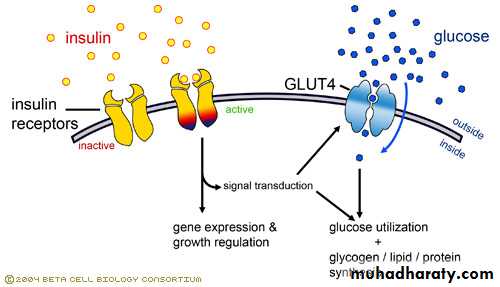
Insulin Action
A-carbohydrate1-Glucose transport (muscle, adipose tissue)
2-Glucose phosphorylation
3-Glycogenesis
4-Glycolysis
5-Pyruvate dehydrogenase activity
6-Pentose phosphate shunt activation
7-decrease Gluconeogenesis and Glycogenolysis
Insulin Action
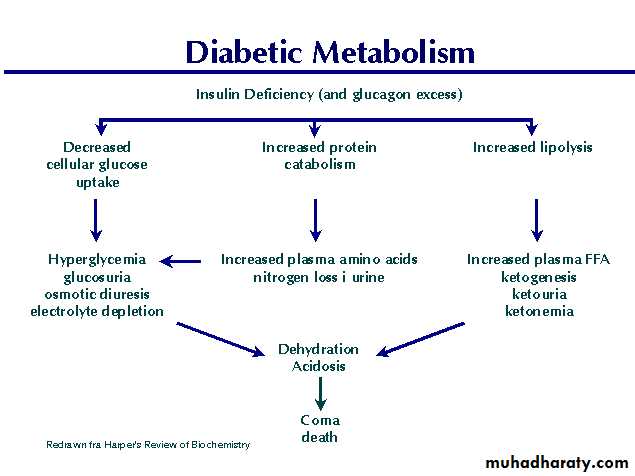
B-Lipid
1- increase Triglyceride synthesis Fatty acid synthesis (liver) Lipoprotein lipase activity
2- decrease Lipolysis , Lipoprotein lipase (muscle)
C-Protein
1- increase Amino acid transport and Protein synthesis
2- decrease Protein degradation
Disease Burden of Diabetes Mellitus
Leading cause of blindness (12.5% of cases)Leading cause of ESRD (42% of cases)
50% of all non-traumatic amputations
2.5x increase risk of stroke
2-4x increase in cardiovascular mortality
DM responsible for 25% of cardiac surgeries
Mortality in DM: 70% due to Cardiovascular disease
DM
A syndrome of absolute or relative insulin deficiency with or without resistance to its function on target cells leading to chronic hyperglycemia which affect cell function and structure with prediliction to vascular system with acute and remote complications.
Natural History of Type 2 Diabetes
Normal
Impaired glucose
toleranceType 2 diabetes
TimeInsulin
resistanceInsulin
productionGlucose
levelb
-cell
dysfunction
SYMPTOMS OF HYPERGLYCAEMIA
Thirst, dry mouthPolyuria
Nocturia
Tiredness, fatigue
Recent change in weight
Blurring of vision
Pruritus vulvae, balanitis (genital candidiasis)
Nausea; headache
Hyperphagia; predilection for sweet foods
Mood change, irritability, difficulty in concentrating, apathy
Classification
1-type 1 immune, idiopathic, LADA(latent autoimmune diabetes of adult)2-typ 2 ,MODY
3-gstational
4-other
a-insulin abnormality and ab
b-insulin receptor =
c-endocrine disease
d-drugs (steroid, thiazide)
e-congenital dis. Fredrichs, turner, down, klinfilter, DI.
TYPE 1 DM
1-genetic predisposition HLA
2-enviromental
a-viral infection
b-cow milk albumin
c-immature immune system
d-stress
e-nitosamine
TYPE 2 DM
1-genetic2-obesity and metabolic syndrome
3-sedentary life
4-age
Metabolic syndrome
HyperinsulinaemiaType 2 diabetes or impaired glucose tolerance
Hypertension
Low HDL cholesterol; elevated triglycerides
Central (visceral) obesity
Microalbuminuria
Increased fibrinogen
Increased plasminogen activator inhibitor-1
Elevated plasma uric acid
Increased sympathetic neural activity
COMPARATIVE CLINICAL FEATURES OF TYPE 1 AND TYPE 2 DIABETES
Type 1 Type 2 Typical age at onset < 40 years > 50 years Duration of symptoms Weeks Months to years Body weight Normal or low Obese Ketonuria Yes No death without insulin Yes No Autoantibodies Yes No complication at dx No 25% Family history of DM Uncommon Common Other autoimmune dis Common Uncommon
• A form of glucose intolerance that is diagnosed in some women during pregnancy.
• Gestational diabetes occurs more frequently among African Americans, Hispanic/Latino Americans, and American Indians. It is also more common among obese women and women with a family history of diabetes.• During pregnancy, gestational diabetes requires treatment to normalize maternal blood glucose levels to avoid complications in the infant.
• After pregnancy, 5% to 10% of women with gestational diabetes are found to have type 2 diabetes.
• Women who have had gestational diabetes have a 20% to 50% chance of developing diabetes in the next 5-10 years.
Gestational diabetes
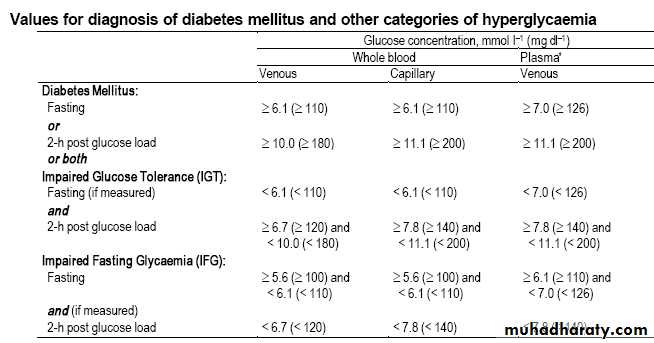
Values of Diagnosis of Diabetes Mellitus
FACTORS ASSOCIATED WITH INCREASED MORTALITY AND MORBIDITY IN PEOPLE WITH DIABETES
Duration of diabetesEarly age at onset of disease
High glycated haemoglobin (HbA1c)
Raised blood pressure
Proteinuria; microalbuminuria
Dyslipidaemia
Obesit
Management of Diabetes Mellitus
Patient education
Behavior modification
Nutrition
Weight control
Physical exercise
Blood glucose monitoring
Medications
Theraputic Goals
FBGPreprandial
2 hPP G
Midnight BG
2 AM BG
HbA1c
Theraputic Goals
In patients with type 2 diabetes, intensive glycaemic control (mean HbA1c 7%) with oral anti-diabetic agents or insulin reduced the development of microvascular complications, particularly retinopathy, by 25% compared with conventional treatment (mean HbA1c 8%).the optimal degree of glycaemic control in older people has yet to be determined. Strict glycaemic control should be avoided in the very frail patient.
older people have reduced symptomatic awareness of hypoglycaemia and limited knowledge of symptoms, and are at greater risk of and from hypoglycaemia.
In the patients with strict glycaemic control in the DCCT, weight gain was common and severe hypoglycaemic episodes occurred three times more often.
In patients with type 1 diabetes, strict glycaemic control (mean HbA1c 7%) reduced the development of retinopathy and other microvascular complications by 76% compared with conventional therapy (mean HbA1c 9%).
Medical Nutrition Therapy
Maintain short and long term body weight
Reach and maintain normal growth and development
Prevent or treat complications
Improve and maintain nutritional status
Decrease lipid intake
Quit smoking
Provide optimal nutrition for pregnancy
Nutrition Recommendations
Carbohydrate60-70% calories from carbohydrates and monounsaturated fats
Protein
10-20% total calories
Fat
<10% calories from saturated fat
10% calories from PUFA
<300 mg cholesterol
Fiber
20-35 grams/day
Low-calorie and sugar-free drinks are useful for patients with diabetes
GLUCOSE ABSORPTION
GLUCOSE PRODUCTION
Metformin
Thiazolidinediones
MUSCLE
PERIPHERAL
GLUCOSE UPTAKE
Thiazolidinediones
Metformin
PANCREAS
INSULIN human
analogue
INSULIN SECRETION
Sulfonylureas: Glyburide, Gliclazide, Glimepiride
Non-SU Secretagogues: Repaglinide, Nateglinide
Incretin; GLP-1 agonist (exentide,liraglutide)
DPPV4 antagonist (sitagliptin,saxagliptin)
GLUCOSE DISPOSAL IN URINE
ADIPOSE TISSUELIVER
Alpha-glucosidase inhibitors
INTESTINE
Sites of Action of Currently Available Therapeutic Options
Insulin
history;
extract 1920, zinc added 1935, NPH 1942, monocomponent 1970,recombinant DNA human 1980, analogues 1990s.
*preparation types;
-rapid acting (lispro, aspart, glulisine ..0.5,0.5-2.5,3-4.5h.
-short acting (soluble, regular) ..0.5-1,1-4,4-6h.
-intermediate acting (NPH,lenti) ..1-3,3-8,7-14h.
-long acting (bovine ultralenti) ..2-4,6-12.12-30h.
-long acting peekless (glargin, detemir) ..1-2,none,18-24h.
*insulin delivery; SC,IM,IV, plastic disposable syringe, pen, pressure jet, pump.
*insulin regimens; conventional (twice), MSI(basal-bolus), CSI(pump).
*complications; hypoglycemia, wt. gain, edema, insulin Ab (resistance),
insulin allergy, lipodystrophy, lipohypertrophy.
Hypoglycemia
*usually due to insulin or sulphonylurea therapy when BG below 60mg/dl.*missed meal, exercise, error dose, lipohypertrophy, gastro paresis, CRF,
malabsorption, Addison's disease, breast feeding, factiscious.
*symptoms
-autonomic- sweat, tremor, hunger, anxiety, tachycardia, tiredness.
-neuroglycopenic- confusion, headache, drowsy, loss conc., incoordinaton.
-during sleep- bad dreams, wet pillows, early morning headache.
*autonomic neuropathy may impair release of glucagon and adrenaline
(counter regulatory hormones).
*morbidity; coma, fits, TIA, brain damage, impair cognition and intellect,
arrhythmia, ischemia, vitreous bleeding, hypothermia, accidents.
*management;
-mild – oral carbohydrate
-sever- parentral glucose, IM or IV glucagon 1mg.
-asses the cause.
Non ketotic hyperosmolar coma
*less common, old, usually type 2, infection, uncontrolled therapy, neglect.*sever hyperglycemia, no ketosis, hypo K, Na, sever dehydration , confusion.*half insulin needed, half NS, antibiotics, K, HCO3.*high death 50%, septicemia, circulatory failure, thromboembolism.Lactic acidosis*usually type 2 taking metformin.*very ill, over breathing, not so dehydrated, no acetone smell, no ketone.*mortality is high 50%. *PH less than 7.2, with increase anion gap, high lactate in bl. Treated by high doses of bicarbonate.
Diabetic Ketoacidosis
*major medical emergency, average mortality 10%*type 1, new, infection, insulin dose changes, stress, AMI, septicemia.
*hyperglycemia, hyperketonemia, acidosis, hypokalemia, hyponatremia.
*polyuria, thirst, wt loss, weakness, vomiting, leg & abdominal pain, acetone
smell, dehydration, hypotension, air hunger, tachycardia, confusion, coma.
*invest; urea, K,H,Na,HCO3,Bl gases,ketone,CBC,Bl &urine culture,ECG,CXR.
*management; admission,NG tube, catheterization, CVP, antibiotics.
-insulin 20u soluble then 5u IM hourly , or analogue SC, or 5u IV with NS,
to decrease BG by 50-100mg/h, double dose if needed.
-fluid; NS 2-3lit,GW 2-3lit when BG fall to 250mg/dl.
-K ; usually in second hour if 3.5mmol/l ,40mmol given in 2h, 3.5-5 give 20.
-HCO3 , given rarely if PH less than 7.
*complications; cerebral edema, ARDS, thromboembolism, DIC, circulatory
failure,
Pathogenesis of diabetic complications
Non-enzymatic glycationOxidative-reductive stress
Increased polyol pathway activity
Intracellular myo-inositol depletion
Increased diacylglycerol synthesis
Increased protein kinase C activity
Haemodynamic disturbances
Haemorrheological and coagulation abnormalities
Microvascular hypertension
Endothelial dysfunction
Increased capillary permeability
retinopathy
retinopathy is one of the most common causes of blindness in adults between 30 and 65 years of age . increases retinal blood flow and metabolism and has direct effects on retinal endothelial cells and pericyte loss, which impairs vascular autoregulationinitially dilates capillaries but also increases production of vasoactive substances and endothelial cell proliferation, resulting in capillary closure. This causes chronic retinal hypoxia and stimulates production of growth factors. Cataract is a complication.CLINICAL FEATURES OF DIABETIC RETINOPATHY
MicroaneurysmsRetinal haemorrhages
Exudates
Cotton wool spots
Venous changes
Neovascularisation
Pre-retinal haemorrhage
Vitreous haemorrhage
Fibrosis
Classification of retinopathy
Background retinopathy(v. dilatation, exudate, microanurysm, blot bleeding)
Maculopathy
(exudate, hemorrhage, edema, ischemia)
Pre-proliferative
(small blot haemorrhages, large retinal haemorrhages Intraretinal microvascular abnormalities Multiple cotton wool spots, Macular oedema with reduced visual acuity)
Proleferative
(Pre-retinal haemorrhage ,Neovascularisation, FibrosisExudative maculopathy)
nephropathy
Is an important cause of morbidity and mortality, and is now among the most common causes of end-stage renal failure (ESRF) .Microalbuminuria is an important indicator of risk of developing overt diabetic nephropathy, although it is also found in other conditions. In particular, the presence of microalbuminuria in patients with type 2 diabetes is associated with an increased risk of macrovascular disease. Progressively increasing albuminuria, or albuminuria accompanied by hypertension, is much more likely to be due to early diabetic nephropathy
RISK FACTORS FOR DEVELOPING DIABETIC NEPHROPATHY
Poor control of blood glucoseLong duration of diabetes
Presence of other microvascular complications
Ethnicity (e.g. Asian races, Pima Indians)
Pre-existing hypertension
Family history of diabetic nephropathy
Family history of hypertension
Classification
pathological-thicining of glomerular BM.
-matrix accumulation in mesungium
-nodular deposition
-nodular or diffuse sclerosis.
*clinical
-hyperfiltr ation(high GFR)
-microalbuminuria(decreasing GFR)
-macroalbuminuria( HT, nephrotic)
-CRF……ESRD
managment
-micro;- control BG, ACEI, ARB
-macro , HT;- aggressive BP control, BG control ,if renal artery stenosis or high K diltiazim or verapamil(non-dihydropyridin Ca antag.).-CRF, ESRD;- diet, renal replacement therapy
neuropathy
a relatively early and common complication affecting approximately 30% of diabetic patients. Although in a few patients it can cause severe disabilityPathology;
-axonal degeneration
-thick schwan cell basal lamina
-patchy segmental demylination
-thick basement membrane of capillary
classification
somatic;- symmetrical(distal,sensory)
-asymmetrical( motor,proximal,amyotrophy)
-mononeuropathy( including mononeuritis multiplex, carpel tunn.)
visceral(autonomic);
-cardiovascular; hypotension(post),fixed HR, resting tachycardia -sudomotor;gustatory sweat, nocturnal sweat, anhydrosis
-pupillary;decrease pupil size, resist medriatics,delay reflex to light
-gastrointestinal;dysphagia, abdominal fullness, vomiting, nocturnal diar,const -vasomotor; cold feet, edema, bolus formation -genitourinary;incontenence , retention, infection, impotence, retrograde eject
Management
*peripheral sensory; BG control, tricyclic, gabapentin, carbamazapin, topical
capsaicin, mexilitine, antioxidant.
*postural hypotension; stocking, fludrocortisones, midodrine, NSAID
*gastroparesis; metoclopramide, erythromycin
*diarrhea; loperamide,clonidine, octeriotide
*constipation; stimulant lax(senna)
*atonic bladder; intermittent catheterization
*excess sweating; anticholinergic, clonidin, topical antimuscarinic
*impotence;sildenafil, tadalafil, sublingual apomorphin, alprostadil(PGE1) inj.
vacuum tumescence device, implant penile prosthesis, psychosexual therapy.
Diabetic foot
*Etiology-somatic neuropathy; reduce pain and proproception, claw toe…inc pressure
-autonomic N; no sweat, fissuring, alter bl. Flow, charcot ..callus
-vascular disease; claudication, cold extremities..ischemia
ulceration, infection, gangrene, amputation
*Management;
-remove callus skin -treat infection
-avoid wt bearing -control BG
-control edema -angiogram, doppler
Diabetes in pregnancy
#Gestational diabetes
*diabetes appear during pregnancy and disappear after(FBG 100,2hPG165)
*risk; obesity, previous macrosomia and family history of T2D,asian,black.
*risk to mother; DKA, worse complications, increase CS, fetal death, birth
injury, increase perinatal mortality.
*risk to fetus; congenital malformation(heart, kidney, skeletal, neural),
macrosomia, polycythemia, hypocalcemia, hypoglycemia, hyperbilirubinemia
#Pregnancy in diabetic women
*specially in type 1
*type 2 may first appear during pregnancy (check OGTT 2W after labor)
#management
-screen for GD in second trimester -plan for pregnancy for type 1
-folic acid before conception -strict control, prevent hypoglycemia
-continuous monitoring during preg. -consult gynecologist early & frequent
Infection in diabetics
*defect in immune system-depressed leucocytes function -affected phagocytosis
-impaired oxidation -depressed T cell function
-decrease chemotaxis -decrease intracellular killing
*increase risk for
-pyelonephritis -TB
-rhinocerebral mucormycosis -emphysematous cholycystitis
-perinephric abscess -candidiasis
-boils -papillary necrosis
-necrotizing fasciitis -osteomylitis
-malignant otitis externa -foot infection
Skin disease in diabetes
*microvascular
-dermopathy -necobiosis lipodica diabetecorum
-bolus diabeicorum
*infection
-candidiasis -boils
*autoimmune
-vetiligo
*drugs
-lipodystrophy -lipohypertrophy
-allergic dermatitis
*others
-eruptive xanthoma -alopecia
-dry skin,fissuring